Anticoagulation Certificate Program Home Study November 2 nd
advertisement
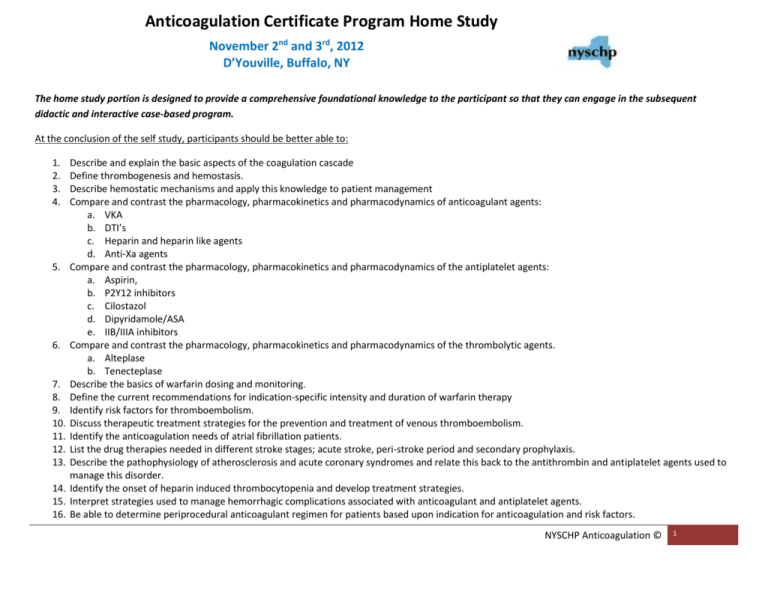
Anticoagulation Certificate Program Home Study November 2nd and 3rd, 2012 D’Youville, Buffalo, NY The home study portion is designed to provide a comprehensive foundational knowledge to the participant so that they can engage in the subsequent didactic and interactive case-based program. At the conclusion of the self study, participants should be better able to: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Describe and explain the basic aspects of the coagulation cascade Define thrombogenesis and hemostasis. Describe hemostatic mechanisms and apply this knowledge to patient management Compare and contrast the pharmacology, pharmacokinetics and pharmacodynamics of anticoagulant agents: a. VKA b. DTI’s c. Heparin and heparin like agents d. Anti-Xa agents Compare and contrast the pharmacology, pharmacokinetics and pharmacodynamics of the antiplatelet agents: a. Aspirin, b. P2Y12 inhibitors c. Cilostazol d. Dipyridamole/ASA e. IIB/IIIA inhibitors Compare and contrast the pharmacology, pharmacokinetics and pharmacodynamics of the thrombolytic agents. a. Alteplase b. Tenecteplase Describe the basics of warfarin dosing and monitoring. Define the current recommendations for indication-specific intensity and duration of warfarin therapy Identify risk factors for thromboembolism. Discuss therapeutic treatment strategies for the prevention and treatment of venous thromboembolism. Identify the anticoagulation needs of atrial fibrillation patients. List the drug therapies needed in different stroke stages; acute stroke, peri-stroke period and secondary prophylaxis. Describe the pathophysiology of atherosclerosis and acute coronary syndromes and relate this back to the antithrombin and antiplatelet agents used to manage this disorder. Identify the onset of heparin induced thrombocytopenia and develop treatment strategies. Interpret strategies used to manage hemorrhagic complications associated with anticoagulant and antiplatelet agents. Be able to determine periprocedural anticoagulant regimen for patients based upon indication for anticoagulation and risk factors. NYSCHP Anticoagulation © 1 Be advised, although the primary reference is the ACCP 2012 guidelines in Chest , there may be other readings the participant is referred to, these will be specifically indicated in each section. The materials are all provided in a PDF format for each section. These materials are to assist you in completing the home study guide and the examination. After completing these sections, the participant will be required to complete the self-study open book test. The test must be completed by no later than October 26, 2012. The home study portion must be completed in order to participate in the live program. A passing score of 70% must be achieved on the self-study online exam. Those failing to achieve this score will be contacted prior to the program for discussion and remediation. 1. Describe and explain the basic aspects of the coagulation cascade 2. Define thrombogenesis and hemostasis. 3. Describe hemostatic mechanisms and apply this knowledge to patient management Readings for the Home Study Guide (provided as pdf) 1. NEJM, 359(9):august, 2008: 938-949 – Mechanisms of Thrombus Formation 2. Refer to appendix A-C of this home study for review of coagulation cascade coordinated with mechanism of anticoagulant drug therapy 3. What Does It Take to Make the Perfect Clot? Arterioscler Thromb Vasc Biol. 2006;26:41-48.) http://atvb.ahajournals.org/cgi/reprint/26/1/41 QUESTIONS: Describe Virchow’s triade and its relationship to thrombosis. Appreciate the differences in the pathophysiology of arterial and venous thrombosis Define the aspects of clot initiation, propagation and amplification. Identify the role of Factor VIIa in and tissue factor in clot formation What are our body’s natural