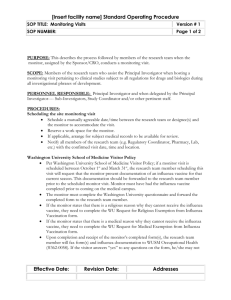
Patient Group Direction development

This Patient Group Direction (PGD) must only be used by pharmacists who have been named and authorised to practice under it.
Patient Group Direction for the Administration of
Trivalent Seasonal Inactivated Influenza Vaccine by
Pharmacists During the 2013/14 Season
(This PGD covers all brands of influenza vaccine as listed in the Department of
Health circular “The influenza immunisation programme 2013/14” https://www.gov.uk/government/publications/flu-immunisation-programme-2013to-2014 )
Version number: 1.0
Change history
Change details Version number
Date
Reference Number:
Valid from:
Expiry date: 1
Patient Group Direction development
Name
Jonathan Mason
Dr Henrietta Hughes
Tony Carson
Job title and organisation
Clinical Adviser
(Medicines)
NHS England (London
Region)
Medical Director
NHS England (London
Region)
Community Pharmacy
Adviser
NHS England (London
Region)
PGD authorisation
Name
Jonathan Mason
Dr Henrietta Hughes
Job title and organisation
Clinical Adviser
(Medicines)
NHS England (London
Region)
Medical Director
NHS England (London
Region)
Screening and
Immunisation Lead
Person signing on behalf of authorising body
Signature
Signature
Date
Date
Reference Number:
Valid from:
Review date:
Expiry date: 2
Training and competency of health professionals
Requirements of health professionals working under the PGD
Qualifications Pharmacist registered with the GPhC or PSNI
Training
The pharmacist should be competent in all aspects of immunisation, in line with the national minimum standards, including: o The reasons for and contraindications to influenza vaccination o The recognition and treatment of anaphylaxis
Authorised pharmacists should have access to o ‘Immunisation against Infectious Disease 2006’ (the Green
Book), and any updates. The current edition can be accessed online from https://www.gov.uk/government/publications/greenbook-the-complete-current-edition o Letter from NHS England, Public Health England and
Department of Health entitled: ‘The flu immunisation programme 2013/14 ’
( https://www.gov.uk/government/publications/flu-immunisationprogramme-2013-to-2014 ) o Relevant Summary of Product Characteristics (SmPC)and
Patient Information Leaflet (PIL) for the brand of influenza vaccine – available at www.medicines.org.uk
Specialist competencies or qualifications
Continuing education and training
Basic Life Support training or update within the last 12 months
Reference Number:
Valid from:
Review date:
Expiry date: 3
Clinical condition
Clinical condition or situation to which this
PGD applies
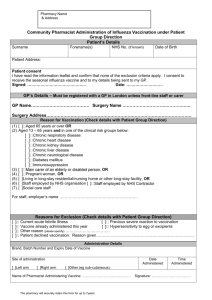
Patient in a defined at-risk group requiring flu vaccination. The Influenza vaccination inclusion criteria are summarised below.
NOTE : This PGD must be read in conjunction with the Green Book chapter on
Influenza. Where information given in the Green Book and individual SmPCs conflict, the guidance given in the Green Book should be followed as it overrides that given in the SmPC
Inclusion criteria
Patients who meet any of the following criteria may be vaccinated:
All those aged 65 years or over (defined as those aged 65 years and over on 31 March 2014 (i.e. born on or before 31 March 1949);
All those aged 13 years to 65 years and in a clinical risk group
Note: The live attenuated influenza vaccine (Fluenz) is the vaccine of choice for children aged 2-17 years, in clinical risk groups, however it is unsuitable for children under the age of 2 years and for those over the age of 2 years with contraindications, such as severe immunodeficiency or egg allergy. In these children, the intramuscular vaccine can be used, unless contraindicated;
Clinical risk groups are: o Chronic respiratory disease:
Asthma that requires continuous or repeated use of inhaled or systemic steroids, or with previous exacerbations requiring hospital admission;
Chronic obstructive pulmonary disease (COPD), including chronic bronchitis and emphysema; bronchiectasis, cystic fibrosis, interstitial lung fibrosis, pneumoconiosis and bronchopulmonary dysplasia (BPD);
Children who have previously been admitted to hospital for lower respiratory tract disease; o Chronic heart disease:
Congenital heart disease;
Hypertension with cardiac complications;
Chronic heart failure;
Individuals requiring regular medication and/or follow-up for ischaemic heart disease; o Chronic kidney disease:
Chronic kidney disease at stage 3, 4 or 5;
Chronic kidney failure;
Nephrotic syndrome;
Kidney transplantation; o Chronic liver disease:
Cirrhosis;
Biliary atresia;
Chronic hepatitis o Chronic neurological disease:
Stroke, or transient ischaemic attack (TIA);
Conditions in which respiratory function may be compromised due to neurological disease (e.g. polio syndrome sufferers);
Clinicians should consider on an individual basis the clinical needs
Reference Number:
Valid from:
Review date:
Expiry date: 4
of patients including individuals with cerebral palsy, multiple sclerosis and related or similar conditions; or hereditary and degenerative disease of the nervous system or muscles; or severe neurological disability; o Diabetes mellitus:
Type 1 diabetes;
Type 2 diabetes requiring insulin or oral hypoglycaemic medicines, diet controlled diabetes; o Immunosuppression due to disease or treatment:
Patients undergoing chemotherapy leading to immunosuppression;
Asplenia or splenic dysfunction;
HIV infection at all stages;
Individuals treated with or likely to be treated with systemic steroids for more than a month at a dose equivalent to prednisolone at 20mg or more per day (any age) or for children under 20kg a dose of 1mg or more per kg per day.
