Food Safety Concerns with Pork Offal Kristin Adams, Annette M. O
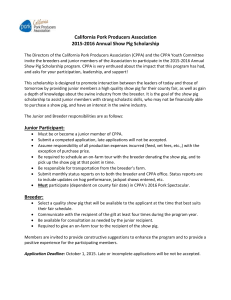
advertisement

Food Safety Concerns with Pork Offal Kristin Adams, Annette M. O’Connor and James S Dickson Keywords: pork, offal, variety meats, pathogens, viruses Abstract: I. Introduction a. Offal – definition (hearts, lungs, livers, kidneys, organ meats) Definition. Offal can have a wide definition, be inedible or edible, and they can also be called “variety meats” or “brocks.” Edible offal is generally divided into three groups of 1) muscle tissues, 2) visceral organs, and 3) portions of the gastrointestinal tract (17). Muscle tissues consists of head meat, weasand (esophagus), and tongues while portions of the gastrointestinal tract include intestines and stomachs. For this review, the main focus will be on the visceral organs, such as heart, liver, kidney, and lung and will also focus upon pork (swine) offal. Therefore, offal will be defined as organ meats, such as heart, kidney, lung, and liver for this review. b. Offal – estimated volume In 1982, it was estimated that 190,000 tons of variety meats or offal were exported to Europe at a value of $110 million (33). In 2013, the United States exported 470,789 metric tons of pork variety meats with a value of $912,718,000 (53). The exportation of pork variety meats has increased because from January to September 2014, the United States exported 384,132 metric tons of pork variety meats with a value of $754,668,000 (54). In month of September alone, the United States exported 44,376 metric tons of pork variety meats with a value of $85,602,000 (54). The top export markets for pork variety meats are Hong Kong/China, Japan, Mexico, Canada, Republic of Korea, and Central and South America (54). c. Uses – human consumption, rendering, general uses Offal can have many uses, which makes it a good revenue generator because of its ability to be used for many different products. For example, offal can be used for human consumption, pharmaceuticals, glues, fertilizers, and much more (46). Edible offals are used for human consumption, and this group can include heart, kidney, and liver. Heart can be used in the manufacture of sausage and luncheon meats, kidneys in soups and stews, and liver can be used to make liver sausage (46). Lungs, which are generally not considered edible offal, can be used to manufacture heparin, a pharmaceutical, or be used in pet foods (46). Any other offal that is deemed unfit for human consumption or rejected by mandatory inspection can be sent to rendering or destroyed. In rendering, the offal is manufactured into fat and other inedible byproducts. Despite offal being a profitable source of revenue for meat producers, the offal produced is considered low commercial value in the United States where edible offal consumption is low. This results in edible offal having a low priority in the US abattoirs (46), so they can be mishandled and are frozen before sale or distribution. Edible offal can be mishandled because some abattoirs collect warm offal in bulk containers and keep those containers at warm temperatures for lengthy periods before packaging (17). In that time frame before packaging, bacterial contamination can increase, and pathogens can become more numerous. In addition, even after packaging, edible offals can be poorly chilled, especially in bulk containers. This results in warmer temperatures for long periods inside the packages, which allows for bacterial growth, especially pathogens. These possibilities of mishandling and poor chilling presents a food safety concern for pork offal because of the chance for pathogen growth, either bacterial or viral. This review will present the prevalence rates of bacterial pathogens, viruses, and parasites in pork offal, highlighting the food safety concerns of mishandled or poorly chilled edible pork offal. II. Description of Search procedure The literature search was done in Web of Knowledge, which includes databases of Web of Science, BIOSIS Citation Index, BIOSIS Previews, CAB Abstracts, Current Contents Connect, Data Citation Index, Derwent Innovations Index, MEDLINE, Zoological Record, and Journal Citation Reports. Timespan covered all years of the databases. The search string was designed initially using the search terms that related to the “population” and “outcome”, as shown in Search Term 1 (Appendix). This was search was too large with 57,935 literatures (49,179 English). After further refinement, the final search used population terms and general outcome terms, but excluded irrelevant research areas such as organ transplantation, fish, poultry, law, history, and sociology and was restricted to English only articles (details described in the appendix). The final web of knowledge search string was Topic = (pork OR pig OR porcine OR swine OR hog) AND (liver OR lung OR heart OR kidney OR “organ meat” OR “variety meat” OR “offal” OR “edible product”) AND Topic = (“shelf life” OR “storage life” OR spoilage OR “off condition” OR “temperature function integration” OR contamination). The citations obtained by the search results were uploaded to the web version of reference management software Endnote and duplicates removed. Each abstract was then screened for relevance to the review using the following set of questions: 1) Does the study describe pig heart, lung, liver, or kidney? If yes, include. 2) Does the study describe shelf life? If yes, include. 3) Does the study describe microbial prevalence and concentration in pig offal? If yes, include. 4) Does the study describe intervention strategies for foodborne pathogens in pig offal? If yes, include. 