File
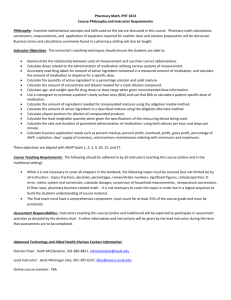
advertisement

Generic Name: naloxone Brand name: NarCan Classification: opioid antagonist; RR <8 or sedation level -4 or -5 Dosage/Route: Dosage/Route prescribed to client: Rate of administration with IV meds: .4 mg; may repeat q 2-3 min. some .1 mg IVstat; may repeat q 3-5 min x Follow Order Set; generally: patients may require up to 2 mg. 3 doses to a total of .4 mg Administer 2.5 mL (.1 mg) longer than 1 Dilute 1 vial of naloxone (.4 mg/mL min, in 9 mL of NS) If needed administer another 2.5 mL .4 mg/10 ML of fluid, want to give over 1 min, 2.5 mL of fluid per dose Repeat. Is dose within recommended DO NOT BOLUS; should be given over ranges? course of time and attempt to arouse pt YES Major Side effects: Ventricular arrhythmias, hypertension/hypotension, pain, n/v Data used to indicate medication is effective: improved respiratory function Medication administration concerns: Monitor resp rate, rhythm, depth, pulse, ECG, BP and LOC frequently for 3-4 hr after expected peak; assess for pain after administration; assess for s/sx of opioid withdrawl Patient/client teaching points: Explain purpose ; explain shorter halflife than opioid so probably will require multiple dosing; explain will completely prevent pain relief and will induce previous pain Generic Name: morphine Brand name: Classification: opioid agonist; Schedule II, binds to opiate receptors in CNS, depresses CNS and alters perception of pain stimuli Major Side effects: -CNS: confusion, sedation, dizziness, dysphoria, eupohoria, floating, hallucinations, HA, unusual dreams -EENT: blurred vision, diplopia, miosis -RESP: respiratory depression -CV: hypotension, bradycardia -GI: constipation, N/V -GU: urinary retention -DERM: flushing, itching -physio/psychological dependence, tolerance Data used to indicate medication is effective: pain evaluation (pain maintained at 6/10 or decreased) Medication administration concerns: Breakthrough pain, changes in LOC, BP, pulse, and respirations, change in bowel function Patient/client teaching points: Caution patient that medication may affect LOC or result in dizziness/drowsiness, and tell them to call for help when ambulating to bathroom Take caution in repositioning in bed, take several minutes to move from lying down, to sitting up, to getting out of bed Tell patient to rotate in bed Q2 hrs (or call for assistance to rotate) to prevent atelectasis Equianalgesic Comparison of Pure Narcotics Drug Name Description 100 x stronger than fentanyl morphine (Sublimaze, Actiq) INCREASING ANALGESIC STRENGTH diacetylmorphine (heroine) oxycodone (Percodan/ Percocet) morphine hydrocodone (Vicodin) methadone meperidine (Demerol) Schedule II 10x more potent than codeine Oxycodone: ER Used in combo w/ ASA or Tylenol Prototype codeine Can be used PCA or Actiq lollipop More lipid soluble; illegal in US (Schedule I) Schedule II Used as analgesic/antitutssive Common outpt LONGEST DURATION Used for detox or maintanence (more mild withdrawl) o Tolerance, less of a buzz Same potency with less duration No antitussive properties Given to stop shivers Post Op Given pain control for allergy to Morphine Schedule II/III 1/10th potency of morphine (5x than ASA /tylnol) Some ppl have genetic block inhibiting them to metabolize to MS Generic Name: hydrocodone/acetominophen Brand name: Vicodin Classification: combination: opioid agonist/nonopioid analgesic combinations; schedule II (III in combination) Why is patient/client receiving this? Management of moderate to severe pain, antitussive; binds to receptors in CNS, alters perception of and response to painful stimuli Dosage/Route: PO: 2.5-10 mg q 3-6 hrs, in combination products acetaminophen should not exceed 4 g/day and should not exceed 5 tablets/day of ibuprofen Availability: 5mg hydrocodone/500 mg acetaminophen Major Side effects: CNS: elevated ICP, seizures, periph neuropathy -CV: torsade de pointes, qt interval prolongation -GI:, hepatotoxicity, pseudomembranous colitis, n/v -Endo: hyperglycemia/hypoglycemia hypersensitivity incl Medication administration concerns: -use with extreme caution in patients taking MAOI’s (produce severe, unpredictable rxns) - assess bp, pulse and respirations, if respiratory is below 10, assess level of sedation -assess bowel function -assess pain: prolonged use may lead to physical and psychological dependence and