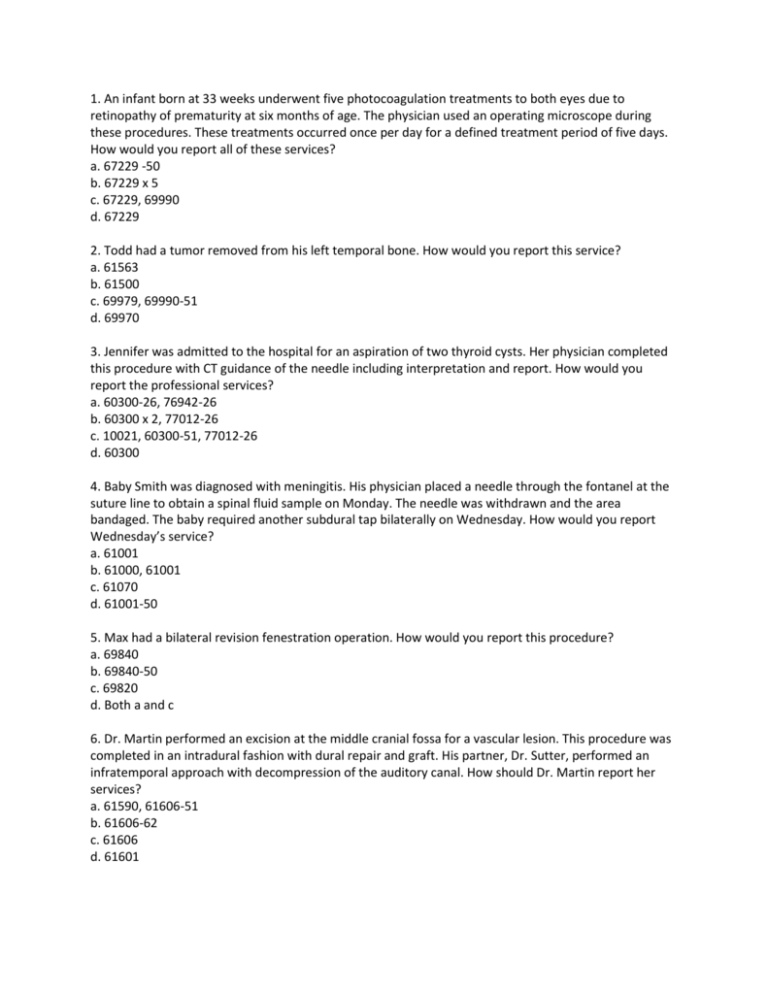
1. An infant born at 33 weeks underwent five photocoagulation treatments to both eyes due to
retinopathy of prematurity at six months of age. The physician used an operating microscope during
these procedures. These treatments occurred once per day for a defined treatment period of five days.
How would you report all of these services?
a. 67229 -50
b. 67229 x 5
c. 67229, 69990
d. 67229
2. Todd had a tumor removed from his left temporal bone. How would you report this service?
a. 61563
b. 61500
c. 69979, 69990-51
d. 69970
3. Jennifer was admitted to the hospital for an aspiration of two thyroid cysts. Her physician completed
this procedure with CT guidance of the needle including interpretation and report. How would you
report the professional services?
a. 60300-26, 76942-26
b. 60300 x 2, 77012-26
c. 10021, 60300-51, 77012-26
d. 60300
4. Baby Smith was diagnosed with meningitis. His physician placed a needle through the fontanel at the
suture line to obtain a spinal fluid sample on Monday. The needle was withdrawn and the area
bandaged. The baby required another subdural tap bilaterally on Wednesday. How would you report
Wednesday’s service?
a. 61001
b. 61000, 61001
c. 61070
d. 61001-50
5. Max had a bilateral revision fenestration operation. How would you report this procedure?
a. 69840
b. 69840-50
c. 69820
d. Both a and c
6. Dr. Martin performed an excision at the middle cranial fossa for a vascular lesion. This procedure was
completed in an intradural fashion with dural repair and graft. His partner, Dr. Sutter, performed an
infratemporal approach with decompression of the auditory canal. How should Dr. Martin report her
services?