Some immunocompromised patients may have a suboptimal immunological response to the vaccine;
Main carers of an elderly or disabled person, i.e. those who are in receipt of a carer’s allowance, or those who are the main carer, or the carer of an elderly or disabled person whose welfare may be at risk if the carer falls ill;
People living in long-stay residential & nursing homes or other long-stay facilities (not including prisons, young offenders institutions, university halls of residence etc.);
Frontline health and social care workers;
Pregnant women at any stage of pregnancy (first, second or third trimesters).
Reference Number:
Valid from:
Review date:
Expiry date: 5
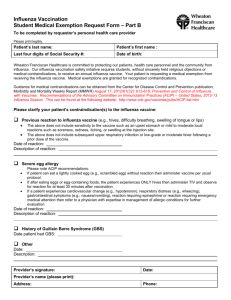
Exclusion criteria
*Current acute febrile illness (Note that if the patient has a minor illness, but there is no fever, then immunisation should proceed);
Individuals with known hypersensitivity to eggs, or egg products – check the SmPC for the individual vaccine, since some vaccines are egg-free;
Individuals with known hypersensitivity to any component or excipient of the vaccine;
Anaphylactic or severe localised or systemic reaction to a previous dose of influenza vaccine;
Consent withheld by patient, parent or guardian;
Seasonal Influenza Vaccination already administered in 2013/14;
Evidence of a worsening neurological condition;
Individuals with Multiple Sclerosis and related conditions or hereditary and degenerative diseases of the Central Nervous System, e.g. Dementia,
Alzheimer’s Disease.
Cautions including any relevant action to be taken
Action to be taken if patient excluded
Action to be taken if patient declines treatment
Individuals with bleeding disorders; especially those on anticoagulant treatment: the intramuscular administration route should NOT be used in patients with bleeding disorders
– the subcutaneous route should be used - see under administration
Advise about avoiding flu and what to do if flu is contracted;
*If patient excluded due to current acute febrile illness advise them (or their parent/guardian) that they can return for immunisation at a later date (offer alternative appointment time);
Inform parents/patients of reason for non immunisation; advise when patient can have the vaccine if applicable;
Signpost to services where they can have a non-NHS immunisation i.e. pay for it themselves if applicable;
Document advice given.
Advise about immunisation and disease complications;
Record refusal in patient record and if possible the reason for refusal;
Advise about protective effects of the vaccine and the risks of infection and disease complications;
Inform or refer to GP.
Details of the medicine
Name, form and strength of medicine
Legal category
Route/method of administration
Trivalent seasonal inactivated influenza vaccine. Suspension for injection in pre-filled syringe.
For further details of vaccines covered by the PGD please refer to Appendix 1 and https://www.gov.uk/government/publications/flu-immunisationprogramme-2013-to-2014
Prescription Only Medicine (POM)
Adults and children over 13 years: 0.5mL
(See note below regarding use outside the terms of the SPC)
Reference Number:
Valid from:
Review date:
Expiry date: 6
Shake vaccine well before use
The vaccine must be stored between +2 and + 8 ºC and protected from light before administration
Dose and frequency
Quantity
Single dose only by intramuscular injection:
Adults and children over 13 years of age - single dose given annually
The preferred site is the deltoid muscle of the upper arm
(offer vaccination in the non-dominant arm), or anterolateral thigh in infants
Note: Individuals with a bleeding disorder should be given the vaccine by deep subcutaneous injection.
Single dose for adults and children over 13 years of age
Single dose for adults and children over 13 years of age Maximum or minimum treatment period
Use outside the terms of the Summaries of Product
Characteristics (SmPCs)
Adverse effects
Common: Pyrexia, nausea, redness, swelling, pain, bruising, hardness at injection site, headache, dizziness, muscle and joint pain, malaise, tiredness, sweating, shivering, fever.
Severe: Hypersensitivity reactions, convulsions
Refer to SmPC and current BNF for full details.
For rare reactions: refer to the Green Book; the current edition can be accessed online from https://www.gov.uk/government/publications/green-book-thecomplete-current-edition
Use the Yellow Card System to report adverse drug reactions
(ADRs) directly to the Commission on Human Medicines
(CHM). Guidance on the use of the Yellow Card System and
Yellow Cards are available in the current BNF or use http://yellowcard.mhra.gov.uk/
Report all significant ADRs to the patient’s GP.
