Immunization Provider Focus Groups: Communication
advertisement

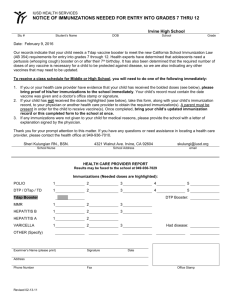
Immunization Provider Focus Groups: Communication Approaches and Needs A Report of Key Findings CDPH IMMUNIZATION BRANCH, INFORMATION & EDUCATION SECTION December 1, 2012 Table of Contents Executive Summary Page 2 I. Goals of Focus Groups Page 5 II. Methodology Page 5 III. Findings: OB-GYN Physicians and Nurse Practitioners Page 9 IV. Findings: Pediatricians and Family Physicians Page 12 V. Recommended Actions Page 23 Appendix 1: Pediatric and Family Medicine Survey Results Page 25 Appendix 2: Appendix 2: Obstetric Medicine Survey Results Page 31 Appendix 3: Follow-up Survey with Medical Assistants Page 35 Acknowledgments This report was prepared by Rebeca Boyte, MAS, and Tammy Pilisuk, MPH. Appendix three, which includes results from a follow-up survey with medical assistants, was prepared by Leslie Heyden. Focus groups were conducted by Martin and Stowe, under contract with Schlesinger and Associates, and under the direction of the California Department of Public Health (CDPH) Immunization Branch, Information and Education (I&E) section. Thanks to the I&E Health Education team, which assisted in the development of the focus group questions and monitored the majority of the groups. Special thanks to Rebeca Boyte, project lead for this effort, Leslie Heyden, for developing and conducting a follow up survey with more than 1,000 medical assistants, and our deep gratitude to the many providers who attended the focus groups sharing their insights, experience, and time to help us learn more about provider communication needs in California. 1 Immunization Provider Focus Groups: Communication Approaches and Needs Executive Summary This report was compiled by the CDPH Immunization Branch based on 12 focus groups and 4 indepth interviews conducted with healthcare providers during May-June 2012. The groups were segmented by provider type and included OB-GYN Physicians, OB-GYN Nurse Practitioners, Pediatricians, Family Physicians, Pediatric Nurse Practitioners, and Physician’s Assistants. All providers completed a short survey prior to group discussion. Four 60-minute interviews were conducted with providers in rural areas. The sessions were conducted by Martin & Stowe, under contract with Schlesinger & Associates. The project was under the direction of the CDPH Immunization Branch, I&E Section. The goal of this research was to identify key strategies providers use to communicate with patients and parents about immunizations, obstacles they face, and to assess needs for additional support from CDPH in the form of handouts, videos, and clinician training. As such, select Immunization Branch educational materials were reviewed for usefulness in aiding providers in informing themselves, their staff, and patients on key immunization issues. Special attention was given to seeking out the most effective ways to communicate with patients or parents who are hesitant to vaccinate. The California Department of Public Health, Immunization Branch will use the key findings from this report to enhance communication strategies and inform the development and updating of educational materials and training resources. Key Findings General Providers were unfamiliar with CDPH materials, but liked them (when materials were shared). Providers want a mechanism to order hard copies for their practices. Providers believe that personal stories are an effective way to motivate vaccine-hesitant patients and parents to get immunized. Referring to trusted resources (i.e. CDC, WebMD, CHOP), including a web link to the ShotbyShot.org story-bank was favored. OBGYNs OB-GYNs support immunizations and typically check patient immunization status. Many do not immunize onsite due to infrastructure and reimbursement barriers. They typically refer patients to a pharmacy or to their Primary Care Physician (PCP) to get vaccinated. OB-GYNs want to order and share the CDPH pregnancy brochure with their patients. OB-GYNs would like ongoing education and training to keep up with changes in vaccine schedules and recommendations. 2 Immunization Provider Focus Groups: Communication Approaches and Needs Pediatricians, Physician’s Assistants, Pediatric Nurse Practitioners, and Family Physicians Provider Communication Issues Providers frequently encounter parental concerns about vaccines and vaccine safety. These include fears about autism, side-effects, overwhelming the immune system, vaccine ingredients (e.g. aluminum), and beliefs that natural immunity is best. Parents also fear that profit is a motive that is influencing vaccinators. Providers continue to serve vaccine-refusing families and accommodate alternative schedules to appease their concerns. Provider Communication Strategies Providers have developed their own communication strategies to address most vaccine concerns. Most, who have been practicing for some time, believe they have adequate up-to-date facts on vaccine safety concerns. Those with experience also find it effective to relate personal stories about VPDs. They had the greatest amount of difficulty in convincing parents to get their children immunized against HPV. Focusing on cancer-prevention (rather than STDs), emphasizing the coverage for an expensive vaccine, and showing graphic photos of possible cancers or genital warts were felt to be effective persuaders. The prenatal interview is a good opportunity to discuss any concerns regarding vaccines. Most pediatricians offer prenatal interviews and are supportive of discussing immunizations during these visits, but only a few parents are scheduling prenatal interviews. Provider Training Needs Doctors and nurses receive adequate immunization-related training for themselves from multiple sources. In contrast, they believe basic training for medical assistants is needed on vaccinepreventable diseases, immunizations, and understanding common misconceptions. Materials Review The California Immunization Coalition’s vaccine safety suite of materials was most useful for well-educated parents, medical assistants, and new providers. CDPH provisional “blocks schedule” was strongly favored as a tool to educate parents in the clinic setting. Some providers also wanted a smart phone or web-based application option to customize the schedule with individual immunization intervals for parents—while staying within the ACIP guidelines. Providers welcome handouts and favor referrals to trusted resources and the ShotbyShot.org story gallery for vaccine-hesitant parents. 3 Immunization Provider Focus Groups: Communication Approaches and Needs “Whooping Cough is on the rise in California” flyer was seen as a great model for using personal stories effectively in print. The CDPH pertussis and measles fact sheets for providers were not favored. These were seen as too wordy and complex. ShotbyShot.org stories were favored as a resource for parents to view at home or in a class setting. Other recommendations included exploring new electronic applications for providers and patients, and serving the needs of low-literacy and ethnically/linguistically diverse populations in California. Highlights of Recommended Actions Below is a list of recommended actions “in brief,” based on findings from the focus groups. A more detailed description of each recommendation is provided on page 23 at the end of this report. GENERAL 1. Partner with California medical associations to promote CDPH materials. 2. Promote CDPH’s Vaccine Safety Fact Sheet for Medical Assistants. 3. Develop or promote training tools on vaccine-preventable diseases and a “Vaccines 101” resource for medical assistants. OB-GYNS 4. Promote CDPH’s “Immunizations for a Healthy Pregnancy” brochure to OB-GYN practices in California. 5. Partner with key organizations to encourage women to schedule a pediatric prenatal interview. 6. Ensure that HPV vaccine messaging does not imply that disease prevention is 100%. 7. Provide training on immunization recommendations for OB-GYNs and their clinical staff. PEDIATRICIANS AND FAMILY PHYSICIANS 8. Develop materials to encourage pregnant women to schedule a prenatal pediatric interview. 9. Work closely with prenatal health professionals and programs to raise awareness among parents about the prenatal pediatric interview. 10. Promote vaccine safety materials for providers to medical training and residency programs. 4 Immunization Provider Focus Groups: Communication Approaches and Needs 11. Adapt the “alternative schedule” vaccine safety brochure for a parent audience. 12. Create a new version of the vaccine safety brochure for lower-literacy parents. 13. Create a simple handout to promote the ShotbyShot.org website. 