Booklet 2010 - Ministry of Health
advertisement

Ministry of Health Rwanda Health Statistical Booklet 2010 Published in July2011 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table of Contents List of Tables: ......................................................................................................................................... 4 List of Figures ......................................................................................................................................... 5 Acronyms: ............................................................................................................................................... 6 Foreword ................................................................................................................................................. 7 Introduction ............................................................................................................................................. 8 Health Sector Infrastructure .................................................................................................................... 9 Health Facilities .................................................................................................................................. 9 Health Facility Equipment and Utilities............................................................................................ 13 Communication ................................................................................................................................. 14 Human Resources ................................................................................................................................. 16 Morbidity and Mortality ....................................................................................................................... 17 Outpatient care .................................................................................................................................. 17 District Hospital Outpatient Morbidity ......................................................................................... 18 Health Centre Outpatient Morbidity ............................................................................................. 19 Hospitalization and Mortality ........................................................................................................... 21 Admissions and mortality in health centers and district hospitals ................................................ 21 Leading causes of mortality in health facilities............................................................................. 22 Family Planning ................................................................................................................................ 24 Ante-Natal Care ................................................................................................................................ 25 Cesarean sections at Hospitals ...................................................................................................... 28 Weight at birth and deaths of newborns........................................................................................ 28 Child immunizations ......................................................................................................................... 29 Growth Monitoring ........................................................................................................................... 30 Malnutrition ...................................................................................................................................... 30 Hospitalization for Childhood Malnutrition.................................................................................. 30 Outpatient treatment of Malnutrition ............................................................................................ 30 Community Health Worker Program .................................................................................................... 31 Community IMCI: ............................................................................................................................ 31 Sexual Violence .................................................................................................................................... 33 TB and HIV/AIDS ................................................................................................................................ 34 Tuberculosis (TB) ............................................................................................................................. 34 HIV /AIDS ........................................................................................................................................ 34 VCT............................................................................................................................................... 34 PIT ................................................................................................................................................ 36 Preventing Mother to Child Transmission (PMTCT) ................................................................... 36 HIV exposed infants follow up ..................................................................................................... 38 Care and treatment ........................................................................................................................ 38 2 Rwanda Ministry of Health Annual Statistical Booklet 2010 HIV among Groups at high risk. ................................................................................................... 38 MALARIA. ........................................................................................................................................... 43 Laboratory ......................................................................................................................................... 45 SURGERY ............................................................................................................................................ 46 RADIOLOGY ....................................................................................................................................... 47 PERFORMANCE-BASED FINANCING:........................................................................................... 47 COMMUNITY-BASED HEALTH INSURANCE /MUTUELLE (CBHI).......................................... 49 Sources of Data ..................................................................................................................................... 51 HMIS ................................................................................................................................................ 51 Rwanda National Population Projections 2007-2022 ................................................................... 51 TracNet ......................................................................................................................................... 51 PBF ............................................................................................................................................... 52 CBHI indicator database ............................................................................................................... 52 Rwanda District Health System Strengthening Tool (DHSST) ........................................................ 52 Rwanda Interim DHS 2007-2008 (RIDHS) ...................................................................................... 52 Annexes: ........................................................................................................................................... 53 3 Rwanda Ministry of Health Annual Statistical Booklet 2010 List of Tables: Table 1: Number of Health Facilities 2009-2010 ................................................................................... 9 Table 2: Number and type of health facility by district ........................................................................ 11 Table 3: Minimum package of services in different facilities ............................................................... 12 Table 4: Availability of power in health facilities ................................................................................ 13 Table 5: Primary source of electricity in health facilities 2009 – 2010 ................................................ 14 Table 6: Availability of water in health facilities.................................................................................. 14 Table 7: Internet/Telephone access for district hospitals and health centers ........................................ 15 Table 8: Availability of computers in district hospitals and health centers .......................................... 15 Table 9: Number of inpatient beds by health facility type .................................................................... 15 Table 10: Vehicle access at district hospitals and health centres .......................................................... 15 Table 11: Facilities with selected fully functional equipment .............................................................. 16 Table 12: Ratio of health workers to population................................................................................... 16 Table 13: Number of outpatient visits in Health Centers and District Hospitals .................................. 17 Table 14: Top ten causes of outpatient visits in district hospitals in 2010............................................ 19 Table 15: Top 10 causes of morbidity in health centers in 2010 .......................................................... 20 Table 16: Number of admissions in health facilities by gender ............................................................ 21 Table 17: Number of deaths reported in health facilities ...................................................................... 21 Table 18: Top ten causes of deaths in district hospitals and Health Centers ........................................ 22 Table 19: Top 10 causes of inpatient hospitalization in district hospitals and health centers among the under five in 2010 ................................................................................................................................. 23 Table 20: Family Planning Users by method and units distributed ...................................................... 24 Table 21: Pregnant women registered for ante-natal care ..................................................................... 25 Table 21: Location of assisted deliveries .............................................................................................. 27 Table 22: Causes of maternal death, 2010 ............................................................................................ 27 Table 23: Caesarian sections in District Hospitals and Referral Hospital ............................................ 