MEDICAL STAFF RULES & REGULATIONS, r 5/97
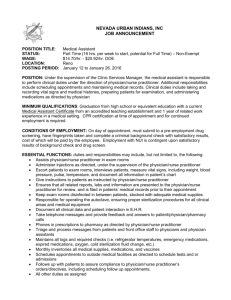
advertisement

FRANKLIN MEMORIAL HOSPITAL MEDICAL STAFF RULES & REGULATIONS Revised by: Medical Staff: April 4, 2011 FMH Board of Trustee: April 26, 2011 Proposed Changes to the FMH Medical Staff Rules & Regulations MEDICAL STAFF RULES & REGULATIONS TABLE OF CONTENTS A. ADMISSION AND DISCHARGE OF PATIENTS ........................................................................................... 3 B. MEDICAL RECORDS .................................................................................................................................... 5 C. GENERAL CONDUCT OF CARE .................................................................................................................. 8 D. GENERAL RULES REGARDING SURGICAL CARE ................................................................................... 11 E. EMERGENCY SERVICES............................................................................................................................ 14 F. INTENSIVE CARE UNIT .............................................................................................................................. 15 G. CLINICAL SERVICE ..................................................................................................................................... 15 H. HEALTH PROFESSION STUDENTS ........................................................................................................... 16 I INTERN AND RESIDENT DOCTORS OF MEDICINE OR OSTEOPATHY.................................................. 16 J. MOONLIGHTING RESIDENTS .................................................................................................................... 17 K. EMERGENCY MEDICAL TECHNICIANS .................................................................................................... 18 2 Proposed Changes to the FMH Medical Staff Rules & Regulations MEDICAL STAFF RULES & REGULATIONS A. ADMISSION AND DISCHARGE OF PATIENTS 1. The hospital shall accept all medical and surgical patients for admitting as per paragraph two below. 2. Only a member of the medical staff may admit a patient to the hospital, except for special situations as outlined in the Bylaws. All practitioners shall be governed by the official admitting policy of the hospital. 3. A member of the medical staff shall be responsible for the medical care and treatment of each patient in the hospital, for the prompt completeness and accuracy of the medical record, for necessary special instructions, and for transmitting reports of the condition of the patient to the referring practitioner and to relatives of the patient where permitted by state and federal law (HIPPA). Whenever these responsibilities are transferred to another staff member of another practice, a note covering the transfer of responsibility shall be entered on the order sheet of the medical record. 4. Except in an emergency, no patient shall be admitted to the hospital until provisional diagnosis or valid reason for admission has been stated. In the case of an emergency such statement shall be recorded as soon as possible. 5. In an emergency case in which it appears the patient will have to be admitted to the hospital, the practitioner shall when possible, first contact the admitting office to ascertain whether there is an available bed. 6. Practitioners admitting emergency cases shall be prepared to justify to the executive committee of the medical staff and the administration of the hospital that the said emergency admission was a bona fide emergency. The history and physical examination must clearly justify the patient being admitted on an emergency basis and these findings must be recorded on the patient's chart as soon as possible after admission. 7. A patient needing admission on an emergency basis who does not have a practitioner on staff may select any practitioner who agrees to so serve in the applicable service to attend to him. Where no such selection is made, a member of the active or provisional staff on duty in that service will be assigned to the patient, on a rotation basis, where possible. The chief of each service shall provide a schedule for such assignments. 8. The chief admitting clerk will schedule patients for admission on the basis of the following order of priorities: a) Emergency Admissions. Adequate documentation will be made within 48 hours of such an admission 3 Proposed Changes to the FMH Medical Staff Rules & Regulations b) Pre-Operative Admissions. This includes all patients already scheduled for surgery. If it is not possible to handle all such admissions, the chief of the surgical service may decide the urgency of any specific admission. c) Routine Admissions. This will include elective admissions involving all services. 9. Patient Transfers. Transfer priorities shall be as follows: a) Emergency Room to appropriate patient bed b) From obstetric patient care area (unit) to general care area, when medically indicated. c) From intensive care unit to post coronary care or general care area. d) From temporary placement in an inappropriate geographical or clinical service area to the appropriate area for that patient. No patient will be transferred without such transfer being approved by the responsible practitioner. 