14. Create a suite of single-sheet disease-specific flyers. 15. Ensure that materials for providers are visually appealing, not text-heavy. 16. Create a poster featuring vaccine-preventable diseases for clinic exam rooms. 17. Develop material for young adults with disease images. 18. Finalize and approve CDPH provisional “blocks schedule.” 19. Encourage pediatricians to notify local obstetricians, midwifes, and childbirth educators regarding their provision of prenatal pediatric appointments. 20. Work with the CDC and AAP to encourage pediatricians to discuss immunizations with expectant parents during the pediatric prenatal visit. I. Goals of Provider Focus Groups To identify: Providers’ immunization communication and training needs Materials deemed valuable and those that need improvement Health professionals willing to participate in a provider review panel for future endeavors II. Methodology Recruitment Provider participation was recruited through our vendor, Schlesinger and Associates. The firm used contact information from purchased lists to recruit six different types of providers: Pediatricians, Pediatric Nurse Practitioners, Family Physicians, Physician Assistants, OB-GYNs, and OB nurses. Those recruited included a spectrum of private practice, large group (e.g., Kaiser Permanente), and clinic based providers. Per our recruitment requirements, nearly 75% of the participants worked primarily with minorities, including African Americans, Native Americans, and Latinos. All recruited providers offered immunizations. Recruitment also considered geographic distribution, with groups representing the San Francisco Bay Area, Central Valley (Fresno), and Los Angeles. For the focus groups in Fresno, Schlesinger subcontracted with Nichols Research, another California-based research 5 Immunization Provider Focus Groups: Communication Approaches and Needs company. To maximize outreach and limit costs, four in-depth phone interviews were used to capture information from rural providers (serving San Joaquin, Placer, Nevada and Kern Counties) in order to identify any unique challenges or preferences (although, ultimately, no discernable urban-rural differences were observed). Group Composition A total of 74 health care professionals participated in the focus groups and four were interviewed via telephone (Figure 1). Their practice experience spanned from 4 years to 35 years. Most groups included a spectrum of both seasoned and newer (4-9 years) practitioners. The vast majority of the participants worked in “office” (n= 50 or 64%) or “clinic” (n=20 or 26%) settings. Only eight (10%) worked in a hospital setting. The majority of the pediatric nurses (61%), pediatricians (63%), and family physicians (57%) participated in the Vaccines for Children Program (VFC). None (0%) of the OB nurse practitioners participated in VFC. Only one obstetrician serving the rural community of Placer County participated in the VFC Program. Each group was stratified by specialty and clinical license, with approximately five to seven participants in each of the 12 group sessions held. Topics and materials remained the same for pediatricians and family physicians. OB-GYNs and OB nurses were asked to review different materials, including immunization information for pregnant women. 6 Immunization Provider Focus Groups: Communication Approaches and Needs Figure 1. Total Number of Participating Healthcare Providers Summary of Focus Groups Conducted 5 focus groups in LA: 5 focus groups in SF: 2 focus groups in Fresno: 4 telephone interviews: Pediatricians (n=5) Pediatricians (n=7) Pediatricians (n=6) Rural Pediatrician (n=1) Pediatric Nurse Practioner (n=7) Pediatric Nurse Practitioner (n=6) 13 OB Nurses (n=5) OB Nurse Practioner ( n=7) 12 OB Physicians (n=7) OB Physicians (n=6) Family Physicians (n=7) Family Physicians (n=5) Total 19 Rural OBGYN Physician (n=1) 14 Rural Family Physicians (n=2) 14 Physician Assistants (n=6) 6 Total= 78 Conducted May-June 2012 Each group approximately 1.5 hours Individual phone interviews 60 minutes -------------------------------------------------------------------------------------------------------------------------Survey Instrument Before each group started, participants were asked onsite to complete a survey. Questions related to pragmatic issues such as the ability to print or download color materials at the office, sources they use to keep up-to date on changing immunization schedules, and opinions on the importance of a prenatal pediatric interview with expectant parents. The majority (60%) of participants indicated that the percentage of vaccine-hesitant parents they see is less than 10%. None saw 50% or more vaccine-hesitant parents. About half of all those surveyed were interested in receiving CDPH materials. Survey results were aggregated and summarized at the end (please see Appendix 1 and 2). 7 Immunization Provider Focus Groups: Communication Approaches and Needs Moderator and Guide For consistency across all groups and interviews, one professional moderator was hired to test materials and gather participants’ impressions and ideas. The moderator was not a subject matter expert but had considerable experience in leading focus groups with both healthcare professionals and consumers. Before the first group, CDPH staff met with the moderator to review key concepts and ensure that input and ideas would be captured effectively. Each group lasted 1.5 hours and had a similar structure. As an ice-breaker the moderator had all participants introduce themselves and describe how long they had been practicing. The moderator used a structured guide, prepared by CDPH staff, to lead the groups and engage them in giving feedback to immunization education materials presented. Tools and Engagement Strategies The moderator used the image below as a likert-type scale for each participant to rate how much they like or disliked a particular material. These were described as “embracing,” “touching,” “looking,” “walking away,”and “running away.” Whenever possible, CDPH staff observed the initial focus groups in San Francisco. In this way, staff was able to text the moderator and give real-time suggestions for pursuing key discussion items. Staff could briefly consult with the moderator outside the room, as needed, while participants were reading materials. A TV monitor was used to play 2-3 minute video personal stories and to elicit comments on whether these were felt to be useful and how they might be used by clinicians. A standard flip chart was used to capture key words and phrases during the groups. These were also used to elicit input on what an “ideal” immunization information tool might look like, encouraging participants to describe their ideas to meet their patients’ educational needs. Sessions were recorded and transcribed after all groups were conducted. CDPH staff used all available input to prepare this final report: the moderator’s summary, transcriptions (including selected quotes), and survey findings. 8 Immunization Provider Focus Groups: Communication Approaches and Needs III. Findings: OB-GYN Physicians and Nurse Practitioners A. OB-GYNs Value Immunizations—whether they provide them or not Most doctors and nurses routinely check new patients’ (whether considering pregnancy or not) immunization statuses and advise vaccination. B. Referring Patients to Pharmacy or Primary Care Physician Common “I think we should be encouraging vaccination. I’m pro-vaccination. I believe it’s one of the most important health measures we’ve ever done…That doesn’t mean we as individuals have to be the ones giving it… But I think part of our discussion with our patients should be, are you up to date on your vaccinations? And it’s part of our new history form.” “I give them a prescription, they go across the street [at a pharmacy], get the vaccine, come back, and all of it’s done.” B. Insufficient Reimbursement is a Barrier “If it’s a lot of money – am I going to be competing with Walgreens for flu shots? It isn’t worth my time. You can go to Walgreens for $20 and get a lot of things. You can get a shingles shot at Walgreens cheaper than I can sell it to a patient. So why bother?” “If they want MMR, Hep B, they have primary care. But I advise them to get it, I just don’t offer it.” “I used to stock HPV and then it just got expensive to stock it because I wasn’t being reimbursed as much as I thought I was going to be.” “The only vaccine I give is Gardasil. The rest of the vaccines are just not worth the trouble in buying, stocking, ordering, making sure they’re in date, giving it. It just isn’t worth my trouble.” “It’s underpaid.” “…And just because I don’t carry it, because I don’t find it cost effective, I’m still going to talk about it. I’m going to say it’s incumbent upon you…” 9 Immunization Provider Focus Groups: Communication Approaches and Needs Review of Patient Materials/Handout Needs 1. Single Sheet Disease Pieces Desired Consensus to include: HPV, Tdap, Hep B, MMR and Varicella From a neutral public health source, not a drug company Preference expressed that disease images and possibly personal stories be included “It just shouldn’t come from Merck. I hand them out, but it is a little cheesy.” “I’d rather have something that’s created by the Department of Public Health as opposed to the drug company; I’d be all for that.” “[Disease fact sheets should be] a one-page thing with the pictures and a few facts about the disease. [These should be available] for individual vaccinations.” 