Chaetomium gracile
advertisement

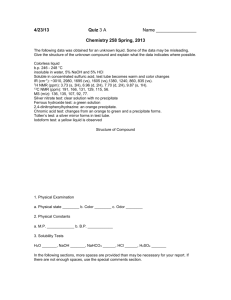
细丽毛壳 Chaetomium gracile 次级代谢产物的分离鉴定及其抗菌 活性* 白欢欢 1,2 吴林蔚 1 杨 涛 1 李国友 1** 1 中国科学院成都生物研究所应用与环境微生物重点实验室 成都 610041 2 中国科学院大学 北京 100049 摘 要 活性筛选显示细丽毛壳(Chaetomium gracile)的大米固态发酵乙酸乙酯提取物具有显著的抗菌活 性,为了研究阐明其抗菌活性物质基础,利用各种色谱分离技术从中分离获得 9 个化合物,综合运用化学 分析和波谱分析,分别被鉴定为麦角甾醇、(22E,24R)-麦角甾-7,22-二烯-3β,5α,6β-三醇、棕榈酸单甘油酯、 eugenitol、对羟基苯甲醛、chaetochromin A、3-吲哚甲酸、腺苷和 chetoquadrin F。其中化合物 6 为主要次 级代谢产物,该化合物在浓度为 0.95 μg/mL 时对大肠杆菌,金色葡萄球菌及枯草芽孢杆菌具有显著抗菌活 性. 图 1 表 1 参 32 关键词 细丽毛壳霉; 固态发酵;次级代谢产物; 抗菌活性;chaetochromin A Isolation and identification of secondary metabolites from fungus Chaetomium gracile and their antimicrobial activities* BAI Huanhuan1, 2, WU Linwei1, YANG Tao1, LI Guoyou1** 1 Key Laboratory of Environmental and Applied Microbiology, Chengdu Institute of Biology, Chinese Academy of Sciences, Chengdu 610041, P. R. China 2University of Chinese Academy of Sciences, Beijing 10049, China Abstract In screening of antimicrobial metabolites, the ethyl acetate extract of solid-state fermented rice culture of the fungus Chaetomium gracile exhibited significant antimicrobial activity. In the process of disclosing the antimicrobial substances, nine compounds were isolated from the ethyl acetate extract by the combination of multiple chromatography methods. They were identified as ergosterol (1), (22E,24R)-ergosta-7,22-diene-3β,5α,6 β-triol (2), glycerol monopalmitate (3), eugenitol (4), p-hydroxylbenzaldehyde (5), chaetochromin A (6), indole-3 carboxylic acid (7), adenosine (8), and chaetoquadrin F (9) based on spectroscopic analysis. Compound 6 was the major metabolite and displayed significant antimicrobial activity against Escherichia coli, Staphylococcu aureu, and Bacillus subtilis at the concentration of 0.95 μg/mL. Fig 1, Table 1, Ref 32 Keywords Chaetomium gracile; Solid-state fermentation; Secondary metabolites; Antimicrobial activity; Chaetochromin A In recent years, fungi are of growing importance as promising sources of bioactive natural products [1-2]. Some fungal metabolites such as micafungin sodium, amrubicin hydrochloride, daptomycin, and ergot alkaloids have been used in clinical treatment, and many novel agents with antibiotic, anti-tumor, anti-infective, and cytotoxic activities from fungi were reported [3-4]. The genus Cheatomium, comprising of more than 350 species, has been widely studied recently, and more and more bioactive secondary metabolites with interesting structures were 收稿日期 Received: 接受日期 Accepted: *国家自然科学基金项目(21272228)资助 Supported by the National Natural Science Foundation of China (No. 21272228) **通讯作者 Corresponding author (E-mail: ligy@cib.ac.cn) isolated from this genus [5-9]. Up to now, more than 200 compounds of diverse structural types were obtained