5) Does the study describe the farm to consumption continuum for pig offal products? If yes, include. The final search identified 1,294 citations written in English and 11 duplicated literatures were excluded. After screening, 1,131 irrelevant articles were excluded and 152 citations were identified as likely relevant and the full texts obtained. From these full texts obtained, they were further screened to narrow the focus to pork offal only, and only discussing hearts, lungs, kidneys, and livers. In addition, of those 152 selected citations, their references were screened for relevant titles pertaining to the topic of this review. After selecting those secondary relevant articles, they were further screened to see if they included any investigation into pathogens, viruses, or parasites in pork offal. Any articles that discussed only meat samples or organ meats not of the focus of this paper (heart, kidney, lung, and liver) were excluded. This process resulted in a final citation amount of approximately 60 citations. III. Bacterial pathogens a. Salmonella Salmonella are prevalent in edible pork offal and can cause salmonellosis. Salmonellosis is one of the important causes of bacterial enteritis in the Netherlands, causing 450 cases out of 100,000 persons per year (45). In the United States, over 1 million cases per year are associated to salmonellosis and causes about 390 deaths (38). Therefore, Salmonella species are important bacterial pathogens and the prevalence of Salmonella species varies in pork offal. One study conducted in 1963 reported a prevalence rate of 3.9% (n=600) of pork livers with the most common species present being S. typhimurium (36%, n=181), S. Heidelberg (16.5%), S. bredeney (9.4%), S. Worthington (6.1%), and S. Newport (5%) (20). The authors also found many minor species present in the positive Salmonella samples, such as S. meleagridis, S. muenchen, S. anatum, S. Dublin, S. cholera suis var. kunzendorf, S. schwarzengrund, S. give, S. livingstone, S. san diego, S. new Brunswick, S. Manchester, S. infantis, S. bovis morbificans, S. derby (1.1%), S. binza, S. cubana, S. enteritidis, S. java, S. Newington, and S. panama (0.5%) (20). The study in 1963 also investigated transportation distances of pigs to slaughterhouses in the Netherlands and found that short distances (40 km, 1-2 hours of travel) resulted in 9.8% (n=274) of pig livers positive for Salmonella species, while long distance travel (4-6 hours) resulted in a lower contamination rate of 6.1% (n=292) (20). In these transportation experiments, the most common Salmonella species were S. typhimurium (32.5%, n=214), S. bredney (17.7%), S. panama (15.8%), S. livingstone (10.5%), and S. meleagridis (6.1%) (20). Another study in Germany (1984) reported a much higher prevalence rate of Salmonella in edible offal, where 72% (n=50) of fresh pork liver, 29.3% (n=58) of frozen pork liver, 77.8% (n=45) of pork heart, 65.3% (n=49) of pork lung were Salmonella positive (41). In these samples, the major Salmonella species were S. typhimurium, S. duisberg, S. derby, S. panama, and S. infantis (41). On the other hand a more recent study (2000) in Germany reported a much lower prevalence rate of 2.7% of pig liver swabs and the most prevalent species were S. typhimurium, S. derby, and S. panama (2). In Canada in 1985, researchers reported that 5% (n=300) of liver samples were contaminated with Salmonella, particularly S. Brandenburg, and they also mentioned that in 1977 29% of refrigerated livers were Salmonella positive (11). Furthermore, a 1984 Netherlands study reported a contamination rate of 4% for pig livers for Salmonella, and they also mentioned it varied due to season (summer or winter), whether the livers were collected at the abattoir or at the retailer, and how large of a sample was taken (58). Generally, the smaller the sample taken (0.1g or 10g), the less likely the chance of isolating Salmonella species, and summer tended to have higher Salmonella positive rates than winter (58). In addition, the retailer tended to have more Salmonella-positive livers than the abattoir due to more cross-contamination in the retailers (58). However, a 2001 Netherlands study had a higher prevalence rate of Salmonella in pork liver swabs at 9.3% and the serotypes found were S. typhimurium DT 104 (43%), S. panama (27%), S. livingstone (6%), and S. derby (4%) (45). A 2008 study conducted in Germany found that 88% of the animals they tested had more than one organ contaminated with S. typhimurium DT104, with 13% of pork lungs being contaminated, while the livers remained undetected (39). Another study in Japan in 2013 reported that 4.5% of pig livers were positive for Salmonella species, including S. typhimuirum, S. derby, and S. infantis (37). A study in 2011 investigated the prevalence of Salmonella in Sardinian pigs and they reported that 14.1% of pig livers were positive for Salmonella (35). The species present in those samples were S. derby, S. typhimuirum DT193, S. typhimurium DT104b, S. panama, and S. rissen (35). In the United Kingdom in 2008, pork offal had a Salmonella prevalence rate of 23.6% (n=131), and this offal included liver, heart, kidney, and stomach (27). The authors also stated that a majority of the Salmonella came from the pork samples, and the most frequently isolated species were S. typhimurium DT104 or DT104b and S. derby (27). Chilling pork livers to an internal temperature of 4°C has been shown to reduce Salmonella by 0.3 log CFU/g and freezing to an internal temperature of 0°C for 6 months reduced Salmonella by 1.8 log CFU/sample (22). However, the effects of chilling and freezing will not eliminate all the Salmonella present in pork offal, so there is still a