2. Comments on HPV Vaccine Communication Patients are concerned about HPV vaccine efficacy Patients who contract HPV after getting vaccinated think the vaccine doesn’t work “There are many people that have gotten the vaccine who will subsequently have [other] strains of HPV. … And the first question they ask is: Well, I thought you gave me the Gardasil vaccine, how come it doesn’t work?” “You have to tell them there are other strains of the virus. It’s not going to protect you from all strains of HPV. It just isn’t.” 3. CDPH’s Pregnancy IZ Brochure: Immunizations for a Healthy Pregnancy Uniformly liked for use during an office visit Deemed helpful for preconception planning Positive tone and imagery especially appreciated “This is what we’re talking about. This is it!” “That’s a winner!” “It’s perfect. And it makes you happy because she’s happy.” “I love where in the middle it brings the whole family. So it’s not just the mom getting the injection. It does cover the whole family.” 10 Immunization Provider Focus Groups: Communication Approaches and Needs 4. Shot by Shot Video OB-GYNs and NPs reviewed “Dylan’s Story,” which related a mother losing her infant to pertussis Most found this story compelling and “real” Most did not favor showing the video during a clinical visit due to time constraints and emotional content Instead most would refer patients to the ShotbyShot.org website to view on their own without time pressure “If you give them a DVD video and say – you know what? I understand you don’t want immunizations, but here’s a DVD. Just talk to your husband, talk to other people who see this and come back and tell me what you think about it. That would probably work better than showing [Mariah’s story] to them.” “I think giving them a website [with] information… will be helpful.” E. OB-GYN Training Needs In the preliminary survey, OB-GYN and NPs showed poor understanding of immunizations recommended before, during, and after pregnancy. OB-GYN MDs and NPs also agreed or strongly agreed they needed training on: Adult immunization recommendations (88%) Immunization recommendations before, during, and after pregnancy (80%) How to discuss immunizations with patients (76%) “That’s just something I don’t know very much about, so I’d love that as part of my own personal information. Because even if I don’t administer the vaccine, I’d like to know … Oh, if you get this vaccine and you can’t pregnant for like six months or whatever. That’s vaccination stuff that I don’t know.” 11 Immunization Provider Focus Groups: Communication Approaches and Needs IV. Findings: Pediatricians and Family Physicians Top Vaccine Concerns Voiced by Parents Autism fear (raised at all focus groups) Vaccine safety/side effects Too many immunizations increase potential for more reactions Physicians/Pharma are in it for the money Immunizations overwhelm the immune system Immunizations have harmful ingredients Natural immunity is better How Practitioners Address Parents’ Concerns at a Visit A. To Appease Parents, They Allow Alternative Schedules “I basically agree with all the providers. We see more resistance of the immunizations over the last ten years and most of them, if they do, it’s because they want to alter the schedule…We just go along with it because it’s better to have some immunizations than none at all.” “I think it’s fine, if parents want to… poke their kids every month, it’s a pain in the a**….There may be no clinical research or anything to the contrary, but it’s still something you have to be compassionate with parents and just accept it and say, okay, we’ll do it this way…” B. They Continue to See Parents Who Refuse Vaccinations “Yeah, I’ve got to pay the bills.” “Some doctors think it’s a good strategy to kick them out of your practice. I don’t buy that because that’s one aspect of the care that I provide, immunizations… you’re still trying to keep them healthy. If they stay with you and in time then you might be able to convince them otherwise, especially as they come to trust you more.” C. They Navigate Concerns with Moms and Dads Fathers were often perceived to be more critical of vaccines. Thus, including them in conversations—and representing them in materials—was felt to be important “Well, fathers are harder. If they come in, my God, then we are in more trouble. Yes. I mean, you know they don’t come, 99% of them don’t come. But when they do come, they really… You know they’re fighting with the mother so they want to come see the doctor themselves. Or something is going on in their family dynamics.” “But again, actually all three families [I see who are refusing immunizations], it’s the father. The father doesn’t want to.” 12 Immunization Provider Focus Groups: Communication Approaches and Needs D. They Explain Flaws in the Wakefield Study “If somebody is concerned about autism, I tell them the guy who wrote the articles got arrested in England, so… He made up all those things, so there’s the problem with that.” E. They Discuss Past Outbreaks/Responsibility to the Community “We had our own experiences recently in 2010. We had kids die. So we can have personal experience of what happened recently.” “I also talk about it as it’s a public health issue. It’s not just your child. I relate the story I had of a kid that caused the whole school to close down because he was exposed to measles.” F. They Discuss Consequences of Not Vaccinating Kids get diseases Kids can die Different protocols used for treating ill patients who are unvaccinated [Re: flu vaccine]: “Probably change their mind, especially when I start saying, did you know 50,000 people die every year from that. They go, really?” “If your kid presents with a high fever and a bad cough, we have to think about things differently. So it’s not just a matter of not getting the vaccine, it’s a matter of changing the way we have to look at your child when they’re sick sometimes. And I also lay the burden on them.” “[Re: unimmunized children] It’s very difficult when they come into a hospital. If they’re not current, they’re exposing all of these immunosuppressed patients in the hospital, so that becomes a health issue.” G. They appeal to a Parent’s Cost-Conscientiousness Pertained mostly to HPV vaccine “I keep telling them, you’d have to pay hundreds of dollars for it, so you’re lucky. You should get it.” “That’s a great thing… $600 a pop for the series, and your insurance pays for it. And it may not if you wait.” 13 Immunization Provider Focus Groups: Communication Approaches and Needs H. They Emphasize VPDs are Just a Plane Ride Away “And living in the big city like Los Angeles or New York, you’re constantly getting exposed to people who come from different places. There is always high risk to be exposed.” “I tell them that, believe me, people are traveling. They can bring it here.” “There are a lot of diseases coming back because people are coming from third world countries.” I. They Find Guilt an Effective Motivator to Vaccinate “So your kid gets something, [and] it’s bad...They have some bad health problem. And now you’re going to have to live with having made a choice of not immunizing. And that needs to be part of the equation and process, in terms of you deciding… You need to go home and think about all the facts, and that should be part of it, as well.” “If your kid has a bad cough when they’re nine or ten, and they go over to their friend’s house, and there’s a three week old baby there, and your kid has got whooping cough — whooping cough isn’t always such a terrible disease. Sometimes it’s just a really bad cough as children get older. What would you do if a three week old got whooping cough? You have to think about that. That’s going to quarantine their children if they have a bad cough for two weeks or not. So I said, I’m not trying to beat you over the brain with this …you’re making a decision. And then you have to think about what the ramifications of that decision are.” J. They Draw on Personal Experiences/Stories