from the genus Cheatomium [10]. Previously studies on the bioactive metabolites from the genus Chaetomium have resulted in the isolation of some metabolites with diverse bioactivities such as cytotoxicity, antimicrobial activity, and inhibitory ability on root elongation [11-14]. In this study, the secondary metabolites of Chaetomium gracile were investigated for the significant antimicrobial activity. As a result, nine metabolites (1-9) were isolated and identified on the basis of spectral analyses. Chaetochromin A (32.7% of the exact) was the major metabolite responding for the antimicrobial activity. Herein we reported the isolation, structural identification and antimicrobial activities of these compounds. 1 Material & Methods 1.1 General High-resolution electrospray ionization mass spectra (HRESIMS) were carried out on a BioTOF-Q mass spectrometer. Optical rotations were measured with a Perkin-Elmer 341 automatic polarimeter. IR spectra were recorded on Perkin-Elmer Spectrum One FT-IR spectrometer (KBr). NMR spectra were performed on Bruker Advance 600 and Bruker Advance 400 spectrometers with TMS as internal standard. Silica gel (200-300 mesh, 300-400 mesh) for column chromatography and silica gel GF254 (10-40 μm) for TLC were purchased from Qingdao Marine Chemical Company, China. All solvents were distilled prior to use. 1.2 Fungus material Chaetomium gracile and the test microbe strains E. coli, S. aureus, B. subtilis, Fusarium oxysporum f. sp. vasinfectum, Fusarium oxysporum f. sp. benincasae, Cochliobolus sativus, Typhula incarnata Lasch ex Fr., Botrytis cinerea Pers ex Fr., Glomerella cingulata (Ston.) Spauld & Schrenk, Sclerotinia sclerotiorum (Lib.) dBy, Gloeostporium mangiferea P.Henn, Colletotrichum capsici (syd.) Butl, Fusarium oxyporum f. sp. nive-um, and Fusarium oxysporum f. sp. cucumerinum were obtained from Institute of microbiology, Chinese Academy of Sciences (CAS), P. R. China. The test bacteria and fungi were stocked on medium (dextrose 20.0 g/L, beef infusion 10 g/L, NaCl 5 g/L, agar 17 g/L) and potato dextrose agar slants at 4 ºC, respectively. 1.3 Fermentation and isolation Seed culture medium was comprised of dextrose (20 g/L), yeast extract (1 g/L), KH2PO4 (3.0 g/L), MgSO4·7 H2O (1.5 g/L), and potato extract (20 %, m/V). The pH of medium was adjusted to 6.0 with 1 mol/L NaOH (aq.). Solid culture medium consisted of rice and 0.3 % peptone. The sterilization was carried out at 121 ºC under 15 psi for 30 min. The fresh mycelium grown on PDA slant at 29 ºC for 4 days was inoculated into 250 mL flasks containing 100 mL sterilized seed medium. Flasks with inoculated medium were placed in rotary shaker at 29 ºC and incubated at 140 rpm for 3 days. The seed culture was inoculated into sterilized