28 Table 24: Birth and perinatal death in health centers and district hospitals .......................................... 28 Table 25: Childhood vaccination and ITN distribution ........................................................................ 29 Table 26: Nutrition status of children monitored in health centers ....................................................... 30 Table 27: Hospitalization for childhood malnutrition and health outcomes ......................................... 30 Table 28: Outpatient treatment of malnutrition and health outcomes................................................... 31 Table 29: Sexual violence by age and gender ....................................................................................... 33 Table 30: CHWs Participation in Community DOTS 2007 to 2010 .................................................... 34 Table 31: Success rate of Sputum Smear + for Tuberculosis enrolled in 2009 .................................... 34 Table 32: HIV testing of Tuberculosis + Patients ................................................................................. 34 Table 33: Anti-Retroviral Therapy in Rwanda from 2007 to 2010 ...................................................... 38 Table 34: Number and percentage of respondents reporting using a condom at the last sexual intercourse by type of partner, age, province and sites, (N=1,136) ................................................... 41 Table 35: HIV prevalence of FCSW by background characteristics, 2010 Rwanda BSS. ................... 42 Table 36: Distribution of Malaria diagnoses by health facility type ..................................................... 44 Table 37: Type of lab Tests conducted at different health facilities ..................................................... 45 Table 38: Type of surgery performed ................................................................................................... 46 Table 39: Selected surgical interventions ............................................................................................. 46 Table 40: Medical imagery and other diagnostic testing procedures .................................................... 47 Table 41: Performance-Based Financing payments by year and PBF package .................................... 47 Table 42: Summary of CBHI income and expenditure ......................................................................... 50 4 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 43: Classification of staff categories by qualification ................................................................. 53 List of Figures Figure 1: Map of Health Facilities in Rwanda, 2010 ............................................................................ 10 Figure 2: Distribution of health facilities by type ................................................................................. 12 Figure 3: Distribution of health facility by management authority ....................................................... 13 Figure 4: Map of Outpatient utilization rate, Rwanda, 2010 ................................................................ 18 Figure 6: Causes of Outpatient visits in district hospitals (updated)..................................................... 19 Figure 7: Distribution of outpatient morbidity in health centers ........................................................... 20 Figure 11: Trend of family planning coverage among married women, 1990-2007 ............................ 24 Figure 10: Infant death ratio by level of health care facility as reported in 2009 and 2010 ................. 29 Figure 12: Children treated by CHWs as part of Community IMCI ..................................................... 31 Figure 13: Outcomes of Community IMCI........................................................................................... 32 Figure 14: Nutritional status-MUAC by CHWs, 2010 ......................................................................... 33 Figure 15: Distribution of people tested for HIV/AIDS by sex ............................................................ 35 Figure 16: Age distribution and seroprevalence of clients tested for HIV in health facilities, Rwanda 2010 ...................................................................................................................................................... 36 Figure 17: Voluntary Counseling and Testing during ante-natal clinics .............................................. 37 Figure 18: Percent of Partner tested from 2003 to 2010 ....................................................................... 37 Figure 19: Circumcision Pattern of Youth Males in the 2009 Rwanda Youth BSS (N = 2,522) ......... 38 Figure 20: Comparison of Youth Sexual Behaviors between 2006 and 2009 BSS, Rwanda ............... 39 Figure 21: Youth Comprehensive Knowledge of HIV/AIDS, Rwanda Comparison between 2006 and 2009 ...................................................................................................................................................... 40 Figure 22: HIV knowledge comparison between 2006 and 2010 FCSW BSS, Rwanda ...................... 43 Figure 23: Graph of proportional morbidity for Malaria 2009-2010 in health centers ......................... 44 Figure 24: Map of proportional malaria morbidity by District 2010 .................................................... 45 Figure 25: Evolution of key Maternal and Child services (Average numbers per facility) .................. 48 Figure 26: Evolution of Average Quality scores from Health Center PBF Quality Assessments ........ 49 Figure 27: Map of Mutuelle Adhesion Rates by district 2010 .............................................................. 50 Figure 28: Evolution du taux d'adhésion aux mutuelles de santé 2003-2011 ....................................... 51 5 Rwanda Ministry of Health Annual Statistical Booklet 2010 Acronyms: ANC – Ante-natal care ARBEF– Association Rwandaise pour le Bien-Etre Familial (Rwanda Association for Family welfare) ART – Anti-retroviral therapy ARV – Anti-retroviral BCG – Bacille Calmette Guerin vaccination CPY - Couple Year Protection DH – District hospital DHS– Demographic and Health Survey DOT- Directly Observed Treatment Short Course DTP – Dyptheria, tetanus, pertusis vaccination ECG- electro-cardiogram EPI –Expanded Program on Immunizations FBO – Faith-based organization FP – Family Planning GO – gynaecology-obstetrics HC – Health centre HiB – Hemophelus Influenza B vaccination HIV/AIDS– Human Immunodeficiency Virus/ Aquired Immunodeficiency Syndrome HMIS – Health Management Information System iHRIS – Integrated Human Resource Information System ITN - Insecticide Treated Nets MCH – Maternal and Child Health NGO– Non-Governmental Organization NID – National Identity card NRH- National Referral Hospital OPD – Out Patient Days P0 – polio vaccination dose zero PBF – Performance-Based Financing RDHSSF – Rwanda District Health System Strengthening Framework RH – Referral Hospital RIDHS – Rwanda Interim Demographic and Health Survey SS+ - Sputum Smear Positive TB – Tuberculosis TPM+ - positive microscope pulmonary tuberculosis VCT –Voluntary Counseling and Testing 6 Rwanda Ministry of Health Annual Statistical Booklet 2010 Foreword As part of the Government of Rwanda’s commitment to produce evidence-based policies and programs, it is imperative that we generate and publish reliable statistics and indicators that can be used by all stakeholders. This Annual Rwanda Health Statistical Booklet has therefore been produced to provide a summary of all key statistics from the Rwandan health sector in 2010. This Booklet will enable policymakers, planners and other interested parties to gain an insight into the current state of the Rwandan Health Sector. These important statistics provide a basis for policies, strategies and planned interventions to ensure they are responsive to the needs of the health sector and, crucially, are focused on addressing current priorities that aim to improve the health of the Rwandan population. Dr Agnes BINAGWAHO Minister of Health 7 Rwanda Ministry of Health Annual Statistical Booklet 2010 Introduction The Rwanda Annual Health Statistical Booklet 2010 has been developed to provide an overview of key statistics in the health sector for 2010. This is the second year in a row that the bulletin has been produced and the first time that there is substantial data available from two calendar years enabling an analysis of trends over time. The Booklet is divided into four chapters: Infrastructure; Human Resources; Morbidity; and Special Programs including Family Planning, TB, HIV/AIDS, Malaria and MCH. This year we have also added a section on several health financing interventions: Performance-Based Financing and Community-Based Health insurance. Other macro level financial information has not been included in this document as this is covered substantially by the National Health Accounts and other special studies and reports. This booklet aims to show key statistics in the health sector from 2010 in a concise, easily accessible manner to ensure valuable statistics are readily available to all interested users. Comparisons with 2009 will help users understand the evolving health situation in Rwanda. Data have been extracted from a variety of sources: the Rwanda District Health System Strengthening Tool (DHSST); the Health Management Information System (HMIS); TracNet; PBF databases for clinical services, community health workers; the Community-Based Health Insurance (CBHI) indicator database, and several surveys, including: the Rwanda Interim DHS 2007-2008 and the WHO Survey of Human resources 2009. Details of all data sources are given in the annexes. This document includes data from primary health care facilties and district hospitals managed by the public sector or faith-based organisations that operate under a convention with the Ministry of Health (known as ‘agrée’). Limited data is also included from national referral hospitals to provide a more comprehensive picture of infrastructure and disease burden. This year the Booklet also includes some data from the newly implemented Community Health Worker Information system (SISCom). It does not include data from private sector clinics or dispensaries. 