a. 61590, 61606-51
b. 61606-62
c. 61606
d. 61601
7. After a snow skiing accident, Barry had a cervical laminoplasty to four vertebral segments. How
should you report this procedure?
a. 63050 x 4
b. 22600, 63051-51
c. 22842, 63045, 63050
d. 63050
8. How is a neuroplasty procedure described in the CPT Professional Edition?
a. The decompression or freeing of intact nerve from scar tissue, including external neurolysis and/or
transposition
b. The surgical repair of nerves using only microscopic techniques
c. The position of nerves tested one or more anatomic digits
d. The decompression or freeing of an intact vein from scar tissue, including external neurolysis and/or
transposition
9. Phyllis fell down on the ice and fractured her leg. The fall also caused severe injury to the muscles and
tore several nerves. Her physician completed suturing of two major peripheral nerves in her leg without
transposition and shortened the bone. After the surgery she was seen by a physical therapist for
ongoing treatment and gait training. How would you report the surgical procedure?
a. 64857, 64859-51, 64876-51
b. 64856, 64857
c. 64857, 64859, 64876
d. 64858, 64857, 64859, 64876
10. John was hospitalized for a repair of a laceration to his left conjunctiva by mobilization and
rearrangement. How should you report this procedure?
a. 65273-LT
b. 67930
c. 65272
d. 67930-LT
11. The patient is a 64-year-old female who is undergoing a removal of a previously implanted
Medtronic pain pump and catheter due to a possible infection. The back was incised; dissection was
carried down to the previously placed catheter. There was evidence of infection with some fat necrosis
in which cultures were taken. The intrathecal portion of the catheter was removed. Next the pump
pocket was opened with evidence of seroma. The pump was dissected from the anterior fascia. A 7-mm
Blake drain was placed in the pump pocket through a stab incision and secured to the skin with
interrupted Prolene. The pump pocket was copiously irrigated with saline and closed in two layers. What
are the CPT and ICD-9-CM codes for this procedure?
A. 62365, 62350-51, 996.75, V53.09
C. 62365, 62355-51, 996.63
B. 62360, 62355, 998.51
D. 36590, 996.75, 998.13
12. The patient is a 73-year-old gentleman who was noted to have progressive gait instability over the
past several months. Magnetic resonance imaging demonstrated a ventriculomegaly. It was
recommended that the patient proceed forward with right frontal ventriculoperitoneal shunt placement
with Codman programmable valve. What is the correct code for this surgery?
A. 62220
B. 62223
C. 62190
D. 62192
13. What is the CPT code for the decompression of the median nerve found in the space in the wrist on
the palmar side?
A. 64704
B. 64713
C. 64721
D. 64719
14. 2-year-old Hispanic male has a chalazion on both upper and lower lid of the right eye. He was placed
under general anesthesia. With an #11 blade the chalazion was incised and a small curette was then
used to retrieve any granulomatous material on both lids. What code should be used for this procedure?
A. 67801
B. 67805
C. 67800
D. 67808
15. MRI reveals patient has cervical stenosis. It was determined he should undergo bilateral cervical
laminectomy at C3 through C6 and fusion. The edges of the laminectomy were then cleaned up with a
Kerrison and foraminotomies were done at C4, C5, and,,C6. The stenosis is central: a facetectomy is
performed by using a burr. Nerve root canals were freed by additional resection of the facet, and
compression of the spinal cord was relieved by removal of a tissue overgrowth around the foramen.
Which CPT codes should be used for this procedure?
A. 63045-50, 63048-50
B. 63020-50, 63035-50, 63035-50
C. 63015-50
D. 63045, 63048 x 3
16. An extracapsular cataract removal is performed on the right eye by manually using an iris expansion
device to expand the pupil. A phacomulsicfication unit was used to remove the nucleus and irrigation
and aspiration was used to remove the residual cortex allowing the insertion of the intraocular lens.
What code should be used for this procedure?