rice solid medium for further fermentation at 29 ºC for 25 days. The fermented solid rice medium (5.0 kg) was soaked with ethyl acetate (8 L×3) at room temperature. The solvent was evaporated in vacuo to afford a residue (29.0 g). The residue was divided into four fractions (Frs. A, B, C, and D) over silica gel column (350g, 300-400 mesh, ф75 mm×400 mm), eluted with petroleum ether-acetone (10 : 1, 6 : 1, 3 : 1, 1 : 1, 0 : 1, successively). Compound 1 (363.5 mg) and 2 (200.0 mg) were obtained by crystallization from acetone solution of Fr. A (7.9 g). Fr. B (794.7 mg) was further separated over Sephadex LH-20 column eluted with CHCl3-MeOH (1 : 1) to yield subfractions B1 (210.0 mg), B2 (39.0 mg), B3 (25.0 mg), B4 (200.0 mg), and B5 (169.1 mg). Compound 3 (20.4 mg) was crystallized from acetone of fr. B2. Compound 4 (15.0mg) was crystallized from methanol solution of fr. B5. The mother liquid of fr. B5 was separated by semi-preparative HPLC (MeOH/H2O, 49/51, 2.5 mL/min, 254 nm) to yield compound 5 (14.7 mg). Fr. C (10.0 g) was separated by Sephadex LH-20 column eluted with CHCl3-MeOH (1 : 1) to yield subfraction C1 (110.0 mg), compound 6 (9.5 g) and subfraction C2 (240.0 mg). Subfraction C2 was further separated by HPLC (MeOH/H2O, 37/63, 2 mL/min, 254 nm) to afford compound 7 (12.5 mg). Compound 8 (18.0 mg) was crystallized from acetone of Fr. D (900 mg). The remaining Fr. D was separated by HPLC (MeOH/H2O, 35/65, 2 mL/min, 254 nm) to afford compound 9 (13.0 mg). 1.4 Biological assays Compounds were tested for antimicrobial activities against the selected microbial strains by using the Oxford cup method [15]. The bacteria were cultured using medium (dextrose 20.0 g/L, beef infusion 10 g/L, NaCl 5 g/L, agar 17g/L). The fungi were cultured using PDA slant. The sample dissolved in DMSO (200 μL, 0.95 μg/mL) was added into each cup, DMSO as negative control. The diameters of inhibition zones were measured after incubating at 37 ºC for 24 h (bacteria) and for 3 days at 28 ºC (fungi). 1.5 Statistical analysis The antimicrobial activity was expressed as diameter value of inhibition zones. Each test was done in three replicates, and the result was presented as mean±SD. All statistical tests were carried out using the SPSS 11.5 for Windows. 2 Results 2.1 Structure identification Ergosterol (1): colorless needle crystal (acetone); [α] 20 −125° (c 1.0, CHCl3); ESI-MS m/z: 397 [M + H]+; D 1H NMR (600 MHz,CDCl3): δ 5.58 (1H, dd, J = 5.4, 2.2 Hz, H-6), 5.38 (1H, dd, J = 5.5, 2.8 Hz, H-7), 5.15 and 5.20 (each 1H, dd, J = 15.6, 7.8 Hz, H-22, 23), 3.63 (1H, m, H-3), 1.03 (3H, d, J = 6.6 Hz, H-21), 0.95 (3H, s, H-19), 0.92 (3H, d, J = 6.6 Hz, H-28), 0.83 and 0.82 (each 3H, d, J = 7.2 Hz, H-26, 27), 0.63 (3H, s, H-18); 13C-NMR (150 MHz, CDCl3): δ 