10. The admitting practitioner shall be held responsible for giving such information as may be necessary to assure the protection of the patient from self harm and to assure the protection of others whenever his/her patients might be a source of danger from any cause whatever. 11 Admission to Intensive Care Units If any question as to the validity of admission to or discharge from the intensive care unit should arise, that decision is to be made through consultation with the chairman of ICU or his/her designate. 12 Utilization a) The attending practitioner is required to document the need for continued hospitalization after specific periods of stay as identified by the utilization reviewers of this hospital, and approved by the executive committee of the medical staff. This document must contain: 1. An adequate written record of the reason for continued hospitalization. A simple reconfirmation of the patient's diagnosis is not sufficient. 2. Plans for post-hospital care. b) Upon request of the reviewers dealing with utilization, the attending practitioner must provide written justification of the necessity for continued hospitalization of any patient. This report must be submitted within one working day of receipt of such request. c) Failure of compliance with this policy will be brought to the attention of the executive committee for action. 13. A patient shall be discharged only on a written order of the attending practitioner. Should a patient leave the hospital against the advice of the attending practitioner or without proper discharge, a notation of the incident shall be made in the patient’s medical record. 4 Proposed Changes to the FMH Medical Staff Rules & Regulations A. Admission & Discharge of Patients 14. In the event of a hospital death, the deceased shall be pronounced dead by the attending practitioner or his/her designee within a reasonable time. The body shall not be released until an entry has been made and signed in the medical record of the deceased by a member of the medical staff or a member of the AHP staff. Exceptions shall be made in those instances of incontrovertible and irreversible terminal disease wherein the patient's course has been adequately documented to within a few hours of death. Policies with respect to release of dead bodies shall conform to state law. 15. It shall be the duty of all staff members to seek to determine if an autopsy is appropriate in any case of unusual deaths and of medical-legal and educational interest, and informs the medical staff (specifically the attending physician) of any autopsy that the hospital intends to perform..1 An autopsy may be performed only with a written consent, signed in accordance with state law or as authorized by the office of the Chief Medical Examiner in the case of a death coming within the purview of that office. (Also see C. 12 for obligations regarding autopsies. All autopsies shall be performed by the hospital pathologist or by a practitioner delegated this responsibility. Provisional anatomic diagnoses shall be recorded on the medical record within two working days and the complete protocol should be made part of the record within 3 months.2 B. MEDICAL RECORDS 1. The attending practitioner shall be responsible for the preparation of a complete and legible medical record for each patient. Its contents shall be pertinent and current. This record shall include identification data; complaint; personal history; family history; history of present illness; physical examination; special reports such as consultations, clinical laboratory and radiology services, and others; provisional diagnosis; medical or surgical treatment; operative report; pathological findings; progress notes; final diagnosis; condition on discharge; summary or discharge note (clinical resume); discharge instructions and follow-up plans; and autopsy report when performed. 2. A complete admission history and physical examination shall be recorded within 24 hours of an inpatient admission, for patients held for extended observation over 12 hours or for any patient on whom an operating room procedure is performed. This report shall include all pertinent findings resulting from an assessment of all the systems of the body. If a complete history has been 1 2 §482.22(d) College of American Pathologists, ANP.33100 5 Proposed Changes to the FMH Medical Staff Rules & Regulations recorded and a physical examination performed within 30 days of the patient's admission to the hospital, or prior to the observation period or operating room procedure, a reasonably durable, legible copy of these reports may be used in the patient's hospital medical record in lieu of the admission history and report of the physical examination, provided these reports were recorded by a member of the medical staff or are countersigned consistent with the provisions in subsection 4, below. In such instances, when the medical history and physical examination are completed within 30 days prior to registration or inpatient