Advice to patient or carer
The vaccine gives 70-80% protection against infection with influenza;
Give the patient a copy of the manufacturer’s patient information leaflet and discuss side effects and their management;
Advise that most reactions usually disappear within 1-2 days without treatment. If the symptoms do not disappear, or the patient experiences other severe symptoms e.g. confusion, persistent drowsiness etc, then they should be advised to contact their General Practitioner or A&E;
Give advice on temperature control;
The Department of Health circular and the Green Book state that none of the influenza vaccines contain thiomersal as an added preservative. However, the SmPC for Fluvirin states
Reference Number:
Valid from:
Review date:
Expiry date: 7
Follow-up
Records to be kept that it contains traces of thiomersal that are left over from the manufacturing process. Check individual package insert for further information;
Refer to SmPCs and current BNF for full list of excipients of the vaccine for potential allergens and potential interactions.
All pharmacists administering the vaccine must ensure the availability of an Anaphylactic Shock Pack or Epinephrine
(Adrenaline) in accordance with local policy and the latest version
(January 2008) of the Anaphylaxis Algorithm http://www.resus.org.uk/pages/reaction.pdf
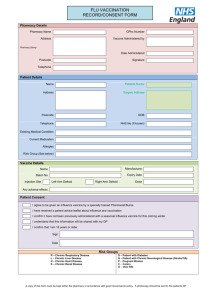
Patient name, address, date of birth and GP details;
Name of vaccine, dose and form administered;
Date administered;
Site of injection;
Manufacturer of product, batch number and expiry date;
Advice given to patient;
Member of staff who administered the medication;
Details of any adverse drug reaction(s) and actions taken including documentation in the patient’s medical record;
Adverse reactions should be reported to the Committee on
Safety of Medicines using the ‘Yellow Card’ reporting system.
Reference Number:
Valid from:
Review date:
Expiry date: 8
Key references
Summaries of Product Characteristics for all brands listed in the above circular.
Available from http://www.medicines.org.uk/emc/
British National Formulary, latest edition
‘Immunisation against Infectious Disease 2006’ (the Green Book) the current edition can be accessed online from https://www.gov.uk/government/publications/green-book-the-complete-currentedition
Reference Number:
Valid from:
Review date:
Expiry date: 9
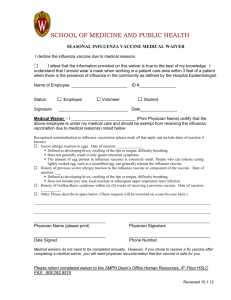
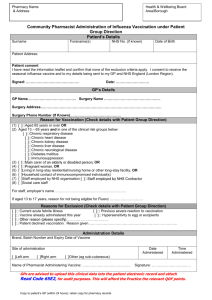
DECLARATION by Pharmacist:
I have been appropriately trained to understand the criteria listed and the administration required to administer seasonal influenza vaccine in accordance with this Patient Group Direction. I confirm that I am competent to undertake administration of influenza vaccine.
Pharmacist’s Name:…………………………….
Pharmacy : ……..………………………..
GPhC/PSNI registration number:……………………….
Expiry Date: ……………………….
Signature: …..………………….. Date: ……………………….
Reference Number:
Valid from:
Review date:
Expiry date: 10
Appendix 1
Vaccines available for the 2013/14 flu immunisation programme
Supplier
Abbott Healthcare
GlaxoSmithKline
Name of product
Influvac Desu
Imuvac
Fluarix
Fluarix Tetra
Janssen-Cilag Ltd
(formerly Crucell UK)
Viroflu
Inflexal
MASTA Inactivated
Influenza Vaccine
(Split Virion) BP
Fluarix
Optaflu
Novartis Vaccines Agrippal
Fluvirin
Optaflu
Vaccine Type
Surface antigen, inactivated
Surface antigen, inactivated
Split virion inactivated virus
Split virion inactivated virus
Surface antigen, inactivated
Surface antigen, inactivated
Split virion, inactivated virus
Split virion inactivated virus
Surface antigen, inactivated, prepared in cell cultures
Surface antigen, inactivated
Surface antigen, inactivated
Surface antigen, inactivated, prepared in cell cultures
Split virion Inactivated virus
Age indications
From 6 months
From 6 months
From 6 months
From 3 years
From 6 months
From 6 months
From 6 months
From 6 months
From 18 years
From 6 months
From 4 years
From 18 years
From 5 years Pfizer Vaccines CSL Inactivated
Influenza Vaccine
Enzira
Sanofi Pasteur MSD Inactivated
Influenza Vaccine
(Split Virion) BP
Split virion Inactivated virus
Split virion, inactivated virus
From 5 years
From 6 months
Reference Number:
Valid from:
Review date:
Expiry date: 11