141.5 (C-8), 139.9 (C-5), 135.7 (C-22), 132.2 (C-23), 119.8 (C-6), 116.5 (C-7), 70.6 (C-3), 55.9 (C-17), 54.7 (C-14), 46.4 (C-9), 43.05 (C-13), 43.03 (C-24), 41.0 (C-4), 40.6 (C-12), 39.3 (C-12), 38.6 (C-1), 37.2 (C-10), 33.3 (C-25), 32.2 (C-2), 28.5 (C-16), 23.2 (C-15), 21.32 (C-11), 21.30 (C-21), 20.15 (C-27), 19.8 (C-26), 17.8 (C-28), 16.4 (C-19), 12.3 (C-18). The NMR data were consistent with those of ergosterol [16]. (22E, 24R)-Ergosta-7, 22-diene-3β, 5α, 6β-triol (2): colorless needles (CHCl3); [α] 20 −64° (c 0.1, Pyridine); D ESI-MS m/z: 431 [M + H]+; 1H-NMR (600 MHz, Pyridine-d5): δ 5.72 (1H, brs, H-7), 5.24 (1H, dd, J = 15.2, 7.2 Hz, H-22), 5.17 (1H, dd, J = 15.2, 7.2 Hz, H-23), 4.83 (1H, m, H-3), 4.30 (1H, s, H-6), 1.50 (3H, s, H-19), 1.03 (3H, d, J = 6.7 Hz, H-21), 0.92 (3H, d, J = 6.7 Hz, H-28), 0.83 (6H, d, J = 4.9 Hz, H-26, H-27), 0.63 (3H, s, H-18); 13C-NMR (150 MHz, Pyridine-d5): δ 141.5 (C-8), 136.1 (C-22), 132.0 (C-23), 120.4 (C-7), 76.1 (C-5), 74.2 (C-6), 67.5 (C-3), 56.1 (C-17), 55.2 (C-14), 43.7 (C-9, C-13), 43.0 (C-24), 42.0 (C-4), 40.8 (C-20), 39.8 (C-12), 38.0 (C-10), 33.8 (C-2), 33.3 (C-25), 32.6 (C-1), 28.4 (C-16), 23.4 (C-15), 22.4 (C-11), 21.3 (C-27), 20.1 (C-26), 19.8 (C-21), 18.8 (C-19), 17.8 (C-28), 12.5 (C-18). We identified compound 2 as (22E, 24R)-ergosta-7, 22-diene-3β, 5α, 6β-triol by comparing its NMR data with those reported [17]. 28 22 21 12 19 2 HO OH 27 OH 16 2 15 H HO 6 O 3 OH OH 1 2' 11 H 7 4 25 16 14 8 24 17 13 9 10 H 5 3 23 11 1 26 20 18 1' OH 3' H3C O O 4 3 2 O H 6 1' 1 3 2 5 OH O 10 H3C 6 5 4 4 4a 5 7 8a 8 3 3 9 HO O 1 7 2 CH3 6 2 1 CHO 6 5 4a 8 HO HO 9 9' 9a NH2 9'a 5 6' 1 2 5' 4'a 7 4 3 O O 10 10' 8' 7' 4 5a 1' 2' 4' 3' OH OH O 2' (s) CH3 3' 9 OH OH O OH OH COOH 5 4 6 3 2 7 8 9 N 5 9N 4 6 N1 8 HO N1 H 5' 2 3 O H 1' H 3' 2' H OH OH 4' H N 7 8 6 Fig. 1 Structure of the secondary metabolites from Chaetomium gracile Glycerol monopalmitate (3): White amorphous power; HR-ESIMS (positive mode) m/z: 353.2669 [M + Na]+; IR (KBr) νmax: 3383 (OH), 2955, 2917, 2850, 1739, 1730, 1697, 1631, 1469, 1418, 1393, 1288, 1267, 1244, 1221, 1197, 1181, 1122, 1114, 1105, 1063, 1046, 993, 944, 720 cm-1; 1H NMR (400 MHz, CDCl3): δ 4.17 (1 H, dd, J = 11.6, 4.7 Hz, H-1′a), 4.12 (1 H, dd, J = 11.6, 6.1 Hz, H-1′b), 3.94 (1 H, m, H-2′), 3.67 (1 H, dd, J = 11.5, 3.9 Hz, H-3′a), 3.57 (1 H, dd, J = 11.5, 5.8 Hz, H-3′b), 2.32 (2 H, t, J = 7.6 Hz, H-2), 1.59 (2 H, m, J = 7.1 Hz, H-3), 1.24 (24 H, overlapped), 0.85 (3 H, t, J = 6.7 Hz, H-16). The 1H-NMR and IR data of compound 2 were in accordance with those of glycerol monopalmitate [18]. Eugenitol (4): white amprohous power; HR-ESIMS (positive mode) m/z: 207.0661 [M + H]+; 1H NMR (400 MHz, Acetone-d6): δ 13.14 (s, 1H, 5-OH), 6.45 (s, 1H, H-8), 6.07 (s, 1H, H-3), 