8 Rwanda Ministry of Health Annual Statistical Booklet 2010 Health Sector Infrastructure Health sector infrastructure covered in this section includes health facilities and selected resources available within those facilities, such as staff, equipment, utilities and transport. It is important to note that this section draws data from multiple sources, primarily the Health Facilities Database, the WHO Human Resource Survey and the Rwanda District Health System Strengthening Tool (DHSST). The coverage of the DHSST represents a sub-set of health facilities, and therefore may not be entirely representative of the national picture. Health Facilities The number of non-private Health Facilities (HFs) in Rwanda at the end of 2010 was 579; this is up from 541 in the previous year. This increase was primarily due to the opening of 11 new health posts, 2 new Prison Dispensaries, 17 new Dispensaries and 8 Health Centers. These are classified as Referral Hospitals, District Hospitals, Health Centers, Health Posts and Dispensaries. Table 1: Number of Health Facilities 2009-2010 Year National Referral Hospitals District Hospitals Police Hospital Health Centers 2009 4 2010 4 40 1 428 40 1 436 Dispensaries 18 35 Prison Dispensaries 16 18 34 541 45 579 Health Posts Grand Total Source: Health Facilities Database, HMIS unit 2009-2010 9 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 1: Map of Health Facilities in Rwanda, 2010 Source: Health Facilities Database, HMIS unit 2010 The number and type of health facility per district is shown in table2 10 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 2: Number and type of health facility by district District BUGESERA BURERA GAKENKE GASABO GATSIBO GICUMBI GISAGARA HUYE KAMONYI KARONGI KAYONZA KICUKIRO KIREHE MUHANGA MUSANZE NGOMA NGORORERO NYABIHU NYAGATARE NYAMAGABE NYAMASHEKE NYANZA NYARUGENGE NYARUGURU RUBAVU RUHANGO RULINDO RUSIZI RUTSIRO RWAMAGANA Grand Total Referral Hospital 2 1 1 4 District Hospital 1 1 2 1 2 1 2 1 1 3 2 1 1 1 1 1 2 1 1 2 2 1 1 1 1 1 1 2 1 1 40 Military/ Police Hospital 1 1 Health Centre 14 15 18 15 20 21 13 15 11 19 15 8 11 13 11 12 12 16 21 17 18 16 8 15 9 13 18 14 16 12 436 Dispensary Prison Dispensary Health Post # of Health Facilities 1 1 3 1 2 16 16 26 19 26 23 16 22 19 25 26 10 14 15 19 18 26 21 27 23 21 19 13 16 12 17 19 18 18 19 35 18 45 579 1 5 1 4 1 3 7 3 5 1 2 4 2 1 5 1 5 1 1 2 2 2 4 7 3 4 2 1 2 1 1 1 3 2 Source: HMIS National Health Facility Database. Excludes private health facilities and FOSACOM Of the 579 health facilities, 76% are health centers, 7% District Hospitals, 8% Health Posts and 6% Dispensaries (see Figure 1). There are also 4 Referral Hospitals, 1 Police Hospitals1 and 18 prison Dispensaries. This analysis, using data from the HMIS National Health Facility Database, encompasses health facilities managed by the public sector or Agrees (faith-based organizations), but does not include private health facilities which administrative districts have not systematically registered. 11 Note: since 2006 Kanombe Military Hospital serves as a District Hospital for the general population in Gasabo district, so it has been re-classified as a District Hospital in this analysis. 11 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 2: Distribution of health facilities by type 0% 1% Health Centers 8% Prison Dispensaries 7% 6% Dispensaries 3% District Hospitals 75% Police Hospital National Referral Hospitals Source: HMIS National Health Facility Database The minimum package of services provided by the main categories of facilities is summarized below: Table 3: Minimum package of services in different facilities Health facilities National Referral Hospital District hospitals Health centres Dispensaries Health posts Minimum package of services provided Advanced inpatient/outpatient services , surgery, laboratory, gynaecology, obstetrics; radiology, specialized services: ophthalmology, dermatology, ENT, stomatology, physiotherapy…. Inpatient/outpatient services, surgery, laboratory, gynaecology obstetrics, radiology Prevention activities, Primary health care, inpatient, referral, maternity Primary health care, outpatient, referral Outreach activities (immunization, family planning, growth monitoring, antenatal care) Two of the four referral hospitals also serve as teaching institutions for doctors and pharmacists. Ndera hospital is the referral hospital for mental health. Two other facilities, Kanombe Military hospital and Kacyiru Police hospital, cover the surrounding civilian population in addition to the Rwandese Defence Forces and the National Police Public health facilities represent 64% of the total number of non-private health facilities in Rwanda, with 28% run by Faith-Based Organizations referred to as “Agrée”, 1% parastatal, 5% private and 2% by Communities. 12 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 3: Distribution of health facility by management authority Number of Facilities by Management Authority 28% Agree Community Parastatal 64% 2% 1% 5% Private Public Source: HMIS National Health Facility Database 2010 Health Facility Equipment and Utilities According to the Rwanda District Health System Strengthening Tool2, a web-based database maintained by all of the districts with data on 465 Health Facilities (of which 41 were DH, Kanombe Military Hospital and Kacyiru Police Hospital, and 424 HCs), 19% of health centers and 2% of district hospitals had no access to power in 2009 – a figure that has been nearly halved to 15% of health centers and 0% of district hospitals in 2010. The improvements have come about mostly because of additional sites being added to the power grid and with the purchase and of generators and solar installations. Table 4: Availability of power in health facilities Power Status No power 2009 79 Health Centers % 2010 19% 64 % 15% 2009 1 District Hospitals % 2010 % 2% 0 0% Some power (inconsistent grid, generator or solar) 176 42% 196 46% 6 15% 8 20% Connected to grid (with consistent access) 166 39% 164 39% 34 83% 33 80% Total 421 424 41 41 Source: Rwanda District Health System Strengthening Tool, 2009-2010 The District Health System Strengthening Tool also showed improvements between 2009 and 2010. The number of health centers with power increased from 81% to 85% of health centers from 2009 to 2010 respectively. There was a slight increase in the proportion of facilities connected to the electricity grid from 43% in 2009 up to 46% in 2010. In most of heath facilities using solar energy and generator, power may not be sufficient. Most other electricity sources remained proportionally the same. 2 The DHSST did not include health posts or dispensaries 13 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 5: Primary source of electricity in health facilities 2009 – 2010 Primary Electricity Source Electricity grid 2009 Percentage 2010 Percentage 198 43% 213 46% 54 12% 49 11% 147 32% 155 33% Biogas 2 0% 1 0% Other 40 9% 7 2% No power 21 5% 40 9% Generator Solar energy Total 462 465 Source: Rwanda District Health System Strengthening Tool, 2009-2010 Water supply did not change between 2009 and 2010 – roughly one quarter of the facilities is connected to the national water supply grid. According to the DHSST the proportion of facilities using local surface water in 2009 is 18% same in 2010. Table 6: Availability of water in health facilities Primary Water sources 2009 Percentage 2010 Percentage Local Water System 149 121 95 84 6 4 2 32% 26% 21% 18% 1% 1% 0% 0% 127 138 93 86 3 4 3 27% 30% 20% 18% 1% 1% 1% - National Grid Rainwater Harvesting Local Surface Water Well or Borehole, Covered Well or Borehole, Uncovered Tanker Truck Unknown Source Doesn't Exist Total 1 462 - 12 466 3% Source: Rwanda District Health System Strengthening Tool, 2009-2010 Communication In 2010, all district hospitals were connected to the internet (up from 88% in 2009), 98% had cell phone coverage (up from 95% in 2009). The improvements were made in internet connectivity at the health center level with 65% having access to the internet in 2010 as opposed to 41% in 2009. The proportion of health centers with cell phone coverage increased from 90% to 97%. 14 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 7: Internet/Telephone access for district hospitals and health centers Facility type Internet 2009 District Hospitals Health Centers 36 88% 2010 41 100% 171 41% 275 65% Cell Phone Coverage 2009 2010 39 95% 40 98% 377 90% 412 97% Source: Rwanda District Health System Strengthening Tool, 2009-2010 All district hospitals have more than one computer facilities in 2010. At health center level the situation improved dramatically during 2010 as only 5% of health centers had no computer facilities (down from 17% in 2009) and 86% had more than one computer (up from 69% in 2009). Table 8: Availability of computers in district hospitals and health centers Health Centers 2009 2010 Hospitals 2009 2010 Availability of functioning computers no computers 71 17% 22 5% 0 0% 0 0% 1 computer 60 14% 9% 1 2% 0 0% >1 computer 290 N 421 100% 425 100% 41 100% 41 100% 37 69% 366 86% 40 98% 41 100% Source: Rwanda District Health System Strengthening Tool, 2009 & 2010 The table bellow shows the number of beds by health facilities’ types. Overall, bed/inhabitants ratio is 1bed for 587, 9259 inhabitants in 2010 compared to 1bed for 585,7581 inhabitants in 2009 Table 9: Number of inpatient beds by health facility type Facility types District Hospital 2009 6,602 2010 6,664 Health Center 9,283 9,585 949 959 16,834 17,208 Referral Hospitals Total Source: DHSST and reports from Referral Hospitals The percentage of district hospitals with ambulance services didn’t change in 2009 to 2010. At the health center level the proportion of facilities with ambulances increase from 15% to 16%. This is likely to be due to the transfer of some vehicles to district hospitals as part of the rationalization of the SAMU ambulance network. The Rwanda District Health System Strengthening Framework further indicates that all District Hospitals and 90% of Health Facilities have access to at least one form of transportation, including 4x4 vehicles, cars, motos or pickup. Table 10: Vehicle access at district hospitals and health centres Vehicle type District hospitals 2009 (N=41) Health Centers 2009 (N=421) 2010 (N=41) 2010 (N=425) Ambulance 39 95% 39 95% 64 15% 66 16% Any type 41 100% 41 100% 379 90% 323 76% 15 Rwanda Ministry of Health Annual Statistical Booklet 2010 Source: Rwanda District Health System Strengthening Tool, 2009 and 2010 According to the DHSST, 90% of hospitals and 95% of health centers have a microscope and 83% of hospitals and 88% of health centers have a refrigerator, 90% of hospitals and 97% of health centers have an autoclave and 65% of health centers have an incinerator. Table 11: Facilities with selected fully functional equipment Binocular Microscope Refrigerator District Hospital 2009 (N=41) 2010 (N=41) 35 85% 37 90% Health Center 2009 (N=421) 2010 (N=425) 361 86% 405 95% 35 85% 34 83% 362 86% 372 88% X-Ray 34 83% 37 90% n/a n/a% n/a n/a% Autoclave 38 93% 37 90% 300 71% 412 97% Anesthesia machine 38 93% 37 90% 6 1% 0 0% Incinerator 37 90% 34 83% 323 77% 275 65% Source: Rwanda District Health System Strengthening Tool, 2009 and 2010 Human Resources In 2010 there were 604 doctors and 8202 nurses/midwives working in Rwanda. Based on 2010 data from the iHRIS, this corresponds to a ratio of 1 doctor per 17,240 inhabitants, 1 midwife per 66,749 inhabitants and 1 nurse per 1,294 inhabitants. This situation has improved since 2009 when the worst off district had nearly 1,405 inhabitants per nurse. The greatest increases were in the categories of Administrative staff (largely attributable to the inclusion of Mutuelle staff, data managers and cashier in this category during 2010) and midwives whose numbers more than doubled between 2009 and 2010. The