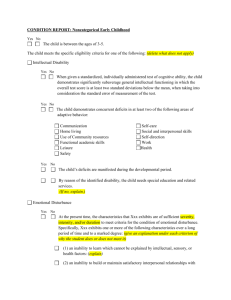
File - the Community-Based Service
advertisement

Asperger Syndrome What is Asperger syndrome? Asperger syndrome (AS) is a developmental disorder that is characterized by: 1 limited interests or an unusual preoccupation with a particular subject to the exclusion of other activities repetitive routines or rituals peculiarities in speech and language, such as speaking in an overly formal manner or in a monotone, or taking figures of speech literally socially and emotionally inappropriate behavior and the inability to interact successfully with peers problems with non-verbal communication, including the restricted use of gestures, limited or inappropriate facial expressions, or a peculiar, stiff gaze clumsy and uncoordinated motor movements AS is an autism spectrum disorder (ASD), one of a distinct group of neurological conditions characterized by a greater or lesser degree of impairment in language and communication skills, as well as repetitive or restrictive patterns of thought and behavior. Other ASDs include: classic autism, Rett syndrome, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (usually referred to as PDD-NOS). Parents usually sense there is something unusual about a child with AS by the time of his or her third birthday, and some children may exhibit symptoms as early as infancy. Unlike children with autism, children with AS retain their early language skills. Motor development delays – crawling or walking late, clumsiness – are sometimes the first indicator of the disorder. The incidence of AS is not well established, but experts in population studies conservatively estimate that two out of every 10,000 children have the disorder. Boys are three to four times more likely than girls to have AS. Studies of children with AS suggest that their problems with socialization and communication continue into adulthood. Some of these children develop additional psychiatric symptoms and disorders in adolescence and adulthood. Although diagnosed mainly in children, AS is being increasingly diagnosed in adults who seek medical help for mental health conditions such as depression, obsessive-compulsive disorder (OCD), and attention deficit hyperactivity disorder (ADHD). No studies have yet been conducted to determine the incidence of AS in adult populations. 1 Characteristics What distinguishes Asperger's Disorder from Autism Disorder is the severity of the symptoms and the absence of language delays. Children with Asperger's Disorder may be only mildly affected and frequently have good language and cognitive skills. To the untrained observer, a child with Asperger's Disorder may just seem like a normal child behaving differently. Children with autism are frequently seen as aloof and uninterested in others. This is not the case with Asperger's Disorder. Individuals with Asperger's Disorder usually want to fit in and have interaction with others; they simply don't know how to do it. They may be socially awkward, not understanding of conventional social rules, or show a lack of empathy. They may have limited eye contact, seem to be unengaged in a conversation, and not understand the use of gestures. Interests in a particular subject may border on the obsessive. Children with Asperger's Disorder frequently like to collect categories of things, such as rocks or bottle caps. They may be proficient in knowing categories of information, such as baseball statistics or Latin names of flowers. While they may have good rote memory skills, they have difficulty with abstract concepts. One of the major differences between Asperger's Disorder and autism is that, by definition, there is no speech delay in Asperger's. In fact, children with Asperger's Disorder frequently have good language skills; they simply use language in different ways. Speech patterns may be unusual, lack inflection or have a rhythmic nature, or it may be formal, but too loud or high pitched. Children with Asperger's Disorder may not understand the subtleties of language, such as irony and humor, or they may not understand the give-and- take nature of a conversation. Another distinction between Asperger's Disorder and autism concerns cognitive ability. While some individuals with autism experience mental retardation, by definition a person with Asperger's Disorder cannot possess a "clinically significant" cognitive delay and most possess average to above average intelligence. While motor difficulties are not a specific criteria for Asperger's, children with Asperger's Disorder frequently have motor skill delays and may appear clumsy or awkward. What causes AS? Current research points to brain abnormalities as the cause of AS. Using advanced brain imaging techniques, scientists have revealed structural and functional differences in specific regions of the brains of normal versus AS children. These defects are most likely caused by the abnormal migration of embryonic cells during fetal development that affects brain structure and “wiring” and then goes on to affect the neural circuits that control thought and behavior. 2 For example, one study found a reduction of brain activity in the frontal lobe of AS children when they were asked to respond to tasks that required them to use their judgment. Another study found differences in activity when children were asked to respond to facial expressions. A different study investigating brain function in adults with AS revealed abnormal levels of specific proteins that correlate with obsessive and repetitive behaviors. Scientists have always known that there had to be a genetic component to AS and the other ASDs because of their tendency to run in families. Additional evidence for the link between inherited genetic mutations and AS was observed in the higher incidence of family members who have behavioral symptoms similar to AS but in a more limited form. For example, they had slight difficulties with social interaction, language, or reading. A specific gene for AS, however, has never been identified. Instead, the most recent research indicates that there are most likely a common group of genes whose variations or deletions make an individual vulnerable to developing AS. This combination of genetic variations or deletions will determine the severity and symptoms for each individual with AS. Diagnosis Diagnosis of Asperger's Disorder is on the increase, although it is unclear whether it is more prevalent or whether more professionals are detecting it. The symptoms for Asperger's Disorder are the same as those listed for autism in the DSM-IV; however, children with AS do not have delays in the area of communication and language. In fact, to be diagnosed with Asperger’s, a child must have normal language development as well as normal intelligence. The DSM-IV criteria for AS specifies that the individual must have "severe and sustained impairment in social interaction, and the development of restricted, repetitive patterns of behavior, interests and activities that must cause clinically significant impairment in social, occupational or other important areas of functioning." The first step to diagnosis is an assessment, including a developmental history and observation. This should be done by medical professionals experienced with autism and other PDDs. If Asperger's Disorder or high-functioning autism is suspected, the diagnosis of autism will generally be ruled out first. Early diagnosis is also important as children with Asperger's Disorder who are diagnosed and treated early in life have an increased chance of being successful in school and eventually living independently. Are there treatments available? The ideal treatment for AS coordinates therapies that address the three core symptoms of the disorder: poor communication skills, obsessive or repetitive routines, and physical clumsiness. There is no single best treatment package for all children with AS, but most professionals agree that the earlier the intervention, the better. 3 An effective treatment program builds on the child’s interests, offers a predictable schedule, teaches tasks as a series of simple steps, actively engages the child’s attention in highly structured activities, and provides regular reinforcement of behavior. This kind of program generally includes: social skills training, a form of group therapy that teaches children with AS the skills they need to interact more successfully with other children cognitive behavioral therapy, a type of “talk” therapy that can help the more explosive or anxious children to manage their emotions better and cut back on obsessive interests and repetitive routines medication, for co-existing conditions such as depression and anxiety occupational or physical therapy, for children with sensory integration problems or poor motor coordination specialized speech/language therapy, to help children who have trouble with the pragmatics of speech – the give and take of normal conversation parent training and support, to teach parents behavioral techniques to use at home 4 Resources Asperger sydrome fact sheet. (2009, October 19). National institute of neurological disorders and stroke. Retrieved from http://www.ninds.nih.gov/disorders/asperger/detail_asperger.htm What's unique about asperger's disorder?. (n.d.). Autism society. Retrieved from http://www.autism-society.org/site/PageServer?pagename=life_aspergers 5 Attention-Deficit/Hyperactivity Disorder (AD/HD) Mario's Story Mario is 10 years old. When he was 7, his family learned he had AD/HD. At the time, he was driving everyone crazy. At school, he couldn’t stay in his seat or keep quiet. At home, he didn’t finish his homework or his chores. He did scary things, too, like climb out of his window onto the roof and run across the street without looking. Things are much better now. Mario was tested by a trained professional to find out what he does well and what gives him trouble. His parents and teachers came up with ways to help him at school. Mario has trouble sitting still, so now he does some of his work standing up. He’s also the student who tidies up the room and washes the chalkboard. His teachers break down his lessons into several parts. Then they have him do each part one at a time. This helps Mario keep his attention on his work. At home, things have changed, too. Now his parents know why he’s so active. They are careful to praise him when he does something well. They even have a reward program to encourage good behavior. He earns “good job points” that they post on a wall chart. After earning 10 points he gets to choose something fun he’d like to do. Having a child with AD/HD is still a challenge, but things are looking better. What is AD/HD? Attention-Deficit/Hyperactivity Disorder (AD/HD) is a condition that can make it hard for a person to sit still, control behavior, and pay attention. These difficulties usually begin before the person is 7 years old. However, these behaviors may not be noticed until the child is older. Doctors do not know just what causes AD/HD. However, researchers who study the brain are coming closer to understanding what may cause AD/HD. They believe that some people with AD/HD do not have enough of certain chemicals (called neurotransmitters) in their brain. These chemicals help the brain control behavior. Parents and teachers do not cause AD/HD. Still, there are many things that both parents and teachers can do to help a child with AD/HD. 6 How Common is AD/HD? As many as 5 out of every 100 children in school may have AD/HD. Boys are three times more likely than girls to have AD/HD. What Are the Signs of AD/HD? There are three main signs, or symptoms, of AD/HD. These are: problems with paying attention, being very active (called hyperactivity), and acting before thinking (called impulsivity). More information about these symptoms is listed in a book called the Diagnostic and Statistical Manual of Mental Disorders (DSM), which is published by the American Psychiatric Association (2000). Based on these symptoms, three types of AD/HD have been found: inattentive type, where the person can’t seem to get focused or stay focused on a task or activity; hyperactive-impulsive type, where the person is very active and often acts without thinking; and combined type, where the person is inattentive, impulsive, and too active. Inattentive type. Many children with AD/HD have problems paying attention. Children with the inattentive type of AD/HD often: do not pay close attention to details; can’t stay focused on play or school work; don’t follow through on instructions or finish school work or chores; can’t seem to organize tasks and activities; get distracted easily; and lose things such as toys, school work, and books. (APA, 2000, pp. 85-86) Hyperactive-impulsive type. Being too active is probably the most visible sign of AD/HD. The hyperactive child is “always on the go.” (As he or she gets older, the level of activity may go down.) These children also act before thinking (called impulsivity). For example, they may run across the road without looking or climb to the top of very tall trees. They may be surprised to find 7 themselves in a dangerous situation. They may have no idea of how to get out of the situation. Hyperactivity and impulsivity tend to go together. Children with the hyperactive-impulsive type of AD/HD often may: Fidget and squirm; Get out of their chairs when they’re not supposed to; Run around or climb constantly; Have trouble playing quietly; Talk too much; Blurt out answers before questions have been completed; Have trouble waiting their turn; Interrupt others when they’re talking (APA, 2000, p. 86) Combined type. Children with the combined type of AD/HD have symptoms of both of the types described above. They have problems with paying attention, with hyperactivity, and with controlling their impulses. Of course, from time to time, all children are inattentive, impulsive, and too active. With children who have AD/HD, these behaviors are the rule, not the exception. These behaviors can cause a child to have real problems at home, at school, and with friends. As a result, many children with AD/HD will feel anxious, unsure of themselves, and depressed. These feelings are not symptoms of AD/HD. They come from having problems again and again at home and in school. How Do You Know if a Child Has AD/HD? When a child shows signs of AD/HD, he or she needs to be evaluated by a trained professional. This person may work for the school system or may be a professional in private practice. A complete evaluation is the only way to know for sure if the child has AD/HD. It is also important to: Rule out other reasons for the child’s behavior, and Find out if the child has other disabilities along with AD/HD. What About Treatment? There is no quick treatment for AD/HD. However, the symptoms of AD/HD can be managed. It’s important that the child’s family and teachers: 8 Find out more about AD/HD; Learn how to help the child manage his or her behavior; Create an educational program that fits the child’s individual needs; and Provide medication, if parents and the doctor feel this would help the child. What About School? School can be hard for children with AD/HD. Success in school often means being able to pay attention and control behavior and impulse. These are the areas where children with AD/HD have trouble. There are many ways the school can help students with AD/HD. Some students may be eligible to receive special education services under the Individuals with Disabilities Education Act (IDEA). AD/HD is specifically mentioned under IDEA's disability category of “Other Health Impairment” (OHI). We’ve included the IDEA’s definition of OHI below and provide information on OHI in a separate fact sheet. Despite the fact that AD/HD is specifically mentioned in IDEA's definition of OHI, some students with AD/HD may not be found eligible for services under IDEA. The AD/HD must affect educational performance. (To learn more about the eligibility