A. 66985
B. 66984
C. 66982
D. 66983
17. An infant who has chronic otitis media was placed under general anesthesia and a radial incision was
made in the posterior quadrant of the left tympanic membrane. A large amount of mucoid effusion was
suctioned and then a ventilating tube was placed in both ears. What CPT and ICD-9-CM codes should be
reported:
A. 69436-50, 381.20
B. 69436-50, 381.4
C. 69433-50, 381.02
D. 69421-50, 381.20
18. A craniectomy is being performed on a patient who has Chiari malformation. Once the posterior
inferior scalp was removed a C-1 and a partial C-2 laminectomy was then performed. The right
cerebellar tonsil was dissected free of the dorsal medulla and a gush of cerebrospinal fluid gave good
decompression of the posterior fossa content. Which CPT code should be used?
A. 61322
B. 61345
C. 61343
D. 61458
19. Under fluoroscopic guidance an injection of a combination of steroid and analgesic agent is
performed on T2-T3, T4-T5, T6-T7 and T8-T9 on the left side into the paravertebral facet joints. The
procedure was performed for pain due to thoracic root lesions. What are the procedure codes?
A. 64479, 64480x3, 77003
B. 64490, 64491, 64492x2, 77003
C. 64520x4, 77003
D. 64490, 64491, 64492
20. An entropian repair is performed on the left lower eyelid in which undermining was performed with
scissors of the inferior lid and inferior temporal region. Deep sutures were used to separate the eyelid
margin outwardly along with stripping the lateral tarsus to provide firm approximation of the lower lid
to the globe. The correct CPT code is:
A. 67914-E4
B. 67924-E2
C. 67921-E2
D. 67917-E1
21. The patient was taken to the procedure room and placed prone and the L4–L5 interspace was
identified using fluoroscopy to determine the injection site. The patient was prepped in routine sterile
fashion with Betadine and covered in sterile drape. 1% lidocaine was used to anesthetize the skin,
subcutaneous tissue, and muscle. Once the proper anesthesia was obtained, a 3 inch, 20 gauge Tuohy
needle was inserted and slowly advanced towards the L4-L5 interspace. Using a 6 cc glass syringe and
the loss-of-resistance technique the epidural space was identified. After aspiration revealed no blood or
cerebrospinal fluid return, the syringes were then changed and 80 mg/ml preservative-free Depo
Medrol and 2 cc of 1% methylparaben free lidocaine were injected in slow incremental fashion. After
aspiration, all needles were removed intact, the skin was cleaned and a Band-Aid was applied. Code this
encounter.
A. 62311
B. 62311, 77003-26
C. 62310, 77003-26
D. 62319, 77003-26
22. A 65-year-old patient presented with ectropion of the right lower eyelid. Repair with tarsal wedge
excision is performed for correction. Attention was then directed to the left eye. The patient also had an
ectropion of the left lower lid which was repaired by suture repair. Code this procedure.
A. 67916-50
B. 67916-E4, 67914-E2
C. 67914-50
D. 67923-E4, 67921-E2
23. A 42-year-old patient returns to the hospital neurology clinic for follow-up. He was checked three
days prior to this visit where a lumbar puncture was done to find the etology of the patient’s headaches.
The headaches have increased in intensity over the past three days. The neurologist examines the
patient and finds a CSF leak from the lumbar puncture. A blood patch by epidural injection is performed
to repair the leak. Code the services for today’s visit.
A. 62272
B. 62273
C. 62270, 62273
D. 62270, 62287
24. A 63-year-old woman presented to the eye clinic as a new patient with symptoms of flashing lights
and floaters in the right eye for two days duration. The ophthalmologist does a general evaluation of the
complete visual system, including dilating her eyes and checking her with the indirect ophthalmoscope,
revealing peripheral retinal tear. The physician explains to the patient that if left untreated, there is a
high likelihood of retinal detachment. The patient agrees to the procedure. The physician lasers the
retinal tear and tells the patient to come back in 24 hours for follow-up. Code this visit.