admission, an update documenting any changes in the patient’s condition is completed within 24 hours after registration or inpatient admission, but prior to surgery or a procedure requiring anesthesia services.3 The update must include all additions to the history, any subsequent changes in the physical findings or patient condition, and any changes to the patient assessment and care plans. The medical history and physical examination are completed and documented by a physician, an oral maxillofacial surgeon, or other qualified licensed individual in accordance with state law and hospital policy.4 3. When the history and physical examination or update are not recorded before an operation or any potentially hazardous diagnostic procedure, the procedure shall be canceled, unless the attending physician states in writing that such delay would be detrimental to the patient. 4. The attending physician shall countersign (authenticate) the history, physical examination and preoperative note when they have been recorded by an individual other than a member of the medical staff. The attending physician is required to countersign only those portions of the history and physical or preoperative note that he did not prepare. 5. Pertinent progress notes shall be recorded at the time of observation, sufficient to permit continuity and transferability of care. Wherever possible, each of the patient's problems should be clearly identified in the progress notes and correlated with specific orders as well as results of tests and treatment. Progress notes shall be written daily on all patients unless they are awaiting nursing home placement or are at SNF level. 3 4 MS.03.01.01 §482.22 (c)(5)(i) / MS.01.01.01 6 Proposed Changes to the FMH Medical Staff Rules & Regulations 6. A full operative report is entered into the medical record upon completion of any operation or high-risk procedure. For the purposes of this section, entered means to be made available for immediate review. The full operative report is entered prior to transferring the patient to the next level of care unless the provider accompanies that patient to that level of care. The full operative report is then entered at that level of care. If the full operative report cannot be entered at that time, then a brief operative note is entered into the medical record. Both the full operative report and a brief operative note contain the following minimal information; the name of the surgeon and assistant, procedure performed procedure findings, estimated blood loss, specimens removed, and postoperative diagnosis. The full operative report shall include a detailed account of the findings at surgery as well as the details of the surgical technique and may be written or dictated. The full operative narrative report is dictated or written within 24 hours of the procedure in cases where a brief operative note was entered immediately following the procedure. 7. Consultations shall show evidence of a review of the patient's record by the consultant, pertinent findings on examination of the patient, the consultant's opinion and recommendations. This report shall within 24 hours be made a part of the patient's record, in order to be available to the physician or other care providers to use in making assessments of the patient’s condition, to justify treatment or continued hospitalization to support or revise the patients’ diagnosis, to support or revised the plan of care, to describe the patients’ progress and to describe the patient’s response to medications, treatments or services. 8. The current obstetrical record shall include a complete prenatal record. The prenatal record may be a legible copy of the attending practitioner's office record transferred to the hospital before admission, but an interval admission note must be written that includes pertinent additions to the history and any subsequent changes in the physical findings. 9. All clinical entries in the patient's medical record shall be authenticated and bear the date, and time of entry. Identification of the author may be by written signature, initials, computer key or other code. 10. Symbols and abbreviations may be used only when they have been approved by the medical staff. An official record of approved abbreviations shall be kept on file in the record room. 11. A discharge summary (clinical resume) shall be written or dictated within 15 days of discharge on all medical records of patients hospitalized. In all instances, the content of the medical record shall be sufficient to justify the diagnosis and warrant the treatment and end results. All summaries shall be authenticated by the responsible practitioner. 7 Proposed Changes to the FMH Medical Staff Rules & Regulations 12. Written consent of the patient is required for release of personally identifiable medical information to persons not otherwise authorized by state or federal law (HIPPA) to receive this information. 