They relate personal anecdotes about VPDs They emphasize that they vaccinate their own kids “I’ve been in medicine for over 30 years. I personally saw all the preventable diseases. So I think quite frequently they come in and say they want everything natural. Then I say, I can tell you what natural looks like. I don’t think they want to go natural on that.” “I’ve seen plenty of H-flu/meningitis and pneumococcal/meningitis. I just tell them what a terrible disease that is. And in the best of hands, kids often don’t turn out normal.” “[I talk about] my patients. They went to Europe. They didn’t immunize their kids at all. They have 15 months old twins. They went to Suffolk, I think… And they developed such a miserable case of chicken pox, they looked like lepers... They stayed in the hospital for three-and-half months. They had this horrible, horrible case of chicken pox… I use this story for all my patients.” “The other thing that I think creates some trust is you always use yourself as an example that my kids were immunized as early as possible as recommended by AAP. That’s one [way] to sell the idea.” 14 Immunization Provider Focus Groups: Communication Approaches and Needs “They’ll ask how many kids do you have? And I have three; every single one of them got fully vaccinated. I think it kind of relates to them on a personal level, it helps a little bit.” K. They Recommend Listening and Empathy in Working with Parents “I try to work with families and patients. I think you can convince the majority of them that comes in with questions… Sometimes it’s on your schedule, and sometimes it’s on whatever schedule they decided on.” “I’ve realized if you can work with them it’s a lot easier… And sometimes they still will not be convinced to get the vaccine, but do not lose a patient… a lot matters - your body language, how you talk to them. If you are with them, say ‘I understand.’ I try to get to the bottom of the problem… [what they’re] really worried about…” L. They Typically Recommend Meningococcal and HPV Vaccines at Tdap Visit HPV vaccine has the most resistance from parents of both girls and boys They prefer steering away from “sex” talk and emphasizing cancer prevention Photos of genital warts were thought to motivate adolescent boys “I talk about it as an anti-cancer drug.” “I take it out of the sexual realm. I say, your kid already has hepatitis B. We gave them that for the same reason. This is another one.” “I touch upon unusual head and neck tumors now that they’re finding in young individuals due to HPV, like where they have to cut out half your tongue and you get cancer of the tonsillar tissue. And it’s just terrible diseases. And often the parents will go, oh, yeah, let’s go ahead and do that one, too.” [Re: Convincing adolescent boys to get the HPV vaccine]. “You can show them the pictures of the penile and perianal warts.” M. Pediatricians recommend pediatric prenatal visits for pregnant women In the preliminary survey, 80% of pediatricians stated that they offer prenatal interviews to future parents Fifty percent of pediatricians discuss immunizations “most of the time” or “always” during prenatal interviews On average, however, less than 25% of all expectant parents scheduled a prenatal interview with pediatricians 15 Immunization Provider Focus Groups: Communication Approaches and Needs Pediatrician and Family Physician Review of IZ Branch Materials 1. Vaccine Safety Fact Sheets A B C D C Providers liked these sheets—and listed resources for trusted information A. Piece for educated, vaccine-hesitant parents only B & C. Provider fact sheets and talking points for new providers/students only D. MA fact sheet for MAs giving shots 16 Immunization Provider Focus Groups: Communication Approaches and Needs 2. Block Schedule (provisional) An excellent tool for themselves and patients; clear preference over CDC schedule Clean simplicity appreciated Quick check of shots due for providers; educational tool for parents: easy-tounderstand what vaccines are due and when Interest in an e-customizable version that can be “individualized” within ACIP time intervals. It should also include capability to show combination vaccines “This is just easier to look at. This would be better for me to show a patient.” “Yes, for the patient room this is perfect. It’s colorful, it’s big…..” “Honestly, this is much more organized; everything is together, only the physician could read this [CDC schedule].” “And you can tell them when you use combination….this is going to be in one shot. So that will help also.” [Re: Block schedule and the app] “I kind of wish that I did always have that.” [Re. Developing a web- based customizable version]. “That’s a good idea; you could print your own.” “Doctors use their iPhones all the time to look up meds, to look up whatever. If they could pull this up too, that would be fantastic.” 3. Sample Pertussis Handout Incorporates personal story in an effective way Where the video was often seen as “too tragic”, the story here in context of the educational leaflet was a powerful warning of what could happen, and providers said they would be more likely to use stories in this format in their medical offices 17 Immunization Provider Focus Groups: Communication Approaches and Needs 4. Pertussis Fact Sheets for Providers These pieces seen as too wordy and were generally not favored by providers. However, these pieces were only reviewed by one pediatric group 5. Shot By Shot Video Providers reviewed “Rachel’s story,” recounting the remorse of a mother that did not vaccinate her child who subsequently got measles. Recommended for class setting Providers would refer parents to the ShotbyShot.org website Most did not favor showing during a clinic visit (time/space considerations and wanting to avoid pressuring parent) “Maybe a hospital [or]…maybe a community presentation on immunizations, I could see wrapping it up with something like that to push the message into their minds, but not in the office.” “Yeah. So [for] the very educated people, I think giving them a website [with] information… that will be helpful.” “You know, I don’t have time to show this. That’s the hesitation.” A Family Practice physician, considering creating a 40-minute loop that plays on their television, said, “But things like this, if they could be incorporated into that loop would be useful, because she’s got a good story to tell. I think there’s a strong message there.” 18 Immunization Provider Focus Groups: Communication Approaches and Needs Recommendations for New Informing Materials 1. Disease-specific handouts/posters desired Similar to OB-GYNs, pediatricians and family physicians favored disease-specific handouts From a neutral public health source, not a drug company Preference to include disease images and possibly personal stories Posters in exam rooms favored as a conversation-starter Adolescent boys said to be very motivated by photo of genital warts Disease handouts should include pictures, information about the disease, the vaccine that prevents it, and who should get vaccinated “Especially for the Gardasil… How can a 12-year-old or 13-year-old make a decision for himself? All he can think is a shot is painful and [the] majority of them say no. I direct the question to the patient and say, ‘Look at these pictures. Would you like to get this or would you want to get vaccinated?’ The kid says, ‘Yes.’ And the mom at that point has left the decision to the kid. So the kid is okay, [and] the doctor is okay.” “The boy is looking at the genital warts picture – I’m getting that. I’m going to get that shot.” [RE: HPV] “I mean, I’ve heard lots of doctors say that when they start showing those pictures they get a lot higher acceptance rate.” “We use posters on the walls, from public health, which is very practical for different rashes; they can see and they can read about it… A lot of people see something visual, it has more… A deeper effect than hearing that. They see it and I explain to them for hours, they might not see the way that images can see. So, I think they are practical. I have ordered so many.” [Re: Disease tear-off sheets] “A lot of people ask, ‘Why do I have to give her that?’ ‘Who gets Diphtheria?’ So it would be nice to have a small background about what the actual illness is because again a lot of us never got it because we got vaccinated against it so we don’t know what it is.” “[Pictures] are good especially for the people that don’t want to vaccinate.” “We have the pictures and vaccinations in every room, so people look at it and ask – do we need to get them?” “[Pictures] are more scary to them, like oh, really? This is what can happen? Because it’s one thing when you’re talking about it and it’s another thing when you’re looking at a picture of Diphtheria or a crippling disease like polio and the child’s leg is going in the [opposite] direction.” 