only category that saw a reduction was that of paramedical and pharmacist a worrisome trend that could be due to the promise of more lucrative careers in private sector. Table 12: Ratio of health workers to population Staff Category 2009 2010 Doctors Nurses Midwives Paramedical Pharmacist Laboratory Technician Administrative and support Staff 579 7200 49 1355 111 931 604 8046 156 1102 72 1144 17,240 1,294 66,749 9,449 144,623 9,102 4.3% 11.8% 218% -17% -35% 22.9% 3565 3738 2785 5% Population/HW % change 2010: Source: Rwanda District Health System Strengthening Tool, Ministry of health: Human resources database 2010 16 Rwanda Ministry of Health Annual Statistical Booklet 2010 Morbidity and Mortality Morbidity data for this booklet is from the HMIS with a health facility reporting rate of 93.5%. It does not include records from National Referral Hospitals or private facilities. Outpatient care In 2010 the total number of new cases seen at HCs and DHs was 9,028,140 of which 8,437,850 (93.4%) were seen in HCs, 590,290 (6.6%) at DHs and 214,512 at referral hospitals. During 2010, the primary curative care utilization rate was approximately 0.81 visits per inhabitant (8,437,850visits/10,412,820 population excluding community based integrated management of child hood illnesses (C-IMCI) by CHW’s) almost the same as in 2009. Table 13: Number of outpatient visits in Health Centers and District Hospitals Health Service level 2009 2010 7,996,598 8,437,850 5.5% District Hospitals 544,284 590,290 8% CHW Home Based care 744123 914,011 22.8% Referral Hospitals 214,512 197,278 -8% 9,481,389 10,139,429 6.9% Health Centers Total % change Source: National HMIS database 2010, CHW Health Information System 2010, 17 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 4: Map of Outpatient utilization rate, Rwanda, 2010 The high OPD utilization rate may be due to the increased availability of ambulances and mutual membership. It is also important to note the contribution of community health workers in the provision of community based care since the introduction of community integrated management of childhood infections (IMCI). The number of OPD seen by CHWs has increased about 23%. The proportion of reportage is 98% while in 2009, only 66% of the CHW cooperatives reported. The diseases treated are childhood infections including fever/ malaria, acute respiratory infections and diarrhea. District Hospital Outpatient Morbidity The most frequent outpatient services provided by district hospitals were dental and ophtalmogical care. Together they represent almost one third of outpatient visits (35%) up from 20% in 2009. An acute respiratory Infection (ARI) and cardiac disease represents respectively 8% and 4% of the total consultation 18 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 14: Top ten causes of outpatient visits in district hospitals in 2010 Disease Group <5 years 5 years and above Total Cases % of Total Diseases of teeth and gums 5,486 115,931 121,417 21% Eye diseases 7,513 73,860 81,373 14% ARI 16,451 28,486 44,937 8% Cardiological problems 2,008 24,122 26,130 4% - 24,456 24,456 4% 1,413 15,801 17,214 3% 782 15,586 16,368 3% Malaria 4,955 10,432 15,387 3% Skin diseases 2,493 12,310 14,803 3% 78 13,824 13,902 3% All other diagnoses 25,384 162,863 188,247 34% Total 66,563 497,671 564,234 100% Gastro-intestinal disorders Physical trauma Urinary tract diseases Gyneco & obstetric diseases Source: National HMIS database 2010 Figure 5: Causes of Outpatient visits in district hospitals (updated) Top ten causes of consultion in districts hospital in 2010 All other diagnoses Gyneco & obstetric diseases Skin diseases Malaria Urinary tract diseases Physical trauma Gastro-intestinal disorders Cardiological problems ARI Eye diseases Diseases of teeth and gums 0 40,000 80,000 120,000 160,000 200,000 Source: National HMIS database 2010 Health Centre Outpatient Morbidity The picture is quite different in the health centers, where infectious diseases are the primary cause of outpatient morbidity: ARI, intestinal parasites and malaria account for well over half of the outpatient morbidity (56%). There was very little change in the distribution of morbidity at the Health Centers level since 2009, where malaria cases represented 16% of outpatient’s consultation versus 8% in 2010 19 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 15: Top 10 causes of morbidity in health centers in 2010 Disease Group ARI Under5 Over5years 1,027,131 Total cases 2,227,647 3,254,778 % of Total 39% Intestinal parasites 161,698 608,396 770,094 9% Malaria 148,022 505,131 653,153 8% Diseases of bones and joints 1,903 562,770 564,673 7% Gastro-intestinal disorders 1,595 438,993 440,588 5% Diseases of teeth and gums 37,483 292,605 330,088 4% 101,001 312,542 413,543 5% 30,584 349,563 380,147 5% 175,992 181,585 357,577 4% Eye diseases 58,481 149,884 208,365 2% All other diagnoses 75,519 989,325 1,064,844 Skin diseases Physical trauma Diarrhea Total 1,819,409 6,618,441 8,437,850 13% 100% Source: National HMIS database 2010 Figure 6: Distribution of outpatient morbidity in health centers Source: National HMIS database 2010 20 Rwanda Ministry of Health Annual Statistical Booklet 2010 Hospitalization and Mortality Admissions and mortality in health centers and district hospitals Data on mortality in this report comes exclusively from health facility reports in the HMIS. They do not include deaths in the community that were not registered at a health facility. As a result, the mortality figures are likely to underestimate the true level of mortality in the country. The total number of admissions in Health Centers and District Hospitals increased by 9% from 419,117in 2009 up to 456,341 in 2010. Sixteen percent (16.5%) of all admission in 2010 were children under 5 years of age and roughly two-thirds (73%) were female. Total deaths among patients admitted in DHs, HCs were 5,171 in 2010, down from 5,022 in 2009. The proportion of death to total death is high for male (54%) than female (46%). Excluding data from referral hospitals for which total number of admissions are not reported, this results in a health facility death rate of 1.6%, down from 1.7% in 2009. The number of death decreased in health centers by 8% from 369 in 2009 to 341 in 2010, this can be attributed to availability of ambulances that have facilitated in referrals of complicated cases to district hospitals. This is, of course, an underestimate of overall mortality rates because it does not include deaths in the community, in referral hospitals or in the private sector. Table 16: Number of admissions in health facilities by gender >=5 years 2009 % <5 years Total >=5 years Total 2010 % Gender <5 years Females 250,585 292,583 70% 34,584 297,636 332,220 73% Males 41,998 47,927 78,607 126,534 30% 40,877 83,244 124,121 27% Total 89,925 329,192 419,117 100% 75,461 380,880 456,341 100% Source: National HMIS database 2009-2010 Table 17: Number of deaths reported in health facilities Deaths 2009 2010 % of change 416 341 -2% District Hospitals 4552 5206 14% Referral Hospitals 2,147 2,055 -4% Total 7,115 7,602 7% Health Centers Source: National HMIS database 2009-2010 21 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure8: Number of deaths reported in health facilities by gender, 2010 Source: National HMIS database 2009-2010 Leading causes of mortality in health facilities The leading cause of death in district hospitals was malaria, accounting for 13% of total deaths in 2010 as compared to 22% in 2009. The other major causes of deaths are HIV & opportunist infections (9%), ARI (9%), Cardiac diseases (5%) and premature birth (5%). Table 18: Top ten causes of deaths in district hospitals and Health Centers Row Labels Malaria ARI HIV & IOS Premature birth Cardiac diseases Tuberculosis Malnutrition Diarrhea diseases Malignant tumors Physical injuries Others 2010 Total 5547 707 589 506 441 412 223 192 188 139 125 2025 % 13% 11% 9% 8% 7% 4% 3% 3% 3% 2% 37% 100% Source: National HMIS database 2010 22 Rwanda Ministry of Health Annual Statistical Booklet 2010 Under five morbidity and mortality During 2010, 1811 under five deaths were reported both from health centres and district hospitals. This represent one third of total death. In 2010, 95 % of the under five deaths in health facilities were in district hospitals. Neonatal and < 1 mortality death contributes for 70 % to the under five mortality, of which 49 % is among neonates. Prematurity was reported among 49 % of the neonatal deaths. Among the 896 neonatal deaths reported in 2010 in health facilities, 571 (64 % died with the 6 days). It appears that neonatal deaths are mainly linked to poor delivery. Causes of neonatal deaths are being investigated through the initiation of child death autopsy in health facilities. . The main causes of under five deaths in heath facilities are prematurity (23.4 %), respiratory tract infections (15.5 %), Malaria (10.5 %) , malnutrition (6.9%) and diarrhea (4.8 %). Disease specific case fatality rates are the highest in prematurity (19.4 %), congenital abnormalities (13.2 %), AIDS /OI (8 %) and Malnutrition (5.6%). Table 19: Top 10 causes of inpatient hospitalization in district hospitals and health centers among the under five in 2010 Diseases Number of Cases % to total cases Number of deaths % to total death Case fatality rate Respiratory tract infections 26,535 35% 292 16% 1.1% Diarrhea 17,319 23% 90 5% 0.5% Paludisme 9,745 13% 198 11% 2.0% Malnutrition 2,327 3% 130 7% 5.6% Prematurity 2,279 3% 441 24% 19.4% Physical Trauma 1,576 2% 9 0% 0.6% Skin diseases 523 1% 13 1% 2.5% Gastro-duodenal diseases 359 0% 10 1% 2.8% Congenital abnormalities 333 0% 44 2% 13.2% Other 14465 21% 584 32% 4.1% Total cases 2010 75461 101% 1811 100% 2.4% 23 Rwanda Ministry of Health Annual Statistical Booklet 2010 MATERNAL AND CHILD HEALTH Family Planning Figure 7: Trend of family planning coverage among married women, 1990-2007 Family Planning coverage among married women 27 13 10 4 1990 2000 2005 2007 Source (Demographic and Health surveys) Routine family planning data are reported from both health centers and district hospitals. At the end of 2010, a total number of 708,265 women of reproductive age were reported as continuing users of contraceptive methods in health centers and districts hospitals (up 31% from 541,483 in 2009). Couple years of protection, family planning indicator based on the distribution of contraceptive commodities, also increased by 36%, from 773,672 to 1,045,218 during the same period The calculation assumes, that among the women of reproductive health 49 % are women in union and that 76% of family planning users are women in union. Therefore Family planning coverage for women in union is 44.7%. The most used method is Depo provera (66%) and Pills (18.5%). Surgical methods (0.1%) and DIU (1%) are not commonly used probably because they require qualified personnel and training. Table 20: Family Planning Users by method and units distributed Method Implant Continuing users at end of Dec 2010 New Users Units distributed