13. Records may be removed from the hospital's jurisdiction and safekeeping only in accordance with a court order, subpoena, or statute. All records are the property of the hospital and shall not otherwise be taken away without permission of the chief executive officer. In case of re-admission of a patient, all previous records shall be available for the use of the attending practitioner. This shall apply whether the patient is attended by the same practitioner or by another. Unauthorized removal of charts from the hospital is grounds for suspension of the practitioner for a period to be determined by the executive committee of the medical staff. 14. Free access to all medical records of all patients shall be afforded to members of the medical staff for bona fide study and research consistent with preserving the confidentiality of personal information concerning the individual patients. All such projects shall be approved by the executive committee of the medical staff before records can be studied. Subject to the discretion of the chief executive officer, former members of the medical staff shall be permitted free access to information from the medical records of their patients covering all periods during which they attended such patients in the hospital. 15. A medical record shall not be permanently filed until it is completed by the responsible practitioner or is ordered filed by the medical records committee. 16. A practitioner's routine standing orders, when applicable to a given patient, shall be reproduced in detail on the order sheet of the patient's record, dated, timed and signed by the practitioner. 17. The patient's medical record shall be complete at time of discharge, including progress notes, final diagnosis and dictated clinical resume. Where this is not possible because final laboratory or other essential reports have not been received at the time of discharge, the patient's chart will be available in a stated place in the medical record room for 15 days after discharge. After written and verbal warning of failure to complete patient records within 30 days after discharge, a practitioner will received an “administrative withdrawal of privileges” as defined in the Practitioner Suspension for Failure to Complete Medical Records policy. Hospital privileges will be reinstated; one the practitioner has notified the administrator on call that his/her records are complete. 18. Authentication of medical records may occur by means of personal signature, a signature stamp used personally by the practitioner, or an electronic means of authentication appropriately protected by password or electronic key system. If a signature stamp is utilized, the practitioner whose signature the stamp represents shall place in the administrative offices of the hospital a signed statement to the effect that they are the only person who has the stamp and used it. There shall be no delegation to another individual. Any unauthorized uses of the stamp, a computer key 8 Proposed Changes to the FMH Medical Staff Rules & Regulations or other code signature shall be referred to the Executive Committee and may be grounds for discipline under the provisions of the medical staff bylaws. C. GENERAL CONDUCT OF CARE 1. Except in an emergency, a general consent form, signed by or on behalf of each patient admitted to the hospital, must be obtained at the time of admission. The admitting officer should notify the attending practitioner whenever such consent has not been obtained. When so notified, it shall, except in emergency situations, be the practitioner's obligation to obtain proper consent before the patient is treated in the hospital. 2. All orders for treatment shall be in writing, except for verbal orders given and implemented in accordance with this section. Verbal orders are limited to urgent situations where immediate written or electronic communication is not feasible. They shall be used only to meet the medical care needs of the patient when the ordering practitioner is unable to write the order themselves. Verbal orders are not to be used for the convenience of the ordering practitioner. Verbal orders, when necessary, shall be dictated to: a) a licensed nurse b) a licensed pharmacist c) a licensed respiratory therapist d) another qualified person authorized to accept such orders consistent with state and federal law All such verbal orders shall be a) signed, dated and timed by the appropriate person when dictated b) repeated back to the practitioner ordering (repeated and verified) Authenticated by the responsible practitioner within 48 hours of giving the order. If the responsible practitioner is not available to authenticate the order within 48 hours, such order may be countersigned by the covering physician who attends the patient within the 48 hour period. The covering physician countersigning the order assumes full responsibility for the order as being complete, accurate and final. Failure of the responsible practitioner to authenticate such order within 48 hours shall be referred to the Medical Staff Executive Committee for appropriate action consistent with the Medical Staff Bylaws. 9 Proposed Changes to the FMH Medical Staff Rules & Regulations 3. The practitioner's orders must be written clearly, legibly and completely and in black ink. 4. Standing orders in general use will be reviewed annually at the respective medical service. A physician may adopt standing orders for personal use and must review them each year. 5. All previous orders are canceled when patients go to surgery. 