process under IDEA, read Evaluating Children for Disability, looking specifically for the section on determining eligibility and what to do if you don't agree with the determination.) If a student is found not eligible for services under IDEA, he or she may be eligible for services under a different law, Section 504 of the Rehabilitation Act of 1973. Regardless of the eligibility determination (yes or no), the school and the child’s parents need to meet and talk about what special help the student needs. Most students with AD/HD are helped by supports or changes in the classroom (called adaptations). Some common changes that help students with AD/HD are listed under “Tips for Teachers” below. More information about helpful strategies can be found in NICHCY’s briefing paper called Attention-Deficit/Hyperactivity Disorder. The resources listed at the end of this publication will also help families and teachers learn more about ways to help children with AD/HD. Tips for Parents Learn about AD/HD. The more you know, the more you can help yourself and your child. See the list of resources and organizations at the end of this publication. Praise your child when he or she does well. Build your child’s abilities. Talk about and encourage his or her strengths and talents. Be clear, be consistent, be positive. Set clear rules for your child. Tell your child what he or she should do, not just what he shouldn’t do. Be clear about what will happen if 9 your child does not follow the rules. Have a reward program for good behavior. Praise your child when he or she shows the behaviors you like. Learn about strategies for managing your child’s behavior. These include valuable techniques such as: charting, having a reward program, ignoring behaviors, natural consequences, logical consequences, and time-out. Using these strategies will lead to more positive behaviors and cut down on problem behaviors. You can read about these techniques in many books. See “Resources” at the end of this publication. Talk with your doctor about whether medication will help your child. Pay attention to your child’s mental health (and your own!). Be open to counseling. It can help you deal with the challenges of raising a child with AD/HD. It can help your child deal with frustration, feel better about himself or herself, and learn more about social skills. Talk to other parents whose children have AD/HD. Parents can share practical advice and emotional support. Call NICHCY to find out how to find parent groups near you. Meet with the school and develop an educational plan to address your child’s needs. Both you and your child’s teachers should get a written copy of this plan. Keep in touch with your child’s teacher. Tell the teacher how your child is doing at home. Ask how your child is doing in school. Offer support. Tips for Teachers Learn more about AD/HD. The resources and organizations at the end of this publication will help you identify behavior support strategies and effective ways to support the student educationally. We’ve listed some strategies below. Figure out what specific things are hard for the student. For example, one student with AD/HD may have trouble starting a task, while another may have trouble ending one task and starting the next. Each student needs different help. Post rules, schedules, and assignments. Clear rules and routines will help a student with AD/HD. Have set times for specific tasks. Call attention to changes in the schedule. Show the student how to use an assignment book and a daily schedule. Also teach study skills and learning strategies, and reinforce these regularly. Help the student channel his or her physical activity (e.g., let the student do some work standing up or at the board). Provide regularly scheduled breaks. 10 Make sure directions are given step by step, and that the student is following the directions. Give directions both verbally and in writing. Many students with AD/HD also benefit from doing the steps as separate tasks. Let the student do work on a computer. Work together with the student’s parents to create and implement an educational plan tailored to meet the student’s needs. Regularly share information about how the student is doing at home and at school. Have high expectations for the student, but be willing to try new ways of doing things. Be patient. Maximize the student’s chances for success. 11 Resource Attention-deficit/hyperactivity disorder. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/Disabilities/Specific/Pages/ADHD.aspx 12 Autism Ryan’s Story Ryan is a healthy, active two-year-old, but his parents are concerned because he doesn’t seem to be doing the same things that his older sister did at this age. He’s not really talking, yet; although sometimes, he repeats, over and over, words that he hears others say. He doesn’t use words to communicate, though. It seems he just enjoys the sounds of them. Ryan spends a lot of time playing by himself. He has a few favorite toys, mostly cars, or anything with wheels on it! And sometimes, he spins himself around as fast as he does the wheels on his cars. Ryan’s parents are really concerned, as he’s started throwing a tantrum whenever his routine has the smallest change. More and more, his parents feel stressed, not knowing what might trigger Ryan’s next upset. Often, it seems Ryan doesn’t notice or care if his family or anyone else is around. His parents just don’t know how to reach their little boy, who seems so rigid and far too set in his ways for his tender young age. After talking with their family doctor, Ryan’s parents call the Early Intervention office in their community and make an appointment to have Ryan evaluated. When the time comes, Ryan is seen by several professionals who play with him, watch him, and ask his parents a lot of questions. When they’re all done, Ryan is diagnosed with a form of autism. As painful as this is for his parents to learn, the early intervention staff try to encourage them. By getting an early diagnosis and beginning treatment, Ryan has the best chance to grow and develop. Of course, there’s a long road ahead, but his parents take comfort in knowing that they aren’t alone and they’re getting Ryan the help he needs. What is Autism? Autism/Pervasive Developmental Disorder (PDD) is a neurological disorder that affects a child’s ability to communicate, understand language, play, and relate to others. PDD represents a distinct category of developmental disabilities that share many of the same characteristics. The different diagnostic terms that fall within the broad meaning of PDD, include: • Autistic Disorder, • Asperger’s Disorder, • Rett’s Disorder, • Childhood Disintegrative Disorder, and • Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS). 13 While there are subtle differences and degrees of severity among these conditions, treatment and educational needs can be very similar for all of them. In the diagnostic manual used to classify mental disorders, the DSM-IV-TR (American Psychiatric Association, 2000), “Autistic Disorder” is listed under the heading of “Pervasive Developmental Disorders.” A diagnosis of autistic disorder is made when an individual displays 6 or more of 12 symptoms across three major areas: (a) social interaction, (b) communication, and (c) behavior. When children display similar behaviors but do not meet the specific criteria for autistic disorder (or the other disorders listed above), they may receive a diagnosis of Pervasive Developmental Disorder Not Otherwise Specified, or PDDNOS. Autism is one of the disabilities specifically defined in the Individuals with Disabilities Education Act (IDEA), the federal legislation under which infants, toddlers, children, and youth with disabilities receive early intervention, special education and related services. IDEA defines the disorder as “a developmental disability significantly affecting verbal and nonverbal communication and social interaction, generally evident before age 3, that adversely affects a child’s educational performance. Other characteristics often associated with autism are engagement in repetitive activities and stereotyped movements, resistance to environmental change or change in daily routines, and unusual responses to sensory experiences.” How Common is Autism? Information from the National Institute of Mental Health and the Center for Disease Control and Prevention (CDC) indicates that between 2 to 6 per 1,000 children (from 1 in 500 to 1 in 150) have some form of autism/PDD. These disorders are four times more common in boys than in girls, although Rett’s Disorder has only been reported and diagnosed in girls. The causes of autism or PDD are unknown. Currently, researchers are investigating areas such as brain development, structure, genetic factors and biochemical imbalance in the brain as possible causes. These disorders are not caused by psychological factors. What are the Signs of Autism? Some or all of the following characteristics may be observed in mild to severe forms: • Communication problems (e.g., using and understanding language); • Difficulty relating to people, objects, and events; • Unusual play with toys and other objects; • Difficulty with changes in routine or familiar surroundings; and • Repetitive body movements or behavior patterns. Children with autism or PDD vary widely in abilities, intelligence, and behaviors. Some children do not speak; others have language that often includes repeated phrases or 14 conversations. Children with more advanced language skills tend to use a small range of topics and have difficulty with abstract concepts. Repetitive play skills, a limited range of interests, and impaired social skills are generally evident as well. Unusual responses to sensory information—for example, loud noises, lights, certain textures of food or fabrics— are also common. What Research is Being Done? Thanks to federal legislation—the Children’s Health Act of 2000 and the Combating Autism Act of 2006—nearly $1 billion over the next five years (2007-2012) has been authorized to combat autism through research, screening, early detection, and early intervention. The National Institutes of Health and the CDC are the lead entities conducting and coordinating multiple research activities. On the education front, the PDA Center at the University of Washington has several sites around the country that provide training and support to schools and families for students with autism spectrum disorders. Research on instructional interventions for children with a broad range of needs is an ongoing national endeavor. Check NICHCY’s Research Summaries and OSEP’s discretionary projects directories on our web site to learn more. Additional information can also be found by selecting "Organizations" on the top right navigation bar of this page. What About School? Early diagnosis and intervention are very important for children with autism/PDD. Under the Individuals with Disabilities Education Act (IDEA), children with autism/PDD may be eligible for early intervention services (birth to 3) and an educational program appropriate to their individual needs. In addition to academic instruction, special education programs for students with autism/PDD (ages 3 to 22) focus on improving communication, social, academic, behavioral, and daily living skills. Behavior and communication problems that interfere with learning often require the assistance of a professional who is particularly knowledgeable in the autism field to develop and help implement a plan which can be carried out at home and school. The classroom environment should be structured so that the program is consistent and predictable. Students with autism/PDD learn better and are less confused when information is presented visually as well as verbally. Interaction with nondisabled peers is also important, for these students provide models of appropriate language, social, and behavioral skills. Consistency and continuity are very important for children with autism/PDD, and parents should always be involved in the development of their child’s program, so that learning activities, experiences, and approaches will be most effective and can be carried over into the home and community. With educational programs designed to meet a student’s individual needs and specialized adult support services in employment and living arrangements, many children and adults with autism/PDD grow to live, work, and participate fully in their communities. 15 Tips for Parents Learn about autism/PDD. The more you know, the more you can help yourself and your child. Your State’s PTI can be especially helpful. You’ll find resources and organizations at the end of this publication and in NICHCY’s online State Resources Sheet. Be mindful to interact with and teach your child in ways that are most likely to get a positive response. Learn what is likely to trigger melt-downs for your child, so you can try to minimize them. Remember, the earliest years are the toughest, but it does get better! Learn from professionals and other parents how to meet your child’s special needs, but remember your son or daughter is first and foremost a child; life does not need to become a neverending round of therapies. If you weren’t born loving highly structured, consistent schedules and routines, ask for help from other parents and professionals on how to make it second nature for you. Behavior, communication, and social skills can all be areas of concern for a child with autism and experience tells us that maintaining a solid, loving, and structured approach in caring for your child, can help greatly. Learn about assistive technology that can help your child. This may include a simple picture communication board to help your child express needs and desires, or may be as sophisticated as an augmentative communication device. Work with professionals in early intervention or in your school to develop an IFSP or an IEP that reflects your child’s needs and abilities. Be sure to include related services, supplementary aids and services, AT, and a positive behavioral support plan, if needed. Be patient, and stay optimistic. Your child, like every child, has a whole lifetime to learn and grow. Tips for Teachers Learn more about autism/PDD. Check out the research on effective instructional interventions and behavior on NICHCY’s web site. The resources and organizations listed in this publication can also help. Make sure directions are given step-by-step, verbally, visually, and by providing physical supports or prompts, as needed by the student. Students with autism spectrum disorders often have trouble interpreting facial expressions, body language, and tone of voice. Be as concrete and explicit as possible in your instructions and feedback to the student. Find out what the student’s strengths and interests are and emphasize them. Tap into those avenues and create opportunities for success. Give positive feedback and lots of opportunities for practice. 16 Build opportunities for the student to have social/collaborative interactions throughout the regular school day. Provide support, structure, and lots of feedback. If behavior is a significant issue for the student, seek help from expert professional resources (including parents) to understand the meanings of the behaviors and to develop a unified, positive approach to resolving them. Have consistent routines and schedules. When you know a change in routine will occur (e.g., a field trip or assembly) prepare the student by telling him or her what is going to be different and what to expect or do. Reward students for each small success. Work together with the student’s parents and other school personnel to create and implement an educational plan tailored to meet the student’s needs. Regularly share information about how the student is doing at school and at home. 17 Resource Autism. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/Disabilities/Specific/Pages/Autism.aspx 18 Blindness/ Visual Impairment Definition The terms partially sighted, low vision, legally blind, and totally blind are used in the educational context to describe students with visual impairments. They are defined as follows: "Partially sighted" indicates some type of visual problem has resulted in a need for special education; "Low vision" generally refers to a severe visual impairment, not necessarily limited to distance vision. Low vision applies to all individuals with sight who are unable to read the newspaper at a normal viewing distance, even with the aid of eyeglasses or contact lenses. They use a combination of vision and other senses to learn, although they may require adaptations in lighting or the size of print, and, sometimes, braille; "Legally blind" indicates that a person has less than 20/200 vision in the better eye or a very limited field of vision (20 degrees at its widest point); and Totally blind students learn via braille or other non-visual media. Visual impairment is the consequence of a functional loss of vision, rather than the eye disorder itself. Eye disorders which can lead to visual impairments can include retinal degeneration, albinism, cataracts, glaucoma, muscular problems that result in visual disturbances, corneal disorders, diabetic retinopathy, congenital disorders, and infection. Incidence The rate at which visual impairments occur in individuals under the age of 18 is 12.2 per 1,000. Severe visual impairments (legally or totally blind) occur at a rate of .06 per 1,000. Characteristics The effect of visual problems on a child's development depends on the severity, type of loss, age at which the condition appears, and overall functioning level of the child. Many children who have multiple disabilities may also have visual impairments resulting in motor, cognitive, and/or social developmental delays. A young child with visual impairments has little reason to explore interesting objects in the environment and, thus, may miss opportunities to have experiences and to learn. This lack of exploration may continue until learning becomes motivating or until intervention begins. 19 Because the child cannot see parents or peers, he or she may be unable to imitate social behavior or understand nonverbal cues. Visual handicaps can create obstacles to a growing child's independence. Educational Implications Children with visual impairments should be assessed early to benefit from early intervention programs, when applicable. Technology in the form of computers and lowvision optical and video aids enable many partially sighted, low vision and blind children to participate in regular class activities. Large print materials, books on tape, and braille books are available. Students with visual impairments may need additional help with special equipment and modifications in the regular curriculum to emphasize listening skills, communication, orientation and mobility, vocation/career options, and daily living skills. Students with low vision or those who are legally blind may need help in using their residual vision more efficiently and in working with special aids and materials. Students who have visual impairments combined with other types of disabilities have a greater need for an interdisciplinary approach and may require greater emphasis on self care and daily living skills. 20 Resource Blindness/ Visual Impairment. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/Disabilities/Specific/Pages/VisualImpairment.aspx 21 Cerebral Palsy Jennifer's Story Jen was born 11 weeks early and weighed only 2½ pounds. The doctors were surprised to see what a strong, wiggly girl she was. But when Jen was just a few days old, she stopped breathing and was put on a ventilator. After 24 hours she was able to breathe on her own again. The doctors did a lot of tests to find out what had happened, but they couldn't find anything wrong. The rest of Jen's time in the hospital was quiet, and after two months she was able to go home. Everyone thought she would be just fine. At home, Jen's mom noticed that Jen was really sloppy when she drank from her bottle. As the months went by, Jen's mom noticed other things she didn't remember seeing with Jen's older brother. At six months, Jen didn't hold her head up straight. She cried a lot and would go stiff with rage. When Jen went back for her six-month checkup, the doctor was concerned by what he saw and what Jen's mom told him. He suggested that Jen's mom take the little girl to a doctor who could look closely at Jen's development. Jen's mom took her to a developmental specialist who finally put a name to all the little things that hadn't seemed right with Jen--cerebral palsy. What is CP? Cerebral palsy--also known as CP--is a condition caused by injury to the parts of the brain that control our ability to use our muscles and bodies. Cerebral means having to do with the brain. Palsy means weakness or problems with using the muscles. Often the injury happens before birth, sometimes during delivery, or, like Jen, soon after being born. CP can be mild, moderate, or severe. Mild CP may mean a child is clumsy. Moderate CP may mean the child walks with a limp. He or she may need a special leg brace or a cane. More severe CP can affect all parts of a child's physical abilities. A child with moderate or severe CP may have to use a wheelchair and other special equipment. Sometimes children with CP can also have learning problems, problems with hearing or seeing (called sensory problems), or intellectual disability. Usually, the greater the injury to the brain, the more severe the CP. However, CP doesn't get worse over time, and most children with CP have a normal life span. Cerebral Palsy as an "Orthopedic Impairment" The Individuals with Disabilities Education Act (IDEA) guides how early intervention services and special education and related services are provided to children with disabilities. Under IDEA, cerebral palsy is considered an "orthopedic impairment," which is defined as . . . 22 ". . . a severe orthopedic impairment that adversely affects a child's educational performance. The term includes impairments caused by congenital anomaly (e.g. clubfoot, absence of some member, etc.), impairments caused by disease (e.g., poliomyelitis, bone tuberculosis, etc.), and impairments from other causes (e.g., cerebral palsy, amputations, and fractures or burns that cause contractures)." 34 Code of Federal Regulations Section 300.8(c)(8) How Common is CP? About 500,000 people in America have some form of CP. Each year 8,000 infants and nearly 1,500 preschool-age children are diagnosed with CP. What Are the Signs of CP There are three main types of CP: Spastic CP is where there is too much muscle tone or tightness. Movements are stiff, especially in the legs, arms, and/or back. Children with this form of CP move their legs awkwardly, turning in or scissoring their legs as they try to walk. This is the most common form of CP. Athetoid CP (also called dyskinetic CP) can affect movements of the entire body. Typically, this form of CP involves slow, uncontrolled body movements and low muscle tone that makes it hard for the person to sit straight and walk. Mixed CP is a combination of the symptoms listed above. A child with mixed CP has both high and low tone muscle. Some muscles are too tight, and others are too loose, creating a mix of stiffness and involuntary movements. Other terms used to describe the different areas of the body that can be affected by CP include: Diplegia--This means only the legs are affected. Hemiplegia--This means one half of the body (such as the right arm and leg) is affected. Quadriplegia--This means both arms and legs are affected, sometimes including the facial muscles and torso. What About Treatment With early and ongoing treatment the effects of CP can be reduced. Many children learn how to get their bodies to work for them in other ways. For example, one infant whose CP keeps him from crawling may be able to get around by rolling from place to place. 23 Children younger than three years old can benefit greatly from early intervention services. Early intervention is a system of services to support infants and toddlers with disabilities and their families. For older children, special education and related services are available through the public school to help each child achieve and learn. Typically, children with CP may need different kinds of therapy, including: Physical therapy (PT), which helps the child develop stronger muscles such as those in the legs and trunk. Through PT, the child works on skills such as walking, sitting, and keeping his or her balance. Occupational therapy (OT), which helps the child develop fine motor skills such as dressing, feeding, writing, and other daily living tasks. Speech-language pathology (S/L), which helps the child develop his or her communication skills. The child may work in particular on speaking, which may be difficult due to problems with muscle tone of the tongue and throat. The child may also find a variety of special equipment helpful. For example, braces (also called AFOs) may be used to hold the foot in place when the child stands or walks. Custom splints can provide support to help a child use his or her hands. A variety of therapy equipment and adapted toys are available to help children play and have fun while they are working their bodies. Activities such as swimming or horseback riding can help strengthen weaker muscles and relax the tighter ones. New medical treatments are being developed all the time. Sometimes surgery, Botox injections, or other medications can help lessen the effects of CP, but there is no cure for the condition. What About School A child with CP can face many challenges in school and is likely to need individualized help. Fortunately, states are responsible for meeting the educational needs of children with disabilities. For children up to age three, services are provided through an early intervention system. Staff work with the child's family to develop what is known as an Individualized Family Services Plan, or IFSP. The IFSP will describe the child's unique needs as well as the services the child will receive to address those needs. The IFSP will also emphasize the unique needs of the family, so that parents and other family members will know how to help their young child with CP. Early intervention services may be provided on a sliding-fee basis, meaning that the costs to the family will depend upon their income. For school-aged children, including preschoolers, special education and related services will be provided through the school system. School staff will work with the child's parents to develop an Individualized Education Program, or IEP. The IEP is similar to an IFSP in 24 that it describes the child's unique needs and the services that have been designed to meet those needs. Special education and related services, which can include PT, OT, and speechlanguage pathology, are provided at no cost to parents. In addition to therapy services and special equipment, children with CP may need what is known as assistive technology. Examples of assistive technology include: Communication devices, which can range from the simple to the sophisticated. Communication boards, for example, have pictures, symbols, letters, or words attached. The child communicates by pointing to or gazing at the pictures or symbols. Augmentative communication devices are more sophisticated and include voice synthesizers that enable the child to "talk" with others. Computer technology, which can range from electronic toys with special switches to sophisticated computer programs operated by simple switch pads or keyboard adaptations. The ability of the brain to find new ways of working after an injury is remarkable. Even so, it can be difficult for parents to imagine what their child's future will be like. Good therapy and handling can help, but the most important "treatment" the child can receive is love and encouragement, with lots of typical childhood experiences, family, and friends. With the right mix of support, equipment, extra time, and accommodations, all children with CP can be successful learners and full participants in life. Tips for Parents Learn about CP. The more you know, the more you can help yourself and your child. See the list of resources and organizations at the end of this publication. Love and play with your child. Treat your son or daughter as you would a child without disabilities. Take your child places, read together, have fun. Learn from professionals and other parents how to meet your child's special needs, but try not to turn your lives into one round of therapy after another. Ask for help from family and friends. Caring for a child with CP is hard work. Teach others what to do and give them plenty of opportunities to practice while you take a break. Keep informed about new treatments and technologies that may help. New approaches are constantly being worked on and can make a huge difference to the quality of your child's life. However, be careful about unproven new "fads." Learn about assistive technology that can help your child. This may include a simple communication board to help your child express needs and desires, or may be as sophisticated as a computer with special software. Be patient, keep up your hope for improvement. Your child, like every child, has a whole lifetime to learn and grow. 25 Work with professionals in early intervention or in your school to develop an IFSP or an IEP that reflects your child's needs and abilities. Be sure to include related services such as speech-language pathology, physical therapy, and occupational therapy if your child needs these. Don't forget about assistive technology either! Tips for Teachers Learn more about CP. The resources and organizations at the end of this publication will help you. This may seem obvious, but sometimes the "look" of CP can given the mistaken impression that a child who has CP cannot learn as much as others. Focus on the individual child and learn firsthand what needs and capabilities he or she has. Tap into the strategies that teachers of students with learning disabilities use for their students. Become knowledgeable about different learning styles. Then you can use the approach best suited for a particular child, based upon that child's learning abilities as well as physical abilities. Be inventive. Ask yourself (and others), "How can I adapt this lesson for this child to maximize active, hands-on learning?" Learn to love assistive technology. Find experts within and outside your school to help you. Assistive technology can mean the difference between independence for your student or not. Always remember, parents are experts, too. Talk candidly with your student's parents. They can tell you a great deal about their daughter or son's special needs and abilities. Effective teamwork for the child with CP needs to bring together professionals with diverse backgrounds and expertise. The team must combine the knowledge of its members to plan, implement, and coordinate the child's services. 26 Resources Cerebral palsy. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/Disabilities/Specific/Pages/CerebralPalsy.aspx Additional Information Assistive technology for children with special needs. (2009). DREAMMS For Kids. Retrieved from http://www.dreamms.org/ NINDS cerebral palsy information page. (2009). National Institute of Neurological Disorders and Stroke. Retrieved from http://www.ninds.nih.gov/disorders/cerebral_palsy/cerebral_palsy.htm 27 Deafness and Hearing Loss Definition The Individuals with Disabilities Education Act (IDEA), formerly the Education of the Handicapped Act (P.L. 94-142), includes "hearing impairment" and "deafness" as two of the categories under which children with disabilities may be eligible for special education and related services programming. While the term "hearing impairment" is often used generically to describe a wide range of hearing losses, including deafness, the regulations for IDEA define hearing loss and deafness separately. Hearing impairment is defined by IDEA as "an impairment in hearing, whether permanent or fluctuating, that adversely affects a child's educational performance." Deafness is defined as "a hearing impairment that is so severe that the child is impaired in processing linguistic information through hearing, with or without amplification." Thus, deafness may be viewed as a condition that prevents an individual from receiving sound in all or most of its forms. In contrast, a child with a hearing loss can generally respond to auditory stimuli, including speech. Incidence Hearing loss and deafness affect individuals of all ages and may occur at any time from infancy through old age. The U.S. Department of Education (2002) reports that, during the 2000-2001 school year, 70,767 students aged 6 to 21 (or 1.3% of all students with disabilities) received special education services under the category of “hearing impairment.” However, the number of children with hearing loss and deafness is undoubtedly higher, since many of these students may have other disabilities as well and may be served under other categories. Characteristics It is useful to know that sound is measured by its loudness or intensity (measured in units called decibels, dB) and its frequency or pitch (measured in units called hertz, Hz). Impairments in hearing can occur in either or both areas, and may exist in only one ear or in both ears. Hearing loss is generally described as slight, mild, moderate, severe, or profound, depending upon how well a person can hear the intensities or frequencies most greatly associated with speech. Generally, only children whose hearing loss is greater than 90 decibels (dB) are considered deaf for the purposes of educational placement. 28 There are four types of hearing loss. Conductive hearing losses are caused by diseases or obstructions in the outer or middle ear (the conduction pathways for sound to reach the inner ear). Conductive hearing losses usually affect all frequencies of hearing evenly and do not result in severe losses. A person with a conductive hearing loss usually is able to use a hearing aid well or can be helped medically or surgically. Sensorineural hearing losses result from damage to the delicate sensory hair cells of the inner ear or the nerves which supply it. These hearing losses can range from mild to profound. They often affect the person's ability to hear certain frequencies more than others. Thus, even with amplification to increase the sound level, a person with a sensorineural hearing loss may perceive distorted sounds, sometimes making the successful use of a hearing aid impossible. A mixed hearing loss refers to a combination of conductive and sensorineural loss and means that a problem occurs in both the outer or middle and the inner ear. A central hearing loss results from damage or impairment to the nerves or nuclei of the central nervous system, either in the pathways to the brain or in the brain itself. Educational Implications Hearing loss or deafness does not affect a person's intellectual capacity or ability to learn. However, children who are either hard of hearing or deaf generally require some form of special education services in order to receive an adequate education. Such services may include: regular speech, language, and auditory training from a specialist; amplification systems; services of an interpreter for those students who use sign language; favorable seating in the class to facilitate lip reading; captioned films/videos; assistance of a notetaker, who takes notes for the student with a hearing loss, so that the student can fully attend to instruction; instruction for the teacher and peers in alternate communication methods, such as sign language; and counseling. Children who are hard of hearing will find it much more difficult than children who have normal hearing to learn vocabulary, grammar, word order, idiomatic expressions, and other aspects of verbal communication. For children who are deaf or have severe hearing losses, early, consistent, and conscious use of visible communication modes (such as sign language, fingerspelling, and Cued Speech) and/or amplification and aural/oral training can help reduce this language delay. By age four or five, most children who are deaf are enrolled in school on a full-day basis and do special work on communication and language development. It is important for teachers and audiologists to work together to teach the child to use his or her residual hearing to the maximum extent possible, even if the 29 preferred means of communication is manual. Since the great majority of deaf children (over 90%) are born to hearing parents, programs should provide instruction for parents on implications of deafness within the family. People with hearing loss use oral or manual means of communication or a combination of the two. Oral communication includes speech, lip reading and the use of residual hearing. Manual communication involves signs and fingerspelling. Total Communication, as a method of instruction, is a combination of the oral method plus signing and fingerspelling. Individuals with hearing loss, including those who are deaf, now have many helpful devices available to them. Text telephones (known as TTs, TTYs, orTDDs) enable persons to type phone messages over the telephone network. The Telecommunications Relay Service (TRS), now required by law, makes it possible for TT users to communicate with virtually anyone (and vice versa) via telephone. Dial 711 to access all TRSs anywhere in the United States. The relay service is free. 30 Resource Deafness and hearing loss. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/disabilities/specific/pages/deafnessandhearingloss.aspx 31 Down Syndrome Definition Down syndrome is the most common and readily identifiable chromosomal condition associated with intellectual disability. It is caused by a chromosomal abnormality: for some unexplained reason, an accident in cell development results in 47 instead of the usual 46 chromosomes. This extra chromosome changes the orderly development of the body and brain. In most cases, the diagnosis of Down syndrome is made according to results from a chromosome test administered shortly after birth. Incidence Approximately 4,000 children with Down syndrome are born in the U.S. each year, or about 1 in every 800 to 1,000 live births. Although parents of any age may have child with Down syndrome, the incidence is higher for women over 35. Most common forms of the syndrome do not usually occur more than once in a family. Characteristics There are over 50 clinical signs of Down syndrome, but it is rare to find all or even most of them in one person. Some common characteristics include: Poor muscle tone; Slanting eyes with folds of skin at the inner corners (called epicanthal folds); Hyperflexibility (excessive ability to extend the joints); Short, broad hands with a single crease across the palm on one or both hands; Broad feet with short toes; Flat bridge of the nose; Short, low-set ears; Short neck; Small head; Small oral cavity; and/or Short, high-pitched cries in infancy. Individuals with Down syndrome are usually smaller than their non-disabled peers, and their physical as well as intellectual development is slower. Besides having a distinct physical appearance, children with Down syndrome frequently have specific health-related problems. A lowered resistance to infection makes these children more prone to respiratory problems. Visual problems such as crossed eyes and far- or nearsightedness are higher in those with Down syndrome, as are mild to moderate 32 hearing loss and speech difficulty. Approximately one third of babies born with Down syndrome have heart defects, most of which are now successfully correctable. Some individuals are born with gastrointestinal tract problems that can be surgically corrected. Some people with Down syndrome also may have a condition known as Atlantoaxial Instability, a misalignment of the top two vertebrae of the neck. This condition makes these individuals more prone to injury if they participate in activities which overextend or flex the neck. Parents are urged to have their child examined by a physician to determine whether or not their child should be restricted from sports and activities which place stress on the neck. Although this misalignment is a potentially serious condition, proper diagnosis can help prevent serious injury. Educational and Employment Implications Shortly after a diagnoses of Down syndrome is confirmed, parents should be encouraged to enroll their child in an infant development/early intervention program. These programs offer parents special instruction in teaching their child language, cognitive, self-help, and social skills, and specific exercises for gross and fine motor development. Research has shown that stimulation during early developmental stages improves the child's chances of developing to his or her fullest potential. Continuing education, positive public attitudes, and a stimulating home environment have also been found to promote the child's overall development. Just as in the typical population, there is a wide variation in mental abilities, behavior, and developmental progress in individuals with Down syndrome. Their level of impairment may range from mild to severe, with the majority functioning in the mild to moderate range. Due to these individual differences, it is impossible to predict future achievements of children with Down syndrome. Because of the range of ability in children with Down syndrome it is important for families and all members of the school's education team to place few limitations on potential capabilities. It may be effective to emphasize concrete concepts rather than abstract ideas. Teaching tasks in a step-by-step manner with frequent reinforcement and consistent feedback has been proven successful. Improved public acceptance of persons with disabilities along with increased opportunities for adults with disabilities to live and work independently in the community, have expanded goals for individuals with Down syndrome. Independent Living Centers, group shared and supervised apartments and support services in the community have proven to be important resources for persons with disabilities. 33 Resource Down syndrome. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/Disabilities/Specific/Pages/DownSyndrome.aspx 34 Duchenne’s Muscular Dystrophy Causes Duchenne muscular dystrophy is a rapidly-worsening form of muscular dystrophy. Other muscular dystrophies (including Becker's muscular dystrophy) get worse much more slowly. Duchenne muscular dystrophy is caused by a defective gene for dystrophin (a protein in the muscles). However, it often occurs in people without a known family history of the condition. Because of the way the disease is inherited, males are more likely to develop symptoms than are women. The sons of females who are carriers of the disease (women with a defective gene but no symptoms themselves) each have a 50% chance of having the disease. The daughters each have a 50% chance of being carriers. Duchenne muscular dystrophy occurs in approximately 1 out of every 3,600 male infants. Because this is an inherited disorder, risks include a family history of Duchenne muscular dystrophy. Symptoms Symptoms usually appear before age 6 and may appear as early as infancy. They may include: Fatigue Mental retardation (possible, but does not worsen over time) Muscle weakness o Begins in the legs and pelvis, but also occurs less severely in the arms, neck, and other areas of the body o Difficulty with motor skills (running, hopping, jumping) o Frequent falls o Rapidly worsening weakness Progressive difficulty walking o Ability to walk may be lost by age 12 By age 10, the person may need braces for walking. By age 12, most patients are confined to a wheelchair. 35 Treatment There is no known cure for Duchenne muscular dystrophy. Treatment aims to control symptoms to maximize quality of life. Gene therapy may become available in the future. Activity is encouraged. Inactivity (such as bedrest) can worsen the muscle disease. Physical therapy may be helpful to maintain muscle strength and function. Orthopedic appliances (such as braces and wheelchairs) may improve mobility and the ability to care for yourself. Prevention Genetic counseling is advised if there is a family history of the disorder. Duchenne muscular dystrophy can be detected with about 95% accuracy by genetic studies performed during pregnancy. Alternative Names Pseudohypertrophic muscular dystrophy; Muscular dystrophy - Duchenne type 36 Resources Duchenne muscular dystrophy. (2009, October 29). Medline plus. Retrieved from http://www.nlm.nih.gov/medlineplus/ency/article/000705.htm Hall, C. D., M.D., Porter, P. B., Ph.D., & Williams, F., M.A. (n.d.). A Teacher's Guide To Duchenne Muscular Dystrophy. In MDA publications. Retrieved from http://www.mda.org/publications/TchrDMD/ dmd2.html 37 Epilepsy Definition According to the Epilepsy Foundation of America, epilepsy is a physical condition that occurs when there is a sudden, brief change in how the brain works. When brain cells are not working properly, a person's consciousness, movement, or actions may be altered for a short time. These physical changes are called epileptic seizures. Epilepsy is therefore sometimes called a seizure disorder. Epilepsy affects people in all nations and of all races. Some people can experience a seizure and not have epilepsy. For example, many young children have convulsions from fevers. These febrile convulsions are one type of seizure. Other types of seizures not classified as epilepsy include those caused by an imbalance of body fluids or chemicals or by alcohol or drug withdrawal. A single seizure does not mean that the person has epilepsy. Incidence About two million Americans have epilepsy; of the 125,000 new cases that develop each year, up to 50% are in children and adolescents. Characteristics Although the symptoms listed below are not necessarily indicators of epilepsy, it is wise to consult a doctor if you or a member of your family experiences one or more of them: "Blackouts" or periods of confused memory; Episodes of staring or unexplained periods of unresponsiveness; Involuntary movement of arms and legs; "Fainting spells" with incontinence or followed by excessive fatigue; or Odd sounds, distorted perceptions, episodic feelings of fear that cannot be explained. Seizures can be generalized, meaning that all brain cells are involved. One type of generalized seizure consists of a convulsion with a complete loss of consciousness. Another type looks like a brief period of fixed staring. Seizures are partial when those brain cells not working properly are limited to one part of the brain. Such partial seizures may cause periods of "automatic behavior" and altered consciousness. This is typified by purposeful- looking behavior, such as buttoning or unbuttoning a shirt. Such behavior, however, is unconscious, may be repetitive, and is usually not recalled. 