LMA GRADE CoSTR
advertisement

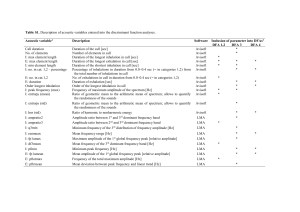
LMA GRADE CoSTR CONSENSUS ON SCIENCE: LMA compared to FM as a primary device for infants at term requiring positive pressure ventilation for resuscitation (3 RCT with 469 patients) For the critical outcome of “achieving vital signs” we have identified low quality evidence from 2 small RCTs and 1 large Quasi RCT, showing that LMA was more effective than the FM (OR 11.43 95% CI 4.01- 32.58). For the critical outcome of “need for subsequent endotracheal intubation after failed LMA or FM”, we have identified low quality evidence from the same RCTs, showing that LMA was more effective than the FM (OR 0.13 95% CI 0.05-34). For the critical outcome of ”Apgar score increasing” we have identified low quality evidence from the same RCTs, not being possible to analyze these outcome for the way of report in each study. For the critical outcome of “dead” we have identified low quality evidence from the same RCTs, showing no difference between LMA or FM. For the important outcome of “morbidity” we have identified low quality evidence from the same RCTs, showing no difference for any variable between LMA or FM (OR 5.76 95% IC 0.7 – 47.32). We did not identify any evidence to address the critical outcomes of “indicators of brain injury” or “long term outcomes”. LMA compared to ETT as a secondary device for infants at term requiring positive pressure ventilation for resuscitation (1 RCT with 40 patients) For the critical outcome of “achieving vital signs or successful resuscitation”, we have identified very low quality evidence from one RCT showing that LMA was as effective as the ETT tube. For the critical outcome of “need for subsequent endotracheal intubation after failed LMA”, we have identified very low quality evidence from the same RCT showing that LMA was as effective as ETT. For the critical outcome of “Apgar score increasing” we have identified very low quality evidence from the same RCT, not being possible to analyze these outcome for the presentation of the results in the study. For the critical outcome of “dead” we have identified very low quality evidence from the same RCT, showing no difference between LMA or FM or ETT. For the important outcome of “morbidity” we have identified very low quality evidence from the same RCT, showing more trauma tissue comparing with LMA vs ETT (OR 2.43 (0.51 – 11.51). We did not identify any evidence to address the critical outcome of indicators of brain injury or long term outcomes comparing LMA, FM or ETT as a secondary device. TREATMENT RECOMMENDATION LMA compared to FM as a primary device for infants at term requiring positive pressure ventilation for resuscitation We suggest that the use of Laryngeal Mask Airway as a primary device for respiratory support in delivery room for newborns at term requiring positive pressure ventilation during neonatal resuscitation as feasible and safe, but there is not enough evidence to recommend it instead of Face Mask (weak recommendation from low quality of evidence). There is limited evidence, however, to evaluate its use for premature infants. The laryngeal mask airway has not been evaluated in the setting of meconium-stained amniotic fluid, during chest compressions, or for administration of emergency intratracheal medications The laryngeal mask airway should be considered during resuscitation of the newborn if face mask and/or endotracheal intubation is unsuccessful or not feasible. LMA compared to ETT as a secondary device for infants at term requiring positive pressure ventilation for resuscitation We suggest that the use of Laryngeal mask airway as a secondary device for respiratory support in the delivery room for newborns at term requiring positive pressure ventilation during neonatal resuscitation as feasible and safe, but there is not enough evidence to recommend it instead of endotracheal intubation (weak recommendation from very low quality evidence).