LRI Pilots SNOMED LOINC OID UCUM Summary
advertisement
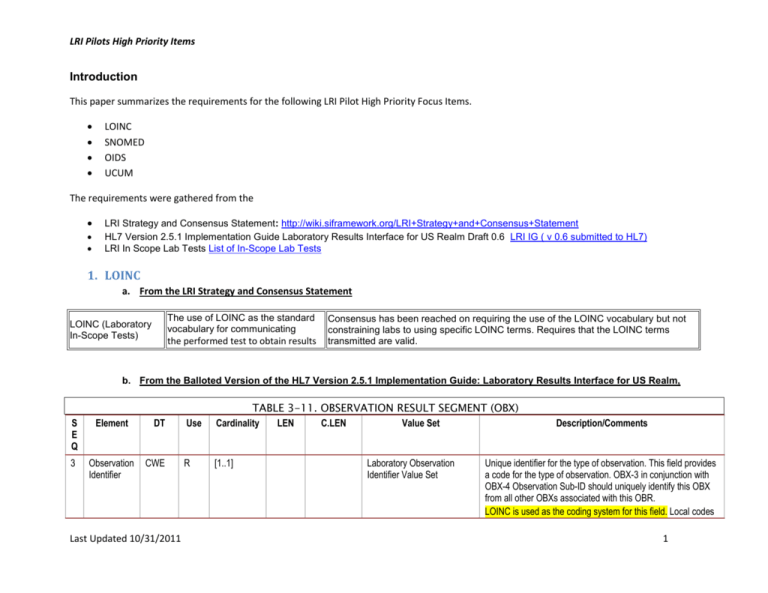
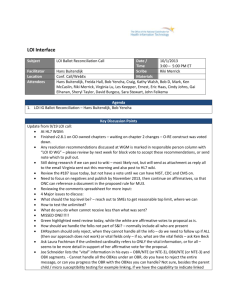
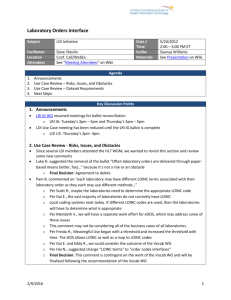
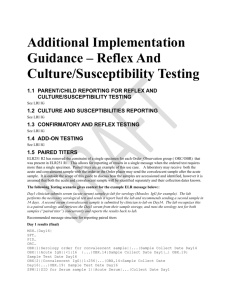
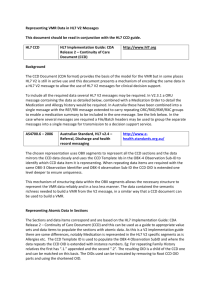
LRI Pilots High Priority Items Introduction This paper summarizes the requirements for the following LRI Pilot High Priority Focus Items. LOINC SNOMED OIDS UCUM The requirements were gathered from the LRI Strategy and Consensus Statement: http://wiki.siframework.org/LRI+Strategy+and+Consensus+Statement HL7 Version 2.5.1 Implementation Guide Laboratory Results Interface for US Realm Draft 0.6 LRI IG ( v 0.6 submitted to HL7) LRI In Scope Lab Tests List of In-Scope Lab Tests 1. LOINC a. From the LRI Strategy and Consensus Statement The use of LOINC as the standard vocabulary for communicating LOINC (Laboratory In-Scope Tests) the performed test to obtain results Consensus has been reached on requiring the use of the LOINC vocabulary but not constraining labs to using specific LOINC terms. Requires that the LOINC terms transmitted are valid. b. From the Balloted Version of the HL7 Version 2.5.1 Implementation Guide: Laboratory Results Interface for US Realm, S E Q Element 3 Observation Identifier DT CWE Last Updated 10/31/2011 Use TABLE 3-11. OBSERVATION RESULT SEGMENT (OBX) Cardinality LEN C.LEN Value Set R [1..1] Laboratory Observation Identifier Value Set Description/Comments Unique identifier for the type of observation. This field provides a code for the type of observation. OBX-3 in conjunction with OBX-4 Observation Sub-ID should uniquely identify this OBX from all other OBXs associated with this OBR. LOINC is used as the coding system for this field. Local codes 1 LRI Pilots High Priority Items may also be used in conjunction with LOINC codes When populating this field with values, this guide does not give preference to the triplet in which the standard (LOINC) code should appear. .3.12.1 OBSERVATION IDENTIFIERS, OBSERVATION VALUES, INTERPRETATIONS AND COMMENTS Laboratory results fall into several broad categories or types of results. The first type of result is a quantitative measure of some property of a specimen and is typically numerical in nature. Often these numeric results are also associated with some sort of interpretation, typically in terms of the normality or abnormality of the measured quantity in relationship to a reference range or normal range. Another type of result is a qualitative result related to the testing of a specimen. This is typically coded or textual in nature. Qualitative results may actually be interpretations of more detailed quantitative measurement. Finally, both quantitative and qualitative results may have comments associated with them. These comments may provide additional clarification, information regarding how the result was obtained, etc. How a particular result should be reported using the OBX segment above depends upon what is being used as an observation identifier for OBX-3. This guide assumes that LOINC is normally being used for the identification of observations. LOINC identifiers can easily be classified as quantitative or qualitative. The LOINC scale property QN (quantitative) indicates that the LOINC identifier is quantitative. All other LOINC identifiers can be treated as qualitative for the purpose of this discussion. Those OBX’s associated with quantitative LOINC identifiers should be using OBX-5 with either the NM (numeric), SN (structured numeric), TS (timestamp), DT (date) or TM (time) data types. These quantitative results can be accompanied by an