ISARP New Brunswick 2014 Program 8
advertisement

INTERNATIONAL SOCIETY FOR ADVANCEMENT
OF RESPIRATORY PSYCHOPHYSIOLOGY
ANNUAL MEETING SEPTEMBER 19-21, 2014
Hosted by Rutgers University – Robert Wood Johnson Medical School
Department of Psychiatry and Office of Global Health
1
CLINICAL ACADEMIC BUILDING
RUTGERS – ROBERT WOOD JOHNSON MEDICAL SCHOOL
125 PATTERSON ST, NEW BRUNSWICK, NJ 08901
2
ISARP New Brunswick 2014 PROGRAM
Friday, September 19, 2014 (evening program open to the
Rutgers community)
5 – 5:30 PM Registration
5:30 – 6:30 PM
Welcome
Anthony Scardella
Rutgers University – Robert Wood Johnson Medical School
New Brunswick, NJ, USA
Organizer’s address
BREATH, BEATS, AND BEHAVIOR: Applied Psychophysiology, Stress
Management, and Behavioral Medicine
Paul Lehrer
Rutgers University – Robert Wood Johnson Medical School
New Brunswick, NJ, USA
6:30-8:30 Reception and registration
3
Saturday, September 20, 2014
8:00 – 8:30 AM
Conference Registration (coffee available)
8:30 – 10:00 AM
Symposium 1 Psychophysiology of coughing in neurological disease and
healthy people
Chair: Paul Davenport
Co-Chair: Karen Hegland
University of Florida, Gainesville, FL, USA
The impact of harmfulness information on urge-to-cough
Thomas Janssens, Sarah Brepoels, Lieven Dupont, Omer Van den Bergh
University of Leuven, Leuven, Belgium
The effect of expiratory muscle strength training (EMST) on
urge-to-cough in stroke patients
Karen W. Hegland1 kwheeler@ufl.edu
Michelle S. Troche,1 Floris Singletary, 2 Paul W. Davenport1
1University of Florida
2Brooks Rehabilitation Clinical Research Center Jacksonville, FL,
USA Gainesville, FL
Deep Brain stimulation and airway protection in Parkinson’s
disease
Michelle S. Troche michi81@PHHP.UFL.EDU
Karen W. Hegland, Alexandra E. Brandimore, Michael Okun, Paul
W. Davenport
University of Florida, Gainesville, FL, USA
Assessment of dystussia in traumatic brain injury
Erin Silverman 1,2,3 epearson@ufl.edu
Sarah Miller3, Christine Sapienza4, Paul W. DavenportPhD1
1University of Florida, Gainesville, FL
2North Florida South Georgia Veteran’s Health System, Malcom Randall
VAMC
3University of Memphis, Memphis, TN, USA
4 Jacksonville University, Jacksonville, FL, USA
4
10:00 – 10:30 AM
Coffee/tea/snack break
10:30 – 12:00 PM
Symposium 2 Respiratory retraining in asthma
Chair: Jonathan Feldman
Ferkauf Graduate School of Psychology, Yeshiva University, Bronx, NY, USA
Dysfunctional Breathing- The significance of a multi-dimensional
view for breathing re-training in asthma
Rosalba Courtney breathandbody@optusnet.com.au
Southern Cross University, East Lismore NSW, Australia
Heart rate variability biofeedback: its role in asthma therapeutics
Paul Lehrer1 lehrer@rwjms.rutgers.edu
Frederick Wamboldt,2 Evgeny Vaschillo1, Charles Irvin,3 Shou-En Lu,1
Milisyaris Aviles, 1 Jessica Graves2
1Rutgers --- The State University of NJ, Piscataway, NJ, USA
2National Jewish Health, Denver, CO, USA
3 University of Vermont, Burlington, VT, USA
Pilot Study of Hypoventilation Treatment on Anxiety in Patients
with Asthma
Alicia E. Meuret,1 ameuret@mail.smu.edu
David Rosenfield,1 Ashton M. Steele,1
Mark. M. Millard,2 Thomas Ritz,1
1Southern Methodist University, Dallas, Texas, USA
2Baylor University Medical Center, Dallas, Texas, USA
Hypoventilation training in asthma: Results from a capnometryassisted breathing training trial
Thomas Ritz,1 tritz@mail.smu.edu
David Rosenfield,1 Ashton M. Steele,1 Mark. M. Millard,2 Alicia E.
