Frontotemporal Dementia - World Federation of Scientists
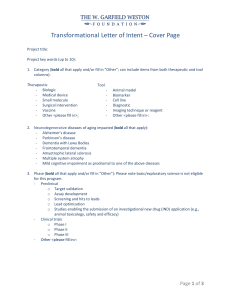
advertisement

Frontotemporal Dementia (FTD): Insights into Wisdom and Altruism Bruce L. Miller, MD Abstract FTD attacks the frontoinsular brain circuits that mediate wisdom and altruism. By contrast, Alzheimer’s disease (AD) attacks posterior brain regions that facilitate memory, navigation, reading and writing. These circuits function in a reciprocal fashion – turning on the frontal circuit turns off posterior brain regions, while turning on posterior circuits turns off frontal brain regions. The symptoms associated with FTD include profound deficits in behavior, social cognition, moral reasoning and empathy. Conversely, navigation, writing and drawing often remain normal or become enhanced in these same patients. Visual creativity is seen in many patients with left frontal or temporal degeneration. In AD, some individuals show enhanced kindness and generosity in the early stages of the illness. The phenomenology of these changes is described, and the aspects of brain aging that protect the future of humanity are noted. Behavioral Variant Frontotemporal Dementia (bvFTD) Patients with behavioral variant frontotemporal dementia (bvFTD) typically present with lateonset behavioral and personality changes that can be mistaken for psychiatric disorders.1 The earliest behavioral changes include disinhibition, socially inappropriate behavior, poor impulse control, hyperorality, diminishing empathy and increasing apathy.2 These behaviors create a personality that is socially disconnected from other people, shows little concern for any difficulties they cause others, has little insight to the situation and shows poor decision making skills. Many of these patients first show up in a neurologist’s office after shoplifting, losing large amounts of money, being swindled, or other behaviors resulting from diminished executive functioning. Social wisdom has disappeared. The degeneration of these frontoinsular circuits has stripped the patient of his social cognitive abilities. By contrast, memory, language and visuospatial skills are initially spared, and cognitive testing may look reasonably normal despite decreased functionality in daily life. Structurally, the imaging shows focal anterior cingulate cortex (ACC) and orbital frontoinsula (FI) degeneration, especially in the right hemisphere.3 Disinhibition is strongly linked to atrophy in the right orbitalfrontal region and apathy correlates with dysfunction in the right cingulate and medial frontal lobes.4 Alzheimer’s Disease (AD) Typical Alzheimer’s disease (AD) begins with memory problems, including impairment in the learning and retrieving of recently learned information.5 Most AD patients maintain appropriate social behavior maintain the expected eye contact with their loved one in an experimental laboratory environment and can become gentler and sweeter at disease onset.6 These skills help them maintain relationships that help and support them, even if specific identities and the details of the relationship are lost. The personality of a typical AD patient presents as someone who is able to maintain an emotional connection and relationship with someone, even if they cannot tell you who the person is and why they know them. In AD, brain atrophy the posterior hippocampal-cingulo-temporal-parietal network involved in the recall of episodic memory.7 8 Normal Aging Healthy old age brings the growth of emotional control, social flexibility, creativity, wisdom, optimism and resilience. Older adults become more adept at mitigating or avoiding negative emotions by focusing on positive stimuli and a positive interpretation of situations and suppressing reactions to the negative.9 10 Over a 30-day evaluation, older individuals were more likely than younger participants to report never experiencing guilt, shame or hostility within the time period.11 In essence, older adults create stable positive experiences and experience fewer and more transient