A. 67210, 92004-25
B. 67145, 92004-25
C. 66821
D. 67145
25. What is the full CPT® code description for 61535?
A. Craniotomy with elevation of bone flap; for subdural implantation of an electrode array, for long-term
seizure monitoring; for removal of epidural or subdural electrode array, without excision of cerebral
tissue (separate procedure)
B. Craniotomy with elevation of bone flap; for removal of epidural or subdural electrode array, without
excision of cerebral tissue (separate procedure)
C. For removal of epidural or subdural electrode array, without excision of cerebral tissue (separate
procedure)
D. For excision of epileptogenic focus without electrocorticography during surgery; ; for removal of
epidural or subdural electrode array, without excision of cerebral tissue (separate procedure)
26. Postoperative Diagnosis: Carpal tunnel syndrome right wrist The patient was brought to the
operating room and sedated by anesthesia. After sterile prepping and draping of the right hand, wrist
and arm the patient’s area of incision was infiltrated with Xylocaine/Marcaine infiltration. After
satisfactory anesthesia an Esmarch bandage was used to exsanguinate the right hand and wrist and used
about the distal forearm as a tourniquet. A curvilinear incision was made on the palmar aspect of the
right wrist. Dissection was carried out through the skin and subcutaneous tissue. Bleeding was
controlled. The median nerve and it branches were identified, retracted, and protected at all times. The
ligament was incised from proximal to distal. A thorough decompression was carried out. A neurolysis
was carried out. The nerve was found to be flattened and ischemic underneath the transverse carpal
ligament. The fascia was closed, the tourniquet was released. A dressing was applied and patient was
transferred to recovery room. Code this procedure.
A. 64721-RT
B. 64450-RT
C. 64614-RT
D. 29848-RT
27. A 35-year-old man presents to the urgent care center with severe neck pain. The physician examines
the patient and makes the diagnosis of cervical nerve impingement and injects an anesthetic agent into
the cervical plexus using three injections. Select the procedure and diagnosis codes.
A. 64400 x 3
B. 64405
C. 64413
D. 64413 x 3
28. A four-year-old with chronic otitis media and fluid buildup in both ears was admitted by her
otolaryngologist for a bilateral tympanostomy. The procedure was performed with placement of
ventilating tubes. The procedure required general anesthetic due to the patient’s age. Select the
procedure code for this procedure.
A. 69420-50
B. 69421-50
C. 69433-50
D. 69436-50
29. A patient presents to the emergency department with complaint of painful eye. The patient states
that her right eye is constantly tearing and is sensitive to light. The physician performs an exam and
identifies a corneal foreign body in the right eye. Utilizing a slit lamp, the foreign body is removed. Code
the encounter.
A. 65205-RT
B. 65220-RT
C. 65222-RT
D. 65435-RT
30. The physician performs a right thyroid lobectomy. The patient was prepped and draped. After
adequate general anesthesia, the neck was incised on the right side and sharp dissection was then used
to cut down onto the strap muscles and sternodcleidomastoid muscles. The strap muscles were
separated and transected on the right side. A small thyroid lobe was visualized and dissected free. There
was no evidence of a tumor. The wound was closed with 3-0 interrupted Vicryl for the platysma, 4-0
Vicryl for the deep tissues and 6-0 fast absorbing gut for the skin. Code the encounter.
A. 60252-RT
B. 60210-RT
C. 60220-RT
D. 60260-RT
31. PROCEDURE: Bilateral lumbar medial branch block under fluoroscopy for the L3, L4, L5 medial
branches for the L4-L5, L5-S/1 facets for diagnostic and therapeutic purposes. PROCEDURE: The patient
was placed in the prone position on the fluoroscopy table and automated blood pressure cuff and pulse
oximeter applied. The skin entry points for approaching the anatomic target points of the bilateral
segmental medial branches or dorsal ramus of L3, L4, L5 were identified with a 22.5 degree from
perpendicular lateral oblique fluoroscopy view and marked. Following thorough Chloraprep preparation
of the skin and draping and 1% lidocaine infiltration of the skin entry points and subcutaneous tissues, a
22 gauge 6" spinal needle was placed under fluoroscopic guidance down on the target point for each
respective segmental medial branch or dorsal ramus. At each point 1 mL consisting of 0.5% bupivacaine
and Depo-Medrol was injected. A total of 80 mg of Depo-Medrol was divided between all six spots. Code
the procedure(s).
