O78 Development of lower limb peripheral vascular disease in the
O78
Development of lower limb peripheral vascular disease in the diabetic haemodialysis population – a 24 year retrospective study
Segun Babafemi 1 , Jocelyn Berdeprado 2 , Suresh Mathavakkannan 2 , Ken Farrington 2 , Paul
Warwicker 2 1. Visiting ISN clinical fellow, LASUTH, Lagos, Nigeria 2. Lister Renal Units,
East and North Hertfordshire NHS Trust
Introduction: There is a significantly increased burden of non-traumatic lower-extremity amputation in the diabetic ESRF population. The incidence is 10 times higher than non ESRF diabetic patients, and 25 times the incidence of non-diabetic population. An analysis of amputations in the US Medicare dialysis programme (‘91 to ‘94) found a crude rate of 4.3/100 pt yrs for all ESRF patients, and 13.8/100 for diabetic ESRF patients. We studied 24 years of data to establish the burden of lower limb vascular disease in our haemodialysis population.
Demographics and analysis: Approx 30% of our dialysis population are diabetic, ranging from
22.4% to 42.2% in our satellite units. Of the diabetic population 54% are Caucasian, the majority of the others are of South East Asian origin. 11% were smokers.
A vascular intervention was defined as an amputation event (either whole limb, transmetatarsal or toe), a major debridement, a surgical or radiological revascularisation, including an arterial angioplasty +/- stent, and embolectomies. There were also a small number who in extremis, were offered but declined amputation, preferring palliation. This too was counted as a ‘vascular intervention’. Interventions for ischaemia arising from vascular access were not included.
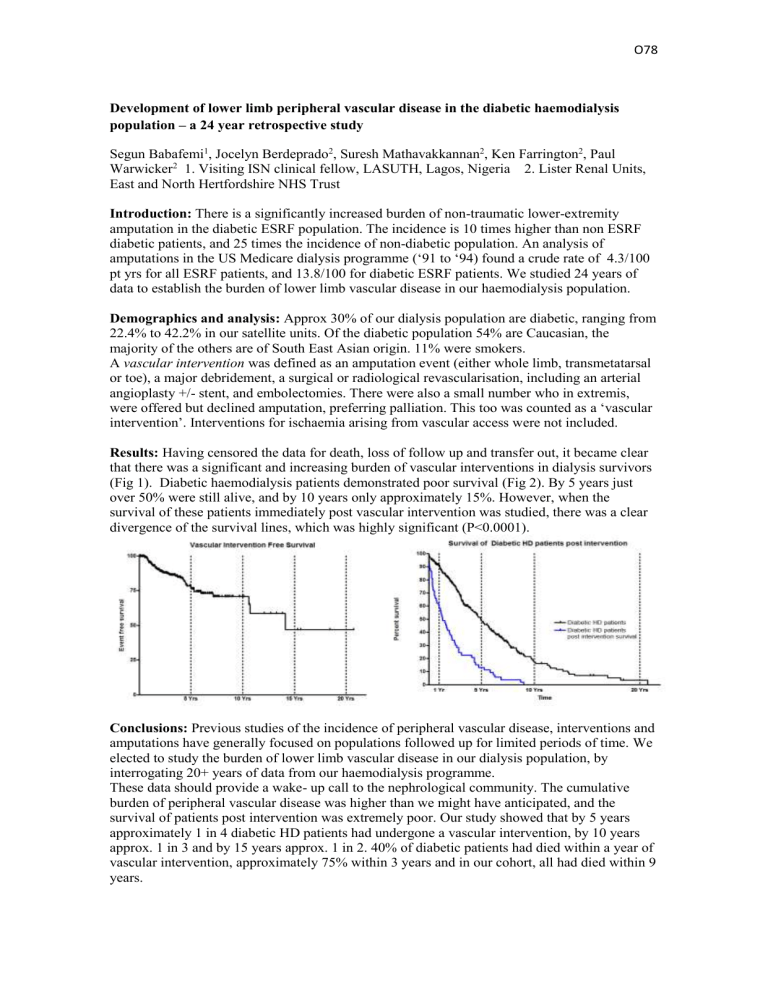
Results: Having censored the data for death, loss of follow up and transfer out, it became clear that there was a significant and increasing burden of vascular interventions in dialysis survivors
(Fig 1). Diabetic haemodialysis patients demonstrated poor survival (Fig 2). By 5 years just over 50% were still alive, and by 10 years only approximately 15%. However, when the survival of these patients immediately post vascular intervention was studied, there was a clear divergence of the survival lines, which was highly significant (P<0.0001).
Conclusions: Previous studies of the incidence of peripheral vascular disease, interventions and amputations have generally focused on populations followed up for limited periods of time. We elected to study the burden of lower limb vascular disease in our dialysis population, by interrogating 20+ years of data from our haemodialysis programme.
These data should provide a wake- up call to the nephrological community. The cumulative burden of peripheral vascular disease was higher than we might have anticipated, and the survival of patients post intervention was extremely poor. Our study showed that by 5 years approximately 1 in 4 diabetic HD patients had undergone a vascular intervention, by 10 years approx. 1 in 3 and by 15 years approx. 1 in 2. 40% of diabetic patients had died within a year of vascular intervention, approximately 75% within 3 years and in our cohort, all had died within 9 years.