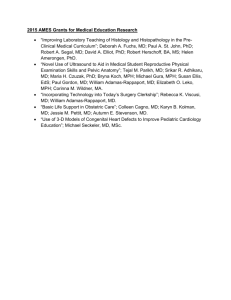
View the poster abstracts - MICHR
advertisement

Poster Abstracts POSTER CATEGORIES Community Partner/Healthcare Provider or Professional: Abstracts # 1-10 Student: Abstracts # 11-13 Faculty/Staff: Abstracts # 14-23 1. Asthma Camp Improves Children’s Asthma Knowledge and Self-Efficacy Lori McQuillan, Joni Zyber, Janice Roberts, Michelle Cox, Donna Bruce Abstract:To dispel misperceptions about asthma and exercise we have instituted an annual Asthma Camp to educate patients and parents to pay attention to asthma symptoms and the importance of taking their medications, even when they feel well. With education, physical activity and camaraderie asthmatic children can better understand their disease, and listening to their bodies and reduce their risk of an asthma attack. Objective: To provide a camping experience for kids with asthma that supports asthma self-care. Design/Method: We recruited a total of 20 children between the ages of 7 and 14 who have been diagnosed with asthma. A pre-experimental onegroup pretest/posttest design was used. Education was in the form of games and activities using the teach-back method. Parents/guardians were mailed the 3-month follow-up questionnaire to determine their satisfaction with the camp and if any reportable changes in the child’s asthma has occurred. Results: The majority of the children (70%) had never been to any camp before, and 30% percent had attended this camp before. Questions on perceived self-efficacy and general asthma knowledge were asked and the kids increased their knowledge on all questions asked. Most of the children already knew about asthma, the triggers, the symptoms and the importance of taking their medication, which we would like to believe is partly due to the education they received from their Asthma nurse or physician. . 2. Implementation of Post-Discharge Telephone Follow-Up with Pediatric Patients; A Comparison of Two Interview Tools Renay Gagleard, Mahesh Sharman, Brian Nolan, D. Kay Taylor, Lori McQuillan, Laurie Shafer, Mattie Pearson, and Jill Folts Background: There has been a renewed focus to improve upon discharge information. Follow-up calls prove to be an invaluable tool in increasing post-discharge compliance. Objective: To determine the effectiveness of a revised tool used for follow up calls to parents of discharged pediatric patients. Design/Methods: Questionnaire #1 asked child’s post-discharge condition, if prescriptions were filled, and if appointments were made. After one year, the tool was revised to ask if the parent name the prescribed meds, the Dr. to be followed up with, and the child’s health status. This was expected to provide us with more insight into improving the discharge follow-up telephone protocol so that we could better identify and tackle problems with readmissions. Results: While this study did not prove that one form was better than the other in a statistical sense, questionnaire #2 did ask more and clearer questions than questionnaire #1, so one could surmise that the change was for the better. Also, this study is a useful step to our overall Quality Improvement goal and will be an important step in the next few studies; which includes a new Asthma Navigator program to reach out to patients discharged with an asthma diagnosis and a future plan to institute a Diabetes Navigator as well. Conclusion: While no statistical significance was made in this study, many qualitative findings were noted that lead to us considering this study a success. These calls DO make a difference and are now an important part of our standard operations. 3. Improving Patient Outcomes Virtually: Converting Evidence-Based Practice to Action Kristen Miller, DrPH, MSPH, Beth King, RN, BSN, MA, CCM Despite the power of modern medicine and the introduction of complex technologies, medicines, and treatments, hospital-acquired conditions continue to develop in patients - conditions that could reasonably have been prevented through the application of evidence-based guidelines. To combat hospital-acquired conditions and similar preventable conditions, the VA National Center for Patient Safety adapted the IHI Breakthrough Series (BTS) model into a virtual collaborative based on evidence-based guidelines which has resulted in improved patient-centered outcomes. The BTS combines condition-specific subject matter experts with coaches to help hospital unit teams select, test, and implement changes. Hospital teams focus on improving patient outcomes by systematically implementing evidence-based practice at the bedside. Past BTS have included Prevention of Injurious Falls and Reducing Postoperative Respiratory Failure. A current collaborative is focused the Prevention of HospitalAcquired Conditions: Catheter-Associated Urinary Tract Infections (CAUTI) or Hospital Acquired Pressure Ulcers (HAPU). Based on a culture of safety and quality improvement, the collaborative learning includes leadership, evidence-based practice, data-driven decision-making, communication, teamwork, a learning culture, and patientcenteredness. This model of implementation is efficient and effective for multi-unit improvement efforts. Many innovative health care organizations have made important breakthroughs in the design and performance of safer systems by focusing on evidence-based practice. The VA National Center for Patient Safety has demonstrated success leading collaboratives using this model. Researchers have published significant evidence on methods of prevention and the Veterans Health Care Administration (VHA) has been a leader on many efforts for years. 