risk of salmonellosis if pork offal is ingested raw. The risk of salmonellosis is present because the prevalence of Salmonella in pork offal varies between 2% and 70%, which is a considerable food safety hazard and concern. b. Campylobacter Campylobacter species, such as Campylobacter jejuni and Campylobacter coli, are found on edible pork offal. Campylobacter species, especially C. jejuni, have been reported to cause over 850,000 illnesses, or about 14 cases per 100,000 persons, and 76 deaths per year in the United States (38), so Campylobacter is a food safety concern and it is prevalent in pork offal. In Japan, a study reported that 12.7% of pigs were positive for Campylobacter, with the most common species being C. coli, followed by C. fetus and C. jejuni (37). These species were obtained from the inside and from the surface of the liver (37). In Northern Ireland, researchers found that 16% of the pig livers they sampled were contaminated with more than one Campylobacter species (32). Those researchers also reported in another study that 1.25% to 10% of their pig liver samples were positive for Campylobacter, and 6% of freshly eviscerated pork livers were infected with Campylobacter species (31). Of those liver samples, 66.7% (n=60) were positive for C. coli, 30% (n=60) for C. jejuni, 3.3% (n=60) for C. lari, and 16.7% (n=24) were infected with more than one species (31). Furthermore, another study reported a contamination rate of 5.98% (n=401) of campylobacter in pork livers in Northern Ireland, with the most common species being C. coli (62%), C. jejuni (36%), and C. lari (2%) (30). In the United Kingdom, 18.3% of pork offal (liver, heart, kidney, stomach) were positive for Campylobacter species, such as C. jejuni (65.8% of samples), C. coli (29.3%), C. fetus, C. lari, and C. lanienae (27). Those authors also investigated the serotypes present, and the most frequent serotype of C. jejuni was HS14 (9.6%, n=146) and HS149 for C. coli (23.1%, n=65) (27). In addition, another study in the United Kingdom reported a prevalence rate of 71.7% of pig livers with 34.4% of samples (n=99) positive for C. jejuni, 42.5% for C. coli, and 3% for C. fetus (23). The serotypes present for C. jejuni were untypeable (63.9%), HS35 (22.2%), HS13 and HS50 (5.6%), and HS22 and HS37 (2.8%) (23). Another study reported that 6% of pig offal was contaminated with C. jejuni or C. coli in total, while pig offal was 2.5% (n=41) positive at the abattoir and 11.5% (n=26) positive at retail (7). In Scotland, 79% of pig livers (n=29) were positive for Campylobacter and 3% of those positive samples had greater than 3x103 CFU/sample (43). These authors described the importance of treating raw liver carefully and to reduce cross-contamination with other foodstuffs (43). Another study reported the contamination rate of pigs livers were 28.5% (n=31) and 3.2% for spleen and kidney (n=31), with 14.5% of the samples positive (n=93) for C. coli and 6.5% for C. jejuni (1). They also reported that C. coli had a higher prevalence rate overall (30%) in organ samples than C. jejuni (1). Campylobacter, particularly C. coli, can be reduced by chilling to an internal temperature of 4°C and by freezing, which has an internal temperature of 0°C (22). Chilling reduced C. coli by 0.7-1.8 log CFU/sample, freezing reduced C. coli by 2.5 log CFU/sample and freezing the liver for 6 months reduced it by 4.4 log CFU/sample (22). Another study demonstrated that freezing and storing livers at -20°C caused around 1 log CFU/g reduction in Campylobacter species (34). These studies demonstrate that freezing and chilling of pork livers can reduce the incidence and contamination rate of Campylobacter species. However, chilling and freezing may not eliminate all the Campylobacter species present on pork offal because chilling and freezing cause an initial reduction, but then the population remains stable (34). Therefore, despite the beneficial effects of chilling and freezing, Campylobacter can still be a food safety concern because it has a varied prevalence rate of 1.25% (31) to 71.7% (23) in pig liver to around 18% of pork offal (27) (heart, liver, kidney, stomach) and less than 4 CFU/g is the minimum infective dose of C. jejuni for humans (34). c. Pathogenic E. coli The prevalence of pathogenic Escherichia coli is unknown for pork offal for few studies have investigated its prevalence. There was one study conducted by Zhu, W. G., S. Q. Xue (59) in 2005 that reported that pork lung and liver swabs had an E. coli O157:H7 prevalence rate of 0.52%. However, any other studies that have investigated the prevalence of pathogenic E. coli was conducted in meat samples, not offal, or were for beef, not pork. Therefore, the prevalence rates reported here are for beef offal, not pork offal. For beef liver samples, the incidence rate of pathogenic E. coli can vary from 8-16% (n=25) in Thailand in 1990 (44) to 33% in Japan in 2009 (21). Furthermore, the Japanese government in 2012 banned the serving of raw beef liver in restaurants because of the presence of E. coli O157:H7 (37). Even though there are not many studies reporting the incidence level of pathogenic E. coli in pork offal, it could be present, so it could represent a food safety issue if pork offal is consumed raw since pathogenic E. coli cause around 63,000 illnesses and 20 deaths per year in the United States (38). d. Yersinia Yersinia species, particularly Yersinia enterocolitica, has been associated or isolated from pork offal. Y. enterocolitica is the third most frequently reported human foodborne pathogen to cause gastroenteritis in Europe (13, 55) while in the United States, Y. enterocolitica is responsible for 98,000 