tolerance Patient/client teaching points: explain therapeutic value to enhance analgesic effect, -instruct pt how and when to ask for and take pain meds -notify if pain control is not sufficien t tramadol (Ultram) Centrally acting analgesic; opioid-like analgesic; schedule IV Why is pt receiving this? Moderate to moderately severe pain, synthetic analgesic that acts at mu receptor Dose IR: PO given either rapid (50-100 mg q 4-6 hrs) or gradual titration (25 mg/day initially increase by 25 mg q 3 days to reach 25 mg qid, eventually 50 mg qid) ER: 100 mg q daily, may titrate up to 300 mg/day if not receiving IR SE dizziness, sedation, HA, constipation, seizures (rare), LESS RESP DEPRESSION, serotonin syndrome, physical/psychological dependence Med admin assess pain before and 2-3 hr following admin, assess bp and rr, not meant for pts w/ opioid dependence, assess previous analgesic hx (i.e. allergies), administered w/out regard to meals ; incr risk of seizures w/ abx and MAOIs, addative CNS depression Pt education Explain purpose of med, how to ask for pain meds, dizziness/drowsiness (driving, fall risk), turn/cough/deep breath q 2 hrs to prevent atelectasis, notify for adverse s/sx NSAIDS (antiinflamatory/analgesic) 1st generation inhibit Cox1 and Cox2 Acetamiinophen (antipyretic/analgesic) 2nd generation inhibit Cox 2 (thought to be safer) COX 1 “GOOD”: found in all tissues, mediates “housekeeping” o Synthesizes prostaglandins to protect gastric mucosa, promote renal blood flow o Promotes platelet aggregation o Synthesizes prostacyclin-> vasodilation o Inhibition results in: bleeding, renal impairment, gastric ulceration BUT prevents clots COX 2 “BAD”: synthesized at site of tissue injury, also found in brain, blood vessels, kidney, and colon o Mediates inflammation, sensitizes receptors to painful stimuli, vasodilation, contribute to colon CA o Inhibition results in: suppression of inflammation/pain/fever, protection against colonCA BUT impairs renal function and promotes MI/stroke ASPIRIN Classification: salicylates Major Side effects: -EENT: tinnitus -GI: bleeding, dyspepsia, epigastric distress, nausea, abd pain, anorexia, hepatotoxicity-Hemat: anemia, hemolysis-Derm: rash, urticarial -Allergic rxns incl. anaphylaxis and laryngeal edema Data used to indicate medication is effective: resolution of pain/fever Medication administration concerns: -may increase risk of bleeding with warfarin, heparin and thrombolytic -Ibuprofen may negate cardioprotective antiplatelet effects of aspirin -may increase activity of sulfonamides -increased risk of GI irritation with NSAIDS Patient/client teaching points: Pt to alert nurse for adverse rxns NSAIDS and types of pain NSAIDS and muscle pain (strain or contusion): o No benefit greater than placebo o MAY actually delay healing; many sports medicine professionals use only for short duration (24-48 hrs) NSAIDS and ligament injury o Limited and mixed results o May be beneficial if promotes mobility o Unsure if healing benefit from anti-inflammatory or analgesic properties NSAIDS and Bone o Marked association between NSAIDS and non-union/delayed healing Acetaminophen: Liver ASA: GI bleed and kidneys Ibuprofen: renal and liver ketorolac (Toradol) NSAID, nonopioid analgesic st Why is pt receiving this? 1 parenteral NSAID : strong analgesia w/ minimal anti-inflammatory , short term mgmt. of pain (not to exceed 5 days total). Inhibits prostaglandin synthesis producing peripherally mediated analgesia. Dose PO (only intended to supplement parenteral therapy): 20 mg initially followed by 10 mg q 4-6 hrs (renal impairment adjustment needed) IM: single dose: 60 mg, multiple dosing 30 mg q 6 hrs ; availability 15 mg/mL IV: single dose: 30 mg, multiple dosing 30 mg q 6 hr (not to exceed 120 mg/day) Administer undiluted: [15-30 mg/mL], administer over at least 15 sec SE Stroke, drowsiness, abnormal thinking, dizziness, asthma, dyspnea, MI, edema, GI bleeding, oliguria, renal toxicity, SJS, TENS, prolonged bleeding time, injection site pain, paresthesia, anaphylaxis Med admin Minimal anti-inflammatory. Administering greater dose increases SE w/ no increased benefit, duration of therapy of all routes should not exceed 5 days, should always initially be given IM/IV. Probenecide increases levels. Lithium toxicity. May decrease effectiveness if used w/ other NSAIDS. Pt education Dizziness (fall risk