4. Employing Community Led Strategies to Address Gender-based Analysis Findings and Improve Health Equity in African American Women Sandy Waddell, RN, BSN; Jodi Burke, MSW; Arthur Franke, PhD A gender-based analysis and community led needs assessment in Inkster, Michigan revealed that women are disadvantaged due to social determinants of health. Psychosocial, economic, and environmental factors were identified as significant challenges in navigating the health care system and to adopting healthier lifestyles that could prevent and control diabetes. Compared to Michigan, Inkster has lower income and education, both of which are significant predictors of health. Multi-level socioecological approaches including empowering women with tools to make healthy choices, promoting social interactions, supporting healthy decision making, reducing access barriers to health care and partnering with community health workers (CHW’s), were employed. A community-engaged implementation method was used to address health inequities, specifically how to effectively improve diabetes-related health practices influenced by gender. Three approaches were selected: health literacy mentoring, increasing opportunities for access and use of community preventive services using CHW’s; and providing messages designed to positively influence lifestyle and gender norms. This project goals are to improve overall health status and diabetes self-management of African-American women in Inkster by: (1) Implementing a socioecological approach to disease management using social support, empowerment, and health literacy; (2) Improve access to and utilization of health care services and community supportive resources to promote healthy lifestyles; and (3) Build community networks and increase awareness of gender-based disparities and their impact on women. Data will be analyzed for changes in attitudes and behaviors to assess the effectiveness of community led gender-based approaches as a promising method to improve diabetes-related health management and outcomes in women. 5. Healthy Men Healthy Communities Rohan Jeremiah, PhD, MPH, Glenda Sneed, MA, Trudy Hall, MPH The purpose of this study was to provide health and wellness information with measurement tools and metrics to African American fraternity members of the Ann Arbor-Ypsilanti-Inkster Alumni Chapter of the Kappa Alpha Psi Fraternity. Furthermore, this program also convened a health summit to educate its members on ways to monitor their personal health status as well as to keep personal health a priority. The study methods included administering a men’s health needs assessment and presenting the results at a first African American Men’s Health Summit. Our findings indicate that most fraternity members represented a higher socioeconomic status (SES) in contrast other African American men in their communities. However, despite a higher SES status and access to health insurance, most fraternity members had similar patterns of concerns for chronic health conditions. The significance of this study draws attention to fact that higher income, education and access to health insurance were not protective factors for the fraternity men’s health outcomes. The implications of our findings motivated several men consider establishing a community health advocate program to educate and motivate African American men to be aware of their health status. 6. Surgical Stapler Adverse Events in the Veterans Health Administration: Root Causes and Lessons Learned Helen J.A. Fuller, Ph.D., Douglas E. Paull, M.D., Linda Williams, R.N. M.S.I. Many operations require the controlled ligation and division of blood vessels and other structures, often through use of a combined cutting and stapling device. Previous studies have found low rates of stapler malfunction, but because of the prevalence of use, many patients may still be affected. Device malfunction has been identified in some cases, and use error, including override of safety functions, may also play a role. The Veterans Health Administration’s Root Cause Analysis (RCA) database was searched for events involving use of a non-skin closure surgical stapler. The resulting 12 RCAs from 13 adverse events were examined. The operations were pulmonary surgery (7/13), laparoscopic nephrectomy (3/13), and bowel surgery (3/13). Patient outcome was death in 46% of cases, transfusion with survival in 31%, and bleeding with no transfusion specified in 23%. Surgical stapler failure mode was unspecified in 5/13 cases. There were two cases in which the failure was identified as a misfire. There were two cases of staple line failure. In addition, there was one case each of the following: use of the stapler without a cartridge; improperly formed staples; and a tear along the suture line. Contributing factors were possible malfunction (4/13), unfamiliarity with device (3/13), and misaligned stapler cartridge (1/13). There are vulnerabilities in the device design that are often not obvious on visual inspection. Since the source of harm may derive from multiple causes and adverse outcomes are rare, the surgical team may not be sufficiently aware of the risk posed by the device. 