Liver
advertisement
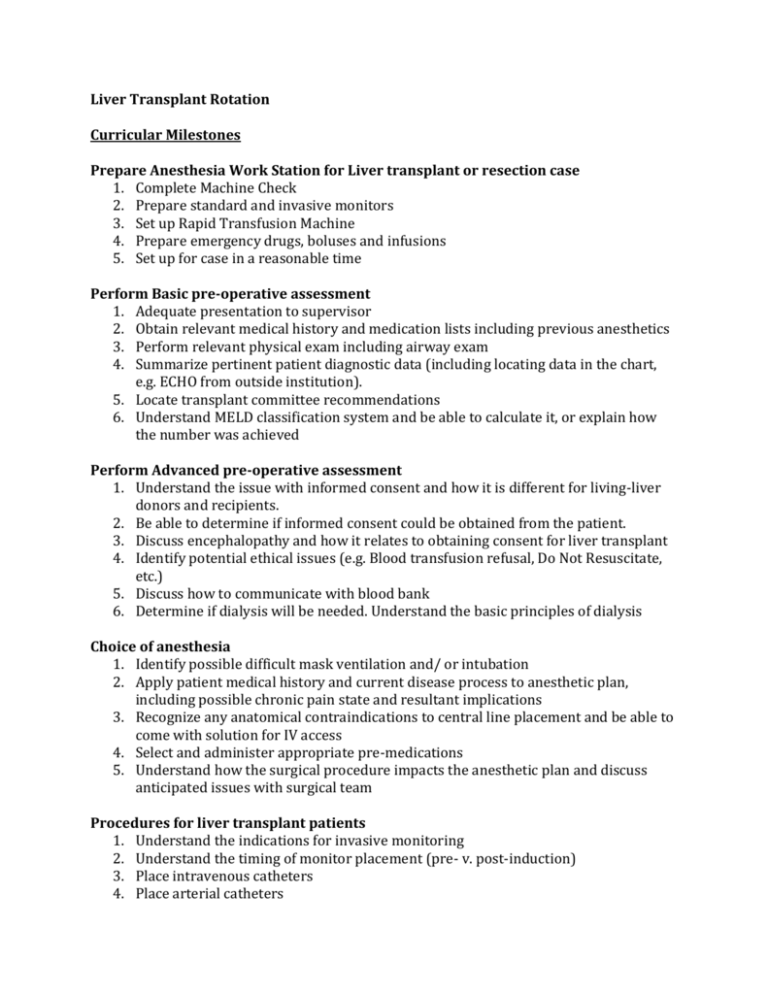
Liver Transplant Rotation Curricular Milestones Prepare Anesthesia Work Station for Liver transplant or resection case 1. Complete Machine Check 2. Prepare standard and invasive monitors 3. Set up Rapid Transfusion Machine 4. Prepare emergency drugs, boluses and infusions 5. Set up for case in a reasonable time Perform Basic pre-operative assessment 1. Adequate presentation to supervisor 2. Obtain relevant medical history and medication lists including previous anesthetics 3. Perform relevant physical exam including airway exam 4. Summarize pertinent patient diagnostic data (including locating data in the chart, e.g. ECHO from outside institution). 5. Locate transplant committee recommendations 6. Understand MELD classification system and be able to calculate it, or explain how the number was achieved Perform Advanced pre-operative assessment 1. Understand the issue with informed consent and how it is different for living-liver donors and recipients. 2. Be able to determine if informed consent could be obtained from the patient. 3. Discuss encephalopathy and how it relates to obtaining consent for liver transplant 4. Identify potential ethical issues (e.g. Blood transfusion refusal, Do Not Resuscitate, etc.) 5. Discuss how to communicate with blood bank 6. Determine if dialysis will be needed. Understand the basic principles of dialysis Choice of anesthesia 1. Identify possible difficult mask ventilation and/ or intubation 2. Apply patient medical history and current disease process to anesthetic plan, including possible chronic pain state and resultant implications 3. Recognize any anatomical contraindications to central line placement and be able to come with solution for IV access 4. Select and administer appropriate pre-medications 5. Understand how the surgical procedure impacts the anesthetic plan and discuss anticipated issues with surgical team Procedures for liver transplant patients 1. Understand the indications for invasive monitoring 2. Understand the timing of monitor placement (pre- v. post-induction) 3. Place intravenous catheters 4. Place arterial catheters 5. Place central venous catheters 6. Placement of basic neuraxial and regional anesthetic techniques (epidural) – for liver resection cases 7. Understands prioritization of procedure completion in context of efficient case start 8. Place dialysis catheter Manage induction of general anesthesia 1. Application of standard monitors (Including pre-induction advance monitoring) 2. Choice of appropriate induction method and agents 3. Understand the timing of monitor placement (pre- v. post-induction Basic Airway management 1. Ventilate lungs via mask or discuss why rapid sequence induction is needed 2. Intubate trachea of patients with easy to moderately difficult airways 3. Choose appropriate Endotracheal Tube 4. Recognize situations appropriate for airway adjuncts, video laryngoscope and / or FOB Preparation of back-up airway devices Advanced Airway Management 1. Recognize need for advanced airway devices 2. Able to successfully use video laryngoscope 3. Able to perform asleep FOI 4. Recognize need for, and utilize airway introducers (i.e. Eschmann) Maintenance of anesthesia - Basic 1. Understand the pharmacology of commonly used anesthetic drugs and their appropriate doses 2. Discuss antibiotic prophylaxis regimen 3. Accurately estimate fluid requirements choose appropriate fluids. 