Module # 4 – Upper GI Bleeding
advertisement

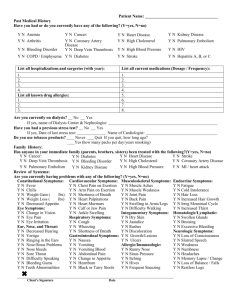
Facilitator Version Module # 4 – Upper GI Bleeding Objectives: 1. Understand the initial diagnostic evaluation and management steps for upper GI bleeding 2. Understand indications for intensive care unit admission in upper GI bleeding 3. Develop a differential diagnosis for upper GI bleeding 4. Understand risks for re-bleeding and strategies for prevention of variceal bleeding in cirrhosis References: Laine L, Jensen DM. “Management of patients with ulcer bleeding.” Am J Gastroenterol. 2012 Mar;107(3):345-60 Garcia-Tsao G, et al. “Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis.” Hepatology. 2007;46(3):922. Villanueva C, et al. “Transfusion Strategies for Acute Upper Gastrointestinal Bleeding” N Engl J Med 2013; 368:11-2 MKSAP 16 CASE 47 yo M with history of alcohol abuse and cirrhosis presents with several episodes of bloody emesis in the setting of a recent EtOH binge. What other historical questions do you want to know? (med students) NSAID use, coffee grounds vs. BRB, retching/emesis prior to development of hematemesis, symptoms of hypovolemia (dizziness/presyncope/orthostasis/etc.), melena or hematochezia, previous history of prior bleeding episodes, abdominal pain The patient reports dark tarry stools since this morning. He has had 5 episodes of coffee ground emesis. He denies NSAID use. He also endorses lightheadedness upon standing. He reports one prior episode of throwing up blood about a year ago but did not seek medical attention. Vital signs in triage are: afebrile, HR 125, BP 80/50, RR 12, SaO2 normal on RA. Per chart review his baseline BP runs 110s/70s. What is your initial differential and what are you initial orders? Roughly how much blood loss would you estimate based on the patient’s vitals? What are you looking for on your focused physical exam? (students and interns) Differential: variceal bleed, PUD (H. pylori vs. NSAIDs), EtOH gastritis, Mallory Weiss tear. Less likely esophagitis, Dieulafoy’s lesion, AVM, malignancy, portal gastropathy. Initial orders: 2 large bore IVs (18 gauge minimum), NS bolus, type and cross, CBC, INR, Chem 7, LFTs, NPO, NG lavage, q4 H/H Estimate at least 20-25% blood loss based on resting hypotension. Orthostatic hypotension or tachycardia suggests 10-20% blood loss, normal vitals <10% Exam: No need to do orthostatics as patient already hypotensive so know blood loss is significant. Looking for mental status, stigmata of chronic liver disease, abdominal exam for tenderness, ascites, and hepatosplenomegaly, RECTAL – appearance of stool most important (i.e. is it melena/hematochezia or not?), not guiac testing. Check for asterixis. Supraclavicular LAD can suggest GI malignancy. The patient is taken to the resus room, 2 large bore peripheral IVs are placed and your labs are drawn. 1.5 L normal saline bolus is orders. On exam, the patient is alert and oriented x3. His sclera are anicteric, heart is notable for regular tachycardia, GI exam shows distended abdomen with fluid wave, caput medusa, spider angiomata, and palmar erythema. There is no asterixis. Rectal exam shows melena. Initial labs: CBC: WBC 10.2, Hgb 8.1, Hct 24, Plt 60. Baseline H/H per chart review is 12/36. Chem 7: Na 131, K 3.1, Cl 100, HCO3 22, BUN 40, Cr 0.9 LFT: TP 6.0, Albumin 3.0, AST 205, ALT 98, Alk Phos 150, T bili 2.0; INR 2.0 NG lavage done showing bright red blood that does not clear after 1.5 L of lavage After 1.5 L NS bolus the patient’s HR decreases to 100 and BP up to 95/60 Additional orders? Where should the patient be admitted? (intern/resident) -Order Pantoprazole and octreotide drips, ceftriaxone, Vitamin K if not ordered with initial orders -Consutl GI for endoscopy -Consider pRBCs transfusion as patient continues to actively bleed even though hemoglobin is not <8. Discuss NEJM article showing improved outcomes with restrictive transfusion strategy (transfusion for Hgb<7) vs. liberal strategy (Hgb<9). Note that massive bleeding was one of the exclusion criteria for this trial. -Transfuse FFP -Patient should be admitted to MICU for emergent EGD given evidence of ongoing bleeding with NG lavage not clearing. Other indications for MICU admission: hypotension/hemodynamic instability, respiratory distress The patient is admitted to the MICU service and is placed on octreotide and pantoprazole drips and ceftriaxone. GI is called and are on their way for emergent endoscopy. 