anticoagulants? NYSCHP Anticoagulation © 2 4. Compare and contrast the pharmacology, pharmacokinetics and pharmacodynamics of anticoagulant agents: a. VKA b. DTI’s c. Heparin and heparin like agents d. Anti-Xa agents 5. Compare and contrast the pharmacology, pharmacokinetics and pharmacodynamics of the antiplatelet agents: b. Aspirin, b. P2Y12 inhibitors c. Cilostazol d. Dipyridamole/ASA e. IIB/IIIA inhibitors 6. Compare and contrast the pharmacology, pharmacokinetics and pharmacodynamics of the thrombolytic agents. a. Alteplase b. Tenecteplase Readings for the Home Study Guide 1. New Antithrombotic Drugs CHEST ACCP guidelines, 9th ed. 2012;141(2_suppl):e120S-e151S 2. Oral Anticoagulant Therapy: CHEST ACCP Guidelines, 9th ed. 2012: e44S-e88S 3. Antiplatelet Drugs CHEST ACCP Guidelines, 9th ed. 2012: e89S-e119S 4. Parenteral Anticoagulants CHEST ACCP Guidelines, 9th ed. 2012: e24S-e36S 5. Refer to appendix D of this home study for review of warfarin metabolism Recommended Readings Anticoagulation Therapy: A Point-of- Care Guide Chapter 2-7 and 9 and 18 Agent Classification Site Route Tmax T Metabolism Elimination Dosing Monitoring of 1/2 action Food & Drug Interactions Warfarin Heparin Enoxaparin Dalteparin Fondaparinux Bivalirudin Argatroban Dabigatran Rivaroxaban Apixaban Aspirin Dipyridamole/ASA Ticlopidine Clopidogrel Prasugrel NYSCHP Anticoagulation © 3 Ticagrelor Cilostazol Abciximab Eptifibatide Tirofiban Alteplase Tenecteplase Vitamin K Protamine Factor VIIa QUESTIONS: List some of the advantages of low-molecular weight heparin (LMWH) over UFH Know each products FDA approved indication and corresponding dosing Know the impact of obesity and renal dysfunction on each of the agents What are the recommendations for validating a therapeutic range for Unfractionated Heparin (UFH) for an institution? 7. Describe the basics of warfarin dosing and monitoring. 8. Define the current recommendations for indication-specific intensity and duration of warfarin therapy Readings for the Home Study Guide (provided as pdf) 1. Oral Anticoagulants CHEST. 2012;141(2_suppl):e44S-e88S 2. Evidenced Based Medicine of Anticoagulant Therapy, CHEST. 2012;141(2_suppl):e152S-e184S NYSCHP Anticoagulation © 4 3. Refer to appendix D of this home study for review of warfarin metabolism Recommended Readings Anticoagulation Therapy: A Point-of- Care Guide Chapter 2, 18 Available from www.ashp.org/bookstore QUESTIONS: List the vitamin K dependent clotting factors that warfarin interferes with and their respective half-lives Describe how warfarin exerts it’s pharmacologic effect. (focus on the difference between anticoagulant and antithrombotic effect) What two reasons do we overlap UFH/LMWH/fondaprinux with warfarin for? How do we monitor warfarin for efficacy? What is the most common target range for warfarin? Describe the metabolism of warfarin and indicate the rationale behind the stereo-specific drug interactions. Indicate factors that are associated with an increased a bleeding while on warfarin What is the recommended INR monitoring for VKA? What is the typical % dosage change that is made to warfarin (either up or down)? Discuss the genetic polymorphisms of the cytochrome P450 2C9 and VKOR1 and their resultant effects on response to warfarin. What is the pathology behind the following side effects of warfarin and how would you manage each episode?: NYSCHP Anticoagulation © 5 a. purple toe syndrome b. warfarin induced skin necrosis (WISN or CISN (for Coumadin induced skin necrosis) Discuss the teratogencity of warfarin and utility/safety in any stage of pregnancy. 9. Identify risk factors for thromboembolism. 10. Discuss therapeutic treatment strategies for the prevention and treatment of venous thromboembolism. Readings for the Home Study Guide (provided as pdf) 1. Prevention of VTE non-surgical CHEST. 2012;141(2_suppl):e195S-e226S 2. Prevention of VTE nonorthopedic surgical CHEST. 