Meuret,1
1Southern Methodist University, Dallas, Texas, USA
2Baylor University Medical Center, Dallas, Texas, USA
12:00 – 1:30 PM
Lunch
5
1:30 – 2:30 PM
Invited Address
Chair: Paul Lehrer
Rutgers – Robert Wood Johnson Medical School
Let's talk about asthma and vocal cord dysfunction
Charles Irvin
University of Vermont, Burlington, VT, USA
2:30-4:00 PM
Poster Session (with coffee)
4:00-5:30 PM
Symposium 3: Effects of voluntary breathing maneuvers
Chair: Thomas Ritz
Southern Methodist University, Dallas, TX, USA
The effect of slow diapragmatic breathing on heart beat and event related
potentials (HEPs)
Richard Gevirtz, rgevirtz@alliant.edu
California School of Professional Psychology, Alliant University
San Diego, CA, USA
Sigh to restore respiratory variability. Proposed mechanism
Evgeny Vaschillo evaschil@rci.rutgers.edu
Bronya Vaschillo, Jennifer Buckman, Sydney Heiss, Marsha Bates
Rutgers University, Piscataway, New Jersey, USA
The effect of sighs on self-reported relief and physiological muscle tension.
Elke Vlemincx elke.vlemincx@ppw.kuleuven.be
Ilse Van Diest, Omer Van den Bergh
University of Leuven, Leuven, Belgium
Indirect regulation of breathing: a detour may be fastest
Jan van Dixhoorn dixhoorn@versatel.nl
Centre for breathing Therapy, Amersfoort and Research Center Linnaeus Institute,
Haarlem. The Netherlands
6
6:00 PM
ISARP Dinner, The Rutgers Club
199 College Avenue, New Brunswick
Sunday, September 21, 2014
7-8:15 AM
Board meeting
8-8:30 AM Registration
8:15-10:30 AM
Symposium 4: Affect and respiratory sensation.
Chair: Alicia Meuret, Southern Methodist University, Dallas, TX, USA
How is breathlessness remembered by patients with Medically
Unexplained Dyspnea?
Marta Walentynowicz Marta.Walentynowicz@ppw.kuleuven.be
Katleen Bogaerts, Linda Stans, Ilse Van Diest, Filip Raes, Omer Van den Bergh
University of Leuven, Leuven, Belgium
Neural processing of short-term habituation and sensitization to dyspnea
Andreas Von Leupoldt1,2 andreas.vonleupoldt@ppw.kuleuven.be
Roland W Esser 2, MMatthias Gamer 2, Christian Büchel2, Maria Cornelia Stoeckel
2
1
2
University of Leuven, Leuven, Belgium
University Medical Center Hamburg-Eppendorf, Hamburg, Germany
7
Affective Modulation of respiratory sensory gating: a mechanism for the
emotion-related overperception of respiratory sensations?
