Additional file 1
advertisement

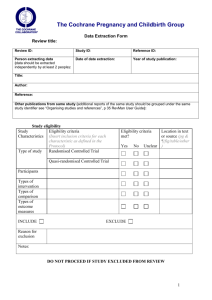
Additional file 1. Details of characteristics and methodological quality of the included studies. Total No. of Study ID Patients (Intervention/ Intervention Group Control Group Duration Primary Outcomes Secondary Outcomes Follow up Quality Control) 49 (28/21) Chen 2005 [21] Chen 2006 [30] ‘Fufang Biejia Tablets’ Ruangan IFN-γ 1MU (IM). (standardized prescription; oral 4 tablets, 6 months HA: intervention group better 2006_2 [20] None Good than control group (P < 0.05). (Modified NS in LN, PC-III & IV-C. Cochrane TID) and access to IFN-γ risk of 1MU (IM). bias 9/16) 116 (58/58) Kang Xian Decoction IFN-α 3MU. 6 months HA, LN & PC-III: intervention ALT & improvement of None Poor (standardized prescription; group better than control group related clinical symptoms: (Modified oral, one dose per day) and ( P < 0.05). intervention group better Cochrane than control group (P < risk of 0.01). bias 5/16) access to IFN-α 3MU. Chen NS in ALT & AST. 138 (68/70) ‘Qianggan Capsule’ Placebo (shape 6 months HA, LN, PC-III & IV-C: ALT, improvement of None Good (standardized prescription; consistent with intervention group better than related clinical symptoms: (Modified oral, 4 g/d) plus intervention group) control group ( P < 0.05). intervention group better Cochrane conventional care. plus conventional than control group (P < risk of care. 0.05). bias Adverse events: 4 cases in 10/16) intervention group and 5 in control group- nausea, vomiting and abdominal discomfort. Chen 2007 [31] 164 (54/58/52) Group I: Bie Jia Jian Pills IFN 3MU (IM) plus 9 months HA: intervention group better Adverse events: In the use None Good (standardized prescription; conventional care. than control group at 6 & 9 of IFN therapy, 80% (Modified oral, 6 g/d) plus months (P < 0.01). patients had cold or Cochrane conventional care. LN & PC-III: Group II better “flu-like” symptoms; some risk of Chen 2010 96 (46/50) [22] Group II: Group I plus than control group at 6 & 9 control group. months (P < 0.01), NS compared leucopenia and ‘Fufang Biejia Ruangan Entecavir 0.5 mg Tablets’ (standardized (oral, QD). 1 year prescription; oral 2 g, TID) Dai 2011 68 (34/34) [23] patients with mild Group I with control group. thrombocytopenia. HA, LN, PC-III & IV-C: NS in ALT & AST. bias 10/16) None Poor intervention group better than (Modified control group (P < 0.05). Cochrane and access to Entecavir 0.5 risk of mg (oral, QD). bias 7/16) ‘Fufang Biejia Ruangan Entecavir 0.5 mg Tablets’ (standardized (oral, QD). 1 year HA, LN, PC-III & IV-C: NS in ALT & AST. intervention group better than Improvement of related (Modified control group (P < 0.05). clinical symptoms: Cochrane and access to Entecavir 0.5 intervention group better risk of mg (oral, QD). than control group (just bias 8/16) prescription; oral 2 g, TID) None Good description). Gao 2000 120 (60/60) ‘HB-Granule-3’ [32] IFN-α 3MU (SC, HA & IV-C: intervention group ALT (P < 0.01) & 3 (standardized prescription; three times per better than control group improvement of related months (Modified oral 10 g, TID). (p<0.05). clinical symptoms: Cochrane NS in LN. intervention group better risk of than control group (just bias 3/16) week). 