negative experiences.12 Older adults show a greater increase in prefrontal cortex (PFC) activity than younger adults when viewing emotional stimuli and may recruit a variety of PFC regions (ventromedial, dorsal and lateral) to compensate for any age-related loss in the area when faced with negative stimuli.13 Socially, older adults improve at recognizing emotions when tested with dynamic, naturalistic stimuli (i.e., emotionally laden, unrehearsed, interactions between real married couples).14 This age-related increase in emotion recognition helps older people form stronger social networks for support and enjoyment, which in turn can help promote cognitive and physical wellbeing through lowered blood pressure, stress, and loneliness as well as mental engagement and stimulation. Older adults are also tend for forgive more readily and quickly15, which may further improve their relationships. In support of the common sense that wisdom increases with age, a large, randomly selected sample of older adults showed an increased composite score for wisdom in studies of societal and interpersonal conflict, despite a concurrent age-related decline in Wechsler Adult Intelligence Score IQ.16 These gains seem to occur mainly between 60 and 80 years old. Reciprocal Networks Human brain activity occurs within spatially distinct, functionally related groups of cortical and subcortical regions.17 18 19 20 21 These functional and structural networks can be imaged on fMRI and monitored for change due to activity or disease. Neurodegenerative diseases such as bvFTD and AD disrupt specific, separate networks – leading to the distinct clinical syndromes. AD affects the default mode network involved in episodic memory while FTD interrupts the emotional salience processing network. 22 The AD and FTD circuits also function in a reciprocal fashion. 23 Activity in the frontal circuit inhibits posterior brain regions, while turning on posterior circuits turns off frontal brain regions. This reciprocity provides some insight into the clinical strengths and deficits seen in patients with these diseases. Discussion Neurodegenerative diseases like bvFTD and AD offer insights into how the brain functions due to the selective destruction of specific networks. We see skills diminished in isolation while other skills thrive, based on the connectivity patterns between neurons. These changes raise interesting questions about who we are and what is our capacity for self determination. They also foster compassion, with increased understanding of the patient’s experience and perspective. These networks may be able to serve as early markers of disease and disease progression. Ultimately, these networks may be able to spread therapeutics along a vulnerable track and protect or restore function. Popular culture today tends to idolize youth and fear, even demonize aging. Aging is seen as a process of steady destruction and demise. While yes, there are physical and cognitive challenges associated with aging, this view misses the joys and strengths of aging: improved emotional well-being, improved ability to resolve highly emotional problems like interpersonal conflicts, the accumulation of wisdom and experience, increased resilience to bounce back from difficulties, creativity, generosity and concerns for future generations. These skills are critical to the survival and evolution of human society. Many of our great artists, leaders and humanitarians barely got started until their golden years. Appreciating and finding the appropriate ways for elderly citizens to contribute to a community is a winning strategy for any society. References 1 Woolley JD, Khan BK, Murthy NK, Miller BL, Rankin KP. The diagnostic challenge of psychiatric symptoms in neurodegenerative disease: Rates of and risk factors for prior psychiatric diagnosis in patients with early neurodegenerative disease. J Clin Psychiatry. 2011 Feb;72(2):126-33. 