19 Immunization Provider Focus Groups: Communication Approaches and Needs 2. Electronic Information Recommendations for New Electronic/Mobile Information Electronic app designed for both provider and patient would probably be web-based Interface with a desktop and/or smart phone app for provider Free smart phone application for patients Send alerts during disease outbreaks Latest news on vaccines and recommendations updated real time Could function as the immunization record for the patient Would remind patient when shots are due or about upcoming appointments “The more input: visual, written, auditory – the more input you have, the better impact you’re going to have. That’s my personal belief. And just because you’re giving them written does not mean they’re going to read it. But if you have given them on a web, you have given them on YouTube, you’ve given them something written to follow that along, an opportunity to then interact with me, it would be more impactful…” “The parents, I think it’s fantastic if they have phones that they can pull up an app. That’s the way of the world now, everything is an app.” “Yeah. Doctors love their phones!” [Re: free app that patients can use to input date of next immunization visit and set reminders] “That would be great!” “It’s a good idea to have a yellow card, but then they don’t remember sometimes when the next immunization date will be. Always we get calls, oh, when’s my child going to get the next shot?” 3. Suggestions for Materials to Encourage Prenatal Pediatric Visits Based on survey results, it’s recommended that materials for pregnant women encourage expecting mothers to schedule prenatal interviews with pediatricians to discuss childhood immunizations Prenatal programs, including breastfeeding, childbirth and baby care classes, should also encourage pediatric prenatal visits. Immunization information dissemination during these programs may also be effective “I think speaking of immunizations, generally [with] new parents or [during the] prenatal interview, they’re more motivated to learn. They want to draw more information as opposed to when the baby is two months old, and they’re coming into the clinic.” 20 Immunization Provider Focus Groups: Communication Approaches and Needs 4. Additional Suggestions for New Materials Consider simpler, briefer formats and comic book-style materials for low-literacy parents Consider a simple to understand video (online or DVD) to explain the need for vaccination For practices serving diverse audiences, translated materials which are also culturallysensitive Visuals of VPDs often recommended. This includes a poster showing images of all VPDs Ensure that future materials for parents include pictures of fathers and possibly even pictures of happy patients getting shots Need for Training 1. Pediatricians Do Not Feel They Need Training The consensus was that pediatricians are well-informed about vaccine safety issues, especially those who have been practicing for many years. “To be honest with you, I think a professional association, the government, the CDC, and health departments have really done a good job of compiling information and made it available to all types of venues. I don’t feel deficient; I think they’ve done a real good job.” “We get training all the time.” “I just came from a conference in Monterey where [immunizations is] a typical topic. That’s there every time I go. It’s so intrinsic to everything we do in pediatrics.” 2. More Training for Medical Assistants Desired by Medical Providers Most providers acknowledged that MAs frequently get questions from parents at the time of vaccine administration While providers agreed that medical advice about vaccines was the purview of the physician, most providers also felt that MAs should receive training in 1) improving their knowledge about vaccines and vaccine safety 2) diseases prevented by immunizations, and 3) understanding the recommended immunization schedule Providers agreed that training MAs would give them positive reinforcement and that the “Vaccine Safety Fact Sheet for Medical Assistants” was an important piece for MAs to understand parents’ concerns 21 Immunization Provider Focus Groups: Communication Approaches and Needs …” [When parents] have a question, then the doctor should have backup. They [MAs] should not say, ‘I don’t know, I don’t have that material.’” “We do in-services, more disease oriented. If there’s a pertussis epidemic or something, we’ll meet with the phone staff and go over some of the things that they might get asked.” “This is important because I actually have an MA whose friends with a lot of our patients because she lives in the community. And she actually tells one of my patient’s moms oh, yeah, that’s the vaccine that I’m not giving my daughter.” “I think it’s good for them to have the information. I don’t know if it’s good for them to be out answering questions. But I think it’s good for them to have the information so that when the parent asks them, they’re not getting some kind of a negative unspoken response.” “Because it’s as simple as, what is that? Oh, that’s this—well, what is it? Uh… And then they can’t. And then they can’t answer the question.” “[MAs need training on] understanding the immunization schedule, especially when we have a lot of patients that only want to do one at a time or they want to split things up. Understanding that even though the doctor doesn’t order it, we are responsible to oversee that they’re on track.” “But I do get sick and take vacation, so I rely on these other girls to have a little heads up or to understand that there is a standard from that comes put every year, [and] it’s updated.” “If the families have questions, we still want them to refer to them to the physician or to the nurse, but more so that they’re really comfortable in what they’re doing.” “Because that’s what we want them to be---really comfortable in what they’re doing and to believe in what they’re doing.” 3. Results of Follow-up Survey with Medical Assistants (Please see Appendix 3) In an effort to better understand the training needs of medical assistants, a short Survey Monkey questionnaire was developed for California MAs When asked about desired training, 50% MAs responded “Diseases that vaccines prevent (disease names, symptoms, long-term and permanent consequences/damage)” Based on the results of the provider focus groups and the medical assistant survey, I&E is recommending the development of an EZIZ lesson on vaccine preventable diseases 22 Immunization Provider Focus Groups: Communication Approaches and Needs V. Recommended Actions GENERAL 1. Partner with relevant California-based medical associations, WIC programs, health plans, STD and women’s health clinics to promote CDPH informing materials among providers who are not currently participating in VFC. 2. Work with medical associations and medical assistant schools to promote CDPH’s “Vaccine Safety Fact Sheet for Medical Assistants” to their MA staff who administers immunizations. 3. Develop or promote training tools on vaccine-preventable diseases and “Vaccines 101” resource for medical assistants. Consider creating an MA-oriented vaccine resource, such as a page on EZIZ that houses existing tools. OB-GYNS 4. Work with the American Academy of Obstetrics and Gynecology (ACOG) and California Immunization Coordinators to promote CDPH’s “Immunizations for a Healthy Pregnancy” brochure to OB-GYN practices in California and to provide immunization training opportunities. 5. Consider partnering with organizations (e.g. birth centers, hospitals, WIC, etc.) that house and/or train childbirth educators, doulas, lactation educators, and lactation consultants to disseminate immunization information prenatally and encourage women to schedule a pediatric prenatal visit. 6. As new HPV vaccine materials are developed or updated, messaging should be clear that the vaccine cannot guarantee disease prevention 100%. But is still highly effective in preventing most genital warts, cervical and other cancers. 7. Provide training on immunization recommendations for OB-GYNs and their clinical staff. Collaborate with ACOG to distribute information to keep OBGYNs up-to-date. PEDIATRICIANS AND FAMILY PHYSICIANS 8. In materials for pregnant women, encourage women to schedule a prenatal interview with their future pediatrician to discuss immunizations. 9. Work closely with prenatal health professionals and programs (e.g., obstetricians, childbirth educators, and lactation educators/consultants, Text4Baby, etc.) to educate parents about the availability of the prenatal pediatric interview and encourage them to ask questions about childhood immunizations. 