illnesses, or 1 case per 100,000 persons, and 29 deaths per year (38). The most common bioserotype to cause yersinosis in Europe is 4/O:3 (15, 55). However, other serovars can be found, such as O:3 and O:9 in Europe, O:3 in Canada, and O:8 and O:5,27 in the United States (40, 51). Y. enterocolitica is isolated from pork offal because pork is a primary reservoir for Y. enterocolitica (40, 55) and if contaminated offal is consumed raw by humans, it can cause yersinosis. Yersiniosis consists of gastroenteritis, abdominal pain without diarrhea, and a fever (47, 55). As for how common Y. enterocolitica contaminates pork offal or is isolated from pork offal varies between each study, but it can have a high prevalence rate. In one study, 80% (n=140) of the porcine liver samples were positive for Y. enterocolitica, and most of the livers were purchased from a retailer (58). On the other hand, another study found that only 4.7% of liver surface swabs (n=1500) were positive for Y. enterocolitica O:3 (55). However, two studies found no Y. enterocolitica on liver, spleen, hearts, or kidneys of pork offal (42, 52). One of those studies points out that the organism may not be evenly distributed on the pork offal, so the true incidence of Y. enterocolitica could be different (42). In southern Germany, one study reported a Y. enterocolitica contamination rate of 70% (n=20) for lungs, 70% for hearts (n=20), 25% for livers (n=20), and 15% for kidneys (n=20) (13), while another study in southern Germany reported an incidence rate of 51% (n=1000) of surface swabs for all of the edible pork offal (lungs, hearts, livers, kidneys, and tongues) (9). In Finland, where the pluck set is removed all at once, along with the tonsils and hung on a hook (14, 15, 55), higher Y. enterocolitica prevalence rates have been reported, possibly due to contamination from the tonsils. They found that 38% of livers (n=13), 86% of kidneys (n=13), and 63% of hearts (n=8) were positive Y. enterocolitica (14). In Latvia, the prevalence rate is 2.9% in pork liver and kidney for Y. enterocolitica 4/O:3 (48). In Canada, 50% of pig hearts, 25% of kidneys, and no livers were positive for Y. enterocolitica O:3 (40). In addition, one study reported the incidence of Yersinia pseudotuberculosis, which was between 0.4% to 4% in the pluck set of pork (esophagus, stomach, lungs, livers, hearts, etc.) (25). The authors also mentioned that the pluck sets could have been contaminated by crosscontamination during removal and processing (25). This is the only study found in our literature search that investigated Y. pseudotuberculosis, so the primary species of concern for pork offal is Y. enterocolitica. Chilling and freezing of pork offal has shown to reduce Y. enterocolitica in livers samples (22). Chilling, where the internal temperature of the liver reached 4°C reduced the CFU/sample by 0.2 logs and freezing (internal temperature of 0°C) reduced the pathogen by 0.9 log CFU/sample, and freezing for 9 months reduced the CFU/sample by 1.8 logs (22). This study shows that chilling and freezing of liver can reduce the amount of Y. enterocolitica present, but they are small or minor decreases. Therefore, Y. enterocolitica can be quite prevalent in the raw offal, even after freezing and chilling, as evidenced by a majority of studies reporting a greater than 25% incidence rate in livers (13, 14, 58), 10% in kidneys (13, 14, 40), 50% for lungs and hearts (13, 14, 40) with some incidences of lower rates (42, 48, 52, 55). These high prevalence rates demonstrate the possibility of humans developing yersinosis if they consume raw pork offal. e. Listeria Another bacterial pathogen reported in offal samples is Listeria monocytogenes. The incidence rate for pork livers varies from 1% (37) to 25.1% (n=171) (29), with the most common serotype being 1/2a. Lower incidence rates have been seen in pork kidney and lung samples, showing no L. monocytogenes present (29). Different prevalence rates are reported for L. monocytogenes when the viscera or pluck set (tongue, esophagus, trachea, lungs, kidneys, heart, diaphragm, and liver) are sampled together, such as 64% in one study (3, 50) while only 5% (n=354) in another study (18). In addition, other Listeria spp. are fairly prevalent in pork kidney and heart at a rate of 12.1% (n=174) and 9.5% (n=210), respectively (29). After these few studies, most of the studies conducted about the prevalence of Listeria spp. or Listeria monocytogenes are for meat samples or meat products. These studies report a wide range of Listeria spp. and L. monocytogenes prevalence in pork offal, so it can be present in pork offal, representing a potential food safety concern. f. Clostridium Clostridium species have been found in pork offal, particularly Clostridium perfringens. One study found that the interior of pork livers had a contamination rate of 21.4% (n=28), while the exterior of the livers was 11.8% (n=76) (5). On the other hand, another study reported that C. perfringens remained undetectable in pork livers, both on the surface and the interior (58). As for pork hearts, there are few studies reporting the prevalence rate, and the one study that sampled hearts did not find any C. perfringens (5). The contamination rate of C. perfringens can vary based upon the study’s isolation and detection method, but the few studies that reported the presence of C. perfringens show that it can present a food safety concern in raw pork offal. IV. Viral human pathogens a. Hepatitis E As for viral human pathogens, or viruses, present in pork offal, the Hepatitis E virus (HEV) is of real concern for it can cause illness in humans. There are also no other viruses reported