Abstract - BioMed Central
advertisement

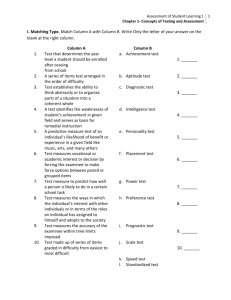
Impact of misspecifying the distribution of a prognostic factor on power and sample size for testing treatment interactions in clinical trials William M. Reichmann, MA1, 2 Michael P. LaValley, PhD2 David R. Gagnon, MD, MPH, PhD2, 3 Elena Losina, PhD1, 2 1. Department of Orthopedic Surgery, Brigham and Women’s Hospital, Boston, MA 2. Department of Biostatistics, Boston University School of Public Health, Boston, MA 3. Massachusetts Veterans Epidemiology Research and Information Center, VA Cooperative Studies Program, Boston, MA Corresponding Author: William M. Reichmann Orthopedic and Arthritis Center for Outcomes Research Brigham and Women’s Hospital 75 Francis Street, BC 4-4016 Boston, MA 02115 Tel: 617-732-5081, Fax: 617-525-7900 wreichmann@partners.org Co-authors Michael P. LaValley Department of Biostatistics Boston University School of Public Health 801 Massachusetts Avenue, 3rd Floor Boston, MA 02118 mlava@bu.edu David R. Gagnon Department of Biostatistics Boston University School of Public Health 801 Massachusetts Avenue, 3rd Floor Boston, MA 02118 gagnon@bu.edu Elena Losina Orthopedic and Arthritis Center for Outcomes Research Brigham and Women’s Hospital 75 Francis Street, BC 4-4016 Boston, MA 02115 elosina@partners.org Grant support: This research was supported in part by the National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases grants T32 AR055885 and K24 AR057827. Key words: simulation design, interaction, conditional power, adaptive design, sample size re-estimation Word count (text only): 4,834 Abstract word count: 345 Abstract Background: Interaction in clinical trials presents challenges for design and appropriate sample size estimation. Here we considered interaction between treatment assignment and a dichotomous prognostic factor with a continuous outcome. Our objectives were to describe differences in power and sample size requirements across alternative distributions of a prognostic factor and magnitudes of the interaction effect, describe the effect of misspecification of the distribution of the prognostic factor on the power to detect an interaction effect, and discuss and compare three methods of handling the misspecification of the prognostic factor distribution. Methods: We examined the impact of the distribution of the dichotomous prognostic factor on power and sample size for the interaction effect using traditional methods or standard methodology. We varied the magnitude of the interaction effect, the distribution of the prognostic factor, and the magnitude and direction of the misspecification of the distribution of the prognostic factor. We compared quota sampling, modified quota sampling, and sample size reestimation using conditional power as three strategies for ensuring adequate power and type I error in the presence of a misspecification of the prognostic factor distribution. Results: The sample size required to detect an interaction effect with 80% power increases as the distribution of the prognostic factor becomes less balanced. Negative misspecifications of the distribution of the prognostic factor led to a decrease in power with the greatest loss in power seen as the distribution of the prognostic factor became less balanced. Quota sampling was able to maintain the empirical power at 80% and the empirical type I error at 5%. The performance of the modified quota sampling procedure was related to the percentage of trials switching the quota sampling scheme. Sample size reestimation using conditional power was able to improve the empirical power under negative misspecifications (i.e. skewed distributions) but it was not able to reach the target of 80% in all situations. Conclusion: Misspecifying the distribution of a dichotomous prognostic factor can greatly impact power to detect an interaction effect. Modified quota sampling and sample size re-estimation using conditional power improve the power when the distribution of the prognostic factor is misspecified. Quota sampling is simple and can prevent misspecification of the prognostic factor, while maintaining power and type I error. 1 Background Randomized controlled trials (RCTs) are the gold standard for evaluating the efficacy of a treatment or regimen. While for most RCTs the primary hypothesis is the overall comparison of two (or more) treatments, there has been a continuing discussion over the last two decades about the use of subgroup analyses and formal tests of interaction in RCTs [1-7]. According to the most recent CONSORT statement, which was published in 2010, the analysis of subgroups should be pre-planned and accompanied by a formal test of interaction [8]. However, systematic reviews of medical and surgical RCTs have shown that many of the analyses of subgroups in RCTs have not been preplanned and have not been accompanied by a formal test of interaction [1-4]. The percentage of trials reporting their results using a formal interaction test was 13% in 1985 [1], 43% in 1997 [2], 6% from 2000 to 2003 [3], and 27% from 2005 to 2006 [4]. Investigators planning subgroup analyses within the framework of RCTs are encouraged to design RCTs to detect interaction effects using a formal interaction test. While statistical software such as nQuery Advisor and SAS can handle power and sample size calculations for detecting interaction effects, a modest body of literature exists describing the effect of the magnitude of the interaction effect and distribution of the prognostic factor have on power and sample size. Two articles by Brookes and colleagues showed that there is low power to detect an interaction when a study is powered only to detect the main effect unless size of the interaction effect is nearly twice as large as the main 2 effect [6, 7]. They also showed that power for the interaction test is maximized when the prognostic factor is distributed evenly. There are many