Appendix A. Laboratory Assessments. All laboratory assessments
advertisement

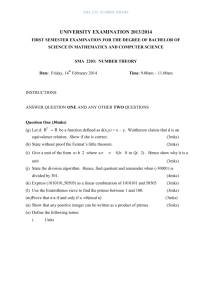
Appendix A. Laboratory Assessments. All laboratory assessments were performed at a CDC certified central laboratory (Medpace Reference Laboratories, Cincinnati, OH, USA). (1) Total cholesterol (TC), triglycerides (TG) and high-density lipoprotein cholesterol (HDL-C) were measured by enzymatic colorimetry (HDL-C was isolated after dextran sulphate precipitation of apoB). The Friedewald formula, or ultracentrifugation if TG concentration was ≥399 mg/dL, was used to calculate LDL-C concentration. Lp(a) was measured by an isoform independent assay standardized to the Northwest Lipid Research Clinic protocol. ApoB and apolipoprotein A-I (apoA-I) were measured by rate nephelometry. High-sensitivity C-reactive protein (HsCRP) was measured by immunonephelometry. MRI measurement of hepatic fat was performed at baseline, at the end of the treatment period (Week 28), and at the end of the off-treatment 24 week followup period (Week 50). MRI assessments of hepatic fat fraction were undertaken at a core facility by a blinded assessor. Patients discontinued medication if ALT or aspartate aminotransferase (AST) levels were: >8xULN, >5xULN at 2 consecutive weekly measurements, or >3xULN in conjunction with total bilirubin >1.5xULN or international normalized ratio >1.5. Statistical Analysis. A 90% power to detect a 20% difference between the 2 groups required a sample size of 60; assuming standard deviation of 22% for the percent change in LDL-C, 158 patients were randomized to compensate for patient drop-outs and to expand the safety database. Efficacy analyses included all patients who received study drug and had at least one postbaseline lipid assessment; mean and two-sample t-test was used for between group comparisons unless the Kolmogorov-Smirnov test of normality was statistically significant (p<0.05), in which case the median and the Wilcoxon rank sum test were utilized. Changes within treatment groups were assessed using the Wilcoxon signed-rank test. Statistical significance was defined as p<0.05. Inflation of type 1 error due to multiple secondary endpoints was controlled by use of a sequential inferential approach in which statistical significance of the primary endpoint was required before drawing inferential conclusions about the first secondary endpoint and inferential conclusions about each successive secondary endpoint required statistical significance of the prior one.(2) Safety analyses used all patients who received at least one dose of study medication. Results at Primary Efficacy Timepoint and over time were repeated by T2DM status and regression analysis was performed to assess the impact of baseline LDL-C, age, gender, and race on LDL-C change. All analyses were performed using SAS version 9.2 (Cary, NC). References 1. Centers for Disease Control and Prevention. Laboratory Quality Assurance and Standards Programs, Lipid Standardization Program, 2010. http://www.cdc.gov/labstandards/lsp.html. Accessed 4/11/2012. 