7. Life Goals Collaborative Care to Improve Health Outcomes for Veterans with Serious Mental Illness Michelle M. Barbaresso, MPH, Margretta G. Bramlet, MEd, Amy M. Kilbourne, PhD, MPH, Kristina M. Nord, MSW, Zongshan Lai, MPH, Lilia Verchinina, PhD, MA, David E. Goodrich, EdD, Joanna G. Bratton, BSW Individuals with serious mental illnesses (SMI, including schizophrenia, bipolar disorder, and major depression) experience a disproportionate burden of medical comorbidity, particularly increased risk of cardiovascular disease (CVD), and are more likely to die earlier than the general population. Life Goals Collaborative Care (LGCC) is an evidence-based collaborative care program designed to address suboptimal health behaviors and the lack of medical care coordination that may increase risk of CVD among persons with SMI. In previous studies, LGCC has been shown to improve physical and mental health outcomes for persons with bipolar disorder, but to date, has not been tested for a broader SMI patient population. The goal of this single-blind randomized controlled trial is to determine whether LGCC, which combines health behavior change strategies with Chronic Care Model principles, compared to usual care improves outcomes and reduces CVD risk among patients with SMI. Our primary hypotheses are that within 12 months, LGCC will be associated with reduced CVD risk factors (lower blood pressure, lower cholesterol or blood sugar levels, or decreased weight), improved health-related quality of life, reduced psychiatric symptoms, or improved health behaviors compared to usual care. In this single-blind randomized controlled effectiveness trial, patients diagnosed with SMI and >=1 CVD risk factor receiving care at The VA Ann Arbor Mental Health outpatient clinic randomized to the LGCC intervention or usual care. LGCC is an evidence-based psychosocial program designed to promote health behavior change and in this study, includes 5 selfmanagement sessions covering personal goal-setting and mental health symptom management reinforced through healthy lifestyles; identification and monitoring of patient medical risk factors via a registry; and medical care management and coordination of care with general medical providers. Primary outcomes assessed at 6 and 12 months include changes in CVD risk factors (e.g., blood pressure, BMI), psychiatric symptoms, and health-related quality of life. Evidence-based interventions such as LGCC, that combine healthy lifestyle coaching with Chronic Care Model principles, may lead to improved health outcomes for patients with SMI and CVD risk factors. Findings from this randomized controlled trial will inform ongoing initiatives to implement collaborative care programs for persons with SMI. 8. Latino Health Equity is Crucial in Washtenaw County Adreanne Waller, Daniel J. Kruger, Charo Ledon, Sharon P. Sheldon, Mikel Llanes, Felipe Riaño, Leonardo Riaño, Glenda Isela Flores Title IV of the Affordable Care Act (ACA) emphasizes the need to "allow for the ongoing, accurate, and timely collection and evaluation of data on disparities in health care services and performance on the basis of race, ethnicity, sex, primary language, and disability status [to enable the utilization of] preventive services to promote wellness, reduce health disparities, and mitigate chronic disease." Between 2000 and 2010, the proportion of Hispanic Washtenaw County residents increased 125% and is projected to increase 233% between 1990-2035. Hispanic births in Washtenaw County increased 151% between 2000-2009. This young and growing population is a critical cultural and economic contributor to our local economy. The average age of death of Washtenaw Latinos (58 years) is 17 years younger than that for Washtenaw Whites and six years younger than Blacks. Increasing access to healthy environments, employment, education and health care provides greater opportunity to maximize the mental and physical health, as well as productivity of these vital community members. To address the chronic lack of population health data on Washtenaw County Latinos, local public health, academics and Latino community collaborated on a community benefit driven assessment called Encuesta Buenos Vecinos (EBV). EBV was designed to assess and enhance the health, wellbeing, and social support of this population. Over 500 Washtenaw County Latinos responded to face-to-face, group and Internet surveys. This presentation will describe the links between health care utilization, access, barriers, diagnoses, as well as numerous associated social determinant predictors providing opportunity for informed intervention of ACA requirements. 