instances in which investigators may be interested in studying the interaction between a prognostic factor and treatment. For example, an investigator is interested in studying the effect in improving functional limitation in persons with meniscal tear and concomitant knee osteoarthritis (OA). For this disease, the two treatment choices are performing arthroscopic partial meniscectomy (APM) and physical therapy (PT). However, the investigator also hypothesizes that the effect of APM compared to PT on functional limitation varies by knee OA severity. In this case, knee OA severity is the prognostic factor and how it is distributed will impact the sample size required to detect the interaction between treatment and OA severity. This article has three objectives. First, we sought to describe differences in power and sample size requirements across alternative distributions of a prognostic factor and magnitudes of the interaction effect. Second, we describe the effect of misspecification of the prognostic factor distribution and how such misspecification affects the power to detect an interaction effect. Third, we describe and discuss three methods of handling misspecification of the prognostic factor distribution by potential readjustment of the sample size or strategy during a trial. Two of these methods are sampling-based and do not require an interim statistical testing of the outcome. The third method uses a twostage adaptive design approach that re-estimates the sample size based on the 3 conditional power at an interim analysis where 50% of the patients have been enrolled. 4 Methods Overview We conducted an analysis examining the impact of how different distributions of a dichotomous prognostic factor affect the power (and sample size needed to obtain 80% power) to detect an interaction between the prognostic factor and treatment in RCTs. We also studied the impact of misspecifying (positive and negative misspecifications) the distribution of the prognostic factor on power and sample size. We varied the magnitude of the interaction effect, the distribution of the prognostic factor, and the magnitude of the misspecification. Lastly, we compare three methods for ensuring appropriate overall power and type I error under the misspecification of the distribution of the prognostic factor. These methods are quota sampling, modified quota sampling, and sample size re-estimation using conditional power. Specification of key parameters used in the paper Treatment variable: The treatment variable was distributed as a binomial variable (active vs. placebo) with probability of 0.5. For the purposes of this paper the treatment variable was assumed to always have a balanced distribution (i.e. 50% on level 1 receiving active treatment; 50% on level 2 receiving placebo). For illustration purposes, we assumed that APM was the active treatment and that PT was the placebo. 5 Prognostic factor: The prognostic factor was defined as dichotomous variable with kj representing the jth level of the prognostic factor. When referring to the distribution of the prognostic factor we indicated the percentage in the k1 level of the prognostic factor, defined as p1. We varied p1 from 10% to 50% in 10% increments. Misspecification of the prognostic factor: The misspecification of the prognostic factor was defined by the parameter q. The misspecification could be positive or negative. For example, if the planned distribution of the prognostic factor was 20% and the actual distribution of the prognostic factor was 25%, then the misspecification of the prognostic factor (q) was +5%. Possible values of q were 15%, -5%, 0 (i.e. no misspecification), +5%, and +15%. Outcome variable: We assumed that our outcome variable was continuous and normally distributed. In our example, the outcome can be interpreted as the improvement in function after APM or PT as measured by a score or scale. We specified the mean improvement for all four possible combinations of treatment and the prognostic factor. We considered two different values (25 and 15) for the mean improvement in the active/k1 treatment/prognostic factor combination (i.e. APM/mild knee OA severity). The mean improvement in the active/k2, placebo/k1, and placebo/k2 groups were held constant at 5, 5, and 0 respectively. We assumed a common standard deviation (σ) of 10 for all four combinations. 6 Magnitude of the interaction: We defined the magnitude of the interaction between prognostic factor and treatment effect according to the method by Brookes and colleagues [6, 7]. Let μij be mean improvement in the ith treatment and jth level of the prognostic factor. We then defined the treatment efficacy in the jth level of the prognostic factor as: j 1 j 2 j (1) We then defined the interaction effect (denoted as θ) as follows: 1 2 11 21 12 22 (2) Thus θ, which served as the basis of our choice of mean improvement values, varied as μ11 varied. The magnitudes of the interaction effect that we considered were 15 and 5. The estimate of the interaction effect was defined as follows: ˆ x11 x21 x12 x22 (3) Then, the variance of the interaction effect under balanced treatment groups and distribution of the prognostic factor p1 can be derived as follows (note that N equals the total sample size for the trial): VAR ˆ VAR x11 x 21 x12 x22 VARx11 VARx 21 VAR x12 VAR x 22 2 n11 2 n21 2 0.5 * p1 * N 2 n12 2 n22 2 0.5 * 1 p1 * N 4 2 4 2 p1 * N 1 p1 * N 4 2 p1 * 1 p1 * N 2 0.5 * p1 * N 2 0.5 * 1 p1 * N (4) 7 Initial sample size for interaction effects The sample size required for the ith treatment and jth prognostic factor to detect the interaction effect described above (a balanced design) with a twosided significance level of α and power equal to 1– β has been previously published by Lachenbruch [9]. 