38 Educational Implications Students with epilepsy or seizure disorders are eligible for special education and related services under the Individuals with Disabilities Education Act (IDEA). Epilepsy is classified as "other health impaired" and an Individualized Education Program (IEP) would be developed to specify appropriate services. Some students may have additional conditions such as learning disabilities along with the seizure disorders. Seizures may interfere with the child's ability to learn. If the student has the type of seizure characterized by a brief period of fixed staring, he or she may be missing parts of what the teacher is saying. It is important that the teacher observe and document these episodes and report them promptly to parents and to school nurses. Depending on the type of seizure or how often they occur, some children may need additional assistance to help them keep up with classmates. Assistance can include adaptations in classroom instruction, first aid instruction on seizure management to the student's teachers, and counseling, all of which should be written in the IEP. It is important that the teachers and school staff are informed about the child's condition, possible effects of medication, and what to do in case a seizure occurs at school. Most parents find that a friendly conversation with the teacher(s) at the beginning of the school year is the best way to handle the situation. Even if a child has seizures that are largely controlled by medication, it is still best to notify the school staff about the condition. School personnel and the family should work together to monitor the effectiveness of medication as well as any side effects. If a child's physical or intellectual skills seem to change, it is important to tell the doctor. There may also be associated hearing or perception problems caused by the brain changes. Written observations of both the family and school staff will be helpful in discussions with the child's doctor. Children and youth with epilepsy must also deal with the psychological and social aspects of the condition. These include public misperceptions and fear of seizures, uncertain occurrence, loss of self control during the seizure episode, and compliance with medications. To help children feel more confident about themselves and accept their epilepsy, the school can assist by providing epilepsy education programs for staff and students, including information on seizure recognition and first aid. Students can benefit the most when both the family and school are working together. There are many materials available for families and teachers so that they can understand how to work most effectively as a team. 39 Resource Epilepsy. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/Disabilities/Specific/Pages/Epilepsy.aspx 40 Fragile X Syndrome (FXS) The most common cause of inherited mental impairment. This impairment can range from learning disabilities to more severe cognitive or intellectual disabilities. (Sometimes referred to as mental retardation.) FXS is the most common known cause of autism or "autistic-like" behaviors. Symptoms also can include characteristic physical and behavioral features and delays in speech and language development. Introduction Once thought of as a typical X-linked recessive condition, Fragile X is now understood as a family of disorders which affects both males and females. It differs from other X-linked conditions in three important ways: Both males and females can have fragile X syndrome (though females are usually more mildly affected) Both males and females can be “carriers” of the Fragile X gene and pass it on to their children Carriers of the Fragile X gene can develop one of the Fragile X- associated disorders; - female carriers can have ovarian insufficiency, infertility and early menopause and male (and less frequently female) carriers can develop an adult onset neurological condition called fragile X- associated tremor/ataxia syndrome (FXTAS). What is the Cause of Fragile X Syndrome? Fragile X syndrome is a genetic condition which is caused by a change in a gene that is inherited at the time of conception. This gene, called the FMR1 gene is found on the X chromosome. When this gene change occurs the FMR1 gene does not work properly. The FMR1 gene is responsible for making a protein that is important in brain development. Therefore when the gene is not working properly brain function including learning, behavior and communication is affected. Physical Features (males and some females, except where noted) Large /protruding ears Recurrent otitis media in childhood Soft skin Flexible joints ( particularly fingers, wrists, elbows) Low muscle tone Flat feet 41 Long face Large testicles (males) Seizure disorder Behavioral, Intellectual, and Social Characteristics (toddlers, school age children and beyond) Speech and language delay Motor delay (late crawling, walking, toileting) Tactile defensiveness and sensory overload (high sensitivity to various fabrics/clothing, loud noises, crowds, food textures & tastes, etc.) Hand-flapping, hand-biting Impulsivity Poor eye contact/gaze aversion Autism spectrum disorders ADHD (attention deficit/hyperactive disorder) Mental retardation, cognitive impairment or intellectual disability Difficulties for Adults (In addition to behavioral, intellectual and social characteristics) Managing transitions to new schools, programs or employment Learning adult living skills such as using transportation and money Managing emotional upsets without aggressive behavior Making and sustaining friendships Issues Common in Females Including some carriers (females are usually less affected than males, but may have some of the features listed at left as well as these) Visual-spatial challenges like reading maps and graphs Executive functioning (the ability to formulate, execute, and carry out a plan) Mathematics Shyness or social anxiety Poor communication skills Difficulty in picking up “social cues” Anxiety, mood swings and depression 42 Important Family History Questions (Positive family history increases possibility of Fragile X) Family history of learning disabilities, mental impairment, including autism and other behavioral disorders Family history of female relatives with infertility, early or premature menopause (symptoms in some females Fragile X carriers) Family history of adults (particularly men) with late (after 50) onset neurological findings including intention tremor, ataxia, memory or cognitive decline, personality or psychiatric changes (symptoms in some older Fragile X carriers) Autism and Fragile X Syndrome Fragile X syndrome can cause a child to have autism or an Autism Spectrum Disorder (ASD) though not all children with fragile X syndrome have autism or an ASD. FACT: For between 2% and 6% of all children diagnosed with autism, the cause is the Fragile X gene mutation. FACT: Approximately one-third of all children diagnosed with fragile X syndrome also have some degree of autism. FACT: Fragile X syndrome is the most common known single gene cause of autism. 43 Resource The national fragile x foundation. (2009, February 10). Retrieved from http://www.fragilex.org/html/home.shtml 44 Global Delays What is Global Developmental Delay A child with developmental delay is a child who is not achieving certain skills as quickly as expected. In other words, the child is not reaching developmental landmarks at the usual age. One subset of children with developmental delay includes those with very early onset of their disorder. These children have delay in walking and other motor skills and their motor difficulties do not get worse over time. This is often referred to as "cerebral palsy." Conditions that are genetic (inherited) are not usually included in this category. Very low birth weight infants account for many, but not all, children who meet the criteria for "cerebral palsy." Causes There are numerous causes of developmental delay. One of the goals of the Pediatric Neurologist is to identify the cause of a child's neurologic or developmental problem. Sometimes this task is easy (for example, if a child had obvious brain injury from a severe brain infection), but more often it is difficult and may require a variety of different tests. The tests we recommend are based on the information we gather from parents and the findings on physical examination. It often takes more than one clinic visit to identify a specific disease, condition or syndrome. Children are constantly changing. As we follow this pattern of change, new diagnoses may be considered. Often, despite the tests and several clinic visits, we are unable to identify a specific diagnosis. There are at least two major reasons for trying to arrive at a specific diagnosis for your child. We need to know what caused the developmental delay to tell parents, siblings and other family members whether another child with developmental delay is likely to be born in this family. Some causes of developmental delay are inherited and others are chance events that are unlikely to recur. Assigning a specific diagnosis allows us to better predict the outcome for a given child and to anticipate any other problems that might arise. Outcome Parents often wonder what developmental delay will mean for the child as he or she gets older. This depends in part on the cause of the developmental delay, but some generalizations are useful. Sometimes, mildly delayed children will catch up during early 45 childhood. Often, however, children who are delayed continue to have problems in adulthood. These problems may affect primarily the motor system and lead to difficulty walking, or even the inability to walk. Sometimes developmental delay affects primarily language or ability to learn. Some children with developmental delay will have other associated problems, such as abnormalities of vision or hearing, behavioral problems, or seizures. In many children all systems are affected. Most children who are delayed have strengths and weaknesses and parents are often the first ones to recognize their child's strengths. The end point of achievements for a child who is developmentally delayed is often different from that of the average child. Exactly what will be achieved in adulthood can vary dramatically within the developmentally delayed population as it does within the "average" population. Management There is almost never a specific medicine or surgical procedure that will correct developmental delay. The most important thing a parent can do for a delayed child is provide a loving and stimulating environment. We often recommend contact with the physical or occupational therapist to assist you in providing appropriate exercises and stimulation for your child. This is usually through the AEA (Area Educational Agency) for families in Iowa. We may also refer your child to other specialists for management of specific problems such as tight muscles or abnormalities of vision. The goal of treatment is to maximize abilities while preventing new problems as much as is possible. 46 Resources Mathews, M.D., K. (2004). Developmental delay. In Trials- Center for Children. Retrieved from http://www.trailscenter.com/gdd.htm Additional Information Dyer, J. (2006). Developmental delay. In JuliaDyer.com. Retrieved from http://www.juliadyer.com/developmentaldelay.htm Tervo, M.D., R. (2003). Identifying patterns of developmental delays can help diagnose neurodevelopmental disorders. In A Pediatric Perspective. Retrieved from http://www.gillettechildrens.org/fileUpload/Vol12No3.pdf Testing for the cause of global developmental delay. (n.d.). AAN Guideline Summary for Parents and Caregivers. Retrieved from http://www.aan.com/globals/axon/assets/2602.pdf 47 Intellectual Disability (formerly Mental Retardation) Matthew's Story Matt is 15 years old. Because Matt has an intellectual disability, he has been receiving special education services since elementary school. These services have helped him tremendously, because they are designed to fit his special learning needs. Last year he started high school. He, his family, and the school took a good hard look at what he wants to do when secondary school is over. Does he want more education? A job? Does he have the skills he needs to live on his own? Answering these questions has helped Matt and the school plan for the future. He's always been interested in the outdoors, in plants, and especially in trees. He knows all the tree names and can recognize them by their leaves and bark. So this year he's learning about jobs like forestry, landscaping, and grounds maintenance. Next year he hopes to get a parttime job. He's learning to use public transportation, so he'll be able to get to and from the job. Having an intellectual disability makes it harder for Matt to learn new things. He needs things to be very concrete. But he's determined. He wants to work outside, maybe in the park service or in a greenhouse, and he's getting ready! What is Intellectual Disability? Intellectual disability is a term used when a person has certain limitations in mental functioning and in skills such as communicating, taking care of him or herself, and social skills. These limitations will cause a child to learn and develop more slowly than a typical child. Children with intellectual disability may take longer to learn to speak, walk, and take care of their personal needs such as dressing or eating. They are likely to have trouble learning in school. They will learn, but it will take them longer. There may be some things they cannot learn. What Causes Intellectual Disability? Doctors have found many causes of intellectual disability. The most common are: Genetic conditions. Sometimes intellectual disability is caused by abnormal genes inherited from parents, errors when genes combine, or other reasons. Examples of genetic conditions are Down syndrome, fragile X syndrome, and phenylketonuria (PKU). 48 Problems during pregnancy. Intellectual disability can result when the baby does not develop inside the mother properly. For example, there may be a problem with the way the baby's cells divide as it grows. A woman who drinks alcohol or gets an infection like rubella during pregnancy may also have a baby with intellectual disability. Problems at birth. If a baby has problems during labor and birth, such as not getting enough oxygen, he or she may have intellectual disability. Health problems. Diseases like whooping cough, the measles, or meningitis can cause an intellectual disability. Intellectual disabilities can also be caused by extreme malnutrition (not eating right), not getting enough medical care, or by being exposed to poisons like lead or mercury. Intellectual disability is not a disease. You can't catch it from anyone. Mental retardation or intellectual disability is also not a type of mental illness, like depression. There is no cure for intellectual disability. However, most children with intellectual disability can learn to do many things. It just takes them more time and effort than other children. How is Intellectual Disability Diagnosed? Intellectual disability is the currently preferred term for the disability historically referred to as mental retardation. Although the preferred name is intellectual disability, the authoritative definition and assumptions put forth by the American Association on Intellectual and Developmental Disabilities (AAIDD) remain the same as those found in the Mental Retardation: Definition, Classification and Systems of Supports manual (Luckasson et al., 2002). The term intellectual disability covers the same population of individuals who were diagnosed previously with mental retardation in number, kind, level, type, and duration of the disability and the need of people with this disability for individualized services and supports. Intellectual disability is diagnosed by looking at two main things. These are: the ability of a person's brain to learn, think, solve problems, and make sense of the world (called IQ or intellectual functioning); and whether the person has the skills he or she needs to live independently (called adaptive behavior, or adaptive functioning). Intellectual functioning, or IQ, is usually measured by a test called an IQ test. The average score is 100. People scoring below 70 to 75 are thought to have an intellectual disability. To measure adaptive behavior, professionals look at what a child can do in comparison to 49 other children of his or her age. Certain skills are important to adaptive behavior. These are: daily living skills, such as getting dressed, going to the bathroom, and feeding one's self; communication skills, such as understanding what is said and being able to answer; social skills with peers, family members, adults, and others. To diagnose an intellectual disability, professionals look at the person's mental abilities (IQ) and his or her adaptive skills. Both of these are highlighted in the definition provided in the Individuals with Disabilities Education Act (IDEA). The IDEA is the federal law that guides how schools provide early intervention and special education and related services to children with disabilities. How Common is Intellectual Disability? As many as 3 out of every 100 people in the country have an intellectual disability (The Arc, 2001). Nearly 614,000 children ages 3 to 21 have some level of intellectual disability and need special education in school (Twenty-sixth Annual Report to Congress, U.S. Department of Education, 2006). In fact, 1 out of every 10 children who need special education has some form of intellectual disability. What Are the Signs of Intellectual Disability? There are many signs of intellectual disability. For example, children with intellectual disability may: sit up, crawl, or walk later than other children; learn to talk later, or have trouble speaking, find it hard to remember things, not understand how to pay for things, have trouble understanding social rules, have trouble seeing the consequences of their actions, have trouble solving problems, and/or have trouble thinking logically. About 87% of people with intellectual disability will only be a little slower than average in learning new information and skills. When they are children, their limitations may not be obvious. They may not even be diagnosed as having intellectual disability until they get to school. As they become adults, many people with intellectual disability can live independently. Other people may not even consider them as having an intellectual disability. 