9. Here for Youth: Developing and Mobilizing a Community Advisory Board to Assess and Improve Mental Health Services for Adolescents Kate Guzman, Caitlin Martin, Craig VanKempen, Max Abuelsa, Jessica Ashmore, Olatola Ibrahim, Carol Fisher, Laura Alexander, David Cordova Mental health problems play a significant role in the burden of disease in the United States (SAMHSA, 2013). Therefore, the prevention of mental health problems represents a major public health concern facing America. In Ypsilanti, the current study location, a recent needs assessment identified mental health as a tier-one priority. Primary health care centers, including the Corner Health Center, provide an innovative context to deliver mental health services to patients who otherwise would not receive mental health services. Mental health services are effective only to the extent that they are embraced by the community. Developing a community-advisory board (CAB) is essential to work toward this goal. Therefore, the purpose of this presentation is to describe the nature of developing and mobilizing a CAB in an effort to work toward assessing and improving mental health services for adolescents. Methods: The present study was guided by community-based participatory research (CBPR) principles. Consonant with CBPR tenets, we established a community advisory board (CAB) in an effort to (a) develop a process by which community members could contribute to identifying community strengths and challenges, (b) establish trust with members of the community, (c) facilitate the recruitment, engagement and retention of the targeted sample, and (d) ensure that research findings accurately described the needs of the community as perceived by participants (Isreal et al., 2005; Minkler and Wallerstein, 2003). In line with the Corner Health’s mission, the CAB represents diverse key stakeholders, including youth. Results: Preliminary findings indicate a marked enthusiasm among CAB members to participate in this process, as well as an increased knowledge among Corner Health Center staff with respect to community members’ perspectives on integrated health services. Conclusions: CBPR methods, including the development of a CAB, help ensure mental health services are tailored to meet the needs of the targeted community. This project has provided Corner Health Center staff the opportunity to learn and seek guidance from CAB members with regard to best practice approaches to integrating mental health services. Perhaps more importantly, this process aims to give voice to key stakeholders in the community, an opportunity that unfortunately is not always the case in research. These developments are necessary steps aimed at establishing community-university-based partnerships for enhanced patient-based outcomes. 10. Community priorities for patient-centered outcomes research Susan Dorr Goold, Zachary Rowe, Lisa Syzmecko, Marion Danis, Stephanie Solomon, Dan Myers, Charo Ledon, Terrance R. Campbell, Carla Cunningham, Sal Martinez Morally complex policy decisions, including research priority-setting, may enjoy greater public trust if they result from fair and public processes. Academic-community partnerships in Michigan and Missouri developed a version of CHAT (CHoosing All Together) to engage minority and underserved communities in deliberations (in English and Spanish) about patient centered outcomes research (PCOR) priorities. PCOR funding options were developed from existing funding priorities, interviews with community organizations and clinicians serving in underserved areas and other key informants. Groups deliberated for 2-2.5 hours in diverse communities. Data collection included pre- and post-deliberation surveys and individual and group priorities. To date, 10 groups (n=123) have deliberated in rural and urban settings. Over 3/4 of participants were minority, 1/3 reported income <$10,000, and 1/4 reported fair/poor health. Quality of life, special needs, patient-doctor relations and access were prioritized over comparing approaches to diagnosis and treatment. Asked “how much input do people like you have in setting research priorities?” 20% said a great deal, 64% some and 16% none at all. Asked “How much input should people like you have in setting research priorities?” 44% said a great deal, 53% some and 3% none at all. Nearly all (94%) found the exercise easy to understand, 74% agreed “Our discussion included responding to each others' arguments,” and 77% agreed “I would trust a process like this to inform funding decisions.” Results suggest underrepresented populations welcome the opportunity to deliberate about PCOR priorities, and prioritize research on quality of life, special needs, patient-doctor relations and access. 11. Transforming Culturally Diverse Communities Through Music Education Michael Spencer, PhD, John Ellis, PhD, Michael Hopkins, PhD, Sue Ann Savas, MSW, Anthony Provenzano, MPA, MSW Candidate, Peter Felsman, PhD Candidate, Paula Dedoux, MSW Candidate El Sistema is a renowned Venezuelan music intervention program that has inspired a global movement due to its social impact on fighting poverty and improving the human condition. The El Sistema model provides high-quality music instruction to children from a broad range of socio-economic backgrounds in over twenty-five countries around the world (Fundacion, 2012). Internationally adopted, this socially innovative paradigm fills a special need in the corridor between Ann Arbor and Detroit, Michigan. This reasons for starting this pilot program in southeast Michigan are threefold: 1) serving socially, racially, and linguistically diverse children in the University of Michigan (U-M) community; 2) planning the scale up of the El Sistema music intervention to include schools and other venues in Detroit; and 3) developing a Social Engagement curriculum of greater depth for University of Michigan School of Music, Theatre, and Dance (SMTD). A single group pretest-posttest multi-method research design will be used to evaluate the effectiveness of the El Sistema Ann Arbor pilot project. The El Sistema program will target 5th grade string instrument students at Mitchell Elementary School. If the intervention is successful, it is expected that by having children participate in regularly and extensively high-quality, ensemble music education students will develop music literacy, a strong sense of personal agency, improved academic performance, and increased sense of community. In addition, U-M graduate student music instructors will develop a sense of social consciousness in delivering music instruction in untraditional community settings using the El Sistema pedagogical model. 