4 2 z1 z1 2 nij 2 2 (5) In these formulas z1–β represents the z-value at the 1–β (theoretical power) quantile of the standard normal distribution and z1–α/2 represents the z-value at the 1–α/2 (probability of a type I error) quantile of the standard normal distribution. Under a balanced design with p1=0.5 we can just multiply nij by four to obtain the total sample size since there are four combinations of treatment and prognostic factor. A limitation of this formula is that it uses critical values from the standard normal distribution rather than the Student’s t-distribution as most statistical tests of interaction are performed using a t-distribution. To account for this we calculated the total sample size required to detect an interaction effect with a two-sided significance level of α and power equal to 1– β: 1. Use formula 5 (above) to calculate the sample size required for each combination of treatment and prognostic factor under a balanced design. 2. Calculate a new sample size nij* required for each combination of treatment and prognostic factor under a balanced design using the following formula 6 below. In this formula the z-critical values have been replaced with t-critical values with nij degrees of freedom. 8 4 2 t1 ,nij 1 t1 ,n 1 2 ij nij* 2 2 (6) 3. Set nij equal to n ij* and repeat step 2. 4. Repeat step 3 until n ij* converges. This will usually occur after 2 or 3 iterations. 5. Lastly, multiply n ij* by 1 to obtain the final total sample size N. p1 1 p1 Effect of misspecifying the distribution of the prognostic factor The effect of misspecifying the distribution of the prognostic factor was evaluated using power curves. Power for the interaction test, where Ψ is the cdf of the Student’s t-distribution, by misspecification of the prevalence of the prognostic, magnitude of the interaction effect, and planned prevalence of the prognostic factor was calculated using equation 7 below. (7) Strategies for accounting for the misspecification of the distribution of the prognostic factor Quota sampling: The quota sampling approach was performed using the following steps. First, for a given set of parameters, we would determine the sample size needed to detect an interaction effect with 80% power. We then fixed the number of participants to be recruited for each level of the prognostic 9 factor. For example, if the final total sample size was 200 and the planned distribution of the prognostic factor was 30% in the k1 group and 70% in the k2 group then exactly 60 subjects would be recruited in the k1 group and 140 in the k2 group. This method removes the variability in the sampling distribution and ensures that the sampled prognostic factor distribution always matches what was planned for. Because of this approach, the observed distribution of the prognostic factor in the trial will always match the planned distribution and there will be no misspecification. However, this method may require turning away potential subjects because one level of the prognostic factor is already filled, delaying trial completion. Also, it may reduce the external validity of the overall treatment results as the trial subjects can become less representative of the unselected population of interest. Because of these limitations we also considered a modified quota sampling approach. Modified quota sampling: The modified quota sampling approach was performed using the following steps. First, as in the quota sampling approach, the sample size needed to detect an interaction effect with 80% power was determined for the pre-specified parameters. Next, the simulated study enrolled the first N/2 subjects. After the first N/2 subjects were enrolled we tested to see if the sampling distribution of the prognostic factor was different from what was planned for using a one-sample test of the proportion. If this result was statistically significant at the 0.05 level then a quota sampling approach was undertaken for the second N/2 subjects to be enrolled to ensure that the sampling distribution of the prognostic 10 factor matched the planned distribution exactly. If the result was not statistically significant then the study continued to enroll normally, allowing for variability in the distribution of the prognostic factor. Sample size re-estimation using conditional power: The last method for accounting for the misspecification of the distribution of the prognostic factor used the conditional power of the interaction test at an interim analysis to reestimate the sample size. We modified the methods of Denne to carry out this procedure [10]. We assumed that the interim analysis occurred after the first N/2 subjects were enrolled. The critical value at the interim analysis (c1) and the final analysis (c2) were determined by the O’Brien-Fleming alpha-spending function [11] using the SEQDESIGN procedure in the SAS statistical software package. We also used the SEQDESIGN procedure to calculate a futility boundary at the interim analysis (b1). Since these critical values are based on a standard normal distribution and not the student’s t-distribution we converted the critical values to those based on the student’s t-distribution. First, we converted the original critical values to the corresponding percentile of the standard normal distribution. We then converted these percentiles to the corresponding critical value of the Student’s t-distribution with N-4 degrees of freedom. At the interim analysis, if the absolute value of the interaction test statistic was less than the futility boundary (t1 < b1) then we stopped the trial for futility and considered the result of the trial to be not statistically significant. If the absolute value of the test statistic was greater than the interim critical value (c1) 11 then we stopped the trial for efficacy and considered the result of the trial to be statistically significant. If absolute value of the test statistic was greater than b1 but less than c1 then we evaluated the conditional power and determined if sample size re-estimation was necessary. The following paragraphs outline this procedure. The following is the