2012;141(2_suppl):e227S-e277S 3. Prevention of VTE orthopedic. CHEST. 2012;141(2_suppl):e278S-e325S 4. Antithrombotic Therapy for VTE Disease CHEST. 2012;141(2_suppl):e419S-e494S 5. Evidenced Based Medicine of Anticoagulant Therapy, CHEST. 2012;141(2_suppl):e152S-e184S Recommended Readings Anticoagulation Therapy: A Point-of- Care Guide Chapter 10 & 11 Available from www.ashp.org/bookstore QUESTIONS: Use the following case to answer questions 1-6: RT is a 67 yo male patients admitted to hospital for community acquired pneumonia (CAP) and chronic obstructive pulmonary disease (COPD) exacerbation and hypertension. His medications upon admission include: spiriva 1 capsule inhaled qday, Advair 50-250 1 puff BID, MVI 1 qday, lisinopril/HCTZ 20/25 1tab qday and calcium 500 elemental qday. He has varicose veins, weight is 287 lbs, HT=5’10”, history of phlebitis. 1. What is the PADUA score? 2. List RT’s risk factors for developing a deep vein thrombosis while in hospital. 3. Is RT a candidate for DVT prevention and if so list all available options and expected efficacy of each. 4. RT develops a DVT and PE while in hospital, provide therapeutic recommendations to manage this event, one using UFH and the other using NYSCHP Anticoagulation © 6 LMWH and when and what dose to begin warfarin with and recommendation for how long to overlap therapy. 5. The recommended duration of warfarin therapy for RT would be, justify your answer: 6. The recommended target INR would be: a. 1-2 b. 1.5-2 c. 2-3 d. 2.5-3.5 Be able to determine if patients who are candidates for outpatient therapy. What is the role of thrombolytics for treatment of acute PE? What about DVT? 11. Identify the anticoagulation needs of atrial fibrillation patients. Readings for the Home Study Guide (provided as pdf) 1. Antithrombotic Therapy in Atrial Fibrillation: CHEST ACCP Guidelines, 9th ed. 2012: e531S-575S 2. Furie KL, Goldstein LB, Albers GW, et al. Oral antithrombotic agents for the prevention of stroke in nonvalvular atrial fibrillation: A science advisory for healthcare professionals from the American Heart Association/American Stroke Association. Published on-line ahead of print. http://stroke.ahajournals.org/content/early/2012/08/02/STR.0b013e318266722a.full.pdf+html 3. Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the management of atrial fibrillation. The Task Force for the Management of Atrial Fibrillation of the European Society of cardiology (ESC). Eur Heart J 2010 Oct;31(19):2369-429. Excellent instructional content (text, figures & tables) on topics related to atrial fibrillation. 4. Altman R, Vidal HO. Battle of oral anticoagulants in the field of atrial fibrillation scrutinized from a clinical practice (the real world) perspective. Thromb J. 2011 Jul 27;9:12. PMID: 21794130 5. Pradaxa (dabigatran) & Xarelto (rivaroxaban) Prescribing Information (Access via www.fda.gov/cder , or www.pradaxa.com & www.xarelto.com) Recommended Readings 1. Anticoagulation Therapy: A Point-of- Care Guide Chapter 9 & Chapter 12 Available from www.ashp.org/bookstore QUESTIONS What are the differences/commonalities for the following types of atrial fibrillation: paroxysmal, persistent, permanent, lone or postoperative? What is the difference between rhythm control and rate control? NYSCHP Anticoagulation © 7 What is the primary purpose of anticoagulation therapy for atrial fibrillation patients? What is the CHADS2 score and how is it calculated? What is the most significant risk of anticoagulation therapy for atrial fibrillation patients? List additional risks of anticoagulation therapy. What is the HAS-BLED score and how is it calculated? When warfarin is selected, what is the dose/administration, goal INR and adverse effects/risk? When dabigatran is selected, what is the dose/administration, monitoring and adverse effect/risk? When rivaroxaban is selected, what is the dose/administration, monitoring and adverse effect/risk? 12. List the drug therapies needed in different stroke stages; acute, peri-stroke period & 20 prophylaxis. Readings for the Home Study Guide (provided as pdf) 1. Antiplatelet Drugs CHEST ACCP Guidelines, 9th ed. 2012: e89S-e119S 2. Antithrombotic and Thrombolytic Therapy for Ischemic Stroke CHEST ACCP Guidelines, 9th ed. 2012: e601S-636S 3. Kral M, Herzig R, Sanak D, et al. Oral antiplatelet therapy in stroke prevention. Minireview. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2010 Sep;154(3):203-10. PMID: 21048805 Note: use this for antiplatelet drug information and not as a guideline. 4. Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: A guideline for health care professionals from the American Heart Association/American Stroke Association. http://stroke.ahajournals.org/content/42/1/227.full.pdf 5. Aggrenox (dipyridamole/ASA); Plavix (clopidogrel); Pletal (cilostazol) & Ticlid (ticlopidine) Prescribing Information Access via www.fda.gov/cder , or www.aggrenox.com, or www.plavix.com, www.pletal.com, www.activase.com Recommended Readings Anticoagulation Therapy: A Point-of- Care Guide Chapter 6 Available from www.ashp.org/bookstore Cardiovascular Pharmacotherapy: A Point-of-Care Guide Chapter 13 Available from www.ashp.org/bookstore QUESTIONS: Describe the difference between an ischemic stroke, transient ischemic attack and intracerebral or subarachnoid hemorrhage. NYSCHP Anticoagulation © 8 When alteplase is selected for acute ischemic stroke, understand patient selection criteria and intravenous dose and administration. Explain the bleeding risks associated with thrombolytics, including intracranial bleeding/hemorrhagic transformation. List the dose, administration, contraindications/major warnings and common ADRs of the antiplatelet agents: a. Aspirin b. Ticlopidine c. Clopidogrel d. ASA/dipyridamole e. Cilostazol 13. Describe the pathophysiology of atherosclerosis and acute coronary syndromes and relate this back to the antithrombin and antiplatelet agents used to manage this disorder. Readings for the Home Study Guide (provided as pdf) 1. Antiplatelet Drugs CHEST ACCP Guidelines, 9th ed. 2012: e89S-e119S 2. Acute Coronary Syndromes: Diagnosis and Management, Part I Mayo Clin Proc. 2009;84(10):917-938 3. Acute Coronary Syndromes: Diagnosis and Management, Part II Mayo Clin Proc. 2009;84(11):1021-1036 ACC/AHA Guidelines and statements pertinent to ACS/CAD also found at : http://my.americanheart.org/professional/StatementsGuidelines/ByTopic/TopicsA-C/ACCAHA-Joint-Guidelines_UCM_321694_Article.jsp 4. 2012 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction (Updating the 2007 Guideline and Replacing the 2011 Focused Update) Circulation. 2012;126:875-910 5. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention Circulation. 2011;124:e574–e651. 6. 2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non– ST-Elevation Myocardial Infarction Circulation. 2011;123:e426-e579 7. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (Updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (Updating the 2005 Guideline and 2007 Focused Update) Circulation. 2009;120:2271-2306. 8. ACCF/ACG/AHA 2010 Expert Consensus Document on the Concomitant Use of Proton Pump Inhibitors and Thienopyridines: A Focused Update of the ACCF/ACG/AHA 2008 Expert Consensus Document on Reducing the Gastrointestinal Risks of Antiplatelet Therapy and NSAID Use Circulation. 2010;122:2619-2633) 9. ACCF/AHA ClopidogrelliClinicallAlert: Approaches to the FDA “Boxed Warning Circulation. 2010;122:537-557. NYSCHP Anticoagulation © 9 Recommended Readings 1. Wallentin L, Becker RC, Budaj A et al. Ticagrelor versus Clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009;361;1045-57. 2. Subberwal S, Bach RG, Chen AY et al. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE Bleeding Score. Circulation 2009;119:1873-82. 