in the literature search we conducted in relation to edible pork offal. Hepatitis E virus is a single-stranded, positive-sense RNA virus without an envelope (19). It is of the genus Hepevirus and the family Hepeviridae, and there are 4 common genotypes, with genotypes 1 and 2 associated with humans and genotypes 3 and 4 associated with swine and being zoonotic (12, 19). Generally HEV is transmitted via the fecal-oral route, but there have been reports of consuming offal, particularly livers of pork or wild boar, can cause an HEV infection in humans (56). For example, in France, HEV was transmitted to a person through consuming figatelli, which contains liver and is not heated during its manufacture (10, 36). It is also not reheated or cooked by the consumer, so there is a chance of contracting HEV if someone consumes HEVcontaminated pork liver (10). Furthermore, there is another study that reported two older gentlemen contracted HEV after eating raw wild boar liver (28). The above studies mention that a human can contract HEV if they consume contaminated pig liver, and the prevalence of HEV positive pork livers varies. In Japan, one study reported a prevalence rate of 1% (n=390) of HEV positive pork livers, with the most common genotype being 3 and 4 (19, 37) while another reported a rate of 2% (10, 12). In France, where consuming figatelli has caused HEV infection in humans, there was a contamination rate of 1.9-11.9% of raw pork livers purchased from grocery stores (10). In the same study, they also found that 58% (n=12) of the figatelli they sampled were HEV positive with genotype 3 and had 103-106 HEV RNA copies per slice (10). In the United States, where HEV is endemic and has a mortality rate of less than 1%, researchers reported a prevalence rate of 11% (n=127) of liver packages purchased from grocery stores with genotype 3 isolated most frequently (12). They also mentioned that even if livers have HEV present, it does not mean it contains infectious virus (12). However, in 2 out of 3 livers they tested, they contained infectious virus (12), so HEV positive livers can be a food safety issue. In the Netherlands, one study reported a contamination rate of 6.5% (n=62) with an average viral load of 65 PDU/g (8). They also mentioned this rate is of concern in the Netherlands because around 900,000 people annually in the Netherlands use raw pork liver, or prepare it, so at a 6% HEV positive rate, there are 60,000 HEV positive livers prepared annually (8). Furthermore, the consumption of raw or undercooked edible offal is common in the Netherlands, so if 3% of the Netherland population consumes raw or undercooked offal, then around 1,800 HEV positive livers are consumed annually, which can present a significant food safety hazard (8). In Southeast Germany, researchers purchased raw pork liver from butcher shops and grocery stores and found that 4% (n=200) of those sampled livers were HEV positive (56). They also reiterated the fact that these HEV positive livers may not contain infectious virions, but is likely, and again it can be a food safety hazard if those livers are consumed raw, which is common in the German diet (56). Another study in India reported the lowest rate of HEV positive livers at 0.83% (n=240) (24) while a study conducted in Canada reported the highest rate of HEV incidence at 20.9% (n=43) of sampled pig livers with a viral load of 103-107 RNA copies/g (26). However, their sample size was small, so the number be lower on a national basis (26). In the United Kingdom, two studies report different HEV prevalence rates, one reports 1.3% (n=80) (4) while the other reports 3% (n=40) (6). These studies report a wide range of HEV positive livers around the world, between 0.83% and 20.9% (24, 26). Despite this range, it shows that HEV positive livers can transmit HEV to humans if they consume raw offal (10, 28, 36) so HEV in raw offal is a food safety concern. V. Parasites There are quite a few parasites that can cause disease or infection of pork offal, but their prevalence rates are not commonly reported in the literature search we conducted. There was one study conducted in 2013 in Taipei that reported the significance of Toxoplasma gondii (16). It reported that 2% of pig livers had T. gondii DNA, but there was no visible sign of infection, such as cysts (16). Another study in 2002 investigated what caused the condemnation of edible offal in pork in Greece (49). They reported that parasites caused 22% of total organ condemnation, whether pork, sheep, or beef organs, and the most common reason pig livers were rejected were due to “milk spots” caused by Ascaris suum or A. lumbricoides, which are intestinal worms (49). Despite these two studies, not many other studies report the prevalence of parasites in pork offal. In addition, if parasites were present in pork offal organs, they would most likely be rejected by inspectors because of obvious signs of infection, such as lesions, cysts, or plaques (57). Some of the more common parasites that could lead to organ rejection are generally organ specific. For example, in pig hearts, if there is any pericarditis, epicarditis, endocarditis, or infection of the heart, or has sarcocysts caused by Sarcocystis miescheneriana, S. suihominis, or S. porcifelis would lead to automatic rejection of the heart for consumption (57). As for pig kidneys, their rejection is caused when they have infarcts (dead tissue), nephritis (infection), congential cysts, or has Stephanurus dentatus, a tropical worm that infects kidneys (57). Pig liver can be rejected for numerous reasons, such as hepatitis (inflammation or infection), tumors, “milk spots” caused by A. suum and