2.37 (s, 3H, H-9), 2.08 (s, 3H, H-10); 13CNMR (100MHz, Acetone-d6): δ 168.0 (C-2), 108.0 (C-3), 183.2 (C-4), 104.7 (C-4a), 160.3 (C-5), 108.9 (C-6), 162.7 (C-7), 93.0 (C-8), 156.9 (C-8a), 20.3(C-9), 7.4 (C-10). It was identified to be eugenitol by comparing its NMR data with those reported [19]. p-Hydroxybenzaldehyde (5): Colorless crystal; HR-ESIMS (positive mode) m/z: 145.0981 [M + Na] +; 1H NMR (400 MHz, Acetone-d6): δ 9.86 (1 H, s, CHO), 7.81 (2 H, d, J = 8.5Hz), 7.02 (2 H, d, J = 8.5 Hz); 13C NMR (100MHz, Acetone-d6): δ 130.5 (C-1), 131.7 (C-2, C-6), 116.8 (C-3, C-5), 164.2 (C-4). It was identified as p-hydroxybenzaldehyde by comparing the spectroscopic data with those reported [20]. Chaetochromin A (6): Yellow amorphous powder; [α] 20 + 630° (c 0.1, CHCl3); ESI-MS (negative mode) D m/z: 545 [M−H]−, ESI-MS (positive mode) m/z: 569 [M + Na] +; 1H NMR (400 MHz, CDCl3): δ 4.15 (1 H, dq, J = 12.3, 6.1 Hz), 2.59 (1 H, dq, J = 13.8, 6.9 Hz), 6.41 (1 H, s), 5.90 (1 H, s), 1.42 (3 H ,d, J = 6.1 Hz), 1.21 (3 H, d, J = 6.9 Hz),15.15 (1H, s), 9.53 (1H, s); 13CNMR (100 MHz, CDCl3):δ 78.6 (C-2, C-2′), 46.4 (C-3, C-3′), 201.0 (C-4, C-4′), 100.0 (C-4a, C-4a′), 164.6 (C-5, C-5′), 105.7 (C -5a, C- 5a′), 160.1 (C-6, C-6′), 99.6 (C-7, C-7′), 160.1 (C-8, C-8′), 102.2 (C-9, C-9′), 142.2 (C-9a, C-9a′), 99.6 (C-10, C-10′), 156.5 (C-10a, C-10a′), 19.8 (2-CH3, 2′-CH3), 10.1 (3-CH3, 3′-CH3). Compound 6 was identified as chaetochromin A by comparing its MS, NMR spectra and optical rotation values with those reported [21]. Indole-3-carboxylic acid (7): white solid powder; HR-ESIMS (positive mode): m/z 184.0372 [M + Na] +; 1H NMR (400 MHz, CD3OD): δ 8.02 (1 H, d, J = 6.9 Hz, H-4), 7.91 (1 H, s, H-2), 7.40 (1 H, d, J = 7.2 Hz, H-7), 7.19 (2 H, m, H-5, 6); 13C NMR (100 MHz, DMSO-d6): δ 165.9 (-COOH), 136.4 (C-8), 132.3 (C-2), 126.0 (C-9), 122.1 (C- 5), 120.9 (C- 6), 120.5 (C- 4), 112.2 (C- 7), 107.3 (C- 3). The 1H-NMR data and 13C-NMR data of compound 6 were identical with those of indole-3-carboxylic acid [22]. Adenosine (8): colorless amorphous powder; HR-ESIMS (positive mode): m/z 268 [M + H] +; 1H NMR (400 MHz, Pyridine-d5): δ 8.75 (1H, s, H-2), 8.63 (1 H, s, H-8), 8.42 (2 H, brs, NH2), 6.74 (1 H, d, J = 5.9 Hz, H-1′), 5.54 (1 H, m, H-2′), 5.09 (1 H, dd, J = 4.9, 3.1 Hz, H-3′), 4.79 (1 H, q, J = 2.6 Hz, H-4′), 4.32 (1 H, dd, J =12.3, 2.6 Hz, Hb-5′), 4.16 (1H, dd, J = 12.3, 2.7 Hz, Ha-5′); 13C NMR (100 MHz, Pyridine-d5): δ 153.7 (C-2), 121.9 (C-5), 158.7 (C-6), 141.0 (C-8), 150.5 (C-4), 91.3 (C-1′), 76.0 (C-2′), 72.8 (C-3′), 88.2 (C-4′), 63.5 (C-5′). The MS and NMR data were consistent with those reported [23]. Chaetoquadrin F (9): white amorphous powder; [α] 20 + 39° (c 0.2, MeOH); HR-ESIMS (positive mode): D m/z 185.0816 [M + H] +; 1H NMR (600 MHz, CD3OD): δ 6.08 (s, 1H, H-5), 4.11 (1H , dd, J = 12.8, 6.2 Hz, H-2′), 2.56 (2H , qd, J = 14.4, 6.4 Hz, H-1′), 1.86 (3H , s, 3-CH3), 1.23 (3H , d, J = 6.2 Hz, H-3′); 13C NMR (150 MHz, CD3OD ): δ 169.3 (C-2), 167.9 (C-4), 162.1 (C-6), 103.0 (C-5), 99.4 (C-3), 66.3 (C-2′), 44.0 (C-1′), 23.4 (C-3′), 8.3 (3-CH3). The NMR data of compound 8 were in accordance with those of chaetoquadrin F [24]. 