interpretation. Coded interpretations should be reported using OBX-8 (abnormal flags) when the values have been drawn from HL7 table 0078. When a coded interpretation is sent, or when a textual interpretation is sent, a second OBX using a non-quantitative LOINC identifier should be used. c. From The Vocabulary Workgroup In-Scope Test List Example Entries Target Propose d category Test componen t / scale / time Methods ACLA Creatinin e Panel Chemistr y Collection duration of urine methodles s Last Updated 10/31/2011 Test Descriptio n Specimen Exampl e LOINC Codes SHORTNAM E Urine 13362-9 Collect duration Time Ur LONG COMMON NAME Sample Values/unit s Status Targete d Format (A1, A2, A3, A4, B1, B2, B3, B4) Collection duration of Urine 2 LRI Pilots High Priority Items in 24 hour Urine ACLA Creatinin e Panel in 24 hour Urine Chemistr y Creatinine methodles s Urine 2161-8 Creat UrmCnc Creatinine [Mass/volume ] in Urine mg/dL Added to flesh out top three hundre d d. Questions What are the problems with using the Example LOINC Codes from the In Scope Test List or your own lab’s LOINC code in OBX3? 2. SNOMED a. From the LRI Strategy and Consensus Statement SNOMED The use of SNOMED as a controlled vocabulary SNOMED is considered to be a viable vocabulary option for CWE data types but needs to be confirmed by pilot testing. b. From the Balloted Version of the HL7 Version 2.5.1 Implementation Guide: Laboratory Results Interface for US Realm, 4.4 SNOMED CT SNOMED CT is a required vocabulary for communicating coded results when reported as Coded With Exception (CWE) data types in OBX.5 for specific result categories as defined below. It is also recommended for specimen source terms in SPM.4. 4.6 VOCABULARY CONSTRAINTS Laboratory Coded Observation Value Set For specific result categories: Organisms Last Updated 10/31/2011 3 LRI Pilots High Priority Items Identify using codes from the SNOMED CT “organism” hierarchy o This will normally exclude the use of codes from the “clinical finding” hierarchy representing the presence of a specific organism (e.g., "312210001^methicillin resistant staphylococcus aureus positive^SCT”, "431256002^culture positive for vancomycin resistant enterococcus^SCT”, "441070005^Human enterovirus present^SCT”). However, in some cases a specific absence finding may be appropriate (e.g., "404520004^no Chlamydia trachomatis found^SCT”). Organism-related substances (e.g. toxin, DNA, RNA, antigen, antibody, etc.) Identify using codes from the SNOMED CT “substance” hierarchy (e.g., "12671002^Clostridium difficile toxin^SCT”, "121181000^Chlamydia trachomatis DNA^SCT”, "121006005^influenza virus A antigen^SCT”) o This will normally exclude the use of codes from the “clinical finding” hierarchy representing the presence of a specific organismrelated substance (e.g., "310541005^Clostridium difficile toxin A detected^SCT”). Currently (as of the January 2011 release) we are not aware of any SNOMED CT codes representing the absence of an organism-related substance. Presence and absence findings Identify using codes from the SNOMED CT “qualifier value" hierarchy (e.g., "52101004^present^SCT”, "10828004^positive^SCT”, "2667000^absent^SCT”, "260385009^negative^SCT”) Anatomic Pathology Use of SNOMED CT codes is recommended, but further evaluation is needed to determine which hierarchies are appropriate for use o The NAACCR examples list "abnormal morphology" codes Clinical genomics and additional clinical areas Consider whether other vocabularies in addition to, or in place of, SNOMED CT might apply TABLE 3-12. OBSERVATION IDENTIFIERS Testing Situation Discussion Conveys