90 days Poor description). Huang 2007 [24] 99 (50/49) ‘Decoction of Radix Salviae Milltorrhizae, Radix Astragali and Rhubarb’ (standardized prescription; oral 100 mL, BID). IFN-α 5MU (IM, 3 months HA & PC-III: intervention group ALT: intervention group 6 Good once every two better than control group (P < better than control group (P months (Modified days). 0.01) at 3-month, NS at 6-month < 0.05) at 3-month, but NS Cochrane follow-up. observed at 6-month risk of LN & IV-C: intervention group follow-up. bias 8/16) better than control group at NS in AST. 3-month (P < 0.01) and 6-month Adverse events: 15 cases follow-up (P < 0.05). “flu-like” symptoms in control group; 3 cases severe diarrhea in intervention group (1 stop treatment). Huang 2009 83 (43/40) [25] ‘Fufang Biejia Ruangan Adefovir dipivoxil 1 year Tablets’ (standardized 10 mg (oral, QD). NS in ALT & AST. None Poor (Modified prescription; oral 4 tablets, Cochrane TID) and access to Adefovir risk of dipivoxil 10 mg (oral, bias 6/16) QD). Kuang 2005 53 (27/26) [26] Bie Jia Jian Decoction LVD 100 mg (QD). 60 days HA: intervention group better Improvement of related None Good (standardized prescription; than control group (P < 0.05). clinical symptoms: (Modified oral, one dose per day). NS in PC-III & IV-C. intervention group better Cochrane than control group (P < risk of 0.05). bias 8/16) NS in ALT & AST. Li 2006 [27] 60 (30/30) ‘Xiexian Oral Liquid’ Placebo 4 months HA, LN & IV-C: intervention AST & improvement of 6 Good months (Modified (standardized prescription; (physiological group better than control group related clinical symptoms: oral 30 mL, QD), plus saline plus food (P < 0.01). intervention group better Cochrane conventional care. coloring), plus than control group (P < risk of conventional care. 0.01). bias 8/16) NS in ALT. Adverse events: 4 cases in intervention group (1 allergic, 3 diarrhea). Li 2011 [28] 88 (44/44) ‘Anluo Huaxian Pills’ Adefovir dipivoxil 9 months HA, LN, PC-III & IV-C: (standardized prescription; 10 mg (oral, QD). intervention group better than oral 6g, BID) and access to control group (P < 0.05). NS in ALT & AST. Adverse events: none. None Poor (Modified Cochrane Adefovir dipivoxil 10 mg risk of (oral, QD). bias 5/16) Lu 2010 82 (42/40) [29] Shen 2003 68 (31/37) [33] ‘Fufang Biejia Ruangan Adefovir dipivoxil 1 year HA & LN: intervention group ALT, AST & Improvement None Good Tablets’ (standardized 10 mg (oral, QD). better than control group (P < of related clinical (Modified prescription; oral 4 tablets, 0.01). symptoms: intervention Cochrane TID) and access to Adefovir NS in PC-III & IV-C. group better than control risk of dipivoxil 10 mg (oral, group (P < 0.05). bias 8/16) QD). Adverse events: none. ‘Ganxian Prescription’ LVD 100 mg (oral, 1 year HA: intervention group better ALT: intervention group (semi-standardized QD). than control group (P < 0.05). better than control (P < (Modified NS in LN & IV-C. 0.05). Cochrane day) and access to LVD 100 NS in AST. risk of mg (oral, QD). Adverse events: none. bias 8/16) prescription, one dose per Shen 2005 120 (40/40/40) Group I: ‘Ganxian Recipe’ LVD 100 mg (oral, 2 years [34] (semi-standardized QD). HA, LN & IV-C: Group II better ALT: Group II better than None None Good Poor than control group (P < 0.05). control group (P < 0.05), (Modified prescription, one dose per NS in HA, LN & IV-C NS comparing Group I with Cochrane day). comparing Group I with control control group. risk of Group II: ‘Ganxian Recipe’ group. bias 7/16) NS in AST. (same as Group I) and Adverse events: 8 cases access to LVD 100 mg diarrhea (3 