A. lumbricoides intestinal worms, Echinococcus granulosus cysts (tapeworm), Tenuicollis cysts (tapeworm), or any kind of cirrhosis (57). Many times pig lungs can be salvaged if the affected tissue is trimmed away, such as blood splashes, but lung rejection occurs when the lungs have Ascaris larvae, Echinoccocus cysts, or lung worms (Metastrongylus apri) (57). The inspection of the organs and offal that takes place during pig slaughter should reject most of the parasite-infected organs, so their prevalence in raw offal should be low and not much of a food safety concern. VI. Summary Acknowledgements The funding for this review paper was provided by the National Pork Board. Appendix Search Term 1 1) TS= ("organ meat" OR "variety meat" OR offal OR “edible product”) 2) TS= (liver OR lung OR heart OR kidney) 3) #1 OR #2 4) TS= (Pork OR Pig OR porcine OR swine OR hog) 5) #3 AND #4 6) TS= (“shelf life” OR “storage life” OR safety OR quality OR spoilage OR “off condition” OR “temperature function integration”) 7) TS= (contamination OR “pathogenic bacteria” OR pathogen OR “microbial flora” OR microflora OR bacteriological OR microbial OR microbiological OR “microbiological profile” OR coliform OR APC OR “aerobic plate count” OR TCC OR “total coliform count” OR Campylobacter OR Salmonella OR “Escherichia coli” OR E. coli OR Yersinia OR psychrotroph* OR enterobacteriaceae OR Staphylococc* OR mesophillic) 8) TS= (refrigeration OR refrigerated OR freezing OR frozen OR chilled OR chilling OR “cold storage” OR “storage temperature” OR packaging OR “vacuum packaged” OR “vacuum packaging” OR decontamination OR antimicrobial OR preservative OR hygienic) 9) #6 OR #7 OR #8 10) #5 AND #9 Search 2 We then tried to use just the population terms, which was a combination of “pig” and “offal” terms, as shown in Search Term 2. The results ended up with 388,337 literature (358,047 were in English). We restricted the research area into “Food Science Technology” and the literature was reduced to 6,339 (English only). However, too many journals were irrelevant to the topic and it was hard to tell which ones should be excluded or kept. Search Term 2: Topic= (Pork OR Pig OR porcine OR swine OR hog) AND Topic= (liver OR lung OR heart OR kidney OR “organ meat” OR “variety meat” OR offal OR “edible product”). Search 3 We then tried to use combined population and outcome terms in Search Term 3. The outcome terms included general shelf life and contamination terms as well as names of specific pathogenic bacteria: Search Term 3: Topic=(Pork OR Pig OR porcine OR swine OR hog) AND Topic=(liver OR lung OR heart OR kidney OR “organ meat” OR “variety mea” OR offal OR “edible product”) AND Topic=(“shelf life” OR “storage life” OR spoilage OR “off condition” OR “temperature function integration” OR contamination OR “pathogenic bacteria” OR “microbial flora” OR microflora OR “microbiological profile” OR coliform OR “aerobic plate count” OR Campylobacter OR Salmonella OR E. coli OR Yersinia OR Staphylococc* OR psychrotroph*). We ended up with 10,356 literatures (8,722 English). Since a lot of the papers were about E. coli, we excluded E. coli papers and reduced the literatures to 8,561 (7,025 English), which was still too many. Search 4 We finally tried to use the population terms and general outcome terms, as shown in Search Term 4, and obtained 4,355 literatures. We excluded irrelevant research areas such as organ transplantation, fish, poultry, law, history, and sociology and reduced the numbers to 2,302 (1,294 English). Search Term 4: Topic= ((Pork OR Pig OR porcine OR swine OR hog) AND (liver OR lung OR heart OR kidney OR “organ meat” OR “variety meat” OR “offal” OR “edible product”)) AND Topic = (“shelf life” OR “storage life” OR spoilage OR “off condition” OR “temperature function integration” OR contamination) Refined by: [excluding] Research Areas=(Legal medicine OR Health Care Sciences Services OR Materials Science OR Government law OR Dentistry Oral Surgery Medicine OR Medical laboratory technology OR History OR Pharmacology pharmacy OR Obstetrics gynecology OR Education educational research OR Fisheries OR Marine freshwater biology OR Public administration OR Behavioral sciences OR International relations OR Orthopedics OR Dermatology OR Automation control systems OR Mathematics OR Imaging science photographic technology OR Critical care medicine OR Life sciences biomedicine other topics OR Ophthalmology OR Demography Or Psychriatry OR Cardiovascular system cardiology OR General internal medicine OR Sociology OR Pediatrics OR Construction building technology OR Cell biology OR Physics OR Electrochemistry OR Research experimental medicine OR Forestry OR Mathematical computational biology OR Genetics heredity OR Biophysics OR Acoustics OR Plant sciences OR Emergency medicine OR Reproductive biology OR Evolutionary biology OR Nuclear science technology OR Radiology nuclear medicine medical imaging OR Rheumatology OR Anatomy morphology OR Social issues OR Transplantation OR Social sciences other topics OR Developmental biology OR Geriatrics gerontology OR Sport Sciences or Surgery OR Information science library science OR Substance abuse OR Neurosciences neurology OR Meteorology atmospheric sciences OR Oncology OR Psychology OR Biodiversity conservation OR Anthropology OR Anesthesiology) AND Languages = (ENGLISH), Timespan=All years. Search language=Auto. VII. References 1. Alecu, A., and D. Botus. 2008. The contamination of pork meat with Campylobacter germs during the technological flow. Bull. Univ. Agric. Sci. 65:234-237. 2. Altrock, A. V., A. Schutte, and G. Hildebrandt. 