conditional power formula proposed by Denne for the two group comparison of means: nt n1 c 2 n2 z1 n1 CP 1 nt n1 (8) Here, c2 is the final critical value, n2 is the sample size at the final analysis, nt is the originally planned total sample size, z1 is the test statistic for the interaction at the interim analysis, n1 is sample size at the interim analysis, δ is the difference in means, and σ is the common standard deviation for the two groups. We updated the formula by replacing z1 with t1 (because the interaction test uses the Student’s t-distribution), δ (difference in means between groups) with θ (magnitude of the interaction effect), and Φ (cumulative distribution function of a standard normal distribution) with Ψ (cumulative distribution function of a student’s t-distribution). Recall that p1 is the proportion in the k1 group and σ is the common standard deviation: nt n1 p1 1 p1 c 2 n2 t1 n1 4 2 CP 1 nt n1 (9) 12 Initially n2=nt as conditional power is calculated as if you were to not re-estimate the sample size. The values of θ, σ, and p1 for the conditional power formula were estimated at the interim analysis. If the conditional power was less than 80% then a new n2 was estimated such that conditional power was 80% and a new final critical value, c2, was calculated as a function of the original final critical value, c~2 , and the interim test statistic t1 using the following formula: c2 c~2 In equation 10, γ1 n1 nt 2 1 t1 2 1 1 and γ 2 n 2 nt 1 2 1 1 2 1 1 (10) so that the final critical value is also a function of n1, n2 (the new total sample size), and nt (the original total sample size). Since all values except n2 are fixed, we can calculate the new critical value c2 for new final sample sizes n2. According to Denne, this method for reestimating the sample size maintains the overall Type I error rate at α (equal to 0.05 in our case) [10]. The final sample size n2 and final critical value c2 were chosen so that the conditional power formula shown in equation 10 was equal to 80%. If the conditional power was greater than 80% at the interim analysis then we used the originally calculated nt as the final sample size (n2=nt) so that the final sample size was only altered to increase the conditional power to 80%. Validating the conditional power formula To ensure that the modification the conditional power formula (formula 9) was appropriate, we performed a validation study using simulations. For each combination of prevalence of the prognostic factor and magnitude of the 13 interaction ran 10 trials to obtain 10 interim test statistics for each combination of parameters. At the interim analysis we calculated the conditional power based on the hypothesized values of θ, σ, and p1. For each trial, the second half of the trial was simulated 5,000 times to obtain the empirical conditional power. Since there were 10 different combinations of prevalence of the prognostic factor and magnitude of the interaction effect and 10 trials for each combination, the plot generated 100 points. We generated a scatter plot of the empirical conditional power based on 5,000 replicates against the calculated conditional power (Figure 2). Values that line up along the y=x line demonstrate that formula provided an accurate estimation of the conditional power. Simulation study details Five thousand replications were performed for each combination of the interaction effect and proportion k1. We first evaluated the empirical power for detecting the interaction effect without accounting for misspecification of the distribution of the prognostic factor. We varied the misspecification of the prognostic factor at -15%, -5%, 0%, +5%, and +15%. For the quota sampling method we did not vary the misspecification of the distribution of the prognostic factor because the definition of the method does not allow for misspecifications. While we did not expect the quota sampling method to have power or type I error estimates that differ from the traditional method, we conducted the simulation study for this study design method to confirm there was no impact on power and type I error. For the modified quota sampling method and sample size re- 14 estimation using conditional power we used the same misspecifications as described above. We calculated the overall empirical power for the interaction effect for all three methods. This was defined as the percentage of statistically significant interaction effects across the 5,000 replicates. Empirical type I error was calculated in a similar fashion for these three methods, but the interaction effect was assumed to be zero and the sample size we used was the sample sizes for the planned interaction effects of 15 and 5. For the sample size re-estimation method we also calculated the empirical conditional power. This was defined as the number of statistically significant interaction effects detected at the 0.05 level among trials that re-estimated the sample size. Because the sample size could change, we also calculated the mean and median final sample size for the entire procedure. The margin of error for empirical power and type I error was calculated using the half width of the 99% confidence interval based on a binomial distribution with a sample size of 5,000. Since trials were planned with 1– β=0.80 α=0.05 this led to margins of error equal of 0.015 and 0.008 when assessing empirical power and type I error respectively. 