6. Automatic stop order shall exist for antibiotics and narcotics unless otherwise specified in the physician orders. Before cancellation the nursing service shall consult the physician. A listing of specific medications for which automatic stop orders are required shall be adopted as needed as part of the Pharmacy & Therapeutics function and maintained by the pharmacy. The pharmacist will notify the physician with a Stop Order when a medication must be renewed. The physician will have 23 hours to renew, change or discontinue the order. If not renewed within 23 hours, pharmacy will contact the physician directly indicating the order in question will be discontinued unless the order is renewed. 7. Drugs and Medications 7-1 All drugs and medications administered to patients shall be those listed in the latest edition of: United States Pharmacopoeia, National Formulary, American Hospital Formulary Service or A.M.A. Drug Evaluations. Such drugs may be administered as ordered unless subject to written pharmacy and therapeutic policy. 7-2 Investigational drugs may be used in accordance with written pharmacy and therapeutic policy, with the Statement of Principles Involved in the Use of Investigational Drugs in Hospitals, and all regulations of the Federal Drug Administration. 8. Any qualified practitioner with clinical privileges in this hospital can be called for consultation within his/her area of expertise. 9. The attending practitioner is primarily responsible for requesting consultation when indicated and for calling in a qualified consultant. a. consultation shall be ordered when: 1. the attending physician deems it necessary 2. as required by services b. the requesting physician should indicate if he wishes consultant to renderopinion only, assume management of a specific problem, or accept patient in transfer. 11. If a nurse has any reason to doubt or question the care provided to any patient or believes that appropriate consultation is needed and has not been obtained, she shall call this to the attention of her superior who will contact the attending physician. If warranted the matter will be referred to the chief of the service wherein the practitioner has clinical privileges. Where 10 Proposed Changes to the FMH Medical Staff Rules & Regulations circumstances are such as to justify such action, the chief of the service may himself request a consultation. 12. Autopsies: 12-1 Indications It is recommended that the physician responsible for a deceased patient’s care seek permission to obtain an autopsy in the following circumstances: a) Explain unknown and unanticipated medical complications. b) Cause of death is not known with certainty on clinical grounds. c) To help allay concerns of family and/or public; provide reassurance. d) Unexpected or unexplained death occurring during or following any dental, medical, or surgical diagnostic procedures, therapies. e) In patients who have participated in clinical trials. f) Unexpected or unexplained deaths which are apparently natural and not subject to a forensic medical jurisdiction. g) Natural deaths which are subject to, but waived by a forensic medical jurisdiction, such as DOA, deaths within 24 hours of admission, deaths in which the patient sustained or apparently sustained an injury while hospitalized. h) Deaths which resulted from high-risk infectious and contagious diseases. i) All obstetric, neonatal, pediatric deaths. j) Deaths at any age in which autopsy may disclose a known or suspected illness which also may have a bearing on survivors or transplant recipients. k) Deaths known or suspected to have resulted from environmental or occupational hazards. 12-2. Permission Permission for performance of an autopsy must be obtained from the deceased patient’s next of kin or other legally appointed person by the attending physician or his/her designee in all cases. Permission will be documented on forms available from the Pathology Services. Permission may also be granted by authorities within the office of the Chief Medical Examiner in cases coming within its jurisdiction. 12-3. Notification The Pathology Department will notify the attending physician of the time, date, and location where the autopsy will be performed and invite the attending physician and other interested practitioners to attend the autopsy. 12-4. Presentation 11 Proposed Changes to the FMH Medical Staff Rules & Regulations The clinical aspects and autopsy findings will be discussed at the appropriate Service meetings on all cases in which an autopsy has been performed. 