2000. Results of the German investigations in the EU project entitled: "Salmonella in pork (Salinpork)". Part 2. Abattoir investigations. Berl. Munch. Tierarztl. 113:225-233. 3. Autio, T., T. Sateri, M. Fredriksson-Ahoma, M. Rahko, J. Lunden, and H. Korkeala. 2000. Listeria monocytogenes contamination pattern in pig slaughterhouses. J. Food Prot. 63:1438-1442. 4. Banks, M., F. Martelli, S. Grierson, H. J. Fellows, W. Stableforth, R. Bendall, and H. R. Dalton. 2010. Hepatitis E virus in retail pig livers. Vet. Rec. 166:29. 5. Bauer, F. T., J. A. Carpenter, and J. O. Reagan. 1981. Prevalence of Clostridium perfringens in pork during processing. J. Food Prot. 44:279-283. 6. Berto, A., F. Martelli, S. Grierson, and M. Banks. 2012. Hepatitis E virus in pork food chain, United Kingdom, 2009-2010. Emerg. Infect. Dis. 18:1358-1360. 7. Bolton, F. J., H. C. Dawkins, and D. N. Hutchinson. 1985. Biotypes and serotypes of thermophilic Campylobacters isolated from cattle, sheep and pig offal and other red meats. J. Hyg.-Cambridge. 95:1-6. 8. Bouwknegt, M., F. Lodder-Verschoor, W. H. M. v. d. Poel, S. A. Rutjes, and A. M. d. R. Husman. 2007. Hepatitis E virus RNA in commerical porcine livers in the Netherlands. J. Food Prot. 70:2889-2895. 9. Bucher, M., C. Meyer, B. Groetzbach, S. Wacheck, A. Stolle, and M. FredrikssonAhomaa. 2008. Epidemiological data on pathogenic Yersinia enterocolitica in Southern Germany during 2000-2006. Foodborne Pathog. Dis. 5:273-280. 10. Colson, P., P. Borentain, B. Queyriaux, M. Kaba, V. Moal, P. Gallian, L. Heyries, D. Raoult, and R. Gerolami. 2010. Pig liver sausage as a source of Hepatitis E virus transmission to humans. J. Infect. Dis. 202:825-834. 11. D'Aoust, J.-Y., U. T. Purvis, R. M. Coulter, and K. Weiss. 1985. Salmonella in fresh pork liver and chicken liver in Canada: a 1979-80 survey. Can. Ins. Food Sci. Technol. J. 18:323-325. 12. Feagins, A. R., T. Opriessnig, D. K. Guenette, P. G. Halbur, and X.-J. Meng. 2007. Detection and characterization of infectious Hepatitis E virus from commerical pigs livers sold in local grocery stores in the USA. J. Gen. Virol. 88:912-917. 13. Fredriksson-Ahomaa, M., M. Bucher, C. Hank, A. Stolle, and H. Korkeala. 2001. High prevalence of Yersinia enterocolitica 4:O3 on pig offal in Southern Germany: a slaughtering technique problem. Syst. Appl. Microbiol. 24:457-463. 14. Fredriksson-Ahomaa, M., T. Korte, and H. Korkeala. 2000. Contamination of carcasses, offals, and the environment with yadA-positive Yersinia enterocolitica in a pig slaughterhouse. J. Food Prot. 63:31-35. 15. Fredriksson-Ahomaa, M., T. Korte, and H. Korkeala. 2001. Transmission of Yersinia enterocolitica 4/O:3 to pets via contaminated pork. Lett. Appl. Microbiol. 32:375-378. 16. Fuh, Y. B., C. S. Lin, T. C. A. Liao, Y. M. Pong, M. C. Tung, C. Y. Fei, and D. S. Lin. 2013. Survey of Toxoplasma gondii in Taipei: livestock meats, internal organs, cat and dog sera. Thai J. Vet. Med. 43:15-21. 17. Gill, C. O. 2005. HACCP in the processing of fresh meat. p. 654-657. In J.N. Sofos (ed.), Improving the safety of fresh meat. Woodhead Publishing Ltd, Boca Raton, FL. 18. Hellstrom, S., R. Laukkanen, K.-M. Siekkinen, J. Ranta, R. Maijala, and H. Korkeala. 2010. Listeria monocytogenes contamination in pork can originate from farms. J. Food Prot. 73:641-648. 19. Ishida, S., S. Yoshizumi, T. Ikeda, M. Miyoshi, A. Goto, K. Matsubayashi, and H. Ikeda. 2012. Detection and molecular characterization of hepatitis E virus in clinical, environmental and putative animal sources. Arch. Virol. 157:2363-2368. 20. Kampelmacher, E. H., P. A. M. Guinee, K. Hofstra, and A. V. Keulen. 1963. Further studies on Salmonella in slaughterhouses and in normal slaughter pigs. Zbl. Vet. Med. B. 10:127. 21. Kanki, M., K. Seto, J. Sakata, T. Harada, and Y. Kumeda. 2009. Simultaneous enrichment of Shiga toxin-producing Escherichia coli O157 and O26 and Salmonella in food samples using universal preenrichment broth. J. Food Prot. 72:2065-2070. 22. King, A. M., R. K. Miller, A. Castillo, D. B. Griffin, and M. D. Hardin. 2012. Effects of lactic acid and commerical chilling processes on survival of Salmonella, Yersinia enterocolitica, and Campylobacter coli in pork variety meats. J. Food Prot. 75:1589-1594. 23. Kramer, J. M., J. A. Frost, F. J. Bolton, and D. R. Wareing. 2000. Campylobacter contamination of raw meat and poultry at retail sale: identification of multiple types and comparison with isolates from human infection. J. Food Prot. 63:1654-1659. 24. Kulkarni, M. A., and V. A. Arankalle. 2008. The detection and characterization of hepatitis E virus in pig livers from retail markets of India. J. Med. Virol. 80:1387-1390. 25. Laukkanen, R., P. O. Martinez, K.-M. Siekkinen, J. Ranta, R. Maijala, and H. Korkeala. 2008. Transmission of Yersinia pseudotuberculosis in the pork production chain from farm to slaughterhouse. Appl. Environ. Microbiol. 74:5444-5450. 26. Leblanc, D., E. Poitras, M.-J. Gagne, P. Ward, and A. Houde. 2010. Hepatitis E virus load in swine organs and tissues at slaughterhouse determined by real-time RT-PCR. Int. J. Food Microbiol. 139:206-209. 27. Little, C. L., J. F. Richardson, R. J. Owen, E. d. Pinna, and E. J. Threlfall. 2008. Campylobacter and Salmonella in raw red meats in the United Kingdom: prevalence, characterization and antimicrobial resistance pattern, 2003-2005. Food Microbiol. 25:538-543. 28. Matsuda, H., K. Okada, K. Takahashi, and S. Mishiro. 2003. Severe Hepatitis E Virus infection after ingestion of uncooked liver from a wild boar. J. Infect. Dis. 188:944. 29. Meyer, C., and A. Stolle. 2009. Incidences of Listeria spp. and Listeria monocytogenes in meat and by-products. Fleischwirtschaft. 89:110-112. 30. Moore, J. E., and R. H. Madden. 