2 Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, van Swieten JC, Seelaar H, Dopper EG, Onyike CU, Hillis AE, Josephs KA, Boeve BF, Kertesz A, Seeley WW, Rankin KP, Johnson JK, Gorno-Tempini ML, Rosen H, Prioleau-Latham CE, Lee A, Kipps CM, Lillo P, Piguet O, Rohrer JD, Rossor MN, Warren JD, Fox NC, Galasko D, Salmon DP, Black SE, Mesulam M, Weintraub S, Dickerson BC, Diehl-Schmid J, Pasquier F, Deramecourt V, Lebert F, Pijnenburg Y, Chow TW, Manes F, Grafman J, Cappa SF, Freedman M, Grossman M, Miller BL. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011 Sep;134(Pt 9):2456-77. 3 Seeley WW, Allman JM, Carlin DA, Crawford RK, Macedo MN, Greicius MD, Dearmond SJ, Miller BL. Divergent social functioning in behavioral variant frontotemporal dementia and Alzheimer disease: reciprocal networks and neuronal evolution. Alzheimer Dis Assoc Disord. 2007 Oct-Dec;21(4):S50-7. 4 Rosen HJ, Allison SC, Schauer GF, Gorno-Tempini ML, Weiner MW, Miller BL. Neuroanatomical correlates of behavioural disorders in dementia. Brain. 2005 Nov;128(Pt 11):2612-25. 5 McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011 May;7(3):263-9. 6 Sturm VE, McCarthy ME, Yun I, Madan A, Yuan JW, Holley SR, Ascher EA, Boxer AL, Miller BL, Levenson RW. Mutual gaze in Alzheimer's disease, frontotemporal and semantic dementia couples. Soc Cogn Affect Neurosci. 2011 Jun;6(3):359-67. 7 Seeley WW, Allman JM, Carlin DA, Crawford RK, Macedo MN, Greicius MD, Dearmond SJ, Miller BL. Divergent social functioning in behavioral variant frontotemporal dementia and Alzheimer disease: reciprocal networks and neuronal evolution. Alzheimer Dis Assoc Disord. 2007 Oct-Dec;21(4):S50-7. Braak H, Braak E. Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiol Aging. 1995 May-Jun;16(3):271-8; discussion 278-84. 8 9 Charles ST. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol Bull. 2010 Nov;136(6):1068-91. 10 Mather M. The emotion paradox in the aging brain. Ann N Y Acad Sci. 2012 Mar;1251:33-49. 11 Hay EL, Diehl M. Emotion complexity and emotion regulation across adulthood. Eur J Ageing. 2011 Sep;8(3):157-168. 12 Carstensen LL, Pasupathi M, Mayr U, Nesselroade JR. Emotional experience in everyday life across the adult life span. J Pers Soc Psychol. 2000 Oct;79(4):644-55. 13 Mather M. The emotion paradox in the aging brain. Ann N Y Acad Sci. 2012 Mar;1251:33-49. 14 Sze JA, Goodkind MS, Gyurak A, Levenson RW. Aging and Emotion Recognition: Not Just a Losing Matter. Psychol Aging. 2012 Jul 23. [Epub ahead of print] 15 Cheng ST, Yim YK. Age differences in forgiveness: the role of future time perspective. Psychol Aging. 2008 Sep;23(3):676-80. 16 Grossmann I, Na J, Varnum ME, Park DC, Kitayama S, Nisbett RE. Reasoning about social conflicts improves into old age. Proc Natl Acad Sci U S A. 2010 Apr 20;107(16):7246-50. 17 Beckmann CF, DeLuca M, Devlin JT, Smith SM. Investigations into resting-state connectivity using independent component analysis. Philos Trans R Soc Lond B Biol Sci. 2005 May 29;360(1457):1001-13. 18 Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, Reiss AL, Greicius MD. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007 Feb 28;27(9):2349-56. 19 Vincent JL, Patel GH, Fox MD, Snyder AZ, Baker JT, Van Essen DC, Zempel JM, Snyder LH, Corbetta M, Raichle ME. Intrinsic functional architecture in the anaesthetized monkey brain. Nature. 2007 May 3;447(7140):83-6. 20 Seeley WW, Crawford RK, Zhou J, Miller BL, Greicius MD. Neurodegenerative diseases target large-scale human brain networks. Neuron. 2009 Apr 16;62(1):42-52. 21 Zhou J, Gennatas ED, Kramer JH, Miller BL, Seeley WW. Predicting regional neurodegeneration from the healthy brain functional connectome. Neuron. 2012 Mar 22;73(6):1216-27. 22 Seeley WW, Crawford RK, Zhou J, Miller BL, Greicius MD. Neurodegenerative diseases target large-scale human brain networks. Neuron. 2009 Apr 16;62(1):42-52. 23 Zhou J, Greicius MD, Gennatas ED, Growdon ME, Jang JY, Rabinovici GD, Kramer JH, Weiner M, Miller BL, Seeley WW. Divergent network connectivity changes in behavioural variant frontotemporal dementia and Alzheimer's disease. Brain. 2010 May; 133(Pt 5):1352-67.