CYP 81,622 191,48 135,365 473,778 Injectable: Depo-Provera 467,955 223,299 1,575,309 393,827 Oral contraceptives (pills) 130,912 72,914 1,395,557 93,038 Natural FP – cycle beads 7,347 3,638 17,509 35,018 IUD 2,862 936 7,093 24,826 Natural FP - selfobservation Barriers 5,179 7,254 0 14,508 11,500 8,525 953,294 7,944 888 285 0 2,280 708,265 335,999 4,084,127 1,045,218 Surgical Contraception Grand Total Source: National HMIS database 2010 24 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 9: Distribution of contraceptive users by method (end 2010) Source: National HMIS database 2010 Ante-Natal Care A total of 321,388 pregnant women registered for Ante-Natal Care (ANC) in 2010. This represents a decrease in ANC coverage rate of 75.3% from 78 % in 2009 (343,164 new registrations). This decrease might be explained by the overestimation of the number of expected pregnancies. Nevertheless, of the women who registered a higher proportion had at least one standard visit (increase from 25% to 30%), and the proportion who had 4 standard visits increased from 14% to 16%. The proportion of high risk pregnancies are almost the same as in 2009 (16%) and 2010 (15%). Table 21: Pregnant women registered for ante-natal care Description New registrations Total 2009 % of new registrations Total 2010 % of new registrations 321,388 323,442 Standard Visit 1st trimester 81,221 25% 96,032 30% Standard Visit 2nd trimester 145,027 45% 134,883 42% Number of women with 4 standard visits 44,555 14% 52,286 16% High-risk pregnancies screened 52,280 16% 47,419 15% % High-risk pregnancies referred 14,827 28.3% 13,445 28.3% Source: National HMIS Database 2009/2010 25 Rwanda Ministry of Health Annual Statistical Booklet 2010 High risk pregnancies referred to the next level of care represent 28% of the total number of high risk pregnancies screened during ANC sessions (almost the same 28% in 2009). This low percentage of referral rate of high risk pregnancies is probably a major contributor to the maternal deaths that occurred in health centers. Assisted deliveries A total of 242,672 assisted deliveries were reported during 2010, of which the vast majority were normal deliveries (86%) and more than two thirds (68%) were in health centers. The maternal health policy promotes delivery in health facilities where the delivery is conducted by a trained health professional in order to reduce any complications that may arise during childbirth. Figure 10: Map of coverage of assisted deliveries in Health Centers If we compare the figure for assisted deliveries in the health centers, district hospitals and referral hospitals to the total number of expected deliveries we can estimate the coverage of assisted deliveries at 56.8% in 2010, a decrease as compared to 61% in 2009. The decrease in assisted deliveries could be attributed to the fact that the number of expected deliveries which is used as denominator to calculate the assisted delivery coverage is overestimated due to the increased use of family planning, resulting in reduction/underestimation of the coverage. Maternal deaths recorded in health centers and district hospitals are almost the same in 2009 and 2010 26 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 22: Location of assisted deliveries 2009 Location of delivery Normal deliveries Dystocic 2010 Total Maternal Deaths Normal deliveries Dystocic Total 1305 165541 Maternal Deaths Health Centers District Hospitals 174207 1,534 175741 45 164236 46,491 26,272 72,763 133 43489 28377 73296 162* +23% Referral Hospitals 2,436 2,868 5,304 38 1960 1875 3835 42 +10% 223,134 30,674 253,808 216 209,685 31,557 242,672 221 -1.8% Total 17 % change in maternal deaths -64% Source: National HMIS database 2009/2010 + KFH, CHUK, CHUB. Maternal deaths occurring in health facilities were 221 out of 242,672 deliveries. This corresponds to a health facility Maternal Death Ratio of 91 deaths per 100,000 in health centers and district hospitals. This is well below the 20072008 RIDHS figure of 690/100,000, but the two figures are not comparable because of the methods of collection used and the fact that the RIDHS also includes maternal deaths and unassisted deliveries in the community. Among all deliveries, the main maternal complications in 2010 are per anal tear (0.43%), Bleeding (0.28%), Infections (0.27%). Table 23: Causes of maternal death, 2010 Causes of death Number maternal death % 75 18 27 14 7 12 10 13 11 33.9% 8.14% 12.21% 6.33% 3.16% 5.42% 4.52% 5.88% 4.97% IO/HIV 9 Amniotic embolism 10 Heart failure 7 Pulmonary embolism 3 Anemia in pregnancy 5 Total 221 Sources: Maternal death audit, MCH/MOH, 2010 4.07% 4.52% 3.16% 1.35% 2.26% 100% Severe bleeding Malaria Septicemia Eclampsia Other infections Unknown causes Obstructive labor Other causes Anesthesia complications 27 Rwanda Ministry of Health Annual Statistical Booklet 2010 Cesarean sections at Hospitals Cesarean section rate slightly increased by 6.7% from 34% in 2009 up to 36.3% in 2010. Overall, the high rate of caesarian section may be partly due to the increased availability of ambulances and better referral of high risk pregnancies. Table 24: Caesarian sections in District Hospitals and Referral Hospital 2009 Health Facility Type #deliveries #dystocic deliveries 2010 #cesarean section cesarean % of total delivery #deliveries #dystocic deliveries #cesarean section cesarean % of total delivery District Hospital 72,763 26,272 24,189 34% 73296 28377 26330 35.90% Referral Hospital 5,304 2,868 1,814 34% 3,835 1,875 1,701 44.30% TOTAL 78,067 29,140 26,372 34% 77,131 30,252 28031 36.30% Source: National HMIS database 2009, 2010, Reports from Referral hospitals Weight at birth and deaths of newborns In 2010, all public and FBO (agree) health facilities reported 241,277deliveries registered in their records. These records indicate that 14,621 newborns, or 6.0% of all recorded births for the year, had a weight less than the acceptable birth rate of 2.5 Kg. Low birth weight is a risk factor for death in infancy. As one would expect with effective referral of high risk pregnancies, the percentage of low birth weight deliveries is substantially higher at district hospitals. Table 25: Birth and perinatal death in health centers and district hospitals Facility Type Health Centers District Hospitals Total 2009 Total births Total deaths Births < 2.5 kg % low BW 2010 Total births Total deaths Births < 2.5 kg % low BW 176331 1410 5642 3.2% 166151 1246 5339 3.2% 73383 3098 11963 16.3% 75126 3345 9233 12.3% 249714 4508 17,605 7.0% 241277 4591 14572 6.0% Source: National HMIS database 2009-2010, data unavailable from referral hospitals Health facilities reported that among 241,277 births registered in Health Centers and District Hosptials during 2010, 4591died in-utero or within hours of birth, representing a proportional mortality of 1.9%, almost the same in 2009 1.8%. 28 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 8: Infant death ratio by level of health care facility as reported in 2009 and 2010 Perninatal mortality rate 2009-2010 5.0% 4.2% 4.5% 4.5% Mortality rate (%) 4.0% 3.5% 3.0% 2.5% 2009 1.8% 1.9% 2.0% 2010 1.5% 1.0% 0.8% 0.7% 0.5% 0.0% Health Centers District Hospitals Average Facility types Source: National HMIS database 2009, 2010. Number of infant deaths (intrauterine+newborns)/total deliveries Child immunizations Based upon routinely reported data from health facilities, immunization coverage decreased for all antigens since 2009, at least a decrease of 10%. This is most probably due to the overestimation of the denominator (children <1), as explained above real coverage rates will be determined by a population survey (DHS 2010). This is illustrated by a mini-survey (277.535 number of households) held in November 2010 in the Northern Province. The proportion of children < 1 was 2.5 % (contrary to the 4.1 % used by HMIS) and the coverage rate of fully vaccinated children was 92 %. Table 26: Childhood vaccination and ITN distribution Indicator Polio O 2009 Number % coverage 291,069 72% 2010 Number % coverage 253,199 61.0% BCG 324,557 80.3% 289,242 69.7% Polio 1-DTP-HepB/Hib1 322,231 79.8% 288,612 69.6% Polio 2-DTP-HepB/Hib2 322,229 79.8% 288,039 69.4% Polio 3-DTP-HepB/Hib3 321,803 79.6% 290,591 70.1% Measles 345,459 85.5% 297,819 71.8% 29 Rwanda Ministry of Health Annual Statistical Booklet 247,589 Children who received Insecticide Treated Nets 2010 163,963 61% 39.5% Source: National HMIS database 2009-2010 Growth Monitoring Children were monitored for nutrition status passed from 2.7 million times in 2009 to around 2.3 million in 2010. This does not represent the number of children weighed because each child is supposed to be monitored monthly, however it does suggest that an average of 193,000 children are monitored each month at health centers. When combined with the CHW growth monitoring reported below, nearly half a million children are monitored each month. In 2010, for all monitored children 9.1% have malnutrition compared to 10% in 2009 Table 27: Nutrition status of children monitored in health centers 2009 Age 0-11 months 827,268 50,637 10,324 426 % malnourished 6.86% 12-23 months 606,693 65,822 16,605 1,404 24-35 months 530,149 51,154 13,350 36-59 months 455,294 53,265 2,419,404 220,878 Total Green Yellow Red 2010 Oedema Green Yellow Red Oedema % malnourished 714410 30628 7157 154 5% 11.96% 513213 54235 12037 816 11.4% 1,817 10.85% 455063 43663 9666 1176 10.5% 14,389 2,477 12.94% 420673 42024 10558 1500 11.1% 54,668 6,124 10.22% 2103359 170550 39418 3646 9.1% Source: National HMIS database 2009-2010 Malnutrition Hospitalization for Childhood Malnutrition 2,136 people were hospitalized for malnutrition in 2010, up from 1,920 in 2009. Deaths of people hospitalized for malnutrition were also down substantially, suggesting more effective case management of malnutrition. Table 28: Hospitalization for childhood malnutrition and health outcomes Registrations Year Level of care 2009 < 5 years >= 5 years Total 2010 < 5 years >= 5 years Total New Cases 1,212 238 1,450 949 209 1158 Old Recovered Cases 437 1,057 33 227 470 1,284 887 1058 91 211 978 1269 Status Referred to Hospital 93 22 115 55 20 75 Lost to follow up 53 12 65 45 14 59 Died 16 3 19 5 0 5 Source: National HMIS database 2009, 2010 Outpatient treatment of Malnutrition 64583 people received outpatient treatment for malnutrition in 2010, down slightly from 75278 in 2009. For all discharged patients 83 % of recovered as compared to 80% in 2009. Deaths of patients treated for malnutrition as outpatients were also down slightly, especially in the over 5 year age group. These figures reveal a worrying statistic: nearly 9% of children who registered for care were lost to follow up. 30 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 29: Outpatient treatment of malnutrition and health outcomes Registrations Year Status Level of care New Cases Old Recovered Cases 2009 < 5 years 35796 28840 26578 563 7272 3370 6787 135 675 19 43068 32210 33365 698 6688 243 30945 24079 26645 362 5009 139 6644 2915 5224 92 644 27 37589 26994 31869 454 