High fiber diet
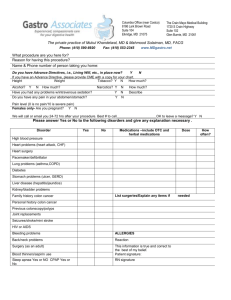
advertisement

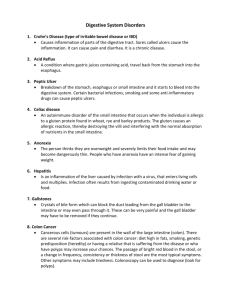
Lower Gastrointestinal Disorders Common Intestinal problems 1-Constipation • Difficulty passing stools or infrequent bowel movements; often diagnosed when individual has a fewer than 3 bowel movements/week Other symptoms may include: • The passage of hard stool • Excessive straining during defecation. Constipation – Causes • Low food intake • Low-fiber diets • Inactivity • Certain disorders : hypothyroidism, diabetes mellitus, and chronic renal disease • Neurological conditions may cause motor problems in the intestine • Higher among women especially during pregnancy • Increases somewhat with aging 1 Side effects of medications and dietary supplements such as : 1. aluminum-containing antacids, 2. iron and calcium supplements. Constipation – Treatment Gradual increase in fiber – wheat bran, fruits ,vegetables and fiber supplements 20-25 grams/day High fiber diet : increase stool weight promote a more rapid transit of materials through the colon Add prunes or prune juice to the diet because it have mild laxative effects Make sure that patient has sufficient fluid intake to prevent dehydration, which draws water from the colon to increase hydration in the rest of the body. Increasing daily exercise Laxatives may be prescribed Laxatives work by: 1. Increasing stool weight 2. Increasing water content of the stool 3. Stimulating peristaltic contractions 2 2- Diarrhea • Diarrhea is characterized by passage of frequent, watery stools In severe cases may cause dehydration and electrolyte imbalances If chronic, may lead to weight loss and malnutrition • Acute diarrhea: Lasts for less than several weeks. • Chronic diarrhea: Lasts for a month or longer. Types and causes of diarrhea a-Osmotic diarrhea : Unabsorbed nutrients attract water to the colon and increase fecal water content The usual causes include: • Lactase deficiency • High intake of poorly absorbed sugars like sorbitol, manitol or fructose which retain fluids in the colon b- Secretory diarrhea: • Intestines are stimulated to secrete fluid that exceeds the colon’s capacity for reabsorption • This type is often due to bacterial food poisoning, intestinal inflammation c- Motility disorders : cause diarrhea by acceleration of entry of fluids into the colon, that shortens the contact time needed for fluid reabsorption 3 Nutrition therapy of diarrhea • The nutrition prescription depends on the medical diagnosis and severity of the condition. 1-Low-residue, low-fat, lactose-free diet: 2-Low residue diet limits foods that contribute to colonic residue, such as those with large amounts of fiber, lactose, fructose. 3-Avoid gas-producing foods because it can increase intestinal distention and cause additional discomfort 4-Avoid of fatty foods because it aggravate diarrhea 5-Avoid coffee and tea because caffeine stimulates GI motility and reduce water reabsorption 6-Oral Rehydration therapy can be used in severe cases Containing water, salts, glucose or sucrose 7-Commercial sports drinks are generally not recommended because their sodium content is too low .May be used with salty snack 8-IV solutions are used in extreme dehydration. 4 3- Fat Malabsorption • Fat is the nutrient most frequently malabsorbed because both digestive enzymes and bile must be present for its digestion • It develops when an illness interferes with the production or secretion of either bile or pancreatic lipase • It develops also as a result of cancer radiation therapy which damage the intestine mucosa. • Motility disorders in the stomach of intestine cause fat malabsorption because they prevent the normal mixing of dietary fat with digestive enzymes. • Fat Malabsorption is often evidenced by steatorrhea 5 Steatorrhea: Excessive fat in the stools resulting from fat malabsorption; characterized by stools that are loose, frothy, and very bad smell due to a high fat content Consequences of Fat Malabsorption • Loss of energy and fatty acids • Loss of Fat-soluble vitamins – A, D, E, K • Loss of Minerals such as Calcium, magnesium, zinc because minerals form soaps with unabsorbed fatty acids. • Bone disease • The risk of Kidney stones increase • The oxalates in foods ordinarily bind to calcium in the small intestine and are excreted in the stool. • If calcium instead binds to unabsorbed fatty acids, oxalates are free to be absorbed into the blood and are excreted in the urine. • The risk of developing oxalate stones increases when urinary oxalate levels are high. Dietary adjustments for fat malabsorption • Fat restricted diet is recommended to relive the symptoms • Fat should not be restricted more than necessary • Medium-chain triglycerides which do not require lipase or bile for digestion and absorption may be used .It does not provide EFA and give 8.1 kcal/g 6 4-Lactose Intolerance • High incidence: approximately 75% of population worldwide Rarely serious and Most individuals (with lactose intolerance) can tolerate milk if consumed with other foods & limit amount consumed at one time. Cause of lactose intolerance • Lactose intolerance is the inability to digest and absorb lactose (the sugar in milk) that results from reduction or loss of lactase, enzyme that digests lactose in milk products Symptoms of lactose intolerance Symptoms of lactose intolerance usually