15 Results Effect of misspecifying the distribution of the prognostic factor on power for the interaction test Power curves when using the traditional study design are shown in Figure 1. There was a small difference in power when comparing the magnitude of the interaction effect and holding the planned prevalence of the prognostic factor and the misspecification of the prognostic factor equal. This was due to rounding up of the final sample size and the choice of using the t-critical values instead of the z-critical values, which were larger when the magnitude of the interaction was larger. As expected, under no misspecification of the prevalence of the prognostic factor, power was at 80%. For negative misspecifications, power was below 80% and power decreased more for a lower planned prevalence of the prognostic factor. For positive misspecifications, power was greater than 80% except when the planned prevalence of the prognostic factor was 50% (i.e. a balanced design). Performance of the quota sampling procedure The quota sampling procedure performed well in terms of empirical power (Table 1) and type I error (Table 2) as a strategy to account for misspecifying the distribution of the prognostic factor. The empirical power was reached or exceeded the target power of 80% for all combinations of θ and distributions of the prognostic factor. The type I error was near the target type I error of 5% for all combinations of sample size and distributions of the prognostic factor. 16 Performance of the modified quota sampling procedure Under no misspecification of the distribution of the prognostic factor, the modified quota sampling procedure performed well with empirical power greater than or equal to 80% across all situations (Table 1). The type I error rate was also near 5% for all combinations under no misspecification (Table 2). Under negative misspecifications of the distribution of the prognostic factor, empirical power was improved in comparison to doing nothing but 80% power was not achieved in all cases (Table 3). The ability of the procedure to attain 80% power under misspecifications of the prognostic factor was dependent on the percentage of trials that switched to quota sampling after 50% enrollment. The likelihood of switching to quota sampling was related to the magnitude of the interaction effect, the planned distribution of the prognostic factor, and the magnitude of the negative misspecification. When the magnitude of the interaction effect was five and the misspecification of the distribution of the prognostic factor was -15%, greater than 99.8% of the trials switched to the quota sampling method and the procedure attained 80% power. However, when the magnitude of the interaction effect was 15, and the misspecification of the distribution of the prognostic factor was -5%, the modified quota sampling approach only attained 80% power when the planned distribution of the prognostic factor was 40% or 50% (Table 3). For positive misspecifications of the distribution of the prognostic factor, the modified quota sampling procedure attained 80% for all combinations of the 17 magnitude of the interaction effect and planned distribution of the prognostic factor (Table 3). Type I error was maintained at 5% or within the margin of error for all combinations of sample size, planned distribution of the prognostic factor, and misspecification of the distribution of the prognostic factor. (Table 4). Validating the conditional power formula Figure 1 shows the validation results for our conditional power formula. All possible values of θ and distribution of the prognostic factor are included, but we did not assume any misspecification in the prognostic factor. When we use trial design parameters in the conditional power formula rather than the estimates, the points line up along the y=x line, which implies that the formula we used to calculate the conditional power was similar to the empirical conditional power. These results give us confidence that the sample size re-estimation presented in the next section performed as expected. Performance of the sample size re-estimation using conditional power procedure Under no misspecification of the distribution of the prognostic factor, using the sample size re-estimation procedure resulted in an increase in overall power due to the requirement of conditional power of 80% at the interim analyis. Across different combinations θ and the planned distribution of the prognostic factor, the empirical power ranged between 88% and 91% (Table 1). Despite the increase in 18 power, type I error was maintained at 5% or less for all of the simulations under no misspecification of the distribution of the prognostic factor (Table 2). When we assumed there was a misspecification of -5% for the distribution of the prognostic factor, the empirical power was greater than 80% except when the planned distribution of the prognostic factor was 10%. In this case the empirical power was 72%-73%, which was an improvement compared to using traditional methods. For a misspecification of the distribution of the prognostic factor of -15% and planned prognostic factor distribution of 20%, the empirical power was also less than 80% (empirical power of 56%-60%), but was higher than using traditional methods. The inability to attain 80% power in these situations was directly related to the fact that more trials were stopped for futility at the interim analysis. In the situations where the empirical power failed to attain 80% power the percentage of trials stopping for futility ranged between 15% and 26% (Table 5). The empirical type I error was below 5% for all combinations of θ, planned distribution of the prognostic factor, and misspecification of the distribution of the prognostic factor. Under the null hypothesis, the percentage of trials stopping for futility ranged between 42% and 45%, while the percentage of trials stopping for efficacy was at most 0.6% (Table 6). Conditional properties are displayed in Table 7. In almost all cases the empirical conditional power greater than 80%. The two situations in which the empirical conditional power was less than 80% was when there was a negative misspecification of -15% of the distribution of the prognostic factor coupled with 19 an initial planned distribution of the prognostic factor of 20%. Here the empirical conditional power was 76% for θ equal to 5 and 15. The mean total sample size was always greater than the original planned sample size. Some of these mean total sample sizes were more than double the final sample size. However, the median sample size was equal to or very close to the original total sample size in all cases (Table 7). 