12. Development of a theory based video to increase CPAP compliance Rie Suzuki, PhD Obstructive sleep apnea (OSA) is one of the most common sleep disorders, affecting an estimated 20 to 30 million Americans. Seventy percent of all patients with OSA are obese and eighty six percent of all obese patients with type 2 diabetes have OSA. The prevalence of OSA increases with age, with a higher prevalence in persons 65 years and older. However, few educational materials have targeted on the Aged Obese Diabetic OSA patient. The purpose of this project is to develop the theory based educational video for patients newly diagnosed with OSA at the University of Michigan Center for Sleep Disorders. The inclusion criteria encompasses patients aged 65 and older, a BMI >30, insulin dependent diabetic, and an apnea hypopnea index>15.The patients also have completed a baseline polysomnogram and are scheduled to return to the lab for a continuous positive airway pressure (CPAP) titration. Social Cognitive Theory was utilized for this project. The video will address not only the knowledge of OSA and diabetic nutrition but also the benefits and the strategies used to increase CPAP compliance and to increase healthy diabetic dieting in patients with OSA. The proposed research design is a pre-post test to access the impact of watching the developed video at home on wearing CPAP every night and eating 3 healthy diabetic meals per day. Self-efficacy, outcome expectations, social support, and knowledge of OSA, how to use CPAP, and the contents of diabetic diet will be measured. 13. Retained Guidewires - A Persistent Problem Theodore E. Dushane, Ph.D, M.D., Douglas E. Paull, M.D. Introduction: More than 6 million central venous catheters are placed each year in the United States. The guidewire can be left behind in the central circulation, which can result in numerous complications, some of them fatal. Because retained guidewires are frequently retrieved by interventional radiologists without long term harm, the problem has received little attention; we used the National Center for Patient Safety database from the 153 VA hospitals over a decade to find relevant root cause analyses (RCAs) and better to describe circumstances, causes, and proposed solutions. Methods: We found 30 RCAs. We coded the root causes using the NCPS Triage System for Root Cause Analysis. We coded the strengths of proposed actions from the RCAs as defined in The Healthcare Failure Mode Effect (HFMEA) Process. Results: We found significant harm using the NCC MERP Index. There was no predominant root cause. Most of the proposed solutions were weak according to the HFMEA Process. Discussion and Conclusions: Also of concern, the actions proposed among the RCA committees across the VA reveal the difficulty of solving device design issues. We will propose (in the poster) significant work-process improvements to ameliorate the situation until a hard fix for the problem is developed. 14. Public, Advocate, and Community-Practice Engagement in the Development of Decision Support Tools for Breast Cancer Alexandra Jeanpierre, MPH, Gregory Powers, MPH, Rachel Tocco, MA, Rebecca Morrison, MPH, Rose Juhasz, PhD, Sarah Hawley, PhD, MPH As part of a National Cancer Institute grant investigating the challenges of individualizing treatment for breast cancer patients, we developed an online decision support tool for newly diagnosed women with early-stage, invasive breast cancer. The tool is part of a randomized control trial to determine if an enhanced decision aid with patient-tailored components (i.e. knowledge building, values clarification, and patient activation) leads to greater patient knowledge about breast cancer treatment options, as well as a preference-concordant decision (i.e. treatment is consistent with the patient’s preferences). During tool development, we engaged with several stakeholder groups to elicit feedback on its content and implementation. Since nearly 1 in 8 (almost 12%) of women in the United States will develop invasive breast cancer over the course of her lifetime, we surveyed a sample of women from the general female population (n=250) on interest in decision support tools. Results from an online survey showed 56% were very or quite interested in a tool designed for them for a major health decision, while 57% were very or quite interested in one designed for a family member. We also conducted cognitive interviews and usability testing of the tool with breast cancer advocates to refine content and make technical improvements. Once the tool was finalized, the study was launched in several surgical practices in the Detroit and Atlanta metropolitan areas. We are currently seeking feedback on the implementation process from surgeons, nurses, and office managers who identify potential users and introduce them to the tool. 15. Assessing the