10. Expand promotion of vaccine safety materials intended for providers to include nursing schools, physician assistant and medical residency programs. 23 Immunization Provider Focus Groups: Communication Approaches and Needs 11. Adapt the current “alternative schedule” vaccine safety brochure for a parent audience. Ensure that pictures of happy fathers are included. 12. Create new version of vaccine safety brochure for parents to include a shorter, simpler version for lower-literacy readers. 13. Create a simple handout (e.g., card) to promote the ShotbyShot.org website for providers to give to vaccine-hesitant patients and parents. 14. Create a suite of single-sheet disease-specific flyers featuring images of the disease, easy-to-understand text about the disease and the vaccine, while possibly highlighting a personal story. Work with medical associations and VFC to distribute. 15. Ensure that informing materials expressly for a provider audience are visually appealing, not overly technical, and not text-heavy. 16. Create a poster featuring vaccine-preventable diseases, suitable for clinic exam rooms. Explore the feasibility of working with medical associations and health plans to co-brand and assist with printing and distribution. 17. Develop material for young adults that includes pictures of vaccine-preventable diseases. 18. Finalize and approve CDPH provisional “blocks schedule” and distribute widely via VFC and medical association partners. Work with physician reviewers to design a customizable smart phone and web-based application for providers to share with parents wishing a more personalized schedule—while staying within the ACIP guidelines. 19. Encourage pediatricians to notify local obstetricians, midwifes, and childbirth educators regarding their provision of prenatal pediatric appointments. 20. Work with the CDC and AAP to encourage pediatricians to discuss immunizations with expectant parents during the pediatric prenatal visit. 24 Immunization Provider Focus Groups: Communication Approaches and Needs Appendix 1: Pediatric and Family Medicine Survey Results and Recommendations Before each focus group began, clinicians in family and pediatric medicine were asked to complete a survey onsite. Below are the results of those surveys. Recommended actions are also included, as appropriate. 1. Do you or your staff download educational materials you receive via email or from a website? Yes: 85.5% No: 14.5% Recommendation: The majority of providers access electronic materials. Continue making educational materials available online. 2. What type of copier do you or your staff use to make copies of patient or provider education materials? Black-and-white copier: 83.6% Color copier: 12.7% We don’t make copies of educational materials: 1.8% Not sure: 1.9% Recommendation: When developing educational materials, make sure they print well in black and white ink. 3. Can your office make enough copies to meet your needs for patient handouts? Yes: 84.9% No: 5.7% Not sure: 9.4% Recommendation: Most providers can make copies of patient handouts. Continue to make downloadable materials available. 4. Does your office have a DVD player that can be used for patient or provider education purposes? Yes: 54.5% No: 43.6% Not Sure: 1.9% Recommendation: Approximately half of providers have access to a DVD player for educational purposes. When developing an educational video, consider producing limited DVD copies and making it available online for download or stream. 25 Immunization Provider Focus Groups: Communication Approaches and Needs 5. Have you or your staff ever ordered free immunization materials from your local health department? Yes: 57.4% No: 33.3% Not Sure: 9.3% Recommendation: Even though it appears that most providers have ordered immunization materials from their local health department, the majority of them were not familiar with the materials critiqued during the focus group discussions. Further promotion of immunization materials to providers is needed. 6. Do you have a professional website? Yes: 58.2% No: 38.2% Not Sure: 3.6% Recommendation: Only about half of providers have a professional website. There are limited opportunities to share immunization education, messaging, and resources on provider websites. Encourage providers without a website to promote your local health department website and CDC, AAP, and CDPH websites to their patients. 7. For those who answered “yes” to above: Do you feature patient education materials or links to educational materials/websites on your website? Yes: 64.5% No: 29% Not Sure: 6.5% Recommendation: Most providers with websites feature educational materials on their websites. Encourage these providers to link to immunization education materials from trusted sources. 8. Do expectant parents schedule a prenatal interview with you? Yes: 80% No: 20% (Please note: this question was analyzed for pediatric doctors only). Recommendation: Most pediatricians provide expectant parents with the opportunity of scheduling a prenatal pediatric appointment. Encourage pregnant women to schedule a pediatric prenatal interview. 26 Immunization Provider Focus Groups: Communication Approaches and Needs 9. Approximately what percentage of expectant parents schedule a prenatal interview with you? Average: 23.07% Median: 15% (Range from <1% to 90%) (Please note: this question was analyzed for pediatric doctors only). Recommendation: Even though prenatal pediatric appointments are available, most parents do not schedule one. Work with WIC and prenatal health professionals to encourage mothers to schedule a pediatric prenatal interview. 10. Do you discuss immunizations during the prenatal interview? Never: 6.25% Sometimes: 43.75% Most of the time: 43.75% Always: 6.25% (Please note: this question was analyzed for pediatric doctors only). Recommendation: Half of pediatricians do not regularly discuss immunizations during the prenatal pediatric interview. Work closely with AAP to encourage physicians to proactively discuss infant immunizations during this visit. 11. How much do you agree or disagree with the following statement? Prenatal interviews are good opportunities to discuss immunizations with parents. Strongly Agree: 31.25% Agree: 43.75% Neither Agree nor Disagree: 18.75% Disagree: 6.25% Strongly Disagree: 0% (Please note: this question was analyzed for pediatric doctors only). Recommendation: Providers are supportive of providing immunization information during the prenatal pediatric interview. Work closely with AAP to encourage physicians to proactively discuss infant immunizations during this visit. 12. What type of patient education material would be useful for discussing TIMING of immunizations with parents? (Please check all that apply.) Brochure/Flyer (for handing out to patients): 89.8% Poster (for posting in waiting/exam rooms): 44.9% PowerPoint slides for parent education: 12.2% I don't need patient education materials to discuss vaccine safety: 0% Other (please specify) or describe your ideal patient education material: 5% (Spanish [2], not specified [2], reminders) Recommendation: Providers make immunization flyers and brochures available to their patients. Continue to make these types of patient education materials available and promote them to healthcare providers. 27 Immunization Provider Focus Groups: Communication Approaches and Needs 13. What type of patient education material would be useful for discussing VACCINE SAFETY with parents? (Please check all that apply.) Brochure/Flyer with FAQs: 90.2% Flyer with reference to credible websites: 33.3% Educational DVD to play in provider office: 29.4% PowerPoint slides for parent education: 7.8% I don't need patient education materials to discuss vaccine safety: 0% Other (please specify): 9.8% (Spanish [2], not specified [3]) Recommendation: Providers make immunization flyers and brochures available to their patients. Continue to make these types of patient education materials available and promote them to healthcare providers. 14. What type of training, if any, would be useful to you or your staff for discussing vaccine safety with parents? (Please check all that apply). Online Training (i.e. webinars, interactive module): 54.3% Script with key messages: 30.4%% PowerPoint slides for staff training: 28.3% No training is necessary at this time: 10.9% Other (please specify): Live Conference; PP slides for NIIW presentation in 2013. May use it at community meetings; Office and Division Meetings; I'm at Kaiser SFO. We provide printed materials and offer a class taught by pediatricians about vaccine safety; personal training; not specified (3); patient education on Med gov vaccination-Debunk vaccines cause autism; I have all of the tools I need. Recommendation: When developing training for providers and/or their staff, make it available online. 