1991. Campylobacter spp. from freshly eviscerated porcine liver in N. Ireland. Microb. Ecol. Health Dis. 4:S74. 31. Moore, J. E., and R. H. Madden. 1998. Occurrence of thermophilic Campylobacter spp. in porcine liver in Northern Ireland. J. Food Prot. 61:409-413. 32. Moore, J. E., and R. H. Madden. 2003. Comparison of eight phenotypic methods for subspecies characterization of thermophilic Campylobacter spp. isolated from pig liver. J. Food Prot. 66:1079-1084. 33. Oblinger, J. L., J. E. Kennedy, C. A. Rothenberg, B. W. Berry, and N. J. Stern. 1982. Identification of bacteria isolated from fresh and temperature abused variety meats. J. Food Prot. 45:650-654. 34. Oosterom, J., G. J. A. Dewilde, E. Deboer, L. H. Deblaauw, and H. Karman. 1983. Survival of Camplyobacter jejuni during poultry processing and pig slaughtering. J. Food Prot. 46:702-706. 35. Piras, F., D. J. Brown, D. Meloni, A. Mureddu, and R. Mazzette. 2011. Investigation of Salmonella enterica in Sardinian slaughter pigs: prevalence, serotype and genotype characterization. Int. J. Food Microbiol. 151:201-209. 36. Renou, C., A.-M. R. Afonso, and N. Pavio. 2014. Foodborne transmission of Hepatitis E virus from raw pork liver sausage, France. Emerg. Infect. Dis. 20:1945-1946. 37. Sasaki, Y., M. Haruna, M. Murakami, M. Hayashida, K. Ito, M. Noda, and Y. Yamada. 2013. Prevalence of Campylobacter spp., Salmonella spp., Listeria monocytogenes, and Hepatitis E Virus in swine livers collected at an abattoir. Jpn. J. Infect. Dis. 66:161-164. 38. Scallan, E., R. M. Hoekstra, F. J. Angulo, R. V. Tauxe, M.-A. Widdowson, S. L. Roy, J. L. Jones, and P. M. Griffin. 2011. Foodborne illness acquired in the United States--major pathogens. Emerg. Infect. Dis. 17:7-15. 39. Scherer, K., I. Szabo, U. Rosler, B. Appel, A. Hensel, and K. Nockler. 2008. Time course of infection with Salmonella Typhimurium and its influence of fecal shedding, distribution in inner organs, and antibody response in fattening pigs. J. Food Prot. 71:699-705. 40. Schiemann, D. A. 1980. Isolation of toxigenic Yersinia enterocolitica from retail pork products. J. Food Prot. 43:360-365. 41. Sinell, H. J., H. Klingbeil, and M. Benner. 1984. Microflora of edible offal with particular reference to Salmonella. J. Food Prot. 47:481-484. 42. Stern, N. J. 1981. Isolation of potentially virulent Yersinia enterocolitica from variety meats. J. Food Sci. 46:41-42. 43. Strachan, N. J. C., M. MacRae, A. Thomson, O. Rotariu, I. D. Ogden, and K. J. Forbes. 2012. Source attribution, prevalence and enumeration of Campylobacter spp. from retail liver. Int. J. Food Microbiol. 153:234-236. 44. Suthienkul, O., J. E. Brown, J. Seriwatana, S. Tienthongdee, S. Sastravaha, and P. Echeverria. 1990. Shiga-like-toxin-producing Escherichia coli in retail meats and cattle in Thailand. Appl. Environ. Microbiol. 56:1135-1139. 45. Swanenburg, M., H. A. P. Urlings, J. M. A. Snijders, D. A. Keuzenkamp, and F. v. Knapen. 2001. Salmonella in slaughter pigs: prevalence, serotypes and critical control points during slaughter in two slaughterhouses. Int. J. Food Microbiol. 70:243-254. 46. Swingler, G. R. 1982. Microbiology of meat industry by-products. p. 179-224. In M.H. Brown (ed.), Meat Microbiology. Applied Science, London. 47. Tauxe, R. V., G. Wauters, V. Goossens, R. Vannoyen, J. Vandepitte, S. M. Martin, P. Demol, and G. Thiers. 1987. Yersinia enterocolitica infections and pork: the missing link. Lancet. 1:1129-1132. 48. Terentjeva, M., and A. Berzins. 2013. Prevalence of Yersinia enterocolitica 4/O:3 in raw pork at retail market in Lativa. Arch. Lebensmittelhyg. 64:136-140. 49. Theodoropoulos, G., E. Theodoropoulou, G. Petrakos, V. Kantzoura, and J. Kostopoulos. 2002. Abattoir condemnation due to parasitic infections and its economic implications in the region of Trikala, Greece. J. Vet. Med. B. 49:281-284. 50. Thevenot, D., A. Dernburg, and C. Vernozy-Rozand. 2006. An updated review of Listeria monocytogenes in the pork meat industry and its products. J. Appl. Microbiol. 101:7-17. 51. Thibodeau, V., E. H. Frost, S. Chenier, and S. Quessy. 1999. Presence of Yersinia enterocolitica in tissues of orally-inoculated pigs and the tonsils and feces of pigs at slaughter. Can. J. Vet. Res. 63:96-100. 52. Tudor, L., E. Mitranescu, L. Tudor, F. Furnaris, and L. Ilie. 2009. The isolation prevalence of bacteria belonging to Yersinia genus isolated from carcasses and organs of wild boar. p. 761-764. In, Sustainable animal husbandry: prevention is better than cure: Proceedings of the 14th International Congress of the International Society for Animal Hygiene, vol. 2. 53. USMEF. 2013. Leading Markets for U.S. Pork Variety Meats Exports. In USDA (ed.) USMEF, Denver, CO. 54. USMEF. 2014. Leading Markets for U.S. Pork Variety Meat Exports. In USDA (ed.) USMEF, Denver, CO. 55. von Altrock, A., U. Roesler, R. Merle, and K.-H. Waldmann. 2010. Prevalence of pathogenic Yersinia enterocolitica strains on liver surfaces of pigs and their antimicrobial susceptibility. J. Food Prot. 73:1680-1683. 56. Wenzel, J. J., J. Preib, M. Schemmerer, B. Huber, A. Plentz, and W. Jilg. 2011. Detection of hepatitis E virus (HEV) from porcine livers in Southeastern Germany and high sequence homology to human HEV isolates. J. Clin. Virol. 52:50-54. 57. Wilson, A. 1998. Wilson's Practical Meat Inspection. Blackwell Science Ltd., London, UK. 58. Woolthuis, C. H. J., D. A. A. Mossel, J. G. V. Logtestijn, J. M. d. Kruijf, and F. J. M. Smulders. 1984. Microbial decontamination of porcine liver with lactic and and hot water. J. Food Prot. 47:220-226. 59. Zhu, W. G., S. Q. Xue, C. X. Xu, and X. F. Guo. 2005. Isolation and identification of Escherichia coli O157:H7 in Guangdong Province. Chinese J. Zoonoses. 21:147-149.