13. Restraints: Restraint standing orders will be followed as outlined in the State and Federal regulations and the policies of Franklin Memorial Hospital. D. GENERAL RULES REGARDING SURGICAL CARE 1. Except in severe emergencies, the history and physical examination, the preoperative diagnosis and clinically indicated laboratory tests must be recorded on the patient's medical record prior to any surgical procedure. The history and physical examination shall have been recorded within 30 days before the surgical procedure is performed or within 24 hours after inpatient admission. If performed within 30 days of admission, an update documenting any changes in the patient’s condition must be completed within 24 hours after inpatient admission or prior to surgery. If not recorded, the operation shall be canceled. In any emergency the practitioner shall make at least a comprehensive note regarding the patient's condition prior to the induction of anesthesia and the commencement of the surgical procedure. 2. A patient admitted for dental care is a dual responsibility involving the dentist and physician member of the medical staff. 2-1 Dentist's Responsibilities a. A detailed dental history justifying hospital admission. b. A detailed description of the examination of the oral cavity and a preoperative diagnosis c. A complete operative report, describing the findings and technique. In cases of extraction of teeth the dentist shall clearly state the number of teeth and fragments removed. All tissue including teeth and fragments shall be sent to the hospital pathologist for examination. d. Progress notes as are pertinent to the oral condition. e. Clinical resume (or summary statement). f. The discharge of the patient shall be on written order of the dentist member of the medical staff. 2-2 Doctors of medicine or osteopathy' Responsibilities: a. Medical history pertinent to the patient's general health. b. A physical examination to determine the patient's condition prior to anesthesia and surgery. 12 Proposed Changes to the FMH Medical Staff Rules & Regulations c. Supervision of the patient's general health status while hospitalized. 3. Written, signed, informed, surgical consent shall be obtained prior to the operative procedure except in those situations wherein the patient's life is in jeopardy and suitable signatures cannot be obtained due to the condition of the patient. Consent forms must have been signed within 60 days prior to performance of surgery. In emergencies involving a minor or unconscious patient in which consent for surgery cannot be immediately obtained from parents, guardian or next of kin or other legally authorized person, the procedure may be performed but these circumstances should be fully explained on the patient's medical record. A consultation in such instances may be desirable before the emergency operative procedure is undertaken if time permits. 4. The anesthetist shall maintain a complete anesthesia record to include evidence of pre-anesthetic evaluation and post-anesthetic evaluation and post-anesthetic follow-up of the patient's condition. In the event that the anesthetist has performed a pre-anesthetic evaluation prior to the immediate operative period, he/she must update and record the pre-anesthetic evaluation to include an evaluation of the patient’s immediate pre-operative status. 5. A list of case types for which a surgical assistant is required shall be maintained and updated by Surgical Services no less than every three years. The following practitioner categories shall be allowed to function as surgical first assistants: doctors of medicine or osteopathy, physician assistants, nurse practitioners, RN first assistants, CNM first assistants and Certified Surgical Technician first assistants. No practitioner shall assist at surgery without being privileged to do so under these Bylaws, Rules and Regulations. 6. Except in an emergency, in any surgical procedure with unusual hazard to life, there must be a second surgeon who is qualified and credentialed by the medical staff present and scrubbed. A listing shall be maintained of case types for which a second surgeon shall be required. 7. All tissues removed in the hospital, except those specifically excluded by written hospital policy, removed at the operation shall be sent to the hospital pathologist or another licensed pathologist who shall make such examination as he may consider necessary to arrive at a tissue diagnosis. His/her authenticated report shall be made part of the patient's medical record. 8. Surgeons must be in the operating room and ready to commence operation at the time scheduled and except in emergency situations, the operating room will be held no longer than 15 minutes after scheduled time. 9. In general the more serious operations should have priority over elective cases to permit more prolonged recovery room observation. 13 Proposed Changes to the FMH Medical Staff Rules & Regulations 10.During such times as there may be a shortage of personnel due to vacations or illnesses, the scheduling of minor cases requiring general anesthesia shall be at the discretion of the operating room supervisor or his/her representative. 11. A sponge, instrument, and needle count is to be taken on all surgical procedures. The decision that such count is not necessary will be the surgeon's and the count sheet of the patient shall make note of that decision. On completion the count sheet of the patient shall become a permanent part of the patient's record. 