50 The remaining 13% of people with intellectual disability score below 50 on IQ tests. These people will have more difficulty in school, at home, and in the community. A person with more severe intellectual disability will need more intensive support his or her entire life. Every child with intellectual disability is able to learn, develop, and grow. With help, all children with intellectual disability can live a satisfying life. What About School? A child with an intellectual disability can do well in school but is likely to need individualized help. Fortunately, states are responsible for meeting the educational needs of children with disabilities. For children up to age three, services are provided through an early intervention system. Staff work with the child's family to develop what is known as an Individualized Family Services Plan, or IFSP. The IFSP will describe the child's unique needs. It also describes the services the child will receive to address those needs. The IFSP will emphasize the unique needs of the family, so that parents and other family members will know how to help their young child with an intellectual disability. Early intervention services may be provided on a sliding-fee basis, meaning that the costs to the family will depend upon their income. In some states, early intervention services may be at no cost to parents. For eligible school-aged children (including preschoolers), special education and related services are made available through the school system. School staff will work with the child's parents to develop an Individualized Education Program, or IEP. The IEP is similar to an IFSP. It describes the child's unique needs and the services that have been designed to meet those needs. Special education and related services are provided at no cost to parents. Many children with an intellectual disability need help with adaptive skills, which are skills needed to live, work, and play in the community. Teachers and parents can help a child work on these skills at both school and home. Some of these skills include: communicating with others; taking care of personal needs (dressing, bathing, going to the bathroom); health and safety; home living (helping to set the table, cleaning the house, or cooking dinner); social skills (manners, knowing the rules of conversation, getting along in a group, playing a game); reading, writing, and basic math; and as they get older, skills that will help them in the workplace. Supports or changes in the classroom (called adaptations) help most students with an intellectual disability. Some common changes that help students are listed under "Tips for Teachers." The resources below also include ways for parents to help their child with an intellectual disability. 51 Tips for Parents Learn about intellectual disability. The more you know, the more you can help yourself and your child. See the resources and organizations in the boxes at the right. Encourage independence in your child. For example, help your child learn daily care skills, such as dressing, feeding him or herself, using the bathroom, and grooming. Give your child chores. Keep her age, attention span, and abilities in mind. Break down jobs into smaller steps. For example, if your child's job is to set the table, first ask her to get the right number of napkins. Then have her put one at each family member's place at the table. Do the same with the utensils, going one at a time. Tell her what to do, step by step, until the job is done. Demonstrate how to do the job. Help her when she needs assistance. Give your child frequent feedback. Praise your child when he or she does well. Build your child's abilities. Find out what skills your child is learning at school. Find ways for your child to apply those skills at home. For example, if the teacher is going over a lesson about money, take your child to the supermarket with you. Help him count out the money to pay for your groceries. Help him count the change. Find opportunities in your community for social activities, such as scouts, recreation center activities, sports, and so on. These will help your child build social skills as well as to have fun. Talk to other parents whose children have intellectual disability. Parents can share practical advice and emotional support. Call NICHCY (1.800.695.0285) and ask how to find a parent group near you. Meet with the school and develop an educational plan to address your child's needs. Keep in touch with your child's teachers. Offer support. Find out how you can support your child's school learning at home. Tips for Teachers Learn as much as you can about intellectual disability. The organizations and resources listed in the boxes at the right will help you identify specific techniques and strategies to support the student educationally. We've also listed some strategies below. Recognize that you can make an enormous difference in this student's life! Find out what the student's strengths and interests are, and emphasize them. Create opportunities for success. 52 If you are not part of the student's Individualized Education Program (IEP) team, ask for a copy of his or her IEP. The student's educational goals will be listed there, as well as the services and classroom accommodations he or she is to receive. Talk to specialists in your school (e.g., special educators), as necessary. They can help you identify effective methods of teaching this student, ways to adapt the curriculum, and how to address the student's IEP goals in your classroom. Be as concrete as possible. Demonstrate what you mean rather than just giving verbal directions. Rather than just relating new information verbally, show a picture. And rather than just showing a picture, provide the student with hands-on materials and experiences and the opportunity to try things out. Break longer, new tasks into small steps. Demonstrate the steps. Have the student do the steps, one at a time. Provide assistance, as necessary. Give the student immediate feedback. Teach the student academic and life skills such as daily living, social skills, and occupational awareness and exploration, as appropriate. Involve the student in group activities or clubs. Work together with the student's parents and other school personnel to create and implement an educational plan tailored to meet the student's needs. Regularly share information about how the student is doing at school and at home. 53 Resource Intellectual disability. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/disabilities/specific/pages/intellectualdisability.aspx 54 Muscular Dystrophy Introduction The first historical account of muscular dystrophy appeared in 1830, when Sir Charles Bell wrote an essay about an illness that caused progressive weakness in boys. Six years later, another scientist reported on two brothers who developed generalized weakness, muscle damage, and replacement of damaged muscle tissue with fat and connective tissue. At that time the symptoms were thought to be signs of tuberculosis. In the 1850s, descriptions of boys who grew progressively weaker, lost the ability to walk, and died at an early age became more prominent in medical journals. In the following decade, French neurologist Guillaume Duchenne gave a comprehensive account of 13 boys with the most common and severe form of the disease (which now carries his nameDuchenne muscular dystrophy). It soon became evident that the disease had more than one form, and that these diseases affected people of either sex and of all ages. What is muscular dystrophy? Muscular dystrophy (MD) refers to a group of more than 30 genetic diseases that cause progressive weakness and degeneration of skeletal muscles used during voluntary movement. The word dystrophy is derived from the Greek dys, which means "difficult" or "faulty," and troph, or "nourish." These disorders vary in age of onset, severity, and pattern of affected muscles. All forms of MD grow worse as muscles progressively degenerate and weaken. The majority of patients eventually lose the ability to walk. Some types of MD also affect the heart, gastrointestinal system, endocrine glands, spine, eyes, brain, and other organs. Respiratory and cardiac diseases are common, and some patients may develop a swallowing disorder. MD is not contagious and cannot be brought on by injury or activity. What causes MD? All of the muscular dystrophies are inherited and involve a mutation in one of the thousands of genes that program proteins critical to muscle integrity. The body's cells don't work properly when a protein is altered or produced in insufficient quantity (or sometimes missing completely). Many cases of MD occur from spontaneous mutations that are not found in the genes of either parent, and this defect can be passed to the next generation. Genes are like blueprints: they contain coded messages that determine a person's characteristics or traits. They are arranged along 23 rod-like pairs of chromosomes, * with one half of each pair being inherited from each parent. Each half of a chromosome pair is 55 similar to the other, except for one pair, which determines the sex of the individual. Muscular dystrophies can be inherited in three ways: Autosomal dominant inheritance occurs when a child receives a normal gene from one parent and a defective gene from the other parent. Autosomal means the genetic mutation can occur on any of the 22 non-sex chromosomes in each of the body's cells. Dominant means only one parent needs to pass along the abnormal gene in order to produce the disorder. In families where one parent carries a defective gene, each child has a 50 percent chance of inheriting the gene and therefore the disorder. Males and females are equally at risk and the severity of the disorder can differ from person to person. Autosomal recessive inheritance means that both parents must carry and pass on the faulty gene. The parents each have one defective gene but are not affected by the disorder. Children in these families have a 25 percent chance of inheriting both copies of the defective gene and a 50 percent chance of inheriting one gene and therefore becoming a carrier, able to pass along the defect to their children. Children of either sex can be affected by this pattern of inheritance. X-linked (or sex-linked) recessive inheritance occurs when a mother carries the affected gene on one of her two X chromosomes and passes it to her son (males always inherit an X chromosome from their mother and a Y chromosome from their father, while daughters inherit an X chromosome from each parent). Sons of carrier mothers have a 50 percent chance of inheriting the disorder. Daughters also have a 50 percent chance of inheriting the defective gene but usually are not affected, since the healthy X chromosome they receive from their father can offset the faulty one received from their mother. Affected fathers cannot pass an X-linked disorder to their sons but their daughters will be carriers of that disorder. Carrier females occasionally can exhibit milder symptoms of MD. How many people have MD? MD occurs worldwide, affecting all races. Its incidence varies, as some forms are more common than others. Its most common forms in children, Duchenne and Becker muscular dystrophy, alone affect approximately 1 in every 3,500 to 5,000 boys, or between 400 and 600 live male births each year in the United States.** Some types of MD are more prevalent in certain countries and regions of the world. Most muscular dystrophies are familial, meaning there is some family history of the disease. ** Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities, July 27, 2005 How does MD affect muscles? Muscles are made up of thousands of muscle fibers. Each fiber is actually a number of individual cells that have joined together during development and are encased by an outer 56 membrane. Muscle fibers that make up individual muscles are bound together by connective tissue. Muscles are activated when an impulse, or signal, is sent from the brain along the peripheral nerves (nerves that connect the central nervous system to sensory organs and muscles) to the neuromuscular junction (the space between the nerve fiber and the muscle it activates). There, a release of the chemical acetylcholine triggers a series of events that cause the muscle to contract. The muscle fiber membrane contains a group of proteins-called the dystrophin-glycoprotein complex-which prevents damage as muscle fibers contract and relax. When this protective membrane is damaged, muscle fibers begin to leak the protein creatine kinase (needed for the chemical reactions that produce energy for muscle contractions) and take on excess calcium, which causes further harm. Affected muscle fibers eventually die from this damage, leading to progressive muscle degeneration. Although MD can affect several body tissues and organs, it most prominently affects the integrity of muscle fibers. The disease causes muscle degeneration, progressive weakness, fiber death, fiber branching and splitting, phagocytosis (in which muscle fiber material is broken down and destroyed by scavenger cells), and, in some cases, chronic or permanent shortening of tendons and muscles. Also, overall muscle strength and tendon reflexes are usually lessened or lost due to replacement of muscle by connective tissue and fat. Are there other MD-like conditions? There are many other heritable diseases that affect the muscles, the nerves, or the neuromuscular junction. These diseases may produce symptoms that are very similar to those found in some forms of MD (such as inflammatory myopathy, progressive muscle weakness, mental impairment, and cardiomyopathy) but they are caused by different genetic defects. The sharing of symptoms among multiple neuromuscular diseases, and the prevalence of sporadic cases in families not previously affected by MD, often makes it difficult for MD patients to obtain a quick diagnosis. Studies of other related muscle diseases may, however, contribute to what we know about MD. How do the muscular dystrophies differ? There are nine major groups of the muscular dystrophies. The disorders are classified by the extent and distribution of muscle weakness, age of onset, rate of progression, severity of symptoms, and family history (including any pattern of inheritance). Although some forms of MD become apparent in infancy or childhood, others may not appear until middle age or later. Overall, incidence rates and severity vary, but each of the dystrophies causes progressive skeletal muscle deterioration, and some types affect cardiac muscle. 