2.2 Biological Activities In the antibacterial test, compound 6 showed significant antibacterial activity against E.coli, S. aureus, and B. subtilis at concentration of 0.95 μg/mL with methicillin (2.5 μg/mL) as positive control. Compound 6 possessed no antifungal activity against the selected fungi. Compounds 1-5 and 7-9 showed no antimicrobial activity against bacteria (>50 μg/mL), and fungi (>200 μg/mL). 7-9b,c Methicillinb,c DMSO 14.0±0.9 -- 16.3±0.1 -- -- 11.2±1.0 -- 12.0±0.4 -- -- 12.2±1.2 -- 12.2±0.3 -- 1-5b,c 6b,c E.coli --a S. aureus B. subtilis Selected fungi -- -- -- -- -- Table 1 Antibacterial and antifungi activity of compounds 1-9 a. -- denotes no measurable halo; b. The concentrations of 1-5 and 7-9 tested against E.coli, S. aureus and B. subtilis were over 50 μg/mL, while the concentration of compound 6 was 0.95 μg/mL and the methicillin was at 2.5μg/mL; c. The concentrations of all of the compounds tested against fungi were over 200 μg/mL. 3. Discussion Chaetomium gracile was reported in 1959 by Shun-Ichi Udgawa, and Kiyotaka Koyama reported that four chaetochromins were isolated from C. gracile [21], and recent studies were mostly focused on xylanase gene and dextranase from this fungus [25_26]. In this study, all compounds (except chaetochromin A) were firstly isolated and identified from C. gracile on the basis of spectral data. Chaetochromin A exhibited strong antimicrobial activity against E. coli, S. aureus, and B. subtilis at concentration of 0.95 μg/mL. It was firstly isolated from C. thielavioideum CHEN NHL2829 in 1980, which induced delayed liver injures in mice and teratogenicity to mice embryo [27-29]. Chaetochromin A showed inhibitory effects on nitric oxide production by activated macrophages with IC50 of 0.8 μM and midbrain cells on KB cells [30]. [31] It also possessed obvious inhibition (IC50 = 0.13-0.24 μg/mL) in mouse embryo limb bud and could inhibit protein biosynthesis and deoxyribonucleic acid to cause strong cytotoxicity [32]. In this study, chaetochromin A was the major metabolite with a percentage of 32.7% in the extract, suggesting that this fungus is a valuable source for chaetochromin A. Reference 1 Stadler M, Keller NP, Paradigm shifts in fungal secondary metabolite research [J]. Mycol Res, 2008, 112 (2): 127-130 2 Cutler HG. Biologically active natural products from fungi: templates