20 Discussion We evaluated the impact of misspecifying the distribution of a prognostic factor on the power and sample size for interaction effects in an RCT setting. We showed that negative misspecification of the distribution of the prognostic factor resulted in a loss of power and a need for an increased sample size, especially when the planned distribution of the prognostic factor moved further away from a balanced design. We evaluated three methods for handling misspecifying the distribution of the prognostic factor when investigating interaction effects in an RCT setting. The first two methods dealt with how the subjects would be sampled. The quota sampling method removed any variability in the prognostic factor and by definition misspecification of the distribution of the prognostic factor was not possible. For example if a trial was set to enroll 200 subjects with 30% in the k1 level of the prognostic factor then enrollment would be capped at 60 subjects in the k1 level and 140 in the k2 level. This method did a good job of maintaining the power at 80% and controlling the type I error at 5%. The modified quota sampling approach did not perform as well in all situations. In summary, this method enrolled subjects randomly for the first half the trial. The sampling method would switch to the quota sampling approach if the distribution of the prognostic factor differed significantly from what was planned. Power was maintained at 80% when the percentage of trials switching to the quota sampling approach was large. However, when the percentage was small and there was a 21 negative misspecification of the distribution of the prognostic factor the power was compromised. The last method used conditional power at an interim analysis (after 50% enrollment) to re-estimate the sample size. We adapted the method used by Denne [10]. This method provided the most consistent results with respect to overall power and type I error. The main reason this method could not maintain empirical power at 80% under a negative misspecification is that too many trials stopped for futility before the sample size could be re-estimated and all of the type II error was used up at the interim analysis. This result does not diminish the value of the sample size re-estimation procedure since misspecification of other trial parameters that diminish power would have a similar effect. The findings from our study detail methods for handling the misspecification of the distribution of a prognostic factor when detecting an interaction effect in an RCT setting. An advantage of the quota sampling approach over using the conditional power formula is that the final sample size does not need to be changed and an interim analysis that uses some of the alpha level does not need to be undertaken. However, the quota sampling approach is sensitive to distortions in misspecifying the distribution of the prognostic factor in terms of trial duration as it may take longer to recruit the necessary patients from the appropriate level of the prognostic factor. Using sample size re-estimation does not have this issue, but it is sensitive to the values used in the conditional power formula. 22 As with any study that uses simulations, there are several limitations to our study. One limitation is that not all interaction effects were explored and we only study a 2 by 2 interaction effect. However summarizing the interaction effect with one contrast would not be feasible if three or more treatments or levels of the prognostic factor were explored. Future work could explore looking at these interaction effects. We also did not examine the impact of informative cross-over. Many times subjects randomized to one arm (ex. non-surgical therapy) in a study will cross-over to another arm (ex. surgical therapy). The impact of differing cross-over rates should be explored. Another limitation is that we did not look at the impact of unequal variances. This should be the goal of future work as levels of a prognostic factor can impact variability in the outcome. Lastly, we only studied the impact of one sample size re-estimation procedure as described by Denne in 2001 [10]. However, there are many different methods of re-estimating the sample size that could be studied [12]. However, the method described by Denne still is a valid and acceptable method according to the FDA guidelines on Adaptive Design Clinical Trials for Drugs and Biologics [13]. 23 Conclusions We examined three methods for dealing with the misspecification of the distribution of the prognostic factor when determining the treatment by prognostic factor interaction effects in an RCT setting. Sample size re-estimation using conditional power was able to improve the power when there was a negative misspecification of the distribution of the prognostic factor while maintaining appropriate type I error. As more studies seek to explore interaction effects as their primary outcome in RCTs, these methods will be useful for clinicians planning their studies. Further research should look at the impact of cross-over between treatment groups. 24 Competing interests The authors declare that they have no competing interests Authors’ contributions WMR designed the simulation study, interpreted the data, and drafted the manuscript. MPL interpreted the data and critically revised the manuscript. DRG interpreted the data and critically revised the manuscript EL interpreted the data and critically revised the manuscript All authors read and approved the final manuscript Acknowledgements and Funding We would like to acknowledge Dr. C. Robert Horsburgh for his valuable comments on earlier drafts of this manuscript. This research was supported in part by the National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases grants T32 AR055885 and K24 AR057827. References 1. Pocock SJ, Hughes MD, Lee RJ: Statistical problems in the reporting of clinical trials. A survey of three medical journals. N Engl J Med 1987, 317(7):426-432. 