57 There are four forms of MD that begin in childhood: Duchenne MD Becker MD Congenital MD Emery-Dreifuss MD Youth/adolescent-onset muscular dystrophies are classified two ways: Facioscapulohumeral MD Limb-girdle MD There are three forms of MD that usually begin in adulthood. Distal MD Myotonic MD Oculopharyngeal MD How are the muscular dystrophies diagnosed? Both the patient's medical history and a complete family history should be thoroughly reviewed to determine if the muscle disease is secondary to a disease affecting other tissues or organs or is an inherited condition. It is also important to rule out any muscle weakness resulting from prior surgery, exposure to toxins, or current medications that may affect the patient's functional status. Thorough clinical and neurological exams can rule out disorders of the central and/or peripheral nervous systems, identify any patterns of muscle weakness and atrophy, test reflex responses and coordination, and look for contractions. Various laboratory tests may be used to confirm the diagnosis of MD. Blood and urine tests Electron microscopy Exercise tests Genetic testing Genetic counseling Magnetic resonance imaging (MRI) Muscle biopsies Immunofluorescence Neurophysiology studies 58 How are the muscular dystrophies treated? There is no specific treatment that can stop or reverse the progression of any form of MD. All forms of MD are genetic and cannot be prevented. Treatment is aimed at keeping the patient independent for as long as possible and preventing complications that result from weakness, reduced mobility, and cardiac and respiratory difficulties. Treatment may involve a combination of approaches, including physical therapy, drug therapy, and surgery. Assisted ventilation is often needed to treat respiratory muscle weakness that accompanies many forms of MD, especially in the later stages. Oxygen is fed through a flexible mask (or, in some cases, a tube inserted through the esophagus and into the lungs) to help the lungs inflate fully. Since respiratory difficulty may be most extreme at night, some patients may need overnight ventilation. A mask worn over the face is connected by tube to a machine that puts out intermittent bursts of forced oxygen. Obese patients with Duchenne MD may develop obstructive sleep apnea and require nighttime ventilation. Patients on a ventilator may also require the use of a gastric feeding tube. Drug therapy may be prescribed to delay muscle degeneration. Corticosteroids such as prednisone can slow the rate of muscle deterioration in Duchenne MD and help children retain strength and prolong independent walking by as much as several years. However, these medicines have side effects such as weight gain and bone fragility that can be especially troubling in children. Immunosuppressive drugs such as cyclosporin and azathioprine can delay some damage to dying muscle cells. Drugs that may provide shortterm relief from myotonia (muscle spasms and weakness) include mexiletine; phenytoin; baclofen, which blocks signals sent from the spinal cord to contract the muscles; dantrolene, which interferes with the process of muscle contraction; and quinine. (Drugs for myotonia are not effective in myotonic MD but work well for myotonia congenita, a genetic neuromuscular disorder characterized by the slow relaxation of the muscles.) Anticonvulsants, also known as antiepileptics, are used to control seizures and some muscle activity. Commonly prescribed oral anticonvulsants include carbamazepine, phenytoin, clonazepam, gabapentin, topiramate, and felbamate. Respiratory infections may be treated with antibiotics. Physical therapy can help prevent deformities, improve movement, and keep muscles as flexible and strong as possible. Options include passive stretching, postural correction, and exercise. A program is developed to meet the individual patient's needs. Therapy should begin as soon as possible following diagnosis, before there is joint or muscle tightness. Dietary changes have not been shown to slow the progression of MD. Proper nutrition is essential, however, for overall health. Limited mobility or inactivity resulting from muscle weakness can contribute to obesity, dehydration, and constipation. A high-fiber, highprotein, low-calorie diet combined with recommended fluid intake may help. MD patients 59 with swallowing or breathing disorders and those persons who have lost the ability to walk independently should be monitored for signs of malnutrition. Occupational therapy may help some patients deal with progressive weakness and loss of mobility. Some individuals may need to learn new job skills or new ways to perform tasks while other persons may need to change jobs. Assistive technology may include modifications to home and workplace settings and the use of motorized wheelchairs, wheelchair accessories, and adaptive utensils. Corrective surgery is often performed to ease complications from MD. What is the prognosis? The prognosis varies according to the type of MD and the speed of progression. Some types are mild and progress very slowly, allowing normal life expectancy, while others are more severe and result in functional disability and loss of ambulation. Life expectancy may depend on the degree of muscle weakness and any respiratory and/or cardiac complications. What research is being done? The National Institute of Neurological Disorders and Stroke (NINDS) supports a broad program of research on MD. The goals of these studies are to increase understanding of MD and its causes, develop better therapies, and, ultimately, find ways to prevent and cure it. The NINDS and its sister institutes, the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Institute of Child Health and Human Development (NICHD), lead the MD research efforts conducted at the National Institutes of Health (NIH) or at grantee institutions throughout the country. Scientists are also exploring several other drugs that may help delay the loss of muscle mass. 60 Resource Muscular dystrophy: hope through research. (2009, October 19). National institute of neurological disorders and stroke. Retrieved from http://www.ninds.nih.gov/disorders/md/detail_md.htm 61 Rett Syndrome Definition Rett syndrome is a disorder of the nervous system that leads to developmental reversals, especially in the areas of expressive language and hand use. Rett syndrome is a developmental disorder. It is not a degenerative disorder. Causes Rett syndrome occurs almost exclusively in girls and may be misdiagnosed as autism or cerebral palsy. Studies have linked many Rett syndrome cases to a defect in the methl-CpG-binding protein 2 (MeCP2) gene. This gene is on the X chromosome. Females have two X chromosomes, so even when one has this significant defect, the other X chromosome is normal enough for the child to survive. Males born with this defective gene do not have a second X chromosome to make up for the problem. Therefore, the defect usually results in miscarriage, stillbirth, or very early death. The condition affects about 1 out of 10,000 children. Groups of the disease have appeared within families and certain geographic regions, including Norway, Sweden, and northern Italy. Symptoms and Signs Rett syndrome has been most often misdiagnosed as autism, cerebral palsy, or non-specific developmental delay. It strikes all racial and ethnic groups, and occurs worldwide in 1 of every 10,000 to 23,000 female births. An infant with Rett syndrome usually has normal development for the first 6 - 18 months. Symptoms range from mild to severe. Apraxia Breathing problems -- problems tend to get worse with stress; breathing is usually normal during sleep and abnormal while awake Change in development Excessive saliva and drooling Floppy arms and legs -- frequently the first sign 62 Intellectual disabilities and learning difficulties (assessing cognitive skills in those with Rett syndrome, however, is difficult because of the speech and hand motion abnormalities) Scoliosis Shaky, unsteady, or stiff gait; or toe walking Seizures Slowing head growth beginning at approximately 5 - 6 months of age Loss of normal sleep patterns Loss of purposeful hand movements; for example, the grasp used to pick up small objects is replaced by repetitive hand motions like hand wringing or constant placement of hands in mouth Loss of social engagement Ongoing, severe constipation and gastro esophageal reflux (GERD) Poor circulation that can lead to cold and bluish arms and legs Severe language development problems Exams and Tests Genetic testing may be done to look for the gene defect associated with the syndrome. However, since the defect is not identified in everyone with the disease, the diagnosis of Rett syndrome is based on symptoms. Different types of Rett syndrome Atypical Classical (meets the diagnostic criteria) Provisional (some symptoms appear between ages 1 and 3) Rett syndrome is classified as atypical if It begins early (soon after birth) or late (beyond 18 months of age, sometimes as late as 3 or 4 years old) Speech and hand skill problems are mild It is appears in a boy (very rare) Treatment Treatment may include: Assistance with feeding and diapering Methods to treat constipation and GERD Physical therapy to help prevent the hands from contracting Weight bearing exercises for those with scoliosis 63 Supplemental feedings can help those with slowed growth. A feeding tube may be needed if the patient breathes in (aspirates) food. Diets high in calories and fat, as well as nasogastric tube feeds, can help increase weight and height. Weight gain may improve alertness and social interactions. Medications such as carbamazepine may be used to treat seizures. Other medications or supplements that have been used or studied include: Bromocriptine Dextromethorphan Folate and betaine L-carnitine, which may help improve language skills, muscle mass, alertness, energy and quality of life while decreasing constipation and daytime sleepiness L-dopa for motor rigidity in later stages of the disease Stem cell therapy, alone or in combination with gene therapy, is another hopeful treatment. Prognosis The disease slowly progresses until the patient is a teenager. Then, symptoms may improve. For example, seizures or breathing problems tend to lessen in late adolescence. Developmental regression or delays vary. Usually, a child with Rett syndrome sits up properly but may not crawl. For those who do crawl, many do so by scooting on their tummy without using their hands. Similarly, some children walk independently within the normal age range, while others are delayed, don't learn to walk independently at all, or don't learn to walk until late childhood or early adolescence. For those children who do learn to walk at the normal time, some keep that ability for their lifetime, while other children lose the skill. Life expectancies are not well studied, although survival at least until the mid-20s is likely. The average life expectancy of a girl with Rett syndrome may be mid-40s. Death is often related to seizure, aspiration pneumonia, malnutrition, and accidents. 64 Resources Rett sydrome. (2009, October 29). Medline plus. Retrieved from http://www.nlm.nih.gov/medlineplus/ency/article/001536.htm What is rett sydrome? (2008). International rett sydrome foundation. Retrieved from http://www.rettsyndrome.org/index.php?option=com_content&task=view&id=16& Itemid=1000 65 Spina Bifida Definition Spina Bifida means cleft spine, which is an incomplete closure in the spinal column. In general, the three types of spina bifida (from mild to severe) are: 1. Spina Bifida Occulta: There is an opening in one or more of the vertebrae (bones) of the spinal column without apparent damage to the spinal cord. 2. Meningocele: The meninges, or protective covering around the spinal cord, has pushed out through the opening in the vertebrae in a sac called the "meningocele." However, the spinal cord remains intact. This form can be repaired with little or no damage to the nerve pathways. 3. Myelomeningocele: This is the most severe form of spina bifida, in which a portion of the spinal cord itself protrudes through the back. In some cases, sacs are covered with skin; in others, tissue and nerves are exposed. Generally, people use the terms "spina bifida" and "myelomeningocele" interchangeably. Incidence Approximately 40% of all Americans may have spina bifida occulta, but because they experience little or no symptoms, very few of them ever know that they have it. The other two types of spina bifida, meningocele and myelomeningocele, are known collectively as "spina bifida manifesta," and occur in approximately one out of every thousand births. Of these infants born with "spina bifida manifesta," about 4% have the meningocele form, while about 96% have myelomeningocele form. Characteristics The effects of myelomeningocele, the most serious form of spina bifida, may include muscle weakness or paralysis below the area of the spine where the incomplete closure (or cleft) occurs, loss of sensation below the cleft, and loss of bowel and bladder control. In addition, fluid may build up and cause an accumulation of fluid in the brain (a condition known as hydrocephalus). A large percentage (70%-90%) of children born with myelomeningocele have hydrocephalus. Hydrocephalus is controlled by a surgical procedure called "shunting," which relieves the fluid buildup in the brain. If a drain (shunt) is not implanted, the pressure buildup can cause brain damage, seizures or blindness. Hydrocephalus may occur without spina bifida, but the two conditions often occur together. 66 Educational Implications Although spina bifida is relatively common, until recently most children born with a myelomeningocele died shortly after birth. Now that surgery to drain spinal fluid and protect children against hydrocephalus can be performed in the first 48 hours of life, children with myelomeningocele are much more likely to live. Quite often, however, they must have a series of operations throughout their childhood. School programs should be flexible to accommodate these special needs. Many children with myelomeningocele need training to learn to manage their bowel and bladder functions. Some require catheterization, or the insertion of a tube to permit passage of urine. The courts have held that clean, intermittent catheterization is necessary to help the child benefit from and have access to special education and related services. A successful bladder management program can be incorporated into the regular school day. Many children learn to catheterize themselves at a very early age. In some cases, children with spina bifida who also have a history of hydrocephalus experience learning problems. They may have difficulty with paying attention, expressing or understanding language, and grasping reading and math. Early intervention with children who experience learning problems can help considerably to prepare them for school. Successful integration of a child with spina bifida into school sometimes requires changes in school equipment or the curriculum. In adapting the school setting for the child with spina bifida, architectural factors should be considered. Section 504 of the Rehabilitation Act of 1973 requires that programs receiving federal funds make their facilities accessible. This can occur through structural changes (for example, adding elevators or ramps) or through schedule or location changes (for example, offering a course on the ground floor). Children with myelomeningocele need to learn mobility skills, and often require the aid of crutches, braces, or wheelchairs. It is important that all members of the school team and the parents understand the child's physical capabilities and limitations. Physical disabilities like spina bifida can have profound effects on a child's emotional and social development. To promote personal growth, families and teachers should encourage children, within the limits of safety and health, to be independent and to participate in activities with their nondisabled classmates. 