A. 64483, 64484, 77003-26
B. 64493-50, 64494-50, 64495-50
C. 64493, 64494, 63395 x 4, 77003-26
D. 64493-50, 64494-50
32. A 43-year-old patient who suffers from severe intermittent vertigo has been definitively diagnosed
with Meniere’s disease. After a year of various treatments, medications, tests, and behavior/lifestyle
changes that have failed to lessen the symptoms, she now presents for a transcanal chemical
labyrinthotomy to the right ear. Dr. Miller visualizes the tympanic membrane with an operating
microscope, cleans the ear canal, and makes a small incision into the tympanic membrane. Gentamicin
is delivered into the right ear. The patient is repositioned with the right ear up and monitored by the
nurse. The perfusion is repeated to achieve the maximum result. The ear is suctioned, cleaned, and
carefully examined for bleeding. The patient tolerated the procedure well and is returned to the
recovery area in satisfactory condition. How would Dr. Miller report his professional services?
a. 386.04, 69801 x 2, 69990-51
b. 386.04, 69905 x 2, 69990-51
c. 386.00, 69801, 69990
d. 386.00, 69905, 69990
33. What code(s) would be reported for the following case?
Preoperative diagnosis: Bilateral impacted ventilating tube
Postoperative diagnosis: Same
Anesthesia: General
Procedure performed: Removal and replacement of new tubes, bilaterally via tympanostomy
Procedure: Sammie, a 16-year-old patient, was admitted and taken to the operative suite and placed
under general anesthesia by inhalation. When adequate sedation was achieved, a 3.8-mm speculum was
inserted into the left ear, wax removed, and speculum removed. The impacted tube was then removed.
A new site was achieved within the same tympanosclerotic plaque and a new tube placed. The same
procedure was repeated to the right ear. Sammie was sent to the recovery suite in stable condition.
a. 69424-50, 69436-50
b. 69433-50
c. 69436-50
d. 69424-50, 69433-50
34. James returned two weeks after surgery, as planned, for a change in his drug delivery system. Today
Dr. Harvey opened the previous incision site. The previously placed reservoir was removed and a new
programmable subcutaneous pump was connected to the catheter and secured with sutures, tested,
and programmed. The subcutaneous incision was closed in layers with a sterile dressing placed. The
patient tolerated the procedure well. How should Dr. Harvey report this service?
a. 62362-58
b. 62365, 62362-59
c. 62350-58
d. 62350, 62355-59
35. Dr. Adams completed an anterior discectomy with decompression including osteophytectomy to
levels C3–C5.During the same session, he stabilized C3–C5 with anterior cervical interbody fusion. For
proper visualization, Dr. Adams used an operating microscope during all phases of the procedure.How
should Dr. Adams report this procedure?
a. 63075, 63078-51, 22551, 22554 x 2, 69990-51
b. 63075, 63078-51, 22551 x 2, 69990-51
c. 63075, 63076, 22554 x 2
d. 63075, 63076, 22551, 22552
36. With which code set or individual codes can add-on code 61781 be correctly reported?
a. 61720–61791
b. 62201 or 77432
c. 77371–77373
d. None of the above
37. Carl, a 28-year-old patient, has a history of epilepsy with recurrent seizures. His seizures are
intolerable even with medication management. He does not experience non-epileptic seizures, which
was confirmed by EEG recordings. Today he underwent an open procedure for implantation of cranial
nerve neurostimulator electrode array, which was coiled around the vagus nerve. The pulse generator
was connected to the neurostimulator array, tested, and repositioned to ensure maximum
effectiveness. The pulse generator was placed and sutured into a created subcutaneous pocket. Again,
the system is tested to ensure proper functionality. The subcutaneous tissues and skin are closed with
deep sutures and skin staples. Carl tolerated the procedure well and was returned to the recovery suite
in stable condition. Which code(s) should be reported for today’s services?