2. Assmann SF, Pocock SJ, Enos LE, Kasten LE: Subgroup analysis and other (mis)uses of baseline data in clinical trials. Lancet 2000, 355(9209):1064-1069. 3. Bhandari M, Devereaux PJ, Li P, Mah D, Lim K, Schunemann HJ, Tornetta P, 3rd: Misuse of baseline comparison tests and subgroup analyses in surgical trials. Clin Orthop Relat Res 2006, 447:247-251. 4. Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM: Statistics in medicine--reporting of subgroup analyses in clinical trials. N Engl J Med 2007, 357(21):2189-2194. 5. Lagakos SW: The challenge of subgroup analyses--reporting without distorting. N Engl J Med 2006, 354(16):1667-1669. 6. Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G: Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives. Health Technol Assess 2001, 5(33):156. 7. Brookes ST, Whitely E, Egger M, Smith GD, Mulheran PA, Peters TJ: Subgroup analyses in randomized trials: risks of subgroup-specific analyses; power and sample size for the interaction test. J Clin Epidemiol 2004, 57(3):229-236. 8. Schulz KF, Altman DG, Moher D: CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Trials, 11:32. 9. Lachenbruch PA: A note on sample size computation for testing interactions. Stat Med 1988, 7(4):467-469. 10. Denne JS: Sample size recalculation using conditional power. Stat Med 2001, 20(17-18):2645-2660. 11. O'Brien PC, Fleming TR: A multiple testing procedure for clinical trials. Biometrics 1979, 35(3):549-556. 12. Chow SC, Chang M: Adaptive Design Methods in Clinical Trials: Chapman and Hall/CRC Press; 2007. 13. Food and Drug Administration. Guidance for Industry: Adaptive Design Clinical Trials for Drugs and Biologics [http://www.fda.gov/downloads/DrugsGuidanceComplianceRegulatoryInformation /Guidances/UCM201790.pdf] Figure Legend Figure 1: Power using traditional study design by magnitude of the interaction effect, planned prevalence of the prognostic factor, and misspecification of the prevalence of the prognostic factor Figure 2: Results of the conditional power validation displaying a plot of the empirical conditional power (y-axis) and calculated conditional power calculated at the interim analysis (x-axis). The solid line represents the y=x line. Tables Table 1. Empirical power for all three methods when there was no misspecification of the distribution of the prognostic factor. Planned distribution of Sample size the prognostic Planned Quota Modified quota re-estimation using factor sampling sampling conditional power θ nt 5 10% 1,418 0.8088 0.8054 0.8836 20% 798 0.8152 0.8082 0.8916 30% 608 0.8178 0.8014 0.8870 40% 532 0.8116 0.8036 0.8866 50% 512 0.8156 0.8098 0.8974 15 10% 178 0.8556 0.8204 0.8890 20% 100 0.8490 0.8128 0.8930 30% 78 0.8442 0.8316 0.9012 40% 68 0.8556 0.8322 0.9038 50% 64 0.8412 0.8256 0.9082 The margin of error based on the 99% confidence interval is 0.015. Table 2. Empirical type I error for all three methods when there was no misspecification of the distribution of the prognostic factor. Planned Sample size distribution of Modified re-estimation the prognostic Planned Quota quota using conditional factor sampling sampling power θ nt 0 10% 1,418 0.0496 0.0534 0.0210 20% 798 0.0484 0.0522 0.0260 30% 608 0.0494 0.0464 0.0286 40% 532 0.0510 0.0514 0.0302 50% 512 0.0532 0.0540 0.0248 0 10% 178 0.0494 0.0512 0.0248 20% 100 0.0488 0.0516 0.0274 30% 78 0.0536 0.0524 0.0224 40% 68 0.0472 0.0496 0.0302 50% 64 0.0482 0.0482 0.0328 The margin of error based on the 99% confidence interval is 0.008. Table 3. Empirical power and percentage of trials switching to the quota sampling scheme for the modified quota sampling method. Planned distribution of Percent of trials the prognostic Planned switching to quota factor Empirical power sampling θ nt Misspecification of the prognostic factor: -5% 5 10% 1,418 0.8012 99.98% 20% 798 0.7736 74.08% 30% 608 0.7802 47.52% 40% 532 0.7932 36.64% 50% 512 0.8060 35.50% 15 10% 178 0.6636 33.04% 20% 100 0.7400 11.06% 30% 78 0.7940 11.84% 40% 68 0.8164 11.90% 50% 64 0.8122 8.48% Misspecification of the prognostic factor: -15% 5 10% 1,418 --20% 798 0.8022 100.00% 30% 608 0.8024 100.00% 40% 532 0.8058 99.94% 50% 512 0.8090 99.82% 15 10% 178 --20% 100 0.7788 89.06% 30% 78 0.7834 63.64% 40% 68 0.7904 49.70% 50% 64 0.8038 40.00% Misspecification of the prognostic factor: +5% 5 10% 1,418 0.8000 98.28% 20% 798 0.8090 67.72% 30% 608 0.8278 49.32% 40% 532 0.8092 37.08% 50% 512 0.7984 36.30% 15 10% 178 0.8880 35.14% 20% 100 0.8656 16.62% 30% 78 0.8542 10.94% 40% 68 0.8350 7.86% 50% 64 0.8198 8.60% Misspecification of the prognostic factor: +15% 5 10% 1,418 0.8738 100.00% 20% 798 0.8010 100.00% 30% 608 0.8092 99.98% 40% 532 0.8088 99.80% 50% 512 0.8064 99.86% 15 10% 178 0.8942 97.82% 20% 100 0.8504 72.44% 30% 78 0.8572 50.72% 40% 68 0.8466 38.48% 50% 64 0.8174 40.88% The margin of error based on the 99% confidence interval is 0.015. Table 4. Empirical type I error and percentage of trials switching to the quota sampling scheme for the modified quota sampling method. Planned distribution of Percent of trials the prognostic Planned Empirical type I switching to quota factor error sampling θ nt Misspecification of the prognostic factor: -5% 0 10% 1,418 0.0528 99.90% 20% 798 0.0506 74.26% 30% 608 0.0498 47.34% 40% 532 0.0480 36.66% 50% 512 0.0492 36.06% 0 10% 178 0.0566 34.74% 20% 100 0.0496 12.12% 30% 78 0.0528 11.24% 40% 68 0.0452 11.30% 50% 64 0.0522 8.80% Misspecification of the prognostic factor: -15% 0 10% 1,418 --20% 798 0.0500 100.00% 30% 608 0.0496 100.00% 40% 532 0.0518 99.92% 50% 512 0.0568 99.76% 0 10% 178 --20% 100 0.0578 89.60% 30% 78 0.0522 62.82% 40% 68 0.0542 50.56% 50% 64 0.0478 41.20% Misspecification of the prognostic factor: +5% 0 10% 