PSYCHOTHERAPY = talking therapy Expressive = patient does
advertisement
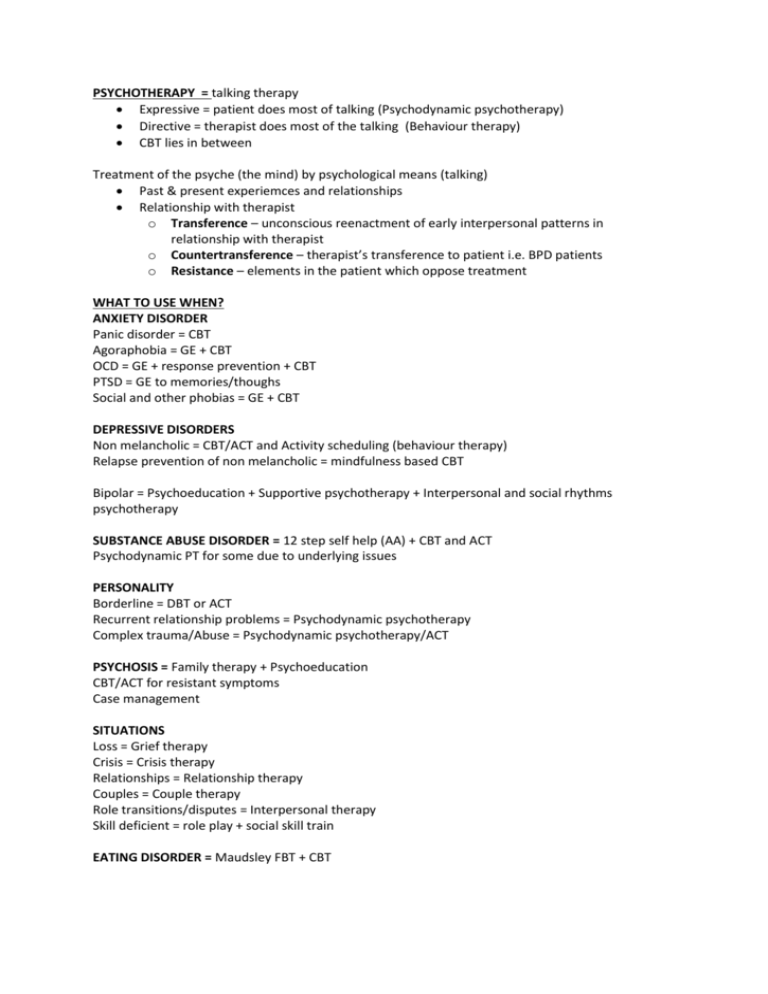
PSYCHOTHERAPY = talking therapy Expressive = patient does most of talking (Psychodynamic psychotherapy) Directive = therapist does most of the talking (Behaviour therapy) CBT lies in between Treatment of the psyche (the mind) by psychological means (talking) Past & present experiemces and relationships Relationship with therapist o Transference – unconscious reenactment of early interpersonal patterns in relationship with therapist o Countertransference – therapist’s transference to patient i.e. BPD patients o Resistance – elements in the patient which oppose treatment WHAT TO USE WHEN? ANXIETY DISORDER Panic disorder = CBT Agoraphobia = GE + CBT OCD = GE + response prevention + CBT PTSD = GE to memories/thoughs Social and other phobias = GE + CBT DEPRESSIVE DISORDERS Non melancholic = CBT/ACT and Activity scheduling (behaviour therapy) Relapse prevention of non melancholic = mindfulness based CBT Bipolar = Psychoeducation + Supportive psychotherapy + Interpersonal and social rhythms psychotherapy SUBSTANCE ABUSE DISORDER = 12 step self help (AA) + CBT and ACT Psychodynamic PT for some due to underlying issues PERSONALITY Borderline = DBT or ACT Recurrent relationship problems = Psychodynamic psychotherapy Complex trauma/Abuse = Psychodynamic psychotherapy/ACT PSYCHOSIS = Family therapy + Psychoeducation CBT/ACT for resistant symptoms Case management SITUATIONS Loss = Grief therapy Crisis = Crisis therapy Relationships = Relationship therapy Couples = Couple therapy Role transitions/disputes = Interpersonal therapy Skill deficient = role play + social skill train EATING DISORDER = Maudsley FBT + CBT Psychodynamic Psychotherapy = Part of unconscious and consciousness are in dynamic/moving flux Feelings -> Thoughts -> Behaviour Feeling come from unconscious impulses and drives developed during early childhood before we can put words to experiences Therapy makes unconscious conscious and lessens associated emotional pain Look at: Symptoms = go to the root Recent events Events in room = how they are responding Past events which formed personality Involves = can be individual or group Free association Dreams Transference = feelings patient brings into the room Identifying psychological defences Help patient improve insight; used in depression, anorexia nervosa and personality Psychoanalysis (exploratory psychotherapy) = Developed by Feud, goal is self-revelation and insight Exploration of the meaning of early experiences and affect emotions/ behavior presently Relationship troubles from relationship with mother Time intensive Need to be able to think abstractly – intelligent, willing to change For individuals who can tolerate ambiguity in explorations of feelings and treatment Supportive Psychotherapy = don’t go deep just listen, clarify and occasionally confront Goal is not insight but reduction of anxiety Strengthen healthy defense mechanisms to assist in day-to-day functioning Techniques include: enhancing self-esteem, clarification, confrontation, rationalization, reframing, encouragement, rehearsal/anticipation, de-catastrophizing, allowing ”venting” of frustrations Interpersonal therapy = focus on role transition and role disputes Short-term treatment looking at relationship patterns and teaching coping mechanisms Good for depression, bipolar Focus on personal social roles and relationships to help deal with current problems Defenses = a dead dog Denial = still put out dinner Repression = can’t remember dogs name Displacement = hard day at work so kick another dog Intellectualization = unemotionally describes detail of death