a. 61885, 64568-59
b. 64568
c. 61531
d. 64570, 61888-59, 64568-59
38. A 6-month-old patient required a bilateral subdural tap through a suture. How would this initial
procedure be reported?
a. 61000
b. 61001-63
c. 61000-50
d. 61020-63, 61000-50
39. A patient with Bell’s palsy is unable to squint, blink, or close her left eyelid. To protect the eye, Dr.
Risser completes a temporary tarsorrhaphy with a Frost suture technique. How would you report this
procedure?
a. 67875-LT
b. 67710-LT
c. 67840-LT
d. 67950-LT
40. What code(s) should be reported with the following case?
Preoperative diagnosis: Total retinal detachment, right eye
Postoperative diagnosis: Same
Procedure performed: Complex repair of retinal detachment with photocoagulation, scleral buckle,
sclerotomy/vitrectomy
Anesthesia: Local
Procedure: The patient was placed, prepped, and draped in the usual manner. Adequate local
anesthesia was administered.
The operating microscope was used to visualize the retina, which has fallen into the posterior cavity. The
vitreous was extracted using a VISC to complete the posterior sclerotomy. Minimal scar tissue was
removed to release tension from the choroid. The retina was repositioned and attached using
photocoagulation laser, a gas bubble, and a suture placement of a scleral buckle around the eye. The
positioning of the retina was checked during the procedure to ensure proper alignment. Antibiotic
ointment was applied to the eye prior to placement of a pressure patch. The patient tolerated the
procedure well and returned to the recovery suite in satisfactory condition.
a. 361.05, 67113-RT, 67107-51, 67145-51, 66990-51
b. 361.05, 67113-RT, 69990-RT
c. 361.00, 67113-RT, 66990-RT
d. 361.00, 67113-RT, 67107-51, 67145-51, 66990-51
41. A patient had a bilateral strabismus surgery involving the medial and lateral rectus muscles. The
surgeon explored and repaired a detached extraocular muscle in the right eye and placed bilateral
posterior fixation sutures with muscle recession. How should you report this procedure?
a. 67316-50, 67332-RT, 67334-50
b. 67316-50, 67332-RT, 67335-50
c. 67312-50, 67340-RT, 67334-50
d. 67312-50, 67340-RT, 67335-50
ANSWERS
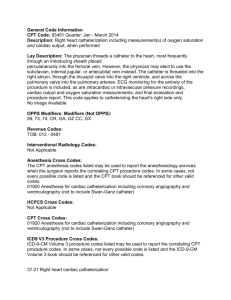
1. “a” The note under Prophylaxis indicate that these services are repetitive, performed in multiple
sessions, and are intended to include all services in a defined treatment period. The parenthetical note
under code 67229 states to use modifier -50 for a bilateral procedure. The operating microscope is
bundled into this procedure. Refer to code 69990 for a list of bundled codes.
2. “d” One way to answer this question is to look in the index of the CPT Professional Edition under the
main heading of Tumor.
3. “b” The professional services for the CT should have a modifier -26. The professional service is the
procedure; therefore, there would be no modifier -26 on code 60300.
4. “a” This question represents a subsequent tap. The code 61000 is reported for an initial procedure.
Modifier -50 is not necessary because it is inherently included in the code description.
5. “b” One way to find this answer is in the index of the CPT Professional Edition under Fenestration
Procedure, Revision. You would attach modifier -50 to indicate a bilateral procedure.
6. “c” Each surgeon should report the work he or she completed. Because Dr. Martin completed the
definitive procedure, use code 61606, which includes the repair and graft.
7. “d” The code 63050 reports two or more vertebral segments, therefore, there is no need to change
the units. You could find this answer by looking in the index of the CPT Professional Edition under
Laminoplasty.
8. “a” You can find this answer by looking up Neuroplasty in the index of the CPT Professional Edition
and reading the definition under the sub-heading.
9. “c” Code 64857 describes suturing of a major peripheral nerve in the leg without transposition. The
add-on code 64859 is used for the second major peripheral nerve. The add-on code 64876 reports the
shortening of the bone.
Add-on codes should not have modifier -51 attached (see Appendix A).
