Colorectal cancer includes cancerous growth involving the colon
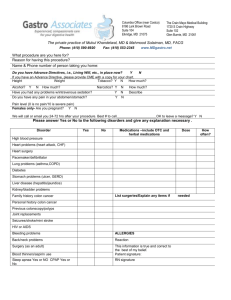
advertisement

Colorectal cancer includes cancerous growth involving the colon, rectum and anus. It is one of the leading causes of cancer mortality worldwide. Colorectal cancers arise from adenomatous polyps in the colon. These mushroom shaped growths are usually benign, but some develop into cancer overtime. Certain risk factors can predispose a person to colorectal cancer. These include age, polyps in the colon, history of cancer, heredity, smoking, diet, physical inacativity, viruses, inflammatory bowel disease, alcohol and environmental factors. Colorectal carcinoma is usually found in individuals of greater than 50 years of age. Risk of developing cancer, in other words, increases with age. Rarely will it be seen in young adults or adolescents. Hereditary nonpolyposis colon cancer (HNPCC) is one cancer of cancer occurring in such young age group and usually occurs in the proximal colon. Histopathologic findings present with poorly differentiated appearance with no difference against sporadic tumor of the colon occurring on the same age group. In adults in their 30’s, familial polyposis coli predisposes individual to have colorectal cancer. Multiple polyps usually develop at around age of 25 and later on develop into cancer before age 40. Symptoms of patients with colorectal carcinoma are usually dependent on the site of the space occupying lesion. Colorectal carcinoma of the proximal bowels do not usually present with obstructive symptoms initially until it approaches a more advance stage. Mechanism of the presentation is due to the fact that stools are liquid in the more proximal part. On the other hand, lesions of the distal colon (transverse colon and left descending colon) present with impingement of stool movement due to the more formed stools present on the said anatomical area. This results in abdominal cramping, change in the character of the stools like its caliber and obstruction that may lead perforation of the colon. In our patient, the patient presented with a 5 week history of crampy abdominal pain of the left lower quadrant accompanied by goat stool-like brownish blood-streaked stools. This presentation is typical of colorectal cancer and true enough when the patient was admitted is our institution due to severe right lower quadrant pain, subsequently diagnosed with appendicitis, a rectosigmoid mass was initially found. Upon opening of the abdomen at the operating room, there was a fecaloid peritoneal fluid. The appendix was approximately 4 x 1 x1 cm, bulbous. There was a 20 cm segment of the rectosigmoid which had a firm, circumferential mass almost completely obstructing the lumen. Multiple incision biopsies was done. There was a 0.7 x 0.7 cm perforation at the antimesenteric side of the sigmoid. There were multiple mesenteric peritoneal implants that are all whithish and grain-like. There was a 1 x 1 cm cystic nodule seen in the omentum at the area of the right upper quadrant. Biopsy of the rectosigmoid mass and peritoneal implants was done. Histopathologic results showed poorly differentiated adenocarcinoma with signet ring cell feature. Final diagnosis of the patient on discharge was poorly differentiated mucinous adenocarcinoma of the rectum and descending colon stage IV. TNM classification and Duke Classification are the most common staging systems used for colorectal cancer. For our patient, intra operative findings of peritoneal implants and a nodule in the omentum aside from the main mass puts the patient on Duke Classification D or TNM stage IV. Development of colon cancer usually develops after development of polyps and only become clinically significant after 5 years from onset of development. Aside from that, only a minority of these polyps turned out to be malignant. In fact, only less than 1 percent of the polyps ever become malignant. Therefore arising malignancy arising from polyps, considering the factors mentioned above, will most probably develop in later stages of life. According to the Centers for Disease Control and Prevention, colon cancer is very rare in below age of 20. Only about one out of one million children will develop colon cancer. Those who do develop colon cancer usually have some type of hereditary condition that causes the formation of abnormal cells. Those children who do develop colon cancer usually have some type of hereditary condition that causes the formation of abnormal cells. Colon cancer in children is often linked to a family colorectal cancer syndrome, or inherited pattern. There is an increasing risk of colorectal cancer in members of families with a family history of intestinal polyps, which can lead to the development of multiple adenomatous polyps (benign tumors). Juvenile polyps are not associated with an increased incidence or risk of cancer. These hereditary conditions are as follow: Hereditary Non-polyposis Colorectal Cancer (HNPCC) or Lynch Syndrome Hereditary nonpolyposis colorectal cancer, often called HNPCC or Lynch Syndrome, is an inherited cancer syndrome that affects the digestive tract, reproductive tract and other major organs. People with Lynch Syndrome have an increased risk of cancers of the stomach, small intestine, liver, gallbladder ducts, upper urinary tract, brain, skin, and prostate. Women with this disorder also have a greatly increased risk of endometrial and ovarian cancer. Colon cancers develop