Rationalization = Paul wants a dog but wife doesn’t. Paul adopts her reasoning Humor = jokes about dead dogs Projection = harry can’t run so makes dog run instead Reaction formation = Janine loves her old dog but says they should get ride of him when she sees him – respond with exact opposite of feelings Acting out = kills dog because parents like sister Behavior Therapy = do first, feel good after Direct patient to do sometime – aim to improve symptoms not underlying cause Exposure and relaxation training Useful in ANXIETY/SUBSTANCE ABUSE Modification of internal & external events which precipitate or maintain emotional distress Graded exposure Activity scheduling Systematic desensitization Flooding – confronting feared stimulus for prolonged periods Positive reinforcement Negative reinforcement Extinction – causing a behaviour to diminish by not rewarding it Punishment (aversion therapy) Biofeedback = understand physiological functions – aim to manipulate For incontinence, stress, PTSD, GAD, migraine = conditions that have autonomic response Cognitive Therapy= moods and feelings are influences by one’s thoughts Psychiatric disturbances are frequently caused by habitual errors in thinking Goal is to help patient become aware of automatic thoughts and correct assumptions with a more balanced view Useful for depression, anxiety disorders, self-esteem problems Use of this therapy presupposes a significant level of functioning Utilises “thought journal” to determine when/where thoughts occur and what underlying error in thinking may be Cognitive Behaviour Therapy (CBT) = thoughts lead to behavior so change both – change thinking Short term approach for emotional, behavioural and psych disorders Combines cognitive & behaviour therapies to teach patient to weaken connections between thinking patterns, habitual behaviours and mood/anxiety problems Elements: education, relaxation exercises, coping skills training, stress management, assertiveness Good Rx for depression/anxiety (mild – moderate); also eating disorders, medication conition NEED SELF-MOTIVATED INDIVIDUALS Mindfulness Based Cognitive Therapy – depression, bipolar, PTSD, anxiety Don’t change your thinking, change relationship to thoughts and feeling Paying attention to own thoughts, defusing them and engaging with reality and curiosity **reduces rate of melancholic depression relapse Acceptance and Commitment Therapy = Mindfulness without meditation Motivational Interviewing = Identify and change maladaptive behaviors (Quit smoking) Match strategies implemented to ones’ readiness to change Derived from CBT & readiness-to-change models Dialectical Behaviour Therapy Therapy that combines CBT technique with approaches from meditation Effective for borderline personality disorder 4 types of skills: mindfulness, emotion regulation, interspersonal effectiveness and distress tolerance Individual & group therapy settings Group psychotherapy Goals: self-understanding, acceptance, social skills Creates a microcosm of society Family Therapy = Family system considered more influential than individual Focuses on: here and now, reestablishing parental authority, strengthening normal boundaries and rearranging alliances Hypnosis = Looks for distortions in family systems Case Management = monitor mental state, risk assessment, compliance and side effects Report back to treating team and mobilise help as needed Good for chronically and severely ill with social issues = Schizophrenia, bipolar, ABI CATT = risk + mental illness Social work = finances, accommodation, vocational



![UW2 - Psychiatric Treatments [2014]](http://s3.studylib.net/store/data/006859622_1-db6167287f6c6867e59a56494e37a7e7-300x300.png)