for tomorrow’s pesticides [M]. In bioregulators, chemistry anduses, Ory RL, Rittig FR, (eds) American Chemical Society: Washington, DC, 1984: 153-170 3 Chin YW, Balunas MJ, Chai HB, Kinghorn AD. Drug discovery from natural sources [J]. The AAPS Journal, 2006, 8 (2): 239-253 4 Debbab A, Aly AH, Proksch P. Bioactive secondary metabolites from endophytes and associated marine derived fungi [J]. Fungal Divers, 2011, 49 (1): 1-12 5 Park JH, Choi GJ, Jang KS, Lim HK, Kim HT, Cho KY, Kim JC. Antifungal activity against plant pathogenic fungi of chaetoviridins isolated from Chaetomium globosum [J]. FEMS Microbiol Lett, 2005, 252 (2): 309-313 6 Bashyal BP, Wijeratne EM, Faeth SH, Gunatilaka AA. Globosumones A-C, cytotoxic orsellinic acid esters from the sonoran desert endophytic fungus Chaetomium globosum [J]. J Nat Prod, 2005, 68 (5): 724-728 7 Zhang J, Ge HM, Jiao RH, Li J, Peng H, Wang YR, Wu JH, Song YC, Tan RX. Cytotoxic chaetoglobosins from the endophyte Chaetomium globosum [J]. Planta Med, 2010, 76 (16): 1910-1914 8 Itoh Y, Kodama K, Furuya K, Takahashi S, Haneishi T, Takiguchi Y, Arai M. A new sesquiterpene antibiotic, heptelidic acid producing organisms, fermentation, isolation and characterization [J]. J Antibiot, 1980, 33 (5): 468-473 9 Jiao W, Feng Y, Blunt J, Cole AL, Munro MH. Chaetoglobosins Q, R, and T, three further new metabolites from Chaetomium globosum [J]. J Nat Prod, 2004, 67 (10): 1722-1725 10 Zhang Q, Li HQ, Zong SC, Gao JM, Zhang AL. Chemical and bioactive diversities of the genus Chaetomium secondary metabolites [J]. Mini Rev Med Chem, 2012, 12 (2): 127-148 11 Xu GB, Li LM, Yang T, Zhang GL, Li GY. Chaetoconvosins A and B, alkaloids with new skeleton from fungus Chaetomium convolutum [J]. Org Lett, 2012, 14 (23): 6025-6055 12 Li GY, Li BG, Yang T, Yan JF, Liu GY, Zhang GL. Chaetocochins A-C, epipolythiodioxopiperazines from Chaetomium cochliodes [J]. J Nat Prod, 2006, 69 (9): 1374-1376 13 Li GY, Li BG, Yang T, Liu GY, Zhang GL. Secondary metabolites from the fungus Chaetomium brasiliense [J]. Helv Chim Acta, 2008, 91(1): 124-129 14 Yang EC, Yang T, Li ZZ, Liu GY, Li GY. Antimicrobial activity of the epipolythiodioxopiperazines from Chaetomium cochliodes. [J]. Nat Prod Res Dev, 2008, 20: 953-955,963 15 Carlson HJ, Bissell HD, Mueller MG. Antimalarial and antibacterial substances separated from higher plants [J]. J Bacteriol, 1946, 52 (2): 155-168 16 Noboru S, Hideyuki T, Kazuo U, Yutaka H, Kenji K, Hideo I. Sterol analysis of DMI-resistant and sensitive of Venturia inaeaualis [J]. Phytochemistry, 1996, 41(5): 1301-1308 17 Piccialli V, Sica D. Four new trihydroxylated sterols from the sponge Spongionella gracillis [J]. J Nat Prod, 1987, 50 (5): 915-920. 