4. Accurately estimate allowable blood loss and need for transfusion 5. Participate in patient positioning 6. Sustain an adequate plane of anesthesia 7. Understand the management of body temperature and maintain normothermia as appropriate 8. Accurately chart in the anesthetic record 9. Maintain appropriate contact with supervising staff Maintenance of anesthesia - Advanced 1. Understand various stages of liver transplantation procedure and what are appropriate interventions for each stage are 2. Be able to anticipate the key issues with each stage of liver transplantation procedure 3. Recognize need for and select appropriate vasoactive medication infusion 4. Understand the need for Transesophageal Echo and when is it most appropriate to use Coordinate within operating room environment 1. Perform timely room turnover between cases 2. Utilize anesthesia technicians and pharmacy staff as appropriate 3. Maintain accurate records of controlled substance administration 4. Arrange transfer of patients to and from the intensive care unit Management of unanticipated intraoperative events/ peri-anesthetic complications (crisis management) 1. Identify, formulate a differential diagnosis, and treat basic intraoperative problems (hypo/hypertension, hypoventilation, hypoxemia, hypercapnia, oliguria, arrhythmias) 2. Understand physiology of significant cardiovascular events (compression of vena cava by surgeons, hypovolemia, hypervolemia, pulmonary embolism, ischemia, myocardial depression) 3. Understand what is meant by “reperfusion syndrome” and steps in managing it. 4. Have familiarity with ACLS guidelines and be able to apply them to OR situations 5. Be able to communicate with surgeons and OR nurses if critical situation arises 6. Maintain appropriate contact with supervising staff 7. Recognize when patients require change in post-surgical disposition (e.g. ICU monitoring, continued artificial airway +/- mechanical ventilation) and communicate this to supervising staff as well as surgical and OR nursing team 8. Provide hand-off to ICU staff in cases where patients are taken directly to ICU postop Emergence and PACU care 1. Prepare the patient for emergence from anesthesia 2. Understand criteria for extubation and apply them appropriately to patient 3. Transfer the patient to the PACU and provide smooth transition to the PACU staff 4. Provide complete and detailed handoff and contact information to PACU staff 5. Manage common postoperative problems (pain, nausea, confusion, hemodynamics, ventilation) 6. Perform post-operative patient visits as appropriate