15. Once families are in your practice, what percentage of them are vaccine hesitant (parents who want to delay or skip immunizations)? 0% (none): 0% 1-9%: 53.7% 10%-19% 35.2% 20%-29% 3.7% 30%-39% 3.7% 40%-49% 3.7% 50% or more 0% Recommendation: While most families immunize, all providers have families who are hesitant about immunizations. Communications about vaccine safety and the benefits of immunizations must continue. 28 Immunization Provider Focus Groups: Communication Approaches and Needs 16. What types of immunization communication or parent education tools do you send home BEFORE the visit, use DURING the consultation or ask parents to review at home AFTER their children’s immunization appointments? (Please check all that apply and describe the material that you use.) Item Brochure/flyer Scientific articles IZ websites Letters Emails Text messages Automated Robo Calls DVD Reminder postcards None Other During 36.7% 6.1% 14.3% 8.2% 8.2% 0.0% 2.0% 4.1% 12.2% 4.1% 2.0% Before 71.4% 12.2% 24.5% 4.1% 2.0% 0.0% 0.0% 4.1% 0.0% 0.0% 0.0% After 38.8% 2.0% 14.3% 2.0% 6.1% 0.0% 0.0% 0.0% 14.3% 0.0% 0.0% Other included: VIS (3), Newborn folder that has all childhood vaccine info. Comments: IZ website list prepared by MD for parents who want to research some more, postcards used to recall appointments for HPV; NP of MD discusses need for vaccines, Articles and websites given upon request; have online material available to print out; Phone calls; Autism/Wakefield article posted in office; CDC Handout summary; Paul Offit's article on vaccine safety addressing Dr. Sear's schedule; CHOP vaccine safety website; educational programming; handout: Facts/side effects Recommendation: Providers like to distribute handouts to their patients, and most give it to them before the appointment. Continue to make patient flyers and brochures available to providers and promote their availability. 17. At what age(s) do you recommend adolescents get vaccinated against meningococcal meningitis? (open-ended question) 54% said they give it during the preteen years (ages 9-12) 23% said they give an additional dose at age 16 or before going to college. 23% said they vaccinate at age 13 or older. Recommendation: While most providers are recommending the meningococcal vaccine during the preteen years, only 20% of them are also recommending the additional dose needed at age 16 or older. Work with medical associations to raise awareness about the recent recommendation at age 16 years. 29 Immunization Provider Focus Groups: Communication Approaches and Needs 18. How do you keep up with immunization information? (Please check all that apply.) CDC website or “Pink Book”: 79.2% Recommendations from my medical association or medical society (e.g., AAP’s “Red Book): 56.6% VFC Program communications: 39.6% EZIZ alerts from the California Department of Public Health, Immunization Branch: 41.5% Other: 20% (Google; info from pediatricians in the office; AAP Guides; CME programs (2); Academic meetings; ID specialist on site; Download of Stanford educ. Library; hospital; articles. Recommendation: Most providers trust the CDC and their medical association for the latest immunization information. Continue working closely with these organizations for provider communication purposes. 19. What newsletters or listservs are you subscribed to and regularly consult? (openended question) None, Kaiser Intranet, California Department of Public Health (2), CDC (7) Newsletter JAAPA, Medscape (2), Epocrates (2), AAPA Medical Watch; Google; AAFP(2), CAPA; Medscape; Redbook MMWR; EZIZ(3); Public Health Newsletters; ACIP newsletter; Upto-Date (3); Audiogiest; Contemporary Pediatrics; AAP(5); IAC; E3IMM; CHDP; VFC; Contemporary Pediatrics, Pediatrics Journal; Packard progress RN Recommendation: Most providers regularly consult newsletters and other communications from the CDC or their medical associations. Continue working closely with these organizations for provider communication purposes. 20. Would you like to receive email updates from California Department of Public Health, Immunization Branch with information about immunization recommendations and resources? Yes! (Please make sure to enter your email address below.) 53.8% No: 46.2% Recommendation: Encourage providers to sign up for EZIZ alerts. 30 Immunization Provider Focus Groups: Communication Approaches and Needs Appendix 2: Obstetric Medicine Survey Results Before each focus group began, clinicians were asked to complete a survey onsite. Below are the results of surveys completed by nurse practitioners and physicians in obstetric medicine. Recommended actions for each response are also included. 1. Do you or your staff download educational materials you receive via email or from a website? Yes: 72% No: 24% Not Sure: 4% Recommendation: The majority of providers access electronic materials. Continue making educational materials available online. 2. What type of copier do you or your staff use to make copies of patient or provider education materials? Black-and-white copier: 68% Color copier: 24% We don’t make copies of educational materials: 8% Not sure: 0% Recommendation: When developing educational materials, make sure they print well in black and white ink. 3. Can your office make enough copies to meet your needs for patient handouts? Yes: 82.6% No: 4.3% Not sure: 13.1% Recommendation: Most providers can make copies of patient handouts. Continue to make downloadable materials available. 4. Does your office have a DVD player that can be used for patient or provider education purposes? Yes: 29.2% No: 58.3% Not Sure: 12.5% Recommendation: Most obstetric providers do not have access to a DVD player in their office. Make educational videos available for download or streaming online. 31 Immunization Provider Focus Groups: Communication Approaches and Needs 5. Have you or your staff ever ordered free immunization materials from your local health department? Yes: 52% No: 28% Not Sure: 20% Recommendation: Even though it appears that most obstetric providers have ordered immunization materials from their local health department, the majority of them were unfamiliar with the materials critiqued during the focus group discussions. Further promotion of immunization materials to providers is needed. 6. Do you have a professional website? Yes: 52% No: 48% Not Sure: 0% Recommendation: Only about half of providers have a professional website. There are limited opportunities to share immunization education, messaging, and resources on provider websites. Encourage obstetric providers without a website to promote your local health department website and CDC, ACOG, and CDPH websites to their patients. 7. For those than answered “yes” to above: Do you feature patient education materials or links to educational materials/websites on your website? Yes: 53.8% No: 38.5% Not Sure: 7.7% Recommendation: Most providers with websites feature educational materials on their websites. Encourage these providers to link to immunization education materials from trusted sources. 8. Approximately what percentage of your patients are under 18 years of age? 0% (none): 0% 1-9%: 48% 10%-19% 40% 20%-29% 12% 30%-39% 0% 40%-49% 0% 50% or more 0% Recommendation: All obstetric providers serve patients under 18 years of age. Educate obstetric providers about the VFC program. 32 Immunization Provider Focus Groups: Communication Approaches and Needs 9. Do you consider yourself to be a primary care physician? Yes. 53.8% No. 30.8% Not sure. 15.4% (Please note: this question was only analyzed for obstetric physicians only) Recommendation: Most obstetricians consider themselves to be primary care physicians. Encourage obstetricians to continue recommending immunizations to their patients. 10. What immunizations do you recommend before, during or after pregnancy? (openended question) Immunization HPV Tdap Td Flu Hepatitis A Hepatitis B Rubella or MMR Meningococcal Pneumococcal Before 50% 68% 14% 59% 23% 41% 45% 4.5% 14% During 0% 81% 9% 77% 14% 18% 0% 4.5% 4.5% After 9% 64% 9% 55% 14% 18% 41% 5.5% 9% Recommendation: Most obstetric providers routinely recommend Tdap and flu immunizations before, during, and after pregnancy. More education is needed to inform obstetric physicians about the recommended schedule. 