18 Chen XZ, Li GY, WU XQ, Huang QC, Zhang GL. Chemical study on Sambucus adnata Wall [J]. Chin J Appl Environ Biol, 2010, 16 (2):197-201 19 Fox CH, Huneck S. The formation of rocellic acid, eugenitol, eugenitin and rupicolin by the mycobiont of Lecanora rupicola [J]. Phytochemistry, 1969, 8 (7): 1301-1304 20 Ayer WA, Browne LM, Feng MC, Orszanska H, Saeedi-Ghomi H. The chemistry of the blue stain fungi. Part 1. Some metabolites of ceratocystis species associated with mountain pine beetle infected lodgepole pine [J]. Can J Chem, 1986, 64 : 904-909 21 Koyama K, Natori S. Chaetochromins B, C and D, Bis (naphtho-γ-pyrone) derivatives from Chaetomium gracile [J]. Chem Pharm Bull, 1987, 35 (2): 578-584. 22 Ren HC, Qin RD, Zhang QY, Cheng W, Liang H. Chemical constituents of Pilea cavalerei subsp. Cavaleriei [J]. Chin J Chin Mater Med, 2012, 37(17): 2581-2584 23 Yang SL, Liu XK. Nucleosides from Smilacina atropurpurea [J]. Chin J Nat Med, 2003, 1 (4): 196-198 24 Fujimoto H, Nozawa M, Okuyama E, Ishibashi M. Five new chromones possessing monoamine oxidase inhibitory activity from an ascomycete, Chaetomium quadrangulatum [J]. Chem Pharm Bull, 2003, 51 (3): 247-251 25 Rao U, Kato M, Kobayashi T, Tsukagoshi N. Characterization of AnRP-mediated negative regulation of the xylanase gene, cgxA, from Chaetomium gracile in Aspergillus nidulans [J]. Lett Appl Microbio, 2003, 36 (1): 59-63 26 Rao U, Kato M, Kobayashi T, Tsukagoshi N. Regulationof the xylanase gene, cgxA, from Chaetomium gracile by transcriptional factors, XlnR and AnRP [J]. Biotechnol Lett, 2002, 24 (13): 1089-1096 27 Ohtsubo, K. Oral toxicity of chaetochromin, a new mycotoxin produced by Chaetomium virescens, to mice [J]. Proc Jpn Assoc Mycotoxicol, 1980, 12: 28-29 28 Ohtsubo, K. Hematopoietic injury and liver necrosis in the mice fed chaetochromin-containing moldy rice diet [J]. Proc Jpn Assoc Mycotoxicol, 1982, 15: 25-27. 29 ItoY, Ohtsubo K. Teratogenicity of oral chaetochromin, a polyphenolic mycotoxin produced by Chaetomium spp., to mice embryo [J]. Bull Environ Contam Toxicol, 1987, 39 (2): 299-303 30 Ishii R, Horie M, Koyama K, Ishikawa Y, Kitanaka S. Inhibitory effects of fungal bis(naphtha-gamma-pyrone) derivatives on nitric oxide production by a murine macrophage-like cell line, RAW 264.7, activated by lipopolysaccharide and interferon-gamma [J]. Bio Pharm Bull, 2005, 28 (5): 786-790. 31 Tsuchiya T, Sekita S, Koyama K, Natori S, Takahashi A. Effect of chaetochromin A, chaetochromin D and ustilaginoidin A, bis (naphtho-γ-pyrone) derivatives, on the mouse embryo limb bud and midbrain cells in culture [J]. Congenit Anom, 1987, 27 (3): 245-250. 32 Koyama K, Ominato K, Natori S, Tashiro T, Tsuruo T. Cytotoxicity and antitumor activities of fungal bis(naphtho-γ-pyrone) derivatives [J]. J. Pharmacobiodyn. 1988, 11 (9): 630-635.