5653 166 >=5 years Total 2010 < 5 years >=5 years Total Referred to Hospital Lost to Died follow up 6013 224 Source: National HMIS database 2009-2010 Community Health Worker Program; Community IMCI: During 2010, Over 743,589children were treated by CHWs comparing to 462, 104 in 2009.The innovative Community Health Worker program began to produce useful data for the first time in 2009 with the roll-out of the Community Health Worker Information System (SISCom). A major focus of CHWs has been on community integrated management of childhood infections (IMCI). Three major ailments: fever, pneumonia and diarrhea. Over two third children treated presented with fever symptoms (77%), cough/cold symptoms were next with 12%. Figure 9: Children treated by CHWs as part of Community IMCI Source: SISCom 2010 31 Rwanda Ministry of Health Annual Statistical Booklet 2010 The SISCom data also suggest that outcomes of CHW IMCI treatment are generally good. 88% were reported cured, while less than 10% were referred and a very small proportion 0.02% died while under the care of the CHW. The mortality data should be interpreted with caution. Figure 10: Outcomes of Community IMCI Source: SISCom 2010 In addition to providing community IMCI, CHWs are involved in nutrition monitoring using simple middle-upper arm circumference measuring tapes. During 2009, CHWs monitored the nutritional status of children more than 7517261 times (an average 626438 children were monitored each month). For the year, less than 1% of the measurements were in the red zone and another 4% were in the yellow zone. Malnutrition rate is high in the following districts: Rusizi (12.3%), Huye 11.5%, Ngororero 9.9% and Gakenke 9%. The districts with low malnutrition rate are Nyarugenge 1.3%, Gasabo 1.2%, Gisagara 1.1%, Ruhango 1%, Kicukiro 1% and Ngoma 0.7%. 32 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 11: Nutritional status-MUAC by CHWs, 2010 Source: SISCom 2010 Sexual Violence Over four thousand and five hundred cases of sexual violence were reported by district hospitals (4,577) and one-third (33%) of these cases had objective symptoms of sexual violence. Ninety-five percent of the cases investigated were among females (95%). The largest group of victims was females between 5 and 18 years of age (57%). Males represented about 5% of the cases investigated; the percentage is the same as in 2009 (5%). Table 30: Sexual violence by age and gender 2010 Type of case < 5 years 5 - 18 years >18 years Total F M F M F M 297 28 869 35 272 7 1508 Number of cases with symptoms of sexual violence Number of cases received at the 831 hospital suspected of sexual violence 92 2602 103 901 48 4577 % change from 2009 18% 22% Source: National HMIS database 2009-2010 33 Rwanda Ministry of Health Annual Statistical Booklet 2010 TB and HIV/AIDS Tuberculosis (TB) In 2010, 7065 TB patients were registered; 6434 (91%) new cases, 442(6.3%) retreatment cases and 139(2, 7%) other cases. The notification rate of all TB cases was 70/100,000 inhabitants and it was 41.4/100,000 inhabitants for the new smear-positive pulmonary cases. Over ninety percent (97.9%) of all TB patients registered in 2010 were tested for HIV. The seroprevalence of HIV was 31.8% among TB patients, ranging from 23% among new smear-positive and 42% among all other cases. About all cases (97.2%) co infected with TB-HIV received Cotrimoxazole-preventive treatment (CPT). The community based DOTS covers 30 out of 30 districts. Table 31: CHWs Participation in Community DOTS 2007 to 2010 Year # of districts Population covered Suspected cases Number of positive suspects Detected by Total Detected by CHW CHW Total % of suspected cases detected by CHW % suspected positive detected by CHW 2009 24 9860652 52,235 5,840 2,275 365 11.2% 13.2% 2010 30 10117029 70325 6850 4049 396 10% 9.7% Source: TRAC Plus/ TB Unit Report 2008-2010 The participation of CHWs is most significant in relation to the administration of treatment: 48.1% of patients registered in 2010 in the districts concerned have received DOTS from CHWs. 10% of all suspected cases were sensitized by CHWs and 9.7% of all confirmed cases were referred to health facilities by CHWs. In 2010 the success rate of treatment by CHWs (97%) and overall treatment success rate (84.8%). Table 32: Success rate of Sputum Smear + for Tuberculosis enrolled in 2009 Success rate of Sputum Smear + Total under Cured Completed treatment treatment 3,140 (78.7%) 4096 335 (8.2%) Overall Success rate of patients Success rate followed by CHW 84.8% 97% Source: TB program annual report 2010 Table 33: HIV testing of Tuberculosis + Patients HIV testing TB patients tested Total TB patients Tested 7065 6914 (97.9%) Number of HIV positive 2198(31.8%) Number of HIV positive under CMX 2,137 (97.2%) Source: TB program annual report 2010 HIV /AIDS VCT During 2010, a total of 1,862,642 people were tested through voluntary counseling and testing services (up from 1,393,018 in 2009) and 1,641,752 (88%) knew their test results. Each year, the average number of people tested voluntary in all health facilities was increased of 25%. The number of VCT sites increased from 403 to 434. (TRAC 34 Rwanda Ministry of Health Annual Statistical Booklet 2010 Plus/ HAS Unit 2009 & 2010 Annual Reports). The pie chart below describes the distribution of tests by gender, 54 % of those tested were female. Figure 12: Distribution of people tested for HIV/AIDS by sex 46% 54% male female Source: TRACPlus/HAS Unit 2010 Annual Report In 2010, about half of those tested were in the age group over 25 years (44.7%). The seroprevalence of HIV is high among people aged above 25 years (3.1% down from 3.6% in 2009). In the age group below 18, the seroprevalence was estimated at 0.7% (down from 0.9% in 2009); in the age group between 18 and 25 years, the seroprevalence was estimated at 1.7% (down from 1.9% in 2009). The chart below shows the percentage of people tested and the percentage of people with HIV Positive by age group. 35 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 13: Age distribution and seroprevalence of clients tested for HIV in health facilities, Rwanda 2010 50 44.8 45 percentage (%) 40 35 30.7 30 24.5 20 % clients tested HIV positive 15 % client tested 25 10 5 3.1 0.7 1.7 0 < 18 years 18-25 years Age >25 years Source: RBC/TRACPlus/HAS Unit 2010 Annual Report. PIT In Rwanda, Provider initiated testing (PIT) was rolled out in all health facilities in 30 December 2010, health facilities have already started to provide PIT services and 187258 patients have been counselled and 5339 (2.8%) tested HIV positive. Preventing Mother to Child Transmission (PMTCT) With regard to Prevention of Mother to Child Transmission of HIV/AIDS (PMTCT), the number of women who were receiving Ante-Natal-Care services in PMTCT settings is 307, 904. Among them 297145 (96.5 %) accepted to be tested for HIV and 99% of the women tested returned for information about their HIV serological status. Among 297145 women tested for HIV in ANC services during the year 2010, 8343 were HIV positive (2.8% of HIV seroprevalence in pregnant women in PMTCT). 36 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 14: Voluntary Counseling and Testing during ante-natal clinics 8343 2010 294289 307904 8704 2009 296230 303113 8806 2008 296286 305995 0 Number of women who were tested HIV Positive Number of women who accepted to be tested for HIV and received their results Number of women who were received in ANC 50000 100000 150000 200000 250000 300000 350000 Source: RBC/ TRACPlus/HAS Unit 2008/2009/2010 Annual Reports. Rwanda has also started to implement the new WHO recommendations of provision of ARV triple therapy to the HIV-infected pregnant women starting at 14 weeks of pregnancy. The launching was done on 15th November 2010. In total, 8072 HIV-infected pregnant women received ARV prophylaxis and triple therapy prophylaxis constituted. HIV-infected pregnant women were estimated to 10,310, 78% of them received ART prophylaxis. From January to December 2010, 250142 (84%) of partners of pregnant women have been tested and 6125 of them tested HIV positive (2.4% of HIV seropositivity). The number increased along the years. Figure 15: Percent of Partner tested from 2003 to 2010 90% 84% 85% 80% 78% 70% 66% 60% 53% 50% 40% 33% 30% 20% % of Partners of pregnant women tested 26% 16% 10% 0% 2003 2004 2005 2006 2007 2008 2009 2010 Source: RBC/ TRACPlus/HAS Unit 2008/2009/2010 Annual Reports. 37 Rwanda Ministry of Health Annual Statistical Booklet 2010 HIV exposed infants follow up Among children expected to receive ARV prophylaxis, 7610 (74%) received it and 7368 started cotrimoxazole at 6 weeks of age. The DNA PCR test was also performed for 7220 exposed infants in their first 2 months of life. Care and treatment The number of patients on ARVs increased from 76726 patients (end 2009) to 89,660 patients by the end of December 2010. The number of HIV infected children on ARVs, increased from 6676 children (end 2009) to 7,479children by the end of December 2009. Health facilities offering ARVs also increased dramatically from 269 to 337 throughout the country. Table 34: Anti-Retroviral Therapy in Rwanda from 2007 to 2010 2007 2008 2009 2010 % change (2009-2010) Patients on ART 48,069 63,149 76,726 89,660 16.8% Children on ART 4,350 5,635 6,676 7,479 12% 171 195 269 337 25% Health facilities providing ART Source: RBC/ TRACPlus/HAS Unit 2008/2010 Annual Reports. The analysis of gender differences of patients on ART treatment show that women represent almost two-thirds of the adult patients (62%), while male and female children are equally represented in the patient population. HIV among Groups at high risk. Youth The 2009 Youth Behavior Surveillance Survey (BSS) in Rwanda carried out in September and October 2009, provided information on male circumcision in youth Figure 16: Circumcision Pattern of Youth Males in the 2009 Rwanda Youth BSS (N = 2,522) Source: RBC/ TRACPlus/HAS Unit 2008/2009/2010 Annual Reports. 