1,418 0.0568 98.68% 20% 798 0.0490 68.74% 30% 608 0.0490 48.10% 40% 532 0.0508 36.48% 50% 512 0.0508 36.64% 0 10% 178 0.0504 34.46% 20% 100 0.0534 16.32% 30% 78 0.0496 10.90% 40% 68 0.0450 8.50% 50% 64 0.0502 8.94% Misspecification of the prognostic factor: +15% 0 10% 1,418 0.0462 100.00% 20% 798 0.0490 100.00% 30% 608 0.0484 100.00% 40% 532 0.0516 99.76% 50% 512 0.0522 99.86% 0 10% 178 0.0452 97.48% 20% 100 0.0444 70.72% 30% 78 0.0526 51.00% 40% 68 0.0524 38.60% 50% 64 0.0528 40.72% The margin of error based on the 99% confidence interval is 0.008. Table 5. Empirical power and the percentage of trials stopping for futility and efficacy for sample size re-estimation using conditional power. Planned Percent distribution of Percent stopping for the prognostic Planned Empirical stopping for efficacy factor power futility θ nt Misspecification of the prognostic factor: -5% 5 10% 1,418 0.7324 16.58% 5.76% 20% 798 0.8410 10.34% 11.76% 30% 608 0.8616 9.02% 13.72% 40% 532 0.8754 8.24% 15.42% 50% 512 0.8868 7.64% 16.22% 15 10% 178 0.7246 17.14% 7.90% 20% 100 0.8232 12.26% 11.82% 30% 78 0.8736 8.94% 14.76% 40% 68 0.8936 7.72% 15.80% 50% 64 0.9010 7.10% 16.38% Misspecification of the prognostic factor: -15% 5 10% 1,418 ---20% 798 0.5614 26.06% 3.5% 30% 608 0.7536 15.46% 7.3% 40% 532 0.8304 10.72% 10.80% 50% 512 0.8750 8.34% 14.32% 15 10% 178 ---20% 100 0.6026 22.68% 4.96% 30% 78 0.7634 15.76% 8.50% 40% 68 0.8412 10.78% 11.86% 50% 64 0.8734 9.32% 14.76% Misspecification of the prognostic factor: +5% 5 10% 1,418 0.9528 3.10% 27.44% 20% 798 0.9194 5.58% 20.94% 30% 608 0.9064 6.26% 18.36% 40% 532 0.8898 7.18% 17.16% 50% 512 0.8868 7.52% 16.02% 15 10% 178 0.9476 3.94% 29.36% 20% 100 0.9194 5.70% 21.78% 30% 78 0.9204 5.94% 20.38% 40% 68 0.9146 6.36% 18.28% 50% 64 0.9056 6.96% 15.88% Misspecification of the prognostic factor: +15% 5 10% 1,418 0.9868 0.94% 45.24% 20% 798 0.9494 3.38% 27.26% 30% 608 0.9186 5.34% 20.84% 40% 532 0.8990 6.98% 17.12% 50% 512 0.8822 8.00% 14.30% 15 10% 178 0.9902 0.78% 49.94% 20% 100 0.9584 3.18% 29.86% 30% 78 0.9412 4.32% 22.32% 40% 68 0.9108 6.56% 17.12% 50% 64 0.8816 8.76% 13.84% The margin of error based on the 99% confidence interval is 0.015. Table 6. Empirical type I error and the percentage of trials stopping for futility and efficacy for sample size re-estimation using conditional power. Planned Percent distribution of Percent stopping for the prognostic Planned Empirical stopping for efficacy factor type I error futility θ nt Misspecification of the prognostic factor: -5% 0 10% 1,418 0.0278 43.48% 0.24% 20% 798 0.0264 44.54% 0.26% 30% 608 0.0262 42.66% 0.20% 40% 532 0.0280 44.16% 0.24% 50% 512 0.0246 42.88% 0.30% 0 10% 178 0.0304 42.94% 0.40% 20% 100 0.0276 42.44% 0.28% 30% 78 0.0252 43.16% 0.54% 40% 68 0.0230 43.08% 0.44% 50% 64 0.0298 42.00% 0.56% Misspecification of the prognostic factor: -15% 0 10% 1,418 ---20% 798 0.0254 43.62% 0.24% 30% 608 0.0278 42.94% 0.30% 40% 532 0.0282 44.00% 0.36% 50% 512 0.0248 42.62% 0.32% 0 10% 178 ---20% 100 0.0326 44.24% 0.50% 30% 78 0.0282 42.52% 0.44% 40% 68 0.0286 42.62% 0.42% 50% 64 0.0296 43.26% 0.50% Misspecification of the prognostic factor: +5% 0 10% 1,418 0.0314 41.46% 0.36% 20% 798 0.0284 42.94% 0.22% 30% 608 0.0296 44.76% 0.44% 40% 532 0.0312 43.82% 0.32% 50% 512 0.0290 44.16% 0.36% 0 10% 178 0.0284 43.64% 0.30% 20% 100 0.0274 43.30% 0.38% 30% 78 0.0296 43.66% 0.44% 40% 68 0.0280 44.24% 0.48% 50% 64 0.0290 43.82% 0.46% Misspecification of the prognostic factor: +15% 0 10% 1,418 0.0244 43.32% 0.28% 20% 798 0.0274 44.44% 0.34% 30% 608 0.0232 43.98% 0.20% 40% 532 0.0290 43.18% 0.32% 50% 512 0.0284 44.22% 0.32% 0 10% 178 0.0282 43.36% 0.38% 20% 100 0.0282 42.50% 0.36% 30% 78 0.0266 43.92% 0.34% 40% 68 0.0266 44.30% 0.46% 50% 64 0.0248 42.48% 0.34% The margin of error based on the 99% confidence interval is 0.008. Table 7 Percentage of trials re-estimating the sample size, conditional power among trials that re-estimated the sample size and overall mean and median sample size for sample size re-estimation using conditional power. Planned distribution of Percent Empirical Mean Median the prognostic Planned re-estimating conditional sample sample factor sample size power size size θ nt Misspecification of the prognostic factor: 0% 5 10% 1,418 37.44% 0.9471 2,500 1,418 20% 798 37.30% 0.9566 1,470 798 30% 608 37.74% 0.9671 1,143 608 40% 532 38.00% 0.9689 984 532 50% 512 39.44% 0.9660 989 512 15 10% 178 37.44% 0.9701 327 178 20% 100 40.48% 0.9674 202 100 30% 78 39.28% 0.9695 150 78 40% 68 42.02% 0.9719 155 68 50% 64 43.58% 0.9748 154 64 Misspecification of the prognostic factor: -5% 5 10% 1,418 49.70% 0.8881 3,568 1,418 20% 798 43.12% 0.9429 1,696 798 30% 608 40.98% 0.9458 1,231 608 40% 532 38.56% 0.9570 1,062 532 50% 512 38.82% 0.9629 987 512 15 10% 178 45.00% 0.8738 402 178 20% 100 42.54% 0.9342 219 100 30% 78 43.56% 0.9660 171 78 40% 68 43.38% 0.9779 153 68 50% 64 44.40% 0.9770 155 64 Misspecification of the prognostic factor: -15% 5 10% 1,418 ----20% 798 51.98% 0.7618 2,425 865 30% 608 47.34% 0.8952 1,439 608 40% 532 44.96% 0.9346 1,155 532 50% 512 41.42% 0.9546 1,028 512 15 10% 178 ----20% 100 48.70% 0.7573 267 100 30% 78 46.80% 0.9167 190 78 40% 68 47.38% 0.9565 161 68 50% 64 44.50% 0.9685 148 64 Misspecification of the prognostic factor: +5% 5 10% 1,418 25.94% 0.9861 1,984 1,418 20% 798 33.26% 0.9747 1,310 798 30% 608 35.76% 0.9676 1,096 608 40% 532 37.68% 0.9618 975 532 50% 512 39.24% 0.9623 969 512 15 10% 178 28.32% 0.9845 263 178 20% 100 35.36% 0.9762 177 100 30% 78 37.42% 0.9840 153 78 40% 68 43.32% 0.9797 150 68 50% 64 45.72% 0.9790 157 64 5 15 10% 20% 30% 40% 50% 10% 20% 30% 40% 50% Misspecification of the prognostic factor: +15% 1,418 15.04% 0.9960 1,472 798 27.34% 0.9824 1,159 608 34.22% 0.9673 1,007 532 38.58% 0.9725 1,026 512 41.56% 0.9644 1,045 178 14.40% 0.9944 190 100 30.38% 0.9888 159 78 37.62% 0.9856 149 68 43.78% 0.9753 151 64 48.00% 0.9708 168 1,418 798 608 532 512 89 100 78 68 64