modification, development and implementation of nutrition education curriculum appropriate for effectively working with cognitive impairements Michelle Gordon-Releford Cognitive Impaired/Special Needs (CI/SN) Nutrition Education Curriculum Committee consists of supervising Educators, programing staff and key community stakeholders who understand the needs of the population with CI/SN. Initial responsibilities of the Committee reviews current nutrition education curriculums, and identify best practices and desired outcomes as to how it applies to groups with CI/SN. Learning materials and evaluation materials will be modified for ease while keeping the integrity of the original curriculum. Staff is trained to interact respectfully with individuals with CI/SN, and how to administer the nutrition education curriculum, with modifications, appropriately. MSU Extension Human Resources and Organization Diversity Staff-External Diversity Organization oversee the training. Both departments encourage staff to approach the nutrition education curriculum with confidence to promote self-efficacy and selfsustainability to participants. Training will also insure consistency across the surveyed population where individuals with CI/SN will provide reliable survey data for the NPA work team to evaluate. The Committee works closely with Institutional Review Board to ensure that the curriculum adheres to accepted privacy and security of collected information and does not infringe on participant rights. Objectives: 1. Nutrition education that is appropriate and useful to CI/SN participants. 2. Increase self-efficacy and selfsustainability through nutrition education that includes food safety, budgeting, and nutrition. 3. Measurable changes in participant behavior will be documented through surveys and participant success stories. 4. Empowerment to market nutrition education to potential community partners who serve individuals with CI/SN. 5. Proficiency offering an additional venue for professional development, with an emphasis on diversity. 16. Cluster Randomized Adaptive Implementation Trial Comparing a Standard Versus Enhanced Implementation Intervention to Improve Uptake of an Effective Re-Engagement Program for Patients with Serious Mental Illness David E Goodrich, Nicholas W. Bowersox, Daniel Almirall, Zongshan Lai, Kristina M. Nord, Amy M. Kilbourne Poor continuity of medical care contributes to premature mortality in persons with serious mental illness. The Veterans Health Administration (VA) developed Re-Engage, an outreach program to identify Veterans with SMI lost-to-care and to reconnect them with VA services. However, such programs often encounter barriers getting implemented into routine care. Adaptive designs are needed when the implementation intervention requires augmentation within sites facing challenges. This poster describes the rationale for an adaptive design study to compare the effectiveness of a standard implementation strategy (Replicating Effective Programs- REP) with REP enhanced with External Facilitation (enhanced REP) to promote Re-Engage uptake. The study employs a four-phase, two-arm, longitudinal, clustered randomized trial design. VA sites (n=158) across the U.S. with a designated provider, at least one Veteran with SMI lostto-care, and who received REP during a 6-month run-in phase. Sites with inadequate uptake were stratified at the cluster level by geographic region and regional service network and randomized to REP (n=49) vs. enhanced REP (n=39) in Phase 2. The primary outcome was the percentage of Veterans on facility outreach lists documented in an electronic registry. The intervention consisted of REP versus REP enhanced by external phone facilitation consults. At 12 months, enhanced REP sites returned to REP and 36 sites with inadequate uptake received enhanced REP for six months in Phase 3. Secondary outcomes included the percentage of Veterans contacted directly and the percentage re-engaged in care. Adaptive designs may produce more relevant, rapid, and generalizable results by validating or rejecting new implementation strategies. 17. Research Program Partnerships to Examine Challenges of Individualizing Breast Cancer Care Rose Juhasz, PhD, Rachel Tocco, MA, Rebecca Morrison, MPH, Gregory Powers, MPH, Alexandra Jeanpierre, MPH, Ann Hamilton, PhD, Kevin Ward, PhD, Jennifer Griggs, MD, MPH, Christopher Friese, PhD, RN, Steven Katz, MD, MPH, The Cancer Surveillance and Outcomes Research Team has established numerous partnerships to lead a large program on the challenges of individualizing breast cancer care. We conduct patient-centered, population-based survey research in collaboration with several Surveillance, Epidemiology, and End Results (SEER) Programs of the National Cancer Institute. Our current study involves a survey of 6,600 patients with early-stage breast cancer to learn more about how these women make testing (Magnetic Resonance Imaging, BRCA genetic tests, and tumor tests) and treatment (surgery, chemotherapy, and radiation) decisions. Survey topics include a variety of patient-reported outcomes such as quality of life, worry about recurrence, satisfaction with testing and treatment decisions, and quality of provider communication. We work with the SEER registries at the Los Angeles County Cancer Surveillance Program (based at University of Southern California) and the Georgia Center for Cancer Statistics (based at Emory University) to ensure the diversity of our patient samples and to secure high response rates for surveys administered in English and Spanish. We also have partnerships with: 1) industry to acquire gene expression assay results for our respondents that estimate risk of cancer recurrence and 2) a cancer cooperative group conducting clinical trials to determine if respondents’ chemotherapy decisions are driven by a research protocol assignment. Taken together, these partnerships enable a detailed assessment of the individualization and quality of systemic and locoregional tests and treatments received by early-stage breast cancer patients. Study results will be used to improve the quality of care for women with breast cancer. 