Cecile Chenivesse1,2,3,4, cchenivesse@ufl.edu
Pei Ying Chan5, Hsiu-Wen Tsai1, Karen Wheeler-Hegland6, Erin Silverman1,
Andreas Von Leupoldt7, Thomas Similowski2,3,4, Paul W Davenport1
1 University of Florida, Gainesville, FL
2 AP-HP, Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Paris, France
3 Sorbonne Universités, Paris, France
4 INSERM, UMR_S 1158, Neurophysiologie Respiratoire Expérimentale et
Clinique, Paris, France
5 Chang Gung University, Taiwan
6University of Florida, Gainesville, FL, USA
7 University of Leuven, Leuven Belgium
Symptom perception and affect: A theoretical account
Omer Van den Bergh, Omer.VandenBergh@ppw.kuleuven.be
University of Leuven, Leuven, Belgium
Psychological treatment of comorbid asthma and panic disorder in Latino
adults: Results from a randomized controlled pilot study
Jonathan M. Feldman,PhD1 JFeldman@aecom.yu.edu
Lynne Matte,1 Alejandro Interian,2 Paul M. Lehrer,3 Bari Scheckner,1 Dara
Steinberg,1 Shou-En Lu,3., Anu Kotay,4 Sumita Sinha,4 Chang Shim5
1Ferkauf Graduate School of Psychology, Yeshiva University
2VA New Jersey Healthcare System
3Rutgers – The State University of New Jersey
4 Montefiore Medical Center/Albert Einstein College of Medicine
5 Jacobi Medical Center/Albert Einstein College of Medicine
Management of psychological comorbidities in females with COPD in a
rural healthcare setting
Sarah Miller1 sarahmilleruf@gmail.com
Erin Silverman2, 3, 4, Belinda Fleming 1
1 University of Memphis, Memphis, TN
2 University of Florida, Gainesville, FL
3North Florida South Georgia Veteran’s Health System, Malcom Randall
VAMC 4Rehabilitation Outcomes Research Center – Malcom Randall VAMC,
Gainesville, FL
10:45 – 11:15 AM
8
Coffee/tea/snack break
11:15 – 12:15 PM
Invited Address
Chair: Omer Van den Bergh, University of Leuven, Leuven, Belgium
Psychological and physiological effects of exposure to inhaled
environmental toxins and irritants.
Nancy Fiedler nfiedler@eohsi.rutgers.edu
Rutgers – The State University of New Jersey, Piscataway, NJ, USA
12:15 – 1:45 PM
(Lunch – on your own, please see restaurant list)
1:45 – 3:45 PM Symposium 5: Social influences on asthma
Chair: Daphne Koinis-Mitchell, The Warren Alpert Medical School of Brown
University, Providence, RI, USA
Child Parent Symptom Perception as Predictors of Asthma Illness
Representations and Asthma Control
Kimberly Arcoleo1 Arcoleo.1@osu.edu
Jonathan Feldman2
1The Ohio State University, College of Nursing, Columbus, OH, USA
2 Yeshiva University, Ferkauf Graduate School of Psychology
Bronx, NY, USA
Cumulative prenatal and early childhood stress associated with poor
lung growth and reduced exhaled nitric oxide in school-aged urban
children.
Yueh-Hsui Mathilda Chiu1 (Rosalind J. Wright) rosalind.wright@mssm.edu
Wayne Morgan,2 Thomas Ritz,3 Brent A. Coull,4 Robert O. Wright,1 Rosalind
Wright1
1Icahn School of Medicine at Mount Sinai, New York, NY
2University of Arizona, Tuscon, AZ
3Southern Methodist Univesity, Dallas, TX
4Harvard School of Public Health, Boston, MA
9
Psychiatric symptoms, bronchodilator response, and symptom
magnification in Latino children with asthma
Elizabeth L. McQuaid1. elizabeth_mcquaid@brown.edu
Nicole R. Nugent,1., Daphne Koinis-Mitchell,1., Ronald Seifer, 1., Glorisa
Canino, 2., Gregory K. Fritz1
1Bradley/Hasbro Children’s Research Center, Alpert Medical School Brown
University, Providence, RI, USA
2Behavioral Sciences Research Institute, University of Puerto Rico Medical
Sciences Campus, San Juan, PR, USA
Immediate Efficacy of a School-based Intervention for Urban Adolescents
with Undiagnosed Asthma: A Randomized Control Trial
Bruzzese, Jean-Marie
Jean-Marie Bruzzese1 Jean-Marie.Bruzzese@nyumc.org
Amarilis Cespedes1, Sharon Kingston2, Beverley J. Sheares3, Zhe Su1, Hossein
Sadeghi3, Meyer Kattan3, David Evans3
1NYU School of Medicine, New York, NY
2Dickinson College, Carlisle, PA
3Columbia University College of Physicians and Surgeons, New York, NY
Rhinitis Symptoms and Asthma Control in Urban Children with Asthma
and Allergic Rhinitis
Robin S. Everhart1
Sheryl J. Kopel,2 Cynthia A. Esteban,2 Elizabeth L. McQuaid,2 Greg Fritz,2
Robert Klein,2 Daphne Koinis-Mitchell2
1 Virginia Commonwealth University, Department of Psychology, Richmond,
VA USA,
2 Bradley/Hasbro Children’s Research Center, Alpert Medical School, Brown
University, Providence, RI USA
3:45 – 4:14 PM
Coffee/tea/snack break
10
4:15 – 5:15 PM
Presidential Address
Asthma and sleep in an urban context: research, education, and
intervention
Daphne Koinis-Mitchell
The Warren Alpert Medical School of Brown University, Providence, RI, USA
5:15 – 5:45 PM
Student Awards and business meeting
Preview of ISARP 2015
ISARP Business Meeting
11
ISARP 2014
Poster Session
Posters should be put up as soon after registration as possible, and left up for the entire meeting. It will
be desirable for poster presenters to be near their posters for periods of time during session breaks, and
should leave contact information near the poster for those interested in discussing it.