10. “a” The code 65273 is reported for hospitalization. The code 65272 is for without hospitalization.
11. C This was a removal of an intrathecal catheter and pump, eliminating multiple choice answer D. The
pump is not being implanted or replaced eliminating multiple choice answer B. Nor is the intrathecal
catheter being implanted, revised or repositioned eliminating multiple choice answer A. Diagnosis
Rationale: This was a complication; an infection due to a nervous system implant, eliminating multiple
choice answers A and D. Seroma is mentioned in the documentation, but there is an “excludes” note for
code 998.51, for infection due to an implanted device (996.60-996.69), eliminating multiple choice
answer B.
12. B This key word to choose the correct shunt being performed is “ventriculo-peritoneal”, leading you
to multiple choice answer B.
13. C The key term to choose the correct answer is “median nerve”, found in code 64721.
14. D There is more than a single chalazion to be removed, eliminating multiple choice answer C. The
chalazion was on the upper and lower lid, eliminating multiple choice answer A. The patient was under
general anesthesia, eliminating multiple choice answer B.
15. D Laminectomy was performed, eliminating multiple choice answer B. Facetectomy and
foraminotomy were performed, eliminating multiple choice answer C. The laminectomy is performed
bilaterally on three segments of the cervical. Modifier 50 is not appended to code 63045-63048, since
the code descriptive has a parenthetical note indicting that these codes include unilateral or bilateral,
eliminating multiple answer A.
16 C The surgery is an extracapsular cataract removal, eliminating multiple choice D. The removal of the
cataract and the insertion of the lens were performed at the same time, eliminating multiple choice A.
The keyword to choose between codes 66982 and 66984 is “iris expansion device” which was used to
remove the cataract, eliminating multiple choice answer B.
17. A The patient is under general anesthesia eliminating multiple choice answer C. A ventilating tube
was placed in the ears eliminating multiple choice answer D. The diagnosis is indexed in the ICD-9-CM
manual under Otitis/ media/chronic/ mucoid, mucous guiding you to code 381.20, eliminating multiple
choice answer B.
18 C The keywords in this craniectomy procedure to guide you to the correct code are cervical (C-1 and
C-2) laminectomy, medulla, and Chiari malformation found in the code description of code 61343.
19 D The patient is having the injection in the paravertebral facet joints, eliminating multiple choice
answers A and C. The code description for code 64490 has the fluoroscopic guidance included in the
code, meaning that it should not be coded separately. Also there is a parenthetical note under code
64492 that states not to report 64492 more than once per day, eliminating multiple choice answer B.
20 B The procedure being preformed is an entropian repair on the left lower eyelid, eliminating multiple
choice answers A and D. Since there was a tarsal strip performed the procedure is an extensive repair,
eliminating multiple choice C.
21. B.This procedure is being performed in the lumbar which eliminates “C” for the cervical or thoracic.
62311 is the correct procedure code since the patient is getting the meds injected by a syringe not a
continuous infusion by a catheter. 77003 is coded since fluoroscopic guidance was used to place the
needle for the therapeutic injection. Modifier 26 is appended for the professional component, physician
not owning the equipment.
22. B. The key word in this scenario is “ectropion”, which eliminates D for one who has entropion. One
of the eyelids had an excision of the tarsal wedge coded with 67916 and modifier E4 is appended to
indicate the procedure was performed on the right lower lid. The other eyelid had a suture repair coded
with 67914 and modifier E2 is appended to indicate the repair was done on the left lower lid. A different
procedure was performed on each eyelid. Modifier 50 would not be appended to the codes since both
lids did not have the same procedure performed.
23. B .The key word in this encounter is “injection” which eliminates the spinal puncture procedure
codes. 62273 is the correct code for the patient’s blood is injected to plug the wound that is causing the
CSF leak (blood patch). This is the only code to bill for this visit, since the lumbar puncture was
performed three days ago.