18. Supporting and maintaining strong partnerships and community-academic connections through evaluation of a statewide community health worker alliance Nicholas Yankey, MPH, MSW, Katherine Mitchell, MSW, Edith Kieffer, MPH, PhD, Caitlin Buechley, BS, Loan Nguyen, BA, Gloria Palmisano, BS, MA, Lee Anne Roman, MSN, PhD Partnerships are essential to supporting and promoting community health worker (CHW) sustainability. In Michigan, connections between community partners and academic institutions have facilitated CHW programs for years. Through these connections, the Michigan Community Health Worker Alliance (MiCHWA) formed to collaboratively support the CHW profession as a united group of stakeholders. Since identifying evaluation as essential to sustainability, MiCHWA’s Steering Committee incorporated evaluation as one of its goals and established the MiCHWA Program Evaluation Advisory Board. The board unites academic and community partners to develop and conduct MiCHWA’s process, context, and outcome evaluation. As an initiative that relies on stakeholder participation, MiCHWA’s evaluation focuses directly on building, maintaining, and strengthening partnerships to promote its work and support CHWs and their programs. The board conducted a partnership survey in 2012 and 2013 to assess Steering Committee member perceptions of the initiative and gauge partnership strength. The survey yielded quantitative and qualitative data showing improvement in Steering Committee members’ knowledge of other community agencies and CHW activities statewide. The data also identified areas for improvement, including new constituencies to add to the Steering Committee and steps to improve partnership activities. This poster will discuss key evaluation elements identified by our communityacademic evaluation board and the tools, findings, challenges, and next steps associated with evaluating partnerships like MiCHWA. The poster will also discuss the need for strong community-academic partnerships to maintain CHW alliances at the state level and maintain CHW programs at the local level. 19. Evaluation Partnership with a Community-Based Client Using a Collaborative, Utilization-Focused Approach: Girls Group, A Case Example Sue Ann Savas, MSW; Laura Sundstrom, MSW; Lindsey Miller, MSW Candidate Girls Group is a community-based program in serving Ann Arbor and Ypsilanti designed to enable young women to develop self-sufficiency and become first generation college students. Over the past ten years, Girls Group has provided individual mentoring and counseling, academic support, and empowerment programming, as well as many other groups, activities, workshops, and camps. The guiding principles for Girls Group are the development of character, leadership, self-confidence, and social consciousness. During the 2013-2014 academic year, with the support of the Community Foundation for Southeast Michigan, Girls Group is implementing a pilot of the Pioneer High School program, the first in-school programming for high school students. The Curtis Center Program Evaluation Group (CC-PEG) at the University Of Michigan School Of Social Work is partnering with Girls Group to evaluate the implementation of the Pioneer program. Using a collaborative, utilization-focused approach, CC-PEG will gather, analyze, report, and interpret program data for program improvement and internal capacity building. The mixed methods design utilizes surveys, observations, focus groups, and key informant interview with program participants, Girls Group staff, and stakeholders. The purpose of the evaluation is to assess the program’s impact on participants and to guide Girls Group on areas of development and capacity building. 20. Engaging High School Students in Injury Prevention Bethany Buschmann, MPH, Peter Ehrlich, MD, MSc, Susan Morrel-Samuels, MPH, MA, Joseph Filipiak Background: The University of Michigan Injury Center’s mission is to conduct highquality research and training, to translate scientific discoveries into practice and policy, and to reduce injuries, violence and related disabilities. The Outreach and Translation Core (OTC), aims to increase awareness and knowledge of injury and violence prevention topics, resources, and interventions and create partnerships within the community to expand the Center’s reach. Methods: To increase injury awareness among adolescents, the OTC implemented an injury prevention campaign contest in the winter of 2013 with Romulus High School in Metro Detroit. The OTC Coordinator delivered a presentation beforehand to the participating classrooms to educate the students on the contest