begin 30 minutes to two hours after eating or drinking foods that contain lactose. Symptoms are usually mild, but they may sometimes be severe. Common signs and symptoms include: • Diarrhea • Nausea • Abdominal cramps • Bloating • Gas Dietary management of lactose intolerance • In the mild cases ,gradually increased consumption of lactosecontaining products • Divide milk intake throughout the day 7 • Consume milk with meals • Chocolate milk may be better tolerated than plain • Aged cheeses well tolerated especially hard cheese, which contains very small quantities of lactose and is usually very rich in calcium (e.g. parmesan, cheddar). • Yogurts with live bacterial cultures that aid in lactose digestion • Addition of lactase preparation to milk or use of enzyme tablet before consumption • patients can also try lactose-free milk ”soy milk” 5-Celiac Disease A condition characterized by an abnormal immune reaction to wheat gluten that causes severe intestinal damage and nutrient malabsorption. Consequences of celiac disease • The immune reaction to gluten causes severe damage to the small intestine mucosa. • Absorptive surface appears flattened due to shortening or absence of villi. • Results in malabsorption of macronutrients, fat-soluble vitamins, electrolytes, calcium, magnesium, zinc, iron, folate, and vitamin B12Develop anemia and low bone density. • Individuals with celiac disease who do not eliminate gluten from the diet are at increased risk of lymphatic and intestinal cancer. 8 Symptoms of celiac disease • Diarrhea • Steatorrhea • Flatulence • Lactase deficiency may result from mucosal damage • children often have stunted growth, underweight • Severe rash • Individuals with celiac disease who do not eliminate gluten from the diet are at increased risk of lymphotic and intestinal cancer. Medical nutrition therapy of celiac disease • Lifelong adherence to a gluten-free diet • Avoid lactose-containing foods if lactase deficiency is found. • Eliminate wheat, rye, barley 9 • Read labels carefully – replace bread, pasta, cereal • Can be social liability • Diet counseling Inflammatory Bowel Disease • Conditions having patterns of inflammation. It is Complex set of genetic and environmental factors (bacteria – irritant- viral) contribute to the development but the exact cause is unknown. Occurs most frequently in persons 15-25 years of age 1-Ulcerative Colitis • An inflammatory bowel disease that involves the colon. Inflammation affects the mucosa and submucosa of the intestinal wall.Involves rectum and extends into the colon • Symptoms of Ulcerative colities: Diarrhea Rectal bleeding Abdominal pain 10 Normal colon Ulcerative Colitis Complications – Ulcerative Colitis: • Weight loss ,fever, weakness are common when most of the colon is involved • A decrease in the oral intake of nutrients is a common symptom and is often due to abdominal pain fever 11 • Mucosal inflammation and its associated diarrhea or bleeding lead to a loss of protein, blood, minerals, electrolytes and trace elements. • severe disease is often associated with anemia, dehydration, fluid & electrolyte imbalances • High risk of developing colon cancer – colectomy may be performed (20-25%) Medical therapy for ulcerative colitis: • Drug therapy Antidiarrheal agents Immunosuppressants Anti-inflammatory agents • Surgical interventions Nutrition therapy for ulcerative colitis: The primary goal are to: • Replace fluid and electrolyte losses • Correction of deficiencies due to protein and blood losses • Low-fiber diet may reduce irritation by minimizing fecal volume • Bowel rest if colon function severely impaired : food and fluids may be withheld and fluids and electrolytes supplied intravenously until colon function is restored. 12 13 Conditions Affecting the Large Intestine 1-Diverticular Disease of the colon • Development of pebble-sized herniations in the intestinal wall known as diverticula.Most often occurs in sigmoid colon • Prevalence increases with age • Development is influenced by the amount of dietary fiber a person consumes • Increasing the stool bulk by high fiber intake may reduce the workload of the intestine muscle that moves the wastes through the colon. • Low-fiber diet increases the pressure in the intestine, causing small areas of the intestinal wall to balloon outward over time. 14 Diverticulitis : Localized inflammation or infection develops in the area around a diverticulum • It is the most common complication of diverticulum • Thought to result from hardened fecal matter that abrades the mucosal lining Causes inflammation May cause microperforation – infection – fistulas – peritonitis Symptoms of Diverticulitis • Persistent abdominal pain • Fever • Constipation • Bleeding • Nausea & vomiting Nutrition therapy for diverticular disease • Gradual increase in dietary fiber – insoluble fibers • Avoid nuts, popcorn, and foods that contain seeds to prevent disease progression • In mild cases clear liquid diet may be advised initially that is gradually progressed to low-fiber, low-residue diet until inflammation and bleeding subside • For severe cases bowel rest is necessary ( IV). Oral intake are gradually started as condition improves. 15 Medical treatment for diverticular disease • Pain relief medication • Antibiotics • Surgical interventions may be needed for affected portion of colon (colectomy 16