from adenomatous polyps that occur at an earlier age than do colon polyps in the general population. Although previously thought of as a disease presenting in adulthood, teenagers from Lynch syndrome families can develop active symptoms, including colon cancers. Lynch Syndrome adenomas do not develop in large numbers but progress to cancer more quickly than the occasional adenomas found in otherwise healthy people. Lynch Syndrome is caused by a genetic mistake, or mutation, in one of four blueprint genes that make DNA repair proteins. When the DNA repair system does not work properly, harmful DNA mistakes are passed on as the cells multiply leading to disorganized growth and the development of cancer. Although mutations in these genes predispose individuals to cancer, not all people who carry these mutations develop cancerous tumors. Careful follow-up, including examination of the large intestine or colon (colonoscopy), have been shown to reduce the risk of this disease. Familial Adenomatous Polyposis (FAP) Familial adenomatous polyposis, is an inherited colorectal cancer syndrome that can be passed from one generation to the next by a specific error or mutation in the genetic code of the APC gene. Virtually everyone that carries a mutation of the APC gene will eventually develop cancer in the lower part of the digestive system, including the large intestine (colon) and rectum. This disease can become active in childhood with the development of adenomatous polyps causing bleeding with bowel movements, diarrhea, or abdominal pain usually in the mid teenage years however, exceptions are the rule. Colon adenomas can progress to cancer without causing apparent symptoms and can be silent killers. The average age for colon cancer is about 39 years. However, colon cancer can develop during the teen years and can develop in the absence of digestive problems. Some people have a variant of the disorder, called attenuated familial adenomatous polyposis, in which adenomas are fewer in number and develop later in life, yet these patients also have significant risk of colorectal cancer but at a later average age of about 55 years. Surgery can reduce the colon cancer risk and is currently the best therapy for this disease. Patients with FAP are at risk for cancers and tumor growths elsewhere in the digestive tract and body. Close follow up with regular checkups is an important way to avoid further complications from this disease. Juvenile Polyposis Syndrome (JPS) Juvenile polyposis syndrome is an inherited condition that is characterized by the development of hamartomatous polyps throughout the digestive tract. The term juvenile polyposis refers to the type of polyp (juvenile polyp) that is found on pathology examination rather than the age at which people are diagnosed with JPS. The number of polyps a person has during his or her lifetime can range from none to hundreds and polyp development can begin at any time in life from early infancy to the geriatric years. Most juvenile polyps are benign (noncancerous), but on occasion these polyps can become cancerous with JPS families having an increased risk of colorectal, stomach, small intestine, or pancreatic cancer. Genetic mistakes in two genes (BMPR1A and SMAD4) have been linked to roughly half of the families with this syndrome meaning other causative genes remain to be identified. This syndrome is known for its unpredictability. Although mutations in the JPS genes predispose individuals to polyp development and colon cancer, not all people who carry these mutations will develop colon cancer or even polyps. For these reasons, gene testing is the only reliable way to know who does and does not have this disease in JPS families with a known gene mutation. Careful follow-up, including upper and lower endoscopy (colonoscopy), can remove polyps for examination and help to reduce the risk of cancer from this disease. Peutz Jeghers Syndrome (PJS) Peutz-Jeghers syndrome is an inherited disorder with a 50% chance of being passed from one generation to the next. Two findings make up this disease: intestinal hamartomatous polyps and blue/black freckling or macules that can be seen on the lips, mouth, nostrils, hands, feet and genitalia. This syndrome has a significant risk of digestive and other cancers that is 15 times greater than that of the general population. The pigmented macules are usually not present at birth but become noticeable within the first 5 years of life. In some individuals, the freckles fad with age, however the disorder can be present in the absence of skin pigmentation. The gastrointestinal polyps found in Peutz-Jeghers Syndrome are typical hamartomas which can be large and bulky causing bleeding, pain, and blockage of the intestinal tract from “telescoping” of the bowel over a polyp resulting in intussusception of the small intestine. The majority of children and adolescents with PJS present with crampy pain, vomiting, and bowel obstruction resulting in emergency surgery to correct the intussusception. Newer management techniques are now designed to identify and remove the small intestinal polyps prior to the occurrence of symptoms thereby hopefully avoiding emergency surgery. This disease is caused by a mistake/mutation in the STK11 or LKB1 gene. Using newer techniques, it is now possible to identify the mistake in over 90% of individuals that have polyps and lip freckles. Long term follow up and surveillance can reduce the cancer risk of this disease.