details and provide them with an introduction to the field of injury prevention. Students were asked to create unique injury or violence prevention messages relevant to their peers, in the form of a print or multimedia project. The contest entries were evaluated on 4 criteria with a rating scale of 0 (poor) to 5 (excellent). Entries were judged on clarity (relevance to peers), presence of actionable prevention message, accuracy (images support content and free of grammar errors), and quality (overall design and preparation/effort). Results: In 2013, 28 students participated and 11 entries were submitted. This year student participation more than doubled; 65 students participated and 18 projects were submitted. Evaluation of the contest entries is currently in progress and a presentation will be held to recognize the winners and award them with Visa gift cards. 21. The Interdisciplinary Model: An Effective Approach to Patient Family-Centered Healthcare at a Tertiary Care Specialty Center Linda Yang, MD, PhD, Sheela Pandey, MSW, Denise Justice, OTLR, Kate Change, MS Objectives: In this study, we evaluated the program’s strengths, weaknesses, and opportunities for improving the patient centered care model as it relates to the care of children with brachial plexus injury. Methods: 50 patients with the diagnosis of Neonatal Brachial Plexus Palsy (NBPP) and their families (children between the ages of 2m-14y; 22 males and 28 females) were sequentially recruited from the University of Michigan NBPP clinic. Patients and families completed the “Family-Centered Care SelfAssessment Tool.” Questions were asked to understand how often patients/families experienced ideal care as they interacted with our interdisciplinary brachial plexus team. Results: The sections regarding “Giving Diagnosis” (2.7± .03) and “Decision Making” (2.53±.46) demonstrated good application of patient centered care, whereas “Family to Family and Peer Support” (1.72±1.07) and “Transitioning to Adulthood” (1.8±.95) afforded potential areas of improvement. Patients with Narakas Classification level 1 or 2 (less extensive) and their families had much better experiences with “Family to Family and Peer Support” than patients with Narakas Classification of level 3 or 4 (more extensive) and their families (p=.04). Conclusions: The “Family-Centered Care SelfAssessment Tool” was valuable in evaluating the strengths and weaknesses in patient centered care of patients with brachial plexus injury. 22. Evaluating the FATE Program: A commitment to Detroit youth in their pursuit to higher education Sue Ann Savas, MSW, Laura Sundstrom, MSW, Brandon Alford, MSW Candidate, Kimson Bryant, MSW Candidate The FATE Program of Give Merit, Inc. is a four-year, cohort-based program that provides resources and opportunities for underserved youth with the goal of motivating each student to graduate high school and attend college. FATE is in the second year of implementation with the first cohort of students from the Jalen Rose Leadership Academy in Detroit, MI. Participants travel to Ann Arbor one Saturday a month for interactive workshops facilitated by community partners related to one of the four FATE guiding principles: academic enrichment, social and cultural awareness, career development, and student mentorship. FATE participants are partnered with a student mentor from the University of Michigan. Participants who complete all four years of the FATE program and graduate high school will receive a $5,000 scholarship to the college of their choice. The University of Michigan School of Social Work Curtis Center Program Evaluation Group (CC-PEG) has partnered with the FATE program for year two of the ongoing evaluation for program improvement and sustainability. The mixed methods design utilizes surveys, observations, focus groups, and key informant interviews with program participants, staff, mentors, and stakeholders. CC-PEG is working with FATE Program stakeholders to document, track, and analyze program implementation and outcomes. 23. A Community in Crisis: Trauma and Dissociation in Detroit Ellen Barrett-Becker, Amanda Burnside, Karen Calhoun, Julie B. Kaplow The city of Detroit has long been identified as a dangerous city to call home. Exposure to community violence and bereavement, particularly deaths involving traumatic circumstances, are common experiences for residents. Despite the media attention Detroit has received, little is known about the rates of trauma exposure or traumaspecific reactions of Detroit’s youngest residents, such as PTSD and dissociation. Research examining the impact of such adversity suggests that dissociation is both common in chronically traumatized youth and detrimental to mental health. The current study evaluated rates of exposure to traumatic events, trauma symptoms, and dissociative symptoms in a sample of eighty-four adolescents, ranging in age from 1018. Results suggest that participants in this sample have experienced a high level of trauma and evidenced elevated levels of posttraumatic symptoms. More than 35% of the sample reported dissociating at least some of the time in the last month. According to the new DSM-V criteria, 23.5% of the sample met criteria for the dissociative subtype of PTSD. Specific types of traumatic experiences were also associated with dissociation. Implications for assessment, diagnosis, and intervention are discussed.