elemental calcium intake, tablet burden, and dose
advertisement
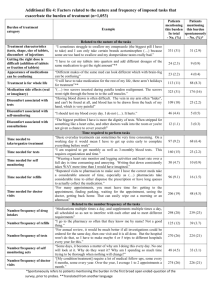
P92 ELEMENTAL CALCIUM INTAKE, TABLET BURDEN, AND DOSE-RELATIVITY OF CALCIUM ACETATE/CARBONATE VERSUS LANTHANUM CARBONATE IN THE TREATMENT OF HYPERPHOSPHATAEMIA Rosamund J Wilson,1 Peter Preston, 2 J Brian Copley2 1 Spica Consultants, Marlborough, UK, 2Shire, Wayne, PA, USA INTRODUCTION: In patients with end-stage renal disease (ESRD), hyperphosphataemia can be managed with calcium (Ca)-based phosphate binders, such as Ca carbonate (CaC)/acetate (CaA), or non-Ca-based binders, such as lanthanum carbonate (LC). Ca-based binders increase systemic Ca load and may be associated with hypercalcaemia, vascular calcification and adynamic bone disease. The aims of this study were to assess the elemental calcium intake, tablet burden, and dose-relativity of CaC/CaA and LC monotherapy. METHODS: We conducted a post hoc analysis of a phase 4, 16-week, real-world study of theefficacy of conversion to LC monotherapy from other phosphate binders (Vemuriet al. 2011; ClinicalTrials.gov: NCT0016012). The study design comprised a 1-week observation period in which patients remained on their existing phosphate binder, a 12-week LC monotherapy titration phase (starting dose: 1500 mg/day; planned maximum dose: 3750 mg/day) and a 4-week LC maintenance period. Baseline was defined as the end of the 1-week observation period. Serum phosphate levels and phosphate binder daily doses were assessed at baseline for patients previously treated with CaC/CaA monotherapy and after 16 weeks of LC monotherapy. Tablet burden was stratified by elemental Ca intake. Doserelativity was defined as the ratio ofmean daily doses required to treat to similar phosphate levels. RESULTS: CaC vs LC A total of 201 patients had recorded doses of both CaC at baseline and LC at week 16. Patients with an elemental Ca intake of ≥ 1.5 g/day (the recommended maximum daily intake of elemental Ca from Ca-based binders) had a mean tablet burden of 9.6 CaC tablets/day (n = 117 [58%]). Patients with an elemental Ca intake ≥ 2.0 g/day (the recommended maximum total daily intake of elemental Ca) had a mean tablet burden of 10.9 CaC tablets/day (n = 76 [38%]). The overall mean tablet burden was 7.4 CaC tablets/day at baseline vs 3.0 LC tablets/day at week 16. CaC:LC dose relativity could not be calculated because CaC was taken in a variety of dose formulations. CaA vs LC A total of 551 patients had recorded doses of both CaA at baseline and LC at week 16. Patients with an elemental Ca intake of ≥ 1.5 g/day had a mean tablet burden of 11.9 CaA tablets or capsules/day (n = 271 [49%]). Patients with an elemental Ca intake ≥ 2.0 g/day had a mean tablet burden of ≥ 13.0 CaA tablets or capsules/day (n = 142 [26%]). The overall mean tablet burden was 8.4 CaA tablets or capsules/day at baseline vs 3.1 LC tablets/day at week 16. The overall CaA:LC dose relativity was 2.0. CONCLUSIONS: Switching patients with ESRD from CaC/CaA monotherapy to LC monotherapy may offer important advantages. These include a reduction in the pill burden, which may improve treatment adherence and thereby phosphate control; and a reduction in elemental Ca intake, lowering the risks of vascular calcification and adynamic bone disease. It is important to consider these findings when decisions are made regarding the use of Ca-based versus non-Ca-based binders for the treatment of hyperphosphataemia in patients with ESRD.