2 Hsu, JC. Multiple Comparisons: Theory and Methods. Chapman & Hall, London, 1996:1-296. Appendix B. Patients Discontinuing Due to Adverse Event Pt. No. Adverse Event (Severity) SAE Mipomersen 1 Lethargy (mod) No 2 Palpitations (mod), Fatigue (sev), Chills (mod), Pyrexia (mod) No 3 Myalgia (mild), ALT increase (sev), AST increase (mod) No 4 LFT abnormal (mod) No 5 LFT abnormal (mod) No 6 Influenza (mod) No 7 Pain (sev) No 8 Depression (sev) No 9 ISR – recall (mod) No 10 Lethargy (sev), Vomiting (sev), Chills (sev) No 11 Hepatic enzyme increase (sev) No 12 Urticaria (mod) No 13 ISR – pain (mod) No 14 Constipation (mod) No 15 Chills (mod), Myalgia (sev), ISR – erythema (mod/sev), pruritus (mod/sev) No 16 ISR – pruritus (mild/sev), erythema (sev) No 17 ALT increase (mod), hepatic steatosis (sev) No 18 ALT increase (mod), platelet count decrease (sev) No 19 Rash (mild) No 20 Presyncope (mild) No 21 ALT increase (mod) No 22 ISR – erythema (mild/mod), pain (mild) No 23 ISR – urticaria (mod), pain (mild/sev) No 24 ISR – swelling (mod/sev), warmth (mild), pain (mod/sev), erythema (mod) No 25 Pain in extremity (sev) No 26 Non-small cell lung cancer (sev) Yes 27 Acute myocardial infarction (sev) Yes 28 Blood creatinine increase (sev), blood urea increase (mod) No Placebo ISR=injection site reaction; LFT=liver function test; SAE=serious adverse event; Mod=moderate; Sev=severe Appendix C. Study Investigators Eddie Armas, MD, Miami, FL Boris Kerzner, MD, Baltimore, MD Armen Arslanian, MD, Brockton, MA Michael Koren, MD, Jacksonville, FL Harold Bays, MD, Louisville, KY Mariananda Kumar, MD, Inverness, FL Prakash Bhatia, MD, PhD, Escondido, CA David Lee, MD, Portland, OR Barry Blumenthal, DO, Aventura, FL Irving Loh, MD, Thousand Oaks, CA Mark Cervi, MD, Greenville, NC Richard Marple, MD, Tulsa, OK Lisa Cohen, DO, New Port Richey, FL Andres Patron, DO, Pembroke Pines, FL Lisa Connery, MD, Norman, OK Edward Portnoy, MD, Westlake Village, CA William Cromwell, MD, Charlotte, NC Geri Poss, MD, San Antonio, TX Michael Davidson, MD, Chicago, IL Matthew Reeves, DO, Bloomington, IN Natalie Doyle, MD, Wilson, NC Sheila Rodstein, MD, Edina, MN Steven Elliott, MD, Evansville, IN Anthony Scarsella, MD, Beverly Hills, CA W. Timothy Garvey, MD, Birmingham, AL Gladstone Sellers, MD, Sandy Springs, GA C. Allen Goetsch, MD, Huntsville, AL Erich Schramm, MD, Ponte Vedra, FL David Hassman, DO, Berlin, NJ Richard Shultzaberger, MD, Greenville, NC John Homan, MD, Newport Beach, CA Louis Stephens, Jr., MD, Simpsonville, SC Timothy Howard, MD, Huntsville, AL Danny Sugimoto, MD, Chicago, IL Richard Hyman, MD, Los Angeles, CA Gregory Thomas, MD, MPH, Mission Viejo, CA Charles Fogarty, MD, Spartanburg, SC Phillip Toth, MD, Indianapolis, IN Ernesto Fuentes, MD, Miami, FL Daniel Weiss, MD, Mentor, OH Peter Jones, MD, Houston, TX Alexander White, MD, Port Orange, FL Eric Klein, MD, Olympia, WA Supplemental Figure Legends Supplemental Figure 1. Patient Flow. This placebo-controlled study enrolled 158 patients; 105 were treated with mipomersen. (Appendix) A B C D Supplemental Figure 2. Correlations In Liver Parameters. PET=primary efficacy time point; EOT=end of treatment. (Appendix) (A). ApoB vs. LDL-C; r=0.95 Percent Changes from Baseline in ApoB vs. LDL-C at PET (B). ApoB vs. Liver Fat; r=-0.52 Percent Change from Baseline in ApoB at PET vs. Change in Liver Fat Fraction at EOT (C). ApoB vs. Alt; r=-0.44 Percent Change from Baseline in ApoB at PET vs. Maximum ALT (D). Liver Fat vs. ALT; r=0.52 Change in Liver Fat Fraction at EOT vs. Maximum ALT (U/L)