38 Rwanda Ministry of Health Annual Statistical Booklet 2010 The 2009 BSS collected information on self-reported circumcision prevalence among male respondents including age at circumcision, type of practitioner who performed the circumcision, reason for not being circumcised and future desire to be circumcised. Circumcised males were also asked the main reason for their circumcision. Tables 10a and 10b display the various results. Overall, only 16% of males aged 15-24 reported having been circumcised. This rate varied by age group, with the 20-24 year old group reporting lower frequency of circumcision (6%). Overall, 93% of those who were circumcised reported having had circumcision performed by a health professional. Overall 61% of circumcised males reported that health and hygiene were the major reasons for undertaking the procedure, while only 17% cited HIV prevention as the primary reason. Youth Sexual behavior trends analysis Figure 17: Comparison of Youth Sexual Behaviors between 2006 and 2009 BSS, Rwanda Source: RBC/ TRACPlus/HAS Unit 2008/2009/2010 Annual Reports. In 2009, the percentage of females who ever had sex was 26% compared to 20% in 2006 (p-value = 0.001). For the males, the increase between 2006 and 2009 was significant but less pronounced (39% vs 34%, p-value = 0.01). Similarly, 35% of the youth reported having sex in the 12 months prior to the 2009 survey, an increase compared to the 2006 survey which reported 26% of youth (p-value < 0.010). However, a gender difference is noticeable. While, in 2009, only 6% more males had sex in the 12 months preceding the 37 survey as compared to 2006, this difference increases to 10% for the females between the two years (or surveys, or survey years). Overall, 28% used condom at first sex in 2009 against 21% in 2006 (p-value < 0.01). In 2009, 51% of the youth used condom at last sex against 39% in 2006 (p-value < 0.0001). This percentage varied among gender as shown in the figure 22 above. For example in 2006 the percentage of females who reported having used condom at last sex was 23% against 45% in 2009 (p-value < 0.0001). For the males, the percentage of those who reported having used condom at last sex was 49% in 2006 vs 59% in 2009 (p-value < 0.001). 39 Rwanda Ministry of Health Annual Statistical Booklet 2010 Youth Comprehensive knowledge of HIV. Figure 18: Youth Comprehensive Knowledge of HIV/AIDS, Rwanda Comparison between 2006 and 2009 Source: RBC/ TRACPlus/HAS Unit 2008/2009/2010 Annual Reports. Two types of trends can be seen in figure 23. In one hand, the percentage of youth who, in 2009, said that “Proper Condom Use” can protect against HIV was 84% against 72% in 2006 (p-value < 0.001). Similar change was also observed in the percentage of those who said “Abstinence” can protect against HIV/AIDS. On the other hand, the percentage of youth who said that “Being faithful to one, uninfected partner can protect against HIV/AIDS” drop from 61% in 2006 to 29% in 2009. Preliminary informal inquiries show that this big decline may be explained by the fact that most prevention programs focus mostly on “Abstinence and Proper Condom Use”. This leads in 2009 to sizeable drop in the percentage of youth who had a “Comprehensive Knowledge” of HIV as compared to 2006 from 19% to 11%. “Comprehensive knowledge” is defined as knowing simultaneously that proper use of a condom, having one faithful partner and abstinence can protect against HIV/AIDS and recognizing that a person apparently in good health can transmit HIV/AIDS at the same time rejecting the two most common misconceptions about HIV/AIDS transmission. 40 Rwanda Ministry of Health Annual Statistical Booklet 2010 Female sex workers Condom use Table 35: Number and percentage of respondents reporting using a condom at the last sexual intercourse by type of partner, age, province and sites, (N=1,136) Did not use condom (N=225) Total Characteristics Age group Use condom With non paying sexual partner only (N=42) With paying partner only (N=856) With both paying and non paying partner Number n % n % n % n % 157 469 342 288 25 67 50 62 16 14 15 22 3 12 14 11 2 2 4 4 105 317 221 173 67 68 65 60 24 73 57 42 15 16 17 15 80 21 26 2 3 40 50 17 21 East Kigali city North West South 266 264 266 274 266 63 24 49 42 47 24 9 18 15 18 5 3 13 13 8 2 1 5 5 3 158 194 160 176 168 59 74 60 64 63 40 43 44 43 43 15 16 17 16 16 Road/public place 1065 114 179 11 17 10 31 5 3 4 688 78 65 68 167 20 16 18 157 35 22 6 4 90 57 26 17 86 317 271 238 271 1336 12 40 49 39 63 225 14 13 18 16 23 17 1 11 6 8 12 42 1 3 2 3 4 3 67 205 179 153 152 856 78 65 66 64 56 64 6 61 37 38 44 213 7 19 14 16 16 16 15-19 20-24 25-29 30-39 40 + Province Site Hotel/Nightclub/other Cabaret/Bar/Restaurant Years of experience <1 1-2 3-4 5-7 8+ Overall On the whole, the vast majority of FCSW (83%) reported using a condom during their last sexual intercourse. Among those FCSW reporting having used a condom, 3% reported using a condom with non paying partners, 64%reported using a condom with a paying partner. This proportion varied by age group, province, site and years of experience. For instance, 91% of the FCSW working in Kigali reported having used condom at last sex compared to 74% of those working in the East Province (p-value <.0001). 41 Rwanda Ministry of Health Annual Statistical Booklet 2010 HIV Prevalence by Background Characteristics Table 36: HIV prevalence of FCSW by background characteristics, 2010 Rwanda BSS. Characteristics N n HIV Prevalence (%) 15 - 19 110 39 35 20 – 24 382 168 44 25 – 29 297 157 53 30 – 39 253 157 62 40 + 70 44 63 East 123 40 33 Kigali city 233 131 56 North 260 122 47 West 251 137 55 South 245 135 55 Road/public place 932 487 52 Hotel/Night-club/Other 90 36 40 Cabaret/Bar/Restaurant Level of education None 90 42 47 Age group Province Site 321 164 51 Primary 652 336 52 Vocational 17 9 53 Secondary 122 56 46 Yes 308 145 47 No 804 420 52 9 3 33 30 11 37 266 156 59 807 395 49 <1 58 20 34 2-3 4-5 6-7 8+ 250 127 51 227 111 49 207 104 50 235 1112 135 565 57 51 Additional occupation Current marital status Married and staying with a husband Separated but cohabitating with another sexual partner Separated but not cohabitating with a sexual partner Never married nor not cohabitating with a sexual partner Years of experience as CSW* Overall Overall, 565 (51%) FCSW tested HIV positive. HIV prevalence varied by age group, province, marital status, other source of income, and years of experience. For instance, HIV prevalence increased with age, from 35% among those aged between 15 and 19 years to 63% among those aged 40 years and above. 42 Rwanda Ministry of Health Annual Statistical Booklet 2010 Likewise, HIV prevalence increased with years of experience as FCSW from 34% among FCSW with less than one year of experience as FCSW to 57% among FCSW with eight or more years of experience as FCSW. Similarly, there was a regional variation in the HIV prevalence with 33% HIV positive among FCSW in the East Province compared to 56% HIV positive among FCSW in Kigali City. HIV prevalence was lower (47%) among FCSW having an additional occupation/source of income compared to 52% among those who did not have an additional occupation/source of income. HIV prevalence was significantly lower among FCSW married and living with their husband (33%) compared to those never married nor not cohabiting with a sexual partner (49%) and those separated but not cohabitating with a sexual partner (59%). HIV comprehensive knowledge Percentage Figure 19: HIV knowledge comparison between 2006 and 2010 FCSW BSS, Rwanda 100 90 80 70 60 50 40 30 20 10 0 85 89 90 95 86 86 92 95 74 69 36 46 18 22 Abstinence Being Faithfull Proper use of Reject mosquito Reject sharing A health looking Comprehensive to one partner condom bite meal with an person can knowledge infected person have HIV/AIDS HIV Knowledge 2006 2009 Source: RBC/ TRACPlus/HAS Unit 2008/2009/2010 Annual Reports. Two types of trends can be seen in Figure 3. On one hand, the proportion of FCSW who correctly rejected that mosquito bites can transmit HIV dropped to 69% compared to 74% in 2006 (p-value <0.0001). On the other hand all the other positive attitude indicators remained the same or increased resulting in an overall increase in comprehensive knowledge from 18% in 2006 to 22% in 2010. MALARIA. Malaria continues to be the top cause of death among patients at district hospitals (654 deaths reported in 2010), the number 8th cause of outpatient morbidity. Malaria death represents 13% of total death in 2010. The malaria mortality rate at district hospitals was 19.2%, during 2010, up from 16.3% in 2009. During the end of 2010 there was a surprising upsurge of malaria cases: During 2010, 655697 cases of malaria were reported, compared to 703,562 in 2008 (a decrease of over 7%). 43 Rwanda Ministry of Health Annual Statistical Booklet 2010 Table 37: Distribution of Malaria diagnoses by health facility type Facility type Health Center District Hospital Malaria diagnosis Simple malaria (confirmed) Severe malaria Grand Total Source: National HMIS database 2009-2010 2009 691,110 2010 645555 12452 10142 703562 655697 Figure 20: Graph of proportional morbidity for Malaria 2009-2010 in health centers Malaria propotional morbidity rate (%) 25.0% 20.0% 15.0% 10.0% 22.1% 19.9% 19.8% 16.7% 15.7% 15.2% 14.8% 14.4% 14.4% 13.5% 12.7% 11.5% 17.3% 12.4% 11.6% 9.9% 9.2% 8.5% 5.5% 5.2% 3.7%4.2% 2.9%2.8% 5.0% 0.0% 01 02 03 04 05 06 07 08 09 10 11 12 01 02 03 04 05 06 07 08 09 10 11 12 2009 2010 Malaria propotional morbidity rate Source: National HMIS database 2009-2010 The graph of proportional morbidity displays the classic seasonal trend with peaks in June and December. The map below shows the geographic distribution of Malaria by district in 2010. This highlights that fact that the highest number of cases are in the Eastern and Southern regions. 44 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 21: Map of proportional malaria morbidity by District 2010 Source: HMIS database, 2010 Laboratory During 2010, approximately 95% of all reported lab tests were conducted at the health centre level. 38.4%) of the tests completed were thick blood smear, 36.6% blood laboratory exam (there is an increase of 2.21% when compared to the result of 2009, 15.5% were stools, in 2009, 39.87%, thick blood smear were 34.4% of blood and 16% of stools. Table 38: Type of lab Tests conducted at different health facilities Type of Lab Exam Thick blood Smear Stools 2009 Health District Centre Hospitals 4708640 278566 2010 Total Health District Centre Hospitals 4987206 5274334 264380 Total 5538714 1853356 134604 1987960 2113024 129589 2242613 Urine 746154 21239 767393 845568 22606 868174 Sputum 157492 96007 253499 164270 95459 259729 Blood 4215576 94709 4310285 5176155 112799 5288954 Other 157015 44788 201803 183394 41263 224657 11838233 669913 12508146 13756745 666096 14422841 TOTAL Lab tests Source: National HMIS database 2009-2010 45 Rwanda Ministry of Health Annual Statistical Booklet 2010 SURGERY A total of 77,469 surgical interventions were performed during 2010, an increase of 8.5% percent since 2009. Over half of all surgeries were urgent interventions (60.8%). The most common type of surgery reported was Major Surgery (60.07%), Composed of Urgent (65.85%) and planned (34.15%) , While minor surgery were 40% with planned of 58. 