3. Mega JL, Close SL, Wivott SD et al. Cytochrome P450 genetic polymorphism and the response to prasugrel: relationship to pharmacokinetic, pharmacodynamic, and clinical outcomes. Circulation 2009;119:2553-60. 4. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor vs. clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045-57. 5. Mahaffey KW, Wojdyla DM, Carroll K, et al. Ticagrelor compared with clopidogrel by geographic region in the Platelet Inhibition and Patient Outcomes (PLATO) trial. Circulation. 2011;124:544-54. 6. Mehta SR, Tanguay JF, Eikelboom JW, et al. Double-dose vs. standard-dose clopidogrel and high-dose vs. low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet. 2010;376:1243. 7. Mehta SR, Granger CB, Boden WE, et al. Early vs. delayed invasive intervention in acute coronary syndromes. N Engl J Med. 2009;360:2165-75. Describe the pathophysiology of acute coronary syndromes and the role pharmacologic therapy has on the outcomes of the disease What is the onset and duration of action of aspirin, clopidogrel, prasugrel and ticagrelor? Compare and contrast the safety and efficacy of clopidogrel, prasugrel and ticagrelor. How do drug interactions, genetic polymorphisms and other factors affect clopidogrel responsiveness? List the risk factors for bleeding in patients receiving anti-thrombotic therapy for coronary artery disease What is the current role of thrombolytics in the management of ST-segment elevation MI? Identify ACS high risk features and differentiate recommended therapy for low and high risk patients. Compare and contrast the safety and efficacy of heparin, LMWH, bivalirudin, fondaparinux and IIbIIIa inhibitors in the management of ACS. NYSCHP Anticoagulation © 10 14.Identify the onset of heparin induced thrombocytopenia and develop treatment strategies. Readings for the Home Study Guide (provided as pdf) 1. Treatment and Prevention of Heparin Induced Thrombocytopenia CHEST. 2012;141(2_suppl):e495S-e530S Recommended Readings Anticoagulation Therapy: A Point-of- Care Guide Chapter 15 Available from www.ashp.org/bookstore QUESTIONS: Describe the pathophysiology of heparin induced thrombocytopenia What is the role of the Elisa PF4 and serotonin release assays? What are the limitations of each? Discuss the time of onset, expected impact on platelets, risk of thrombosis. Understand how to use this data in Warkentin’s 4T prediction model. Develop a therapeutic recommendation for a patient with suspected HIT with thrombosis. List pros and cons of available treatment options, doses and monitoring. 15. Interpret strategies used to manage hemorrhagic complications associated with anticoagulant and antiplatelet agents Readings for the Home Study Guide (provided as pdf) 1. Anticoagulation Therapy: A Point-of- Care Guide Chapter 7 2. Evidence Based Medicine of Anticoagulant Therapy. CHEST. 2012;141(2_suppl):e152S-e184S Recommended Readings 1. Rolfe S, Papadopoulos S, Cabral K. Controversies of anticoagulation reversal in life-threatening bleeds. 2010 Journal of Pharmacy Practice 2010; 23:217-225 2. Van Ryn J et al. Dabigatran etexilate-a novel, reversible, oral direct thrombin inhibitor: Interpretation of coagulation assays and reversal of NYSCHP Anticoagulation © 11 anticoagulant activity. 2010;103:1116-27 3. Miyares MA, Davis K. Newer oralanticoagulants: A review of laboratory monitoring options and reversal agents in the hemorrhagic patient. Am J Health-Syst Pharm 2012;69:1473-84. QUESTIONS: List the risk factors for increased anticoagulant bleeding (Table 7-1) a. Anticoagulationb. Patientc. Procedures- List 4 different approaches to reversing anticoagulation effects (Table 7-2) a. b. c. d. What are the main characteristics of urgent, semi-urgent, non-urgent reversal and “rebound risk” for each (table 7-3, 7-4, 7-5, 7-6, figure 7-1) a. Urgentb. Semiurgentc. NonurgentList the factors impacting extent and speed of reversal (table 7-8) a. Thrombosis riskb. Bridge therapy requirementsc. Patient risk factorsd. Intensity of current