12. A roster shall be maintained of all practitioners, including surgical assistants, and their specific surgical privileges. E. EMERGENCY SERVICES 1. The medical staff or other qualified and credentialed personnel shall provide 24 hour emergency medical and surgical coverage for the emergency room. X-ray, laboratory, and anesthesia services will be available at all hours necessary. 2. Twenty-four hour in-house emergency room coverage will be provided by full-time emergency room doctors of medicine or osteopathy and their affiliated physician assistants or other qualified and credentialed personnel. These individuals are also required to respond to in-patient emergencies pending arrival of the appropriate physician. 3. The routine outpatient form shall be completed and signed by the attending clinician. 4. This form shall include the history, significant physical and laboratory findings, diagnosis and disposition. 5. There shall be a plan for the case of mass casualties at the time of any major disaster, based upon the hospital's capabilities in conjunction with other emergency facilities in the community. It shall be developed by a committee which includes at least 1 member of the medical staff or AHP, the Chief Nursing Officer or his/her designee, and a representative from hospital administration. When approved by the medical staff and governing body, the plan shall be appended to this document. 6. All doctors of medicine or osteopathy shall be assigned to posts and it is their responsibility to report to their assigned stations. The chief of medical staff and the chief executive officer or their designees will work as a team to coordinate activities and directions. In case of evacuation of patients from one section of the hospital to another or evacuation from hospital premises, the chief of the medical staff or incident commander during the disaster will authorize the movement of patients. All policies concerning direct patient care will be a joint responsibility of the service chiefs and the Chief Executive officer of the hospital. 14 Proposed Changes to the FMH Medical Staff Rules & Regulations 7. The disaster plan should be rehearsed at least twice a year, preferably as part of a coordinated drill in which other community emergency services participate. The drills, which should be realistic, must involve the medical staff, as well as administrative, nursing and other hospital personnel. A written report and evaluation of all drills shall be made. F. INTENSIVE CARE UNIT 1. An intensive care unit is a controlled area staffed by skilled personnel and modern emergency equipment providing care of the highest quality for the acutely ill medical and surgical patients. 1-1 The purpose of the intensive care unit is: a) To provide the best possible physical and emotional care for patients with acute myocardial infarction, arrhythmias, and other serious medical and surgical conditions. b) To detect and attempt to correct danger signs that could lead to a cardiac or respiratory emergency by continuous skilled observation. c) To provide definitive treatment for such emergencies. 1-2 Policies of the ICU a) The unit director will be responsible for the conduct of the unit. b) The attending physician shall at all times retain, in accordance with written ICU policies, responsibility for the medical management of his/her patient. In placing the patient in the unit, the physician indicates his/her wish for prompt resuscitative efforts. Consultation for seriously ill patients may be well advised. c) The unit director will serve as liaison between the attending doctors of medicine or osteopathy and the unit nursing staff regarding priorities, policies and all other matters connected with the unit. 1-3 Criteria for admission to the unit include: a) Those patients having suspected impending or acute myocardial infarctions. b) Those patients having acute manifestations or other cardiac or life-threatening respiratory problems. 15 Proposed Changes to the FMH Medical Staff Rules & Regulations c) Any conflicts concerning bed utilization will be resolved be the director or his/her designee. G. CLINICAL SERVICE 1. The Maternal & Child Health, Adult Medicine and Surgical Services shall adopt procedural regulations to cover the areas of medical care, evacuation, and ongoing education. 2. Each service will formulate the criteria for the various medical and surgical privileges and will constantly update these criteria. 3. H. Each service shall have at least six meetings each year. HEALTH PROFESSION STUDENTS 1. Health profession students may from time to time be granted temporary clinical status at the hospital for the purpose of furthering their education and of providing the intellectual stimulation of teaching to the medical staff. 2. Applications for such temporary clinical status shall include a letter from the student’s professional school attesting to his/her status as a student at the school, describing the student’s present training and experience, and setting forth the school and the student’s expectations for their experience at Franklin Memorial Hospital. All students shall be covered by malpractice insurance. 