67 Resource Spina bifida. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/Disabilities/Specific/Pages/SpinaBifida.aspx 68 Traumatic Brain Injury Susan's Story Susan was 7 years old when she was hit by a car while riding her bike. She broke her arm and leg. She also hit her head very hard. The doctors say she sustained a traumatic brain injury. When she came home from the hospital, she needed lots of help, but now she looks fine. In fact, that’s part of the problem, especially at school. Her friends and teachers think her brain has healed because her broken bones have. But there are changes in Susan that are hard to understand. It takes Susan longer to do things. She has trouble remembering things. She can’t always find the words she wants to use. Reading is hard for her now. It’s going to take time before people really understand the changes they see in her. What is Traumatic Brain Injury? A traumatic brain injury (TBI) is an injury to the brain caused by the head being hit by something or shaken violently. (The exact definition of TBI, according to special education law, is given below.) This injury can change how the person acts, moves, and thinks. A traumatic brain injury can also change how a student learns and acts in school. The term TBI is used for head injuries that can cause changes in one or more areas, such as: thinking and reasoning, understanding words, remembering things, paying attention, solving problems, thinking abstractly, talking, behaving, walking and other physical activities, seeing and/or hearing, and learning. 69 The term TBI is not used for a person who is born with a brain injury. It also is not used for brain injuries that happen during birth. The definition of TBI below comes from the Individuals with Disabilities Education Act (IDEA). The IDEA is the federal law that guides how schools provide special education and related services to children and youth with disabilities. IDEA's Definition of "Traumatic Brain Injury" Our nation’s special education law, the Individuals with Disabilities Education Act (IDEA) defines traumatic brain injury as... “...an acquired injury to the brain caused by an external physical force, resulting in total or partial functional disability or psychosocial impairment, or both, that adversely affects a child’s educational performance. The term applies to open or closed head injuries resulting in impairments in one or more areas, such as cognition; language; memory; attention; reasoning; abstract thinking; judgment; problem-solving; sensory, perceptual, and motor abilities; psycho-social behavior; physical functions; information processing; and speech. The term does not apply to brain injuries that are congenital or degenerative, or to brain injuries induced by birth trauma.” [34 Code of Federal Regulations §300.8(c)(12)] How Common is Traumatic Brain Injury? More than one million children receive brain injuries each year. More than 30,000 of these children have lifelong disabilities as a result of the brain injury. What Are the Signs of Traumatic Brain Injury? The signs of brain injury can be very different depending on where the brain is injured and how severely. Children with TBI may have one or more difficulties, including: Physical disabilities: Individuals with TBI may have problems speaking, seeing, hearing, and using their other senses. They may have headaches and feel tired a lot. They may also have trouble with skills such as writing or drawing. Their muscles may suddenly contract or tighten (this is called spasticity). They may also have seizures. Their balance and walking may also be affected. They may be partly or completely paralyzed on one side of the body, or both sides. Difficulties with thinking: Because the brain has been injured, it is common that the person’s ability to use the brain changes. For example, children with TBI may have trouble with short-term memory (being able to remember something from one minute to the next, like what the teacher just said). They may also have trouble with their longterm memory (being able to remember information from a while ago, like facts learned last month). People with TBI may have trouble concentrating and only be able to focus their attention for a short time. They may think slowly. They may have trouble talking 70 and listening to others. They may also have difficulty with reading and writing, planning, understanding the order in which events happen (called sequencing), and judgment. Social, behavioral, or emotional problems: These difficulties may include sudden changes in mood, anxiety, and depression. Children with TBI may have trouble relating to others. They may be restless and may laugh or cry a lot. They may not have much motivation or much control over their emotions. A child with TBI may not have all of the above difficulties. Brain injuries can range from mild to severe, and so can the changes that result from the injury. This means that it’s hard to predict how an individual will recover from the injury. Early and ongoing help can make a big difference in how the child recovers. This help can include physical or occupational therapy, counseling, and special education. It’s also important to know that, as the child grows and develops, parents and teachers may notice new problems. This is because, as students grow, they are expected to use their brain in new and different ways. The damage to the brain from the earlier injury can make it hard for the student to learn new skills that come with getting older. Sometimes parents and educators may not even realize that the student’s difficulty comes from the earlier injury. What about School? Although TBI is very common, many medical and education professionals may not realize that some difficulties can be caused by a childhood brain injury. Often, students with TBI are thought to have a learning disability, emotional disturbance, or mental retardation. As a result, they don’t receive the type of educational help and support they really need. When children with TBI return to school, their educational and emotional needs are often very different than before the injury. Their disability has happened suddenly and traumatically. They can often remember how they were before the brain injury. This can bring on many emotional and social changes. The child’s family, friends, and teachers also recall what the child was like before the injury. These other people in the child’s life may have trouble changing or adjusting their expectations of the child. Therefore, it is extremely important to plan carefully for the child’s return to school. Parents will want to find out ahead of time about special education services at the school. This information is usually available from the school’s principal or special education teacher. The school will need to evaluate the child thoroughly. This evaluation will let the school and parents know what the student’s educational needs are. The school and parents will then develop an Individualized Education Program (IEP) that addresses those educational needs. 71 It’s important to remember that the IEP is a flexible plan. It can be changed as the parents, the school, and the student learn more about what the student needs at school. Tips for Parents Learn about TBI. The more you know, the more you can help yourself and your child. See the list of resources and organizations at the end of this publication. Work with the medical team to understand your child’s injury and treatment plan. Don’t be shy about asking questions. Tell them what you know or think. Make suggestions. Keep track of your child’s treatment. A 3-ring binder or a box can help you store this history. As your child recovers, you may meet with many doctors, nurses, and others. Write down what they say. Put any paperwork they give you in the notebook or throw it in the box. You can’t remember all this! Also, if you need to share any of this paperwork with someone else, make a copy. Don’t give away your original! Talk to other parents whose children have TBI. There are parent groups all over the U.S. Parents can share practical advice and emotional support. Call NICHCY (1-800-6950285) or find resources in your state, online at (www.nichcy.org/states.htm) to locate parent groups near you. If your child was in school before the injury, plan for his or her return to school. Get in touch with the school. Ask the principal about special education services. Have the medical team share information with the school. When your child returns to school, ask the school to test your child as soon as possible to identify his or her special education needs. Meet with the school and help develop a plan for your child called an Individualized Education Program (IEP). Keep in touch with your child’s teacher. Tell the teacher about how your child is doing at home. Ask how your child is doing in school. Tips for Teachers Find out as much as you can about the child’s injury and his or her present needs. Find out more about TBI. See the list of resources and organizations at the end of this publication. Give the student more time to finish schoolwork and tests. Give directions one step at a time. For tasks with many steps, it helps to give the student written directions. Show the student how to perform new tasks. Give examples to go with new ideas and concepts. 72 Have consistent routines. This helps the student know what to expect. If the routine is going to change, let the student know ahead of time. Check to make sure that the student has actually learned the new skill. Give the student lots of opportunities to practice the new skill. Show the student how to use an assignment book and a daily schedule. This helps the student get organized. Realize that the student may get tired quickly. Let the student rest as needed. Reduce distractions. Keep in touch with the student’s parents. Share information about how the student is doing at home and at school. Be flexible about expectations. Be patient. Maximize the student’s chances for success. 73 Resources Traumatic brain injury. (n.d.). Nichcy. Retrieved from http://www.nichcy.org/Disabilities/Specific/Pages/TBI.aspx Additional Information Cohen, S. L. (2004). What is traumatic brain injury? In Traumatic Brain Injury.com. Retrieved from http://www.traumaticbraininjury.com/ Overview of traumatic brain injury. (2009). CNS. Retrieved from http://www.neuroskills.com/tbi/injury.shtml YouTube. (2008). Traumatic brain injury [Motion picture]. Retrieved from http://video.google.com/videosearch?hl=en&source=hp&q=Traumatic+Brain+Injur y&um=1&ie=UTF8&ei=m9b4SvCFDcmztgev5IyeCw&sa=X&oi=video_result_group& ct=title&resnum=14&ved=0CEcQqwQwDQ# 74 Williams Syndrome Overview Williams syndrome is a rare genetic disorder that can lead to problems with development. Symptoms Delayed speech that may later turn into strong speaking ability and strong learning by hearing Developmental delay Easily distracted, attention deficit disorder (ADD) Feeding problems including colic, reflux, and vomiting Inward bend of the small finger (clinodactyly) Learning disorders Mild to moderate mental retardation Narrowing of the large artery that leaves the heart (aorta) Personality traits including being very friendly, trusting strangers, fearing loud sounds or physical contact, and being interested in music Short compared to the rest of the person's family Slack joints that may change to stiffness as patient gets older Sunken chest (pectus excavatum) Unusual appearance of the face o Flattened nasal bridge with small upturned nose o Long ridges in the skin that run from the nose to the upper lip (philtrum) o Prominent lips with an open mouth o Skin that covers the inner corner of the eye (epicanthal folds) o Partially missing teeth, defective tooth enamel, or small, widely spaced teeth Treatment There is no cure for Williams syndrome. Avoid taking extra calcium and vitamin D. Treat high levels of blood calcium if present. Blood vessel narrowing can be a significant health problem and is treated based on how severe it is. 75 Physical therapy is helpful to patients with joint stiffness. Developmental and speech therapy can also help these children; for example, verbal strengths can help make up for other weaknesses. Other treatments are based on a patient's symptoms. It can help to have treatment coordinated by a geneticist who is experienced with Williams syndrome. Causes Williams syndrome is a rare condition caused by missing genes. Parents may not have any family history of the condition. However, a person with Williams syndrome has a 50% chance of passing the disorder on to each of his or her children. The cause usually occurs randomly. Williams syndrome occurs in about 1 in 8,000 births. One of the 25 missing genes is the gene that produces elastin, a protein that allows blood vessels and other tissues in the body to stretch. It is likely that having only one copy of this gene results in the narrowing of blood vessels seen in this condition. Tests & diagnosis Signs include: Blood vessel narrowing including supravalvular aortic stenosis, pulmonary stenosis, and pulmonary artery stenosis Farsightedness High blood calcium level (hypercalcemia) that may cause seizures and rigid muscles High blood pressure Unusual pattern ("stellate" or star-like) in iris of the eye Tests for Williams syndrome: Blood pressure check Blood test for missing chromosome (FISH test) Echocardiography combined with Doppler ultrasound Kidney ultrasound 76 Prognosis About 75% of those with Williams syndrome have some mental retardation. Most patients will not live as long as normal, due to complications. Most patients require full-time caregivers and often live in supervised group homes. Prevention There is no known way to prevent the genetic problem that causes Williams syndrome. Prenatal testing is available for couples with a family history of Williams syndrome who wish to conceive. Complications Calcium deposits in the kidney and other kidney problems Death (in rare cases from anesthesia) Heart failure due to narrowed blood vessels Pain in the abdomen When to contact a doctor Many of the symptoms and signs of Williams syndrome may not be obvious at birth. Call your health care provider if your child has features similar to those of Williams syndrome. Seek genetic counseling if you have a family history of Williams syndrome. 77 Resources Williams syndrome. (2009). Google. Health. Retrieved from https://health.google.com/health/ref/Williams+syndrome Additional Information NINDS williams syndrome information page. (2008, September 9). National Institute of Neurological Disorders and Stroke. Retrieved from http://www.ninds.nih.gov/disorders/williams/williams.htm Williams syndrome. (2009). Learn.Genetics. Retrieved from http://learn.genetics.utah.edu/content/disorders/whataregd/williams/ Books Bartke, S., & Siegmüller, J. (2004). Williams syndrome across languages. Retrieved from http://books.google.com/books?id=gzhvSJZLVIwC&pg=PA1&dq=williams+syndro me#v=onepage&q=&f=false Semel, E. M., & Rosner, S. R. (2003). Understanding Williams syndrome: behavioral patterns and interventions. Retrieved from http://books.google.com/books?id=rJm-3DgHvQC&printsec=frontcover&dq=williams+syndrome#v=onepage&q=&f=false 78 Compiled by: Mary Dougherty, Jamie Glath, Megan Mead, Chelsea Pierleoni for CP Rochester as a requirement of a service learning project for St. John Fisher College for the course Diversity in American Society 79