24. B. Code 67145 is the correct procedure code since the patient had a retinal tear (retinal break) and
the physician uses a laser light (photocoagulation) to seal the retina back into place. Code 92004 is
coded to report the evaluation of the complete visual field. The patient is new patient. An evaluation of
the eye was performed in addition to performing the procedure. Modifier 25 is appended to the
evaluation code.
25. B.The description for code 61535 is indented which means the description from 61533 up to the
semicolon is the beginning of the full description for 61535.
26. A. The keywords for narrowing your search to the correct code is “carpal tunnel” and “median
nerve,” which is found in the code descriptive of 64721. RT is appended to indicate the surgery is
performed on the right side.
27. C. There was an anesthetic agent injected in the “cervical plexus,” eliminating codes A and B.
Although three injections are performed, only one nerve is involved. It is inappropriate to report
multiple units unless the procedure is performed bilaterally, which in this case it is not.
28. D. A tympanostomy was performed eliminating multiple choice answers A and B. The patient was
under general anesthesia which leads you to procedure code 69436.
29. C. The key terms for this scenario are “Corneal foreign body” removal with a “slit lamp”. This
procedure is reported with 65222. RT is appended to indicate the procedure is performed on the right
eye.
30. C. The patient is having a “thyroid lobectomy,” eliminating multiple choice answers A and D, which is
a thyroidectomy (removal of the thyroid). 60220 is the correct code since the scenario indicates that a
small thyroid lobe (total lobe) is dissected free; it does not indicate that part of the lobe was removed.
31. D. When coding for facet joint or facet joint nerve injections, you report each level that is injected. In
this case, the joints for L4-L5 and L5-S1 were injected. The codes for facet joint and facet joint nerve
injections are unilateral. The procedure was performed bilaterally at each level, therefore modifier 50
should be reported. In the coding guidelines for facet joint injections, it states that fluoroscopic guidance
is included. This service should not be reported separately.
32. c. The patient in this question underwent a labyrinthotomy (incision), not a labyrinthectomy
(excision). Refer to the notes in the CPT® Professional Edition for correct reporting. The parenthetical
notes under code 69801 provide instructions for reporting once per day, and notes provided with the
add-on code for the operating microscope indicate modifier -51 should not be reported with this code.
33. c. Refer to the parenthetical notes with code 69424 in the CPT® Professional Edition for correct
reporting. This code is not reported in conjunction with code 69436. Modifier -50 is reported for a
bilateral procedure.
34. a. One way to find this answer in the index of the CPT® Professional Edition is under “Infusion Pump”
then “Spinal Cord.” This was a planned procedure during a postoperative period; therefore, modifier -58
would be reported. Notice that code 62362 includes the implantation or replacement; therefore, the
removal is included with the replacement of the subcutaneous pump.
35. d. Review the parenthetical notes listed with both the discectomy and arthrodesis codes in the CPT®
Professional Edition; these notes provide code conjunction guidance. According to the inclusion notes
with code 69990, the operating microscope code would not be reported.
36. d. Code 61781 is new for 2011. Review the CPT® Professional Edition parenthetical note under this
code for proper code selection and reporting.
37. b. This was an initial implantation for the neurostimulator array and pulse generator. Code 64568
includes the creation of the skin pocket and testing of the system, according to CPT® Changes: An
Insider’s View 2011.
38. a. This procedure code is described as unilateral or bilateral; therefore, modifier 50 is not required.
Additionally, the description includes an infant and suture site.
39. a. Tarsorrhaphy is used to help patients who are unable to close their eyelids. In patients with Bell’s
palsy (or other conditions that impede the ability to blink or close the eyelids), this procedure keeps the
eyes protected and lubricated until the patient recovers from a paralysis condition.
40. b. Code 67113 includes multiple procedures related to complex repair of a retinal detachment.
These inclusive procedures, if performed, would not be reported separately. The use of the operating
microscope would be reported without a modifier -51.
41. d. The CPT® Professional Edition provides multiple illustrations with strabismus surgery. These
illustrations are helpful for review of anatomic locations of muscles. Codes for strabismus surgery are
selected by the number and type of muscles used during a procedure. Additionally, add-on codes are
provided to help define other conditions or procedures that may be completed at the time of the
surgery.