precautions), take as directed, avoid use w/ ETOH, ASA, acetaminophen, adverse s/sx celecoxib (Celebrex) NSAID, 2nd generation COX Inhibitor (COX2 inhibitor) Why is pt receiving this? relief of osteoarthritis, RA, mgmt. of acute pain incl. dysmenorrhea. Inhibits COX 2 (“the bad cox”) which results in less ulcerogenic SE but does not provide beneficial platelet aggregation. Dose PO: chronic conditions typically 200 mg/day; acute pain: 400 mg initially then 200 mg additionally PRN first day, then 200 mg twice daily SE dizziness, HA, insomnia, MI, STROKE, THROMBOSIS, edema, GI Bleeding, exfoliative dermatitis, SJS, TENS Med admin May decrease effectiveness of ACE inhibitors, thiazide diuretics, and furosemide, lithium toxicity. Use w/ 1st generation nullifies benefits of 2nd generation selectivity. Assess pts for allergy to SULFONAMIDEs, ASA, or NSAIDS, assess for skin rash. Administered w/out regard to meals, capsules may be opened. Pt education Take as directed, notify if signs of GI toxicity or other s/sx occur dronabinol (Marinol) Schedule I Level of evidence weak: may not work for RA, hyperalgesia o May have some neuroprotective quality: slow progression of Alzheimer’s LUNG INJURY is irreversible even after abstainence, so SMOKING NEVER RECCOMENDED Adverse effects in youth Nursing responsibilities o Decrease opioid use o Assess for CV Risks (may cause MI even w/ no risk factors;) o Professionalism/communication o ONLY USE FDA Approved formulations Generic Name: acetaminophen Brand name: Tylenol Classification: analgesic, antipyretic Dosage/Route: 325-650 mg PO q6hrs OR 1 g PO tid or qid OR 1300 mg q8hrs (So as not to exceed 3g/24 hrs) 1000 mg IV q6hrs OR 650 mg IV q4hrs (not to exceed 1000 mg/dose, 4g/day, and less than 4hr dosing interval) Rate of administration with IV meds: Intermittent infusion: infuse over 15 min IV diluents compatible with IV medication: N/A Major Side effects: -CNS (IV): agitation, anxiety -CV (IV)): hypotension or hypertension -GI: hepatotoxicity -GU: renal failure with chronic use -DERM: rash -HEMAT: neutropenia, pancytopenia -MS (IV): muscle spasms Data used to indicate medication is effective: pain evaluation (pain maintained at 6/10 or decreased), temperature via temporal artery (fever reduced to < or equal to 38.5 C) Medication administration concerns: Hepatotoxicity with chronic acetaminophen or alcohol use Patient/client teaching points: During medication reconciliation, confirm no use of OTC medications as can increase hepatotoxic effects acetylcysteine (Mucomyst) Therapeutic antidote Why is pt receiving this? PO: antidote for mgmt. of potentially hepatotoxic overdose of acetaminophen Dose PO: 140 mg/kg initially followed by 70 mg/kg q 4 hr for 17 additional doses; can also be given IV: loading odse 150 mg/kg over 60 min followed by maintanence dose 50 mg/kg over 4 hrs then second maintanence dose 100 mg/kg over 16 hr Dilute in D5W to concentrations varying based on dose and on pt wt SE drowsiness, vasodilation, tachycardia, rhinorrhea, bronchospasm, chest tigntess, n/v, stomatitis, rash, allergic rxns Med admin activated charcoal may absorb Mucomyst and decrease effectiveness. IV most effective if administered within 8 hrs of OD; assess severity of ingestion, plasma levels, Assess for anaphyalaxis w/ IV, monitor cardiac/renal function, serum glucose and electrolytes. AVOID contact w/ metals/rubbers. Dilute 20% PO w/ cola, water or juice. Pt education Explain medication purpose Nitrous oxide Used often in dental procedures 100% excretion through lungs High analgesia at low []’s Inhalation anesthetic Halothane (-ane) Volatile liquids (mixed w/ O2) propofol (Diprivan) General anesthetic HIGH ALERT Why is pt receiving this? Induction of general anesthesia, maintanence of balanced anesthesia when used with other agents. Initiation/maintanence of monitored anesthesia care (MAC) sedation of intubated patients in ICU. Short acting hypnotic w/ unkown MOA Given IV SE propofonol infusion syndrome, discoloration of urine (green), bradycardia, hypotension, dizziness, apnea, burning/tingling at IV site Med admin Works less than 60 sec, lasts about 5 min. Addative CNS depression. Assess RR pulse and BO continouolsy Frequently casues apnea lasting >60 s. Monitor for infusion syndrome (metabolic acidosis, hyperkalemia, lipemia, rhabdo, hepatomegaly, cardiac/renal failure). Assess allergy to egss/soybeans