4 units of FFP are ordered. The patient continues to have BRB from the NG tube. His HR is back up to 120 and BP down to 80/60. Repeat H/H come back at 6/18. Any additional orders? (upper level resident) -Transfuse 2 units pRBCs, bolus -Place central line. Which kind? Cordis to facilitate fluid resuscitation. Traditional triple lumen CVCs can’t infuse large volumes of fluid rapidly due to their length and small diameter (remember Poiseuille’s law?). You can actually infuse fluids much faster through 2 large bore PIVs vs. a triple lumen CVC. What other options do you have if the patient continues to actively bleed? (upper level resident) -Balloon tamponade with Blakemore tube can be attempted as a temporizing measure to definitive endoscopic therapy or TIPS. Patient needs to be intubated for this to be done. -TIPS can be considered in hemorrhage refractory to endoscopic/medical therapy You place a cordis, bolus 2 more liters of NS and transfuse 2 units of pRBCs in addition to the FFP previously ordered. The patient’s HR drops back to 90 and BP is up to 100/60. GI performs endoscopy which shows multiple columns of varices with stigmata of recent hemorrhage. The patient is banded x4. The patient is monitored in the MICU overnight. His H/H are stable at 8.2/24 for the last 12 hours and his vital signs are now stable. What changes can you make to his medications? How long should the patient remain in the hospital? What are risk factors for rebleeding? (upper level resident) The patient needs to complete 72 hours of octreotide drip. The PPI can be stopped at this time. Continue antibiotics for SBP prophylaxis. Continue H/H monitoring but frequency can be decreased. If ascites present on exam or imaging should be tapped to r/o SBP. Risk factors for rebleeding: Endoscopic: Visible vessel, active bleeding, adherent clot, variceal bleeding. Clinical: Advanced age, comorbid illness, coagulopathy, large volume bleeding, bleeding that began during hospitalization The patient is transferred to the medicine service and continued on the octreotide drip for a total of 72 hours without signs of rebleeding. RUQ US is obtained which shows an echogenic liver and moderate volume ascites. You tap his ascites with ultrasound guidance and this confirms portal HTN and absence of SBP. You decide the patient is stable for discharge. What new medications do you prescribe and what is your follow-up plan? -Need 7 day course total of prophylactic antiobitcs. IV ceftriaxone can be converted to norfloxacin or ciprofloxacin to complete treatment course at discharge -Follow-up endoscopy usually recommended at 4-6 weeks after banding. AASLD guidelines recommend endoscopic variceal ligation be repeated every 1 to 2 weeks until obliteration, with the first surveillance EGD performed 1 to 3 months after obliteration and then every 6 to 12 months to check for variceal recurrence -Non-selective beta-blockade: this is more controversial, but guidelines recommend combination of banding + non-selective beta-blocker in all patients with compensated cirrhosis who have bled from varices. For primary prevention the recommendation for BB is in all patients except those with Childs A cirrhosis + small varices (these patients should have routine EGD monitoring). Recommended initial doses are nadolol 40 mg once a day or propranolol 20 mg bid at low dose titrated to HR 55-60. Caution that recent data suggests BB may worsen survival in those with diuretic resistant ascites and guidelines recommend d/c of BB if patient develops this. MKSAP 16 Questions: Question 19 – Manage high risk peptic ulcers. Answer D. Question 58 – Manage upper GI bleeding and hemodynamic instability. Answer A. Question 65 –Evaluate obscure upper GI bleeding. Answer C. Question 75 – Variceal bleed prophylaxis. Answer A. Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111). 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student