3. Students to whom temporary clinical status are granted shall be individually assigned to an appropriate service and shall be responsible to the chief of that service and under the supervision of a member of the medical staff. They shall not be members of the medical staff. At all times the responsible member of the medical staff is responsible for the actions of the student. 4. Health Profession Students may interview patients, perform physical examinations, review medical information, write histories, physical examinations, and other narrative notes in the medical record, and perform procedures under the supervision of a member of the Medical Staff. All invasive procedures must be performed under the direct supervision of a member of the Medical Staff. 5. All orders by students must include the name of the responsible member of the medical staff and those orders must be signed by the same member of the medical staff before such orders are carried out. 6. I. If the responsible practitioner is unavailable, a covering practitioner shall be designated in writing. INTERN AND RESIDENT DOCTORS OF MEDICINE OR OSTEOPATHY 16 Proposed Changes to the FMH Medical Staff Rules & Regulations Intern and resident doctors of medicine or osteopathy may from time to time be granted temporary clinical status at the hospital for the purpose of furthering their education and providing the intellectual stimulation of teaching to the medical staff. Applications for such temporary clinical status shall include a letter from the physician’s training program hospital attesting to his/her status as a physician in training, describing the physician’s present training and experience, and setting forth the program and the physician’s expectations for their experience at Franklin Memorial Hospital. Intern and resident doctors of medicine or osteopathy to whom temporary clinical privileges may be granted shall be individually assigned to an appropriate service, shall be responsible to the chief of that service and under the supervision of a member of the medical staff. They shall not be members of the medical staff. At all times the responsible practitioner is responsible for the actions of the individual intern and/or resident. If the responsible practitioner is unavailable, a covering practitioner shall be designated in writing. J. MOONLIGHTING RESIDENTS From time to time, residents who are not yet eligible for Board Certification may be utilized at Franklin Memorial Hospital to assist Primary and Hospitalist doctors of medicine or osteopathy with practice coverage. The resident doctors of medicine or osteopathy are considered independent contractors and not considered employees of Franklin Memorial Hospital 1. Qualifications The resident must: a) Be independently licensed in the State of Maine (cannot moonlight on training license) b) Be in their last year of residency. c) Submit a letter from the director of the residency program attesting to the qualifications of the resident and endorsing the activity of moonlighting d) Be credentialed in accordance with Franklin Memorial Hospital Medical Staff Bylaws 2. Overview of supervision The attending physician will meet with the resident and go over plans and obligations. The resident will act as the on-call physician and be the primary responder for the practice. The attending physician will be available continuously by either phone or in person during the residents’ shift. 3 Specific rules for supervision a) The resident will notify the attending of all admissions. The attending will visit and write a note within 48 hours of each admission b) The resident will review discharge plans with the attending on all patients being discharged. The resident is responsible for dictating the discharge summary and writing discharge orders. 17 Proposed Changes to the FMH Medical Staff Rules & Regulations c) The resident will consult the attending on all transfers to the ICU or to another acute care facility. d) The resident will consult with and co-manage with the attending on all ICU patients and all other seriously ill or complex patients. e) The attending will complete a written evaluation form as proscribed by the residents’ training program. A copy of this will be retained in the residents’ file in the Office of Medical affairs and the original forwarded to the residency program director. f) The residents’ privileges will not exceed those of the attending physician g) The resident under the direct supervision of an attending who holds the privilege to perform the procedure may perform procedures. J. EMERGENCY MEDICAL TECHNICIANS 1. Ambulance personnel are allowed to assist in the hospital if the following criteria are met: a) the ambulance personnel must: i. be a licensed E.M.T. - A or accredited by the state iii. and have their credentials approved by the emergency room chief b) while in the hospital, ambulance personnel wear appropriate clothing with identifying patches c) no more than three ambulance personnel be present in the emergency room at any time without a patient whom they have transported. d) the ambulance personnel stay either in the emergency room itself or in the cafeteria unless requested to go elsewhere by the emergency room nurse or a physician to attend a patient. 18