11. How much do you agree or disagree with the following statements? I would like training on how to discuss immunizations with my patients. Strongly Agree: 16% Agree: 60% Neither Agree nor Disagree: 24% Disagree: 0% Strongly Disagree: 0% I would like training on immunization recommendations before, during, and after pregnancy. Strongly Agree: 28% Agree: 52% Neither Agree nor Disagree: 20% Disagree: 0% Strongly Disagree: 0% 33 Immunization Provider Focus Groups: Communication Approaches and Needs I would like training on all adult immunization recommendations. Strongly Agree: 28% Agree: 60% Neither Agree nor Disagree: 12% Disagree: 0% Strongly Disagree: 0% Recommendations: Approximately 82% of obstetricians would like training on immunization recommendations. Work with CDC and ACOG to provide training to obstetric physicians and nurses about immunization recommendations. 12. Doctors who enroll in the national Vaccines for Children (VFC) program receive routine childhood vaccines for no out-of-pocket costs. This allows them to provide immunizations to children, 0 through 18 years of age, who meet certain criteria. Are you interested in learning more about the VFC program? YES. 47.8% (email addresses collected for those interested) No. 52.2% Recommendation: Inform obstetricians about the VFC program. 13. How do you keep up with immunization information? (Please check all that apply.) CDC website or “Pink Book”: 50% Recommendations from my medical association or medical society (e.g., AAP’s “Red Book, ACOG): 58.3% VFC Program communications: 8.3% EZIZ alerts from the California Department of Public Health, Immunization Branch: 25% Other: 5% (County of LA, Medscape, CMA Foundation, organization alerts, hospital) Recommendation: Work with CDC and ACOG for obstetric provider communication purposes. 14. What newsletters or listservs are you subscribed to and regularly consult? (open-ended question) LA County sends us stuff; Medscape (3); Quanta MD, Web MD, SERMO, MDINY; Green Journal (2), OB-GYN news(2); EZIZ; All OBGYN, ABC, CMA, SERMO, NPR, ACOG (4), AWHONN; Up to Date(2); Clinical Library; Prescriber’s letter; various through CDPH 15. Would you like to receive email updates from California Department of Public Health, Immunization Branch with information about immunization recommendations and resources? YES: 50% (those interested were prompted to enter email address). NO. Not at this time. Thank you: 50% 34 Immunization Provider Focus Groups: Communication Approaches and Needs Appendix 3: Follow-up Survey with Medical Assistants Background and Methodology As stated in the report, medical assistant training was one of the topics that discussed during each of the focus groups and interviews. The focus groups were asked a series of questions to assess providers’ opinions about whether patients and parents of patients ask MAs questions about immunizations and whether MAs should respond to questions and concerns about immunizations. In each group there was discussion regarding what training, if any, medical assistants should have regarding immunization and/or how to deal with patient inquiries. Most providers shared that MAs did not have training that specifically addresses how to respond to inquiries on immunization, but are clearly instructed to refer the parent/patient to the doctor. Nevertheless, most agreed these types of questions are asked of MAs, and that if MA training in these areas is made available, it needs to help the MA learn about the importance of immunizations, what diseases immunizations prevent, and common immunization concerns or misconceptions. However, regardless of being trained or not, due to the liability attaching to the provider, medical assistants would still be instructed to refer any questions to the doctor. In an effort to better understand the training needs of medical assistants and to compare what providers said MAs do and need with what MAs really do and need, a short Survey Monkey questionnaire was developed for California MAs. The survey, administered on July 9 to California medical assistants via the EZIZ listserv, one of the listservs developed by the CDPH, Immunization Branch, received more than 1,000 responses within 24 hours. Results The following charts show three of the questions MAs were asked in the online survey and how they responded. 35 Immunization Provider Focus Groups: Communication Approaches and Needs 36 Immunization Provider Focus Groups: Communication Approaches and Needs Findings Significant highlights from the MA survey include: • Most (85%) MAs said that parents/patients ask them questions or voice their concerns about side effects of vaccines • Half (49%) of the MAs said that parents/patients want to know what disease is prevented by the vaccine the MA is administering •Most (74%) MAs said that they answer at least some of the vaccine-related questions they receive from patients/parents • Most (64%) MAs said they would like training/information about vaccine safety (side effects, ingredients, etc.) •Half (50%) of MAs said they would like training/information about the diseases (including symptoms, long terms consequences/damage from the disease, etc.) that are prevented by the vaccines they administer 37 Immunization Provider Focus Groups: Communication Approaches and Needs Comparison of results: provider focus groups versus medical assistants Comparing the two data sources--Is there a disconnect? When the data from the focus groups and the MA survey are compared, there are some striking similarities as well as some stark contrasts. Some responses from medical assistants are consistent with opinions shared by providers in the focus groups, but they differed significantly on other issues. This is especially true of what medical assistants say they do versus what providers tell medical assistants to do or want them to do. For example, when responding to inquiries about MAs answering questions about immunizations, the majority of providers in the focus groups related instructing MAs not to answer questions regarding immunization, but to refer any inquiry to a doctor or nurse. All focus group respondents agreed this was the correct policy. However, 74% of MAs responded that they answer at least some questions about immunizations from patients and parents. Only 16% of MAs said they refer all immunization questions to the doctor or nurse. At first this might appear to be a disconnect. However, what may appear to be a disconnect may actually be a reflection of providers’ concerns about liability issues attaching to the provider. The key to the apparent disconnect between medical assistants and providers is likely the result of physician concerns about their liability for MAs’ actions, given that the MA scope of practice is quite limited. This is consistent with what the EZIZ team and others in the IZ Branch have heard for years about what medical assistants are actually doing on the job versus what providers are comfortable having them do—or even what providers are comfortable about in terms of knowing what their MAs are doing. Moreover, when developing training for medical assistants, physician liability and MA scope of practice should be an important consideration. Although the medical assistant scope of practice in California does not clearly identify what MAs are not allowed to do, it is generally assumed that MAs should not give advice. While the majority of medical assistants (64%) said they’d like training on vaccine safety, there are tools on the topic already available for MA informational purposes only. The California Immunization Coalition’s “Vaccine Safety Fact Sheet for Medical Assistants,” reviewed during the focus groups, is a flyer that was very well-received by providers; in past focus groups, MAs also agreed it was useful. Trainings about vaccine safety, however, could easily be misconstrued as condoning MAs giving medical advice. One area where providers and medical assistants are in accord is about MAs needing to know what diseases are prevented by the immunizations they administer. According to provider focus group results, providers believe basic training for medical assistants is needed on vaccinepreventable diseases, immunizations, and common misconceptions about vaccines. When asked what topics they would like more training/information about, half of the MAs responded “Diseases that vaccines prevent (disease names, symptoms, long-term and permanent consequences/damage).” 38 Immunization Provider Focus Groups: Communication Approaches and Needs Recommendations Based on the results of the provider focus groups and the medical assistant survey, I&E is recommending that a resource be made available to medical assistants on vaccine preventable diseases. This may include the inclusion of existing tools and resources on vaccine-preventable diseases or developing materials (e.g., flyers, fact sheets, lesson) to be housed in EZIZ. 39 Immunization Provider Focus Groups: Communication Approaches and Needs