anticoagulationNYSCHP Anticoagulation © 12 e. Dose of anticoagulantf. Ability of patient to eliminate anticoagulant- g. Predictability of reversal agent effects Briefly list some of the considerations for reversal of each of the following agentsa. Unfractionated heparin b. Low Molecular weight heparin c. Fondaparinuxd. DTI e. Warfarin List usual doses for FFP, Vitamin K, Activated factor VII, and PCC for reversal of life-threatening bleed in a patient on warfarin (table 7-9). List usual protamine dose(s) for reversal of heparin and low-molecular-weight heparin associated bleeding (table 7-11). What is the usual dose of FFP and how does issue of volume impact use of FFP? (page 146-147) What is main difference between PCC3/PCC4/Activated PCC? (page 147-148) Patient Case: 69 year old patient admitted to hospital for mental status changes and possible UTI now has some hemoptysis. Medications: Warfarin 3mg, metoprolol 12.5mg BID, Lisinopril 10mg daily, Bactrim DS BID (started 2 days ago) NYSCHP Anticoagulation © 13 PMH: paroxysmal atrial fibrillation, congestive heart failure, Labs: Calcium 8.7 mg/dL, Sodium 136 mmol/L, Potassium 4.3 mmol/L, WBC 13.3 K/ul, Hg 9 G/dL, Platelets 397 K/UL, Creatinine 1.8 mg/dL, INR-3.8 1. List and answer (to extent possible) the 2 “reversal considerations” for this patient. (page 123) 2. List and answer (to extent possible) the “other considerations” for this patient. (123-124) 3. Does the patient have any risk factors for increased bleeding (Table 7-1)? 4. Develop an anticoagulation reversal plan using “Reversal Options”(page 126-127) as a guide. 16. Be able to determine periprocedural anticoagulant regimen for patients based upon indication for anticoagulation and risk factors Readings for the Home Study Guide (provided as pdf) 1. Chest supplement, 9th edition, 326S-350SAppendix Table 3.1 and 3.2 Recommended Readings Martin MT, Kuchta AM, Nutescu EA. A clinician's guide to perioperative bridging for patients on oral anticoagulation Journal of Pharmacy Practice. 2010;23:303-312 QUESTIONS: 1. List those procedures that are of low risk and may not require interruption of anticoagulation. 2. List the questions that must be answered prior to determining periprocedural anticoagulation regimen. NYSCHP Anticoagulation © 14 3. List those procedures that place patients at high risk of bleed. 4. Describe the risk categories (i.e. high, moderate, low) of thromboembolism based on patient’s past medical history of a mechanical heart valve, or atrial fibrillation, or venous thromboembolism. 5. Describe the optimal level of anticoagulation based upon risk categories described in #4. Patient Case 69 year old patient is planning to have knee replacement surgery Medications: Warfarin 3mg, metoprolol 12.5mg BID, Lisinopril 10mg daily PMH: paroxysmal atrial fibrillation, congestive heart failure, chronic kidney disease Labs: Calcium 8.7 mg/dL, Sodium 136 mmol/L, Potassium 4.3 mmol/L, WBC 13.3 K/ul, Hg9 G/dL, Platelets 397 K/UL, Creatinine 1.8 mg/dL, INR2.1 1. What is this patient’s TE risk category? 2. What is this patient’s risk of bleed and procedural risk? 3. Should warfarin be discontinued prior to procedure and if so, at what time should that occur? NYSCHP Anticoagulation © 15 Appendix A NYSCHP Anticoagulation © 16 APPENDIX B http://image.absoluteastronomy.com/images/encyclopediaimages/c/co/coagulation_full.svg.png NYSCHP Anticoagulation © 17 APPENDIX C http://www.chelationtherapyonline.com/GarryGordon/images/regulate.gif NYSCHP Anticoagulation © 18 APPENDIX D http://images.google.com/imgres?imgurl=http://www.nature.com/clpt/journal/v80/n1/images/clpt2006377f1.jpg&imgrefurl=http://www.nature.com/clpt /journal/v80/n1/fig_tab/clpt2006377f1.html&usg=__KKTc9kQ_T1gonv1A0EEdNc8GpBQ=&h=568&w=605&sz=48&hl=en&start=2&um=1&tbnid=1q8Wkp5ctT DqUM:&tbnh=127&tbnw=135&prev=/images%3Fq%3Dwarfarin%2Bmetabolism%26hl%3Den%26rlz%3D1W1DLUS_en%26sa%3DN%26um%3D1 NYSCHP Anticoagulation © 19