in Control (oral, QD). group, 5 in Group I), 2 cases dizziness in Group II, 3 cases upper respiratory infection-like symptoms in control group. Sun 2010 [35] 55 (30/25) ‘Anluo Huaxian Pills’ Adefovir dipivoxil 48 weeks HA: intervention group better ALT, AST & Improvement None Poor (standardized prescription; 10 mg (oral, QD). than control group (P < 0.05). of related clinical (Modified oral 6g, TID) and access to NS in LN, PC-III & IV-C. symptoms: intervention Cochrane Adefovir dipivoxil 10 mg group better than control risk of (oral, QD). group (P < 0.05). bias 7/16) Wang 2006 160 (50/60/50) Group I: experienced LVD 100 mg (oral, 6 months HA, LN, PC-III & IV-C: Group None Good [36] clinical decoction QD). II better than control group at 3 (Modified (semi-standardized and 6 months (P < 0.01); Group Cochrane prescription, one dose per I better than control group in HA risk of day). at 3 and 6 months (P < 0.01). bias Group II: Group I plus 10/16) control group. Wang 2010 98 (49/49) [37] ‘Fufang Biejia Ruangan Adefovir dipivoxil 1 year HA, LN, PC-III & IV-C: ALT: intervention group Tablets’ (standardized 10 mg (oral, QD). intervention group better than better than control group (P (Modified control group (P < 0.05). < 0.05). Cochrane prescription; oral 4 tablets, None Poor TID) and access to Adefovir risk of dipivoxil 10 mg (oral, bias 6/16) QD). Wei 2010 44 (22/22) [38] ‘Fufang Biejia Ruangan Adefovir dipivoxil 1 year HA, LN, PC-III & IV-C: Tablets’ (standardized 10 mg (oral, QD). intervention group better than (Modified control group (P < 0.05). Cochrane prescription; oral 4 tablets, NS in ALT & AST. None Good TID) and access to Adefovir risk of dipivoxil 10 mg (oral, bias 9/16) QD). Xie 2009 [39] Yang 2009 [40] 62 (32/30) Conventional care. 6 months HA, LN, PC-III & IV-C: ‘Huaxian Fugan intervention group better than Prescription’ (standardized ALT, AST & Improvement None Good of related clinical (Modified prescription; oral 100 mL, symptoms: intervention Cochrane BID), plus conventional group better than control risk of care. group (P < 0.01). bias 8/16) 120 (60/60) ‘Fufang Biejia Ruangan Tablets’ (standardized control group (P < 0.05). LVD 100 mg (oral, 6 months HA, LN, PC-III & IV-C: QD) plus prescription; oral 4 tablets, conventional care. NS in ALT & AST. None Good intervention group better than (Modified control group (P < 0.05). Cochrane TID), and access to LVD risk of 100 mg (oral, QD) plus bias 9/16) conventional care. Yin 2004 102 (52/50) ‘Herbal Compound 861’ [41] Placebo (shape (standardized prescription; consistent with oral 7 capsules, TID). 24 weeks PC-III, MMP9, TIMP1 & ALT & AST: intervention None Good TIMP2: intervention group group better than control (Modified ‘Herbal Compound better than control group (P < group (P < 0.05). Cochrane 861’; oral 7 0.05). NS in Improvement of risk of capsules, TID). NS in HA, LN, IV-C, MMP1 & related clinical symptoms. MMP2. bias 8/16) Adverse events: dry throat, nausea, abdominal discomfort, constipation in both groups (the number of patients not mentioned). Zhang 2000 [42] 78 (39/39) ‘Kanggan Xianfang’ Conventional care. 6 months HA, PC-III & TGF-β1: ALT & Improvement of None Good (standardized prescription; intervention group better than related clinical symptoms: (Modified oral 8g, TID) plus control group (P < 0.05). intervention group better Cochrane than control group (P < risk of 0.05). bias 8/16) conventional care.