Avenues of Improvement in the Nurses and Physician Relationship
advertisement
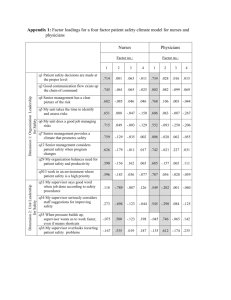
Avenues of Improvement in the Nurses and Physician Relationship for Better Patient Care: a Quality Improvement Survey Avnish Tripathi M.D., PhD, MPHa Jon Isaac M.D.a Ryan Yates M.D.a Affiliations a Division of Internal Medicine, Department of Medicine, University of Mississippi School of Medicine, Jackson MS Correspondence to: Avnish Tripathi MD, PhD, MPH; Division of Internal Medicine, Department of Medicine, University of Mississippi School of Medicine, 2500 N State St, Jackson 39216; Email: atripathi@umc.edu Word count: 393 Avnish Tripathi Background The need for cohesive working between physicians and nurses for quality patient care is well established. Several factors such as work environment, hospital policies, training, and sociodemographic characteristics may influence the relationship between physicians and nurses. It is therefore essential to examine such factors and explore avenues of improvement at institutional level. The objective of this survey study was to understand nurse's perspective and suggestions on the relationship with physicians at the University of Mississippi Medical Center (UMMC). Methods All permanent and float nurses working on one UMMC floor were invited to participate in the webbased anonymous and self-explanatory survey. The survey elements were derived from the Hospital Care Quality Information from the Consumer Perspectives (HCAHPS) and Quality Improvement Implementation Survey instruments. It was pre-piloted by two nurses. Standard imputation was done for missing data of less than 15% for objective questions. The descriptive and logistic regression analysis was used to examine the data. Results A total of 35 nurses completed the survey with the estimated response rate of 67%. Majority were females (94%); <40 years of age (54%); and non-white race/ethnicity (57%). A majority had Associates Degree in Nursing (60%); had >= 5 years of experience; and worked at UMMC <5 years (77%). Responses related to questions on work environment suggested lack of satisfaction regarding: time spent on paperwork (40%); overall workload (71%); available clerical support (60%); leadership from nursing administration (51%); non-nursing tasks required on daily basis (68%); receiving recognition of job well done (60%). A majority of nurses reported having satisfactory work relationship with physicians (69%) and that conflicts are uncommon (66%). Logistic regression suggested that those with non-white race/ethnicity (odds ratio 13.9; p-value= 0.019) and age >= 40 years (odds ratio 10.9; p-value= 0.008) were significantly more likely to report unsatisfactory relationship with physicians. More than 80% nurses agreed that further cultivation of patient centered work culture and strategies for mutual discussion on conflicts between nurses and physicians is needed. Most redundant themes in the open-ended suggestions were: inclusion of nurses during morning rounds; periodic communication about patient care plan; and greater respect of nurses' assessment of patient. Conclusion The survey highlights several avenues of quality improvement in working environment and interrelationship between nurses and physicians. Every effort should be made to understand similar deficiencies hospital wide to ultimately facilitate development of targeted quality improvement plans.