8% and urgent of 41.2% Table 39: Type of surgery performed Type of surgery 2009 Planned Urgent 2010 Total Planned Urgent Total % change Major surgery 15,638 27,751 43,389 15890 30643 46,533 7.2% Minor surgery 17,510 10,533 28,043 18192 12744 30,936 10.3% Total surgical 33,148 38,284 71,432 34,082 43,387 77,469 8.5% Source: National HMIS database 2009-2010 Table 40: Selected surgical interventions 2009 Selected surgical Planned Urgent 2010 Total Planned Urgent Total General Surgery: Appendectomy Hernia Laparotomy Thyroidectomy Cataract Adenomectomy Trachoma Glaucoma Others Gyneco-obstetrical surgery: Caesarean section Hysterectomy Ectopic pregnancy Other Laparotomies (G-O) Myomectomy Curettage Orthopedic surgery: Amputations Osteosynthesis Others 101 1,903 364 147 2,272 94 1 222 95 153 543 8 4 - 196 2,056 907 155 2,276 94 1 222 5373 1468 6841 1,625 369 22564 84 24189 453 27 368 175 159 143 255 22 1636 149 687 1602 36 96 1679 106 1899 362 145 2088 83 1 243 5479 73 188 508 1 5 3 1 0 1825 179 2087 870 146 2093 86 2 243 7304 170 623 197 1795 1524 346 24 388 196 183 24806 92 116 272 13 1550 26330 438 140 660 209 1733 185 783 3281 151 643 2029 44 48 2011 195 691 4040 Source: National HMIS database 2009, 2010 46 Rwanda Ministry of Health Annual Statistical Booklet 2010 RADIOLOGY Reports from district hospitals on medical imagery and other diagnostic testing procedures indicate over 113,970 X-rays conducted during 2010 (22% more than in 2009). Overall, 21% more diagnostic testing procedures were undertaken in 2010. There were sharp increases in the number of abdominal radiology exams (176%). Table 41: Medical imagery and other diagnostic testing procedures Exam type 2009 93,422 Total Radiology Exams 2010 % change 22% 113970 Lungs 43,608 50632 16% Bones 44,204 57108 29% Abdomen without preparation 3,302 3569 8% Abdomen with dyes 391 1078 176% Other Radiology 1,917 1583 -17% Gastroscopy 725 858 18% Echography 25,375 29790 17% 958 665 -31% 120,480 145,283 21% ECG Total Exams Source: National HMIS database 2009-2010 PERFORMANCE-BASED FINANCING: Between 2009 and 2010 there was a 9.4% increase in funding for purchase of indicators as part of the performance-based financing initiatives. The amount was split fairly evenly between HIV (47%) and primary care indicators (53%). Table 42: Performance-Based Financing payments by year and PBF package PBF Package 2009 2010 % Change 2009-2010 PMA 2,404,033,343 2,594,998,464 8% VIH 2,030,597,207 2,256,593,237 11% Grand Total 4,434,630,550 4,851,591,700 9% Source: PBF database 2009-2010 47 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 22: Evolution of key Maternal and Child services (Average numbers per facility) Source: PBF database 2009-2010 48 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 23: Evolution of Average Quality scores from Health Center PBF Quality Assessments Source: PBF database 2009-2010 COMMUNITY-BASED HEALTH INSURANCE /MUTUELLE (CBHI) Membership has continued to expand in the community-based health insurance program. Average adhesion rate for the country stood at 91% in 2010. As displayed in the map in Error! Reference source not found., dhesion rates are not evenly distributed across the country, but range from a low of 78% in Ruhango district up to 99% in Karongi, Nyamasheke and Gatsibo districts. 49 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 24: Map of Mutuelle Adhesion Rates by district 2010 Source: CBHI department records The individual membership payment represents 46% of total income. The total Expenditure represents 68% of total income. Table 43: Summary of CBHI income and expenditure Income 2010 Individual membership payments to the mutuelle fund 7,550,768,265 Membership payment on behalf of individual by other organizations (Global Fund, Commercial firms, etc…. 2,870,891,857 Other receipts (copayment, donations, interest, etc….) 5,954,045,397 TOTAL INCOME 16,375,705,519 Expenditure Cost of hospitalization for mutual members, other care OPD, drugs, etc…) for mutual members and payments made to other heath centers for care provided to mutual members 5,877,736,888 Amount transferred to the district pooling risk 4,119,816,273 Running cost for mutual section (salaries, stationary, supervision, Training, etc… 1,162,811,154 TOTAL EXPENSES 11,160,364,315 Profit/Loss 5,215,341,204 % Profit/Loss 31,8% NB: the cost of Drugs, OPD, hospitalizations are combining in the same line 50 Rwanda Ministry of Health Annual Statistical Booklet 2010 Figure 25: Evolution du taux d'adhésion aux mutuelles de santé 2003-2011 Evolution of enrollement rate(%), CBHI,2003-2010 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 2003 2004 2005 2006 2007 2008 2009 2010 Source: Rapport Annuel CTAMS Sources of Data HMIS The main source of data on morbidity and mortality is the Health Management Information System (GESIS). This system has been recently upgraded to capture data from monthly and annual reporting formats that were revised at the end of 2007. Data is recorded in health centres and hospitals on registers and patient forms and is then compiled monthly and transmitted on paper forms to district hospitals. These reports are entered into the HMIS at the district hospitals and transmitted electronically to the HMISUnit at the central level where data are uploaded into the central database. At the time this analysis was produced, 93.5% of expected monthly reports were entered into the system for all district hospitals and health centres in Rwanda. For certain types of analysis, such as coverage rate calculations, adjustments are sometimes made to compensate for under-reporting. It is important to note that the HMIS does not currently include private health facilities, nor does it include data from National Reference Hospitals. Rwanda National Population Projections 2007-2022 Population denominators have been obtained from the National Institute of Statistics Rwanda (NISR), population projections are based upon the 2002 census. TracNet Rwanda’s TRACnet is a dynamic phone and web-based information management solution that collects, stores, retrieves, and disseminates critical program, patient and drug information related to HIV/AIDS care and treatment. Funded through CDC/PEPFAR, the system is developed by Voxiva and supports the Government of Rwanda in the rapid expansion of HIV/AIDS clinical services in hospitals and health centres throughout the country. Under the leadership of the Ministry of Health and the Treatment and Research AIDS Centre (TRAC), TRACnet has increased the efficiency of Rwanda’s HIV and AIDS program management and has enhanced the Government’s capacity to monitor the quality of patient care. Deployment of TRACnet started in late 2004, and as of December 2010, the system has been scaled up to 337 facilities providing care and treatment services to 89,660 ART patients. TRACnet collects HIV/AIDS aggregated data of all health centres providing HIV AIDS services with a satisfactory completeness of 90% and timeliness of 62%. 51 Rwanda Ministry of Health Annual Statistical Booklet 2010 PBF Performance-based financing (PBF) uses a web-based database to collect a very selected number of mostly output indicators that are used to track progress and calculate performance based payments for community health worker cooperatives, health centres and district hospital. The system also uses data from quarterly quality evaluations to ensure that data and service quality are maintained, and to reduce the performance payment accordingly. The system is in the process of being expanded to integrate community-based services (Community PBF). PBF data is cited occasionally for comparison purposes because the reporting rate is virtually 100% and the data are carefully validated each quarter. CBHI indicator database The community-based health insurance program uses a web-based database to collect a very limited number of indicators that are used to track progress and determine the financial viability of individual CBHI or mutuelle sections. The reporting rate for 2010 was approximately 84% of the 428 mutuelle sections reporting. Rwanda District Health System Strengthening Tool (DHSST) Over the past few years, the Clinton Foundation has been supporting the Ministry of Health to strengthen its district health system, leading to the development of the Rwanda District Health System Strengthening Framework. In 2008, this Framework was applied to all districts of Rwanda. In 2009 a completely new, web-enabled version was developed and data were collected in December 2010. It is a costing and strategic planning tool for use by District Health Units, health centres and district hospitals in Rwanda. The data collection phase of this project gathered valuable data on, amongst other areas, health infrastructure, equipment, finances and staffing to facilitate gap analyses and needs costing. The tool’s underlying data includes 40 district hospitals and 396 health centres and will soon include the national reference hospitals. It does not include private health facilities. It is currently being simplified in order for it to be updated on an annual or semi-annual basis by all districts. Rwanda Interim DHS 2007-2008 (RIDHS) The 2007-2008 Rwanda Interim Demographic and Health Survey was carried out from December 2007 to April 2008 as a follow-up to three previous surveys undertaken in 1992, 2000 and 2005. A total of 7,377 households were interviewed. Three questionnaires were administered: the household questionnaire, the women’s questionnaire, and the men’s questionnaire. The survey covered demographic characteristics, marital status, birth history, knowledge and use of family planning methods, fertility preferences, antenatal and delivery care, breastfeeding practices, vaccination and childhood illnesses, male circumcision as well as blood testing for anemia and malaria. 52 Rwanda Ministry of Health Annual Statistical Booklet 2010 Annexes: Table 44: Classification of staff categories by qualification Staff Category Qualification Administrative Staff and Administrator A1, A Administrator A2, Public Administrator A0, Accountant A0, Accountant A1, Accountant A2, C Accountant A3, Support Staff Law A0, Law A1, Law A2, Economist A0, Economist A1, E Economist (MA), Financial A1, Financial A0, Management A0, Management A1, Management (MA), Secretary A1, Secretary A2, Secretary A3, Law (MA), Communication A0, Demographer A0, Computer Technician A0, Other Support Staff, drivers, Electrician A1, Electrician A2, Electrician A3, Electromechanical Engineer A0, Electromechanical Engineer A1, Electromechanical Engineer A2, Electrician (A0), Electrician(A1), Electrician(A2), Documentalist Doctors, Specialist Doctors Doctors Bio-Chemistry A2, Human Biologist A1, LABO.A0, LABO.A1, Laboratory technician LABO.A2, LABO.A3 Medical Assistant A1, Medical Assistant A2, INF.(MA),.NurseA0, Nurses Nurse.A1, Nurse.A2, Nurse.A3, Health auxilliary, Midwife A1 Midwives Anaethesiologist A0, Anaethesiologist A1, Dentist A0, Dentist Paramedical A1, Hygienist +Assistant A1, Hygienist +Assistant A2, Physiotherapist A0, Physiotherapist A1, Physiotherapist A2, Physiotherapist A3, Physiotherapist (MA), Environmental Health A0, Nutritionist A0, Nutritionist A1, Nutritionist A2, Ophtalmologist A1, Orthopedist A1, Psychiatrist A0, Clinical Psychologist A0, Clinical Psychologist A1, Radiologist A1, Radiologist A2, Mental Health A1, Public Health A0, Public Health A1, Ophtalmologist A0, ASS SOC.A1, ASS SOC.A2, Educators .A3+Mon Ens., Educators A0, Educators A1, Educators A2, Sociology A0 Pharmacist A0, Pharmacist A1 Pharmacist Other (no qualification mentionned) Other 53
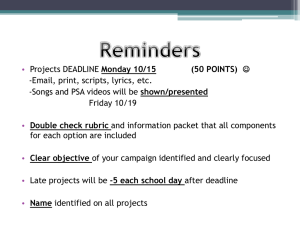
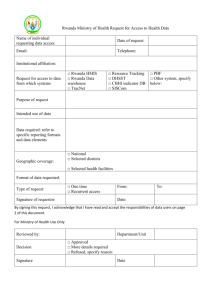
![Government of [Rwanda] - UNDP-UNEP Poverty](http://s2.studylib.net/store/data/005359438_1-2c42f5844b4637cd375e392bd4b49b8d-300x300.png)