ordinal value and interpretation Last Updated 10/31/2011 OBX.2 Observatio n Type OBX.3 Observatio n Identifier : LOINC part = scale OBX.5 Observatio n value OBX.6 Units CWE ORD Ordinal as a code. SNOMED CT shall be used when code exists; otherwise a local code. Sending [empty] OBX.8 Abnormal Flags May be populated with codes from HL7 table 0078 OBX.7 Reference Range May be populated NTE Segment May be populated with comments, not clinical findings 4 LRI Pilots High Priority Items ordinals as codes is the preferred ELR approach. Conveys observation and interpretation CWE NOM Coded observation. SNOMED CT shall be used when code exists; otherwise it’s a local code. [empty] May be populated with codes from HL7 table 0078 May be populated May be populated with comments, not clinical findings. c. Questions What are the problems including SNOMED Codes in OBX.5 for OBX.2 CWE Values? 3. OIDS a. From the LRI Strategy and Consensus Statement OIDs The usage of OIDs by clinical laboratories, and a discussion of the policy The LRI workgroups will develop a 12-24 month roadmap that and technology issues surrounding the usage of OID's focuses on OID piloting and future implementation b. From the Balloted Version of the HL7 Version 2.5.1 Implementation Guide: Laboratory Results Interface for US Realm, .5.6 Conformance to this Guide Conformance to this guide is through the use of a combination of OIDs in MSH-21 as noted below: Base Profile LRI R1 – ID: 2.16.840.1.113883.9.16 Indicates that the message adheres to the rules set out in this guide. When this profile is present in MSH.21, it shall be accompanied by one of Profile GU or Profile NG and one of Profile RU or Profile RN. Additionally, other profiles may be present that further constrain the message as agreed to by two or more exchange parties. However, those profiles are strictly voluntary and shall not conflict with any of the three profiles already listed, nor shall any additional profile be marked by any exchange party as minimally required to successfully send or receive Lab Results when Profile LRI is present in MSH.21. Last Updated 10/31/2011 5 LRI Pilots High Priority Items Profile GU – ID: 2.16.840.1.113883.9.12 Indicates Globally Unique Identifiers are supported via required use of an ISO OID as noted in this guide. Profile NG – ID: 2.16.840.1.113883.9.13 Indicates Non-Global Identifiers (Profile NG) were constructed using an alternate method for providing strong identifiers noted in this guide; these identifiers are not guaranteed to be globally unique. Profile RU –ID: 2.16.840.1.113883.9.14 Indicates that the test can be identified by only using either the placer order number, and/or filler order number. Profile RN – ID: 2.16.840.1.113883.9.15 Indicates that the test can be identified by using the universal service identifier and either the placer order number or the filler order number. The Profiles GU and NG are mutually exclusive, as are RU and RN; allowable combinations: Base + GU + RU Base + GU + RN Base + NG + RU Base + NG + RN Profiles GU and RN require the Use of OIDS. What do these require? GU requires OIDS for Assigning Authorities and Facilities in PID.3 – Patient Identifier List PID.18 – Patient Account Number PID.21 – Mother’s Identifier NK1.12 - Next of Kin / Associated Parties Employee Number NK1.33 - Next of Kin/Associated Party’s Identifiers PV1.5 – Preadmit Number PV1.19 – Visit Number PV1.50 – Alternate Visit ID MSH.21 – Message Profile Identifier Last Updated 10/31/2011 6 LRI Pilots High Priority Items ORC.2 – Placer Order Number ORC.3 – Filler Order Number ORC.4 – Placer Group Number OBR.2 – Placer Order Number OBR.3 – Filler Order Number OBX.18 – Equipment Instance Identifier ORC.8 – Parent OBR.29 – Parent SPM.2 – Specimen Identifier SPM.3 – Specimen Parent IDs MSH.3 – Sending Application MSH.4 – Sending Facility MSH.5 – Receiving Application MSH.6 – Receiving Facility MSH.34 – Last Update Facility FSH.3 – File Sending Application FSH.4 – File Sending Facility FSH.5 – File Receiving Application FSH.6 – File Receiving Facility BHS.3 – Batch Sending Application BHS.4 – Batch Sending Facility BHS.5 – Batch Receiving Application BHS.6 – Batch Receiving Facility PV1.7 – Attending Doctor PV1.8 – Referring Doctor PV1.9 – Consulting Doctor PV1.17 – Admitting Doctor PV1.52 – Other Healthcare Provider PV2.13 – Referral Source Code ORC.10 – Entered By ORC.11 – Verified By Last Updated 10/31/2011 7 LRI Pilots High Priority Items ORC.12 – Ordering Provider ORC.19 – Action By OBR.10 – Collector Identifier OBR.16 – Ordering Provider OBR.28 – Result Copies To OBX.16 – Responsible Observer OBX.25 – Performing Organization Medical Director SFT.1 – Software Vendor Organization NK1.13 – Organization Name PV2.23 – Clinic Organization Name ORC.21 - Ordering Facility Name OBR.23 – Performing Organization Name RN requires OIDs for ORC.2 – Order Place Number or OBR.2 Placer Order Number} + OBR.4 – Universal Service Identifier ORC.3 – Filler Order Number or OBR.3 – Filler Order Number} + OBR.4 – Universal Service Identifier OBR.29 – Parent + OBR.50 – Parent Universal Service Identifier ORC.8 – Parent or OBR.29 – Parent} + OBR.50 – Parent Universal Service Identifier c. Questions What are the problems with using implementing Profile GU? What are the problems with implementing Profile RN? 4. UCUM a. From the LRI Strategy and Consensus Statement UCUM Suitability of UCUM as the standard for units of measure to be used as The LRI workgroups will develop a 12-24 month roadmap that part of a laboratory reporting implementation guide focuses on UCUM piloting and future implementation b. From the Balloted Version of the HL7 Version 2.5.1 Implementation Guide: Laboratory Results Interface for US Realm, Last Updated 10/31/2011 8 LRI Pilots High Priority Items Identifies UCUM Units of Measure to be used in TQ1.2 Quantity; TQ1.5 Relative Time and Units; TQ1.6 Service Duration; TQ1.13 Occurrence Duration. All fields that have the TQ1 data type are deprecated. OBX.6 Units - Usage C(R/RE) with a CWE data type and Cardinality 0..1.. Units of Measure are only required for 2 data types. The following table gives examples of how the different fields in the OBX segment interact to create the complete observation TABLE 3-12. OBSERVATION IDENTIFIERS Testing Situation Discussion OBX.2 OBX.3 OBX.5 OBX.6 Units OBX.8 OBX.7 NTE Observation Observation Observation Abnormal Reference Segment Type Identifier: value Flags Range LOINC part = scale Numeric result along with NM QN number May be May be May be May be interpretation populated populated populated populated with UCUM with codes with Units from HL7 comments, table 0078 not clinical findings. Numerical intervals, ratios, inequalities SN QN structured numeric May be populated with UCUM Units May be populated with codes from HL7 table 0078 May be populated May be populated with comments, not clinical findings. Time like quantitative result with interpretation TS, TM, DT QN timestamp, time or date [empty] May be populated with codes from HL7 table 0078 May be populated May be populated with comments, not clinical findings. c. Questions 1. What are the problems with using UCUM Units of Measure in OBX6 for OBX2 NM and SN values? Last Updated 10/31/2011 9