B4
Aviles-Velez
avilesmi@rwjms.rutgers.edu
Effect of Heart Rate Variability Biofeedback on Methacholine
Airway Reactivity in a Sample of Steroid Naïve Asthma
Patients
Milisyaris Aviles-Velez,1 Jessica Graves,2 Charles Irvin,3
Frederick Wamboldt2 Shou-En Lu, Paul Lehrer1
A1
Brandimore
aessman@ufl.edu
Respiratory kinematics of reflex and voluntary
cough in healthy adults
Alexandra E. Brandimore, Michelle S. Troche, Paul
W. Davenport,
Karen W. Hegland
University of Florida, Gainesville, FL, USA
B1
Chiu
cornelchiu@yahoo.com
Autonomic effects of heart rate variability in a
study of patients with mild and moderate asthma
Cornel Chiu,1 Evgeny Vaschillo, 1 Milisyaris Aviles,1
Shireen Hamza, 1 Maria Katsamanis, 1 Frederick
Wamboldt, 2 Jessica Graves, 2 Shou-En Lu,1 Paul
Lehrer1
1Rutgers – The State University of New Jersey,
Piscataway, NJ, USA
2National Jewish Health, Denver, CO, USA
A3
Cox
pcox1@hmc.psu.edu
Sensory distraction via cutaneous stimulation
reduces dyspnea in COPD patients.
Phillip Cox DO, Ben Bartsch, Philippe Haouzi
Penn State Hershey Medical Center, Division of
Pulmonary and Critical Care Medicine
12
B9
Eddie
Heart Rate Variability Biofeedback to Reduce
daveddie@scarletmail.rutgers.edu Craving During Treatment for Substance Use
Disorders
David Eddie, 1 Chrys Kim, 1 Paul Lehrer, 1 Erin
Deneke,2 Marsha E. Bates1
1Rutgers – The State University of New Jersey,
Piscataway, NJ, USA
2
Caron Treatment Centers, Wernersville PA, USA
D5
Grinberg
alice.grinberg@gmail.com
A4
Guardiola
jerry.yu@louisville.edu
Activation of chemosensors in the lung
stimulates breathing
Juan Guardiola. Jerry Yu
Robely Rex VA Medical Center and University of
Louisville, Louisville, KY, USA
C1
Leyro
Nicotine withdrawal severity moderates the relation
between panic disorder status and physiological stress reactivity
Teresa M. Leyro 1
Michael J. Zvolensky 2
1
Rutgers – The State University of New Jersey, Piscataway, NJ, USA
2
University of Houston, Houston, TX, USA
teresa.leyro@rutgers.edu
D1
Oken
okentt@gmail.com
Respiratory disease and executive functioning
among adults in the United States
Alice Grinberg,1 Renee Goodwin 1, 21 Department
of Psychology, City University of New York (CUNY),
Flushing, NY USA
2 Department of Epidemiology, Mailman School of
Public Health, New York, NY, USA
The relationship between heart rate variability,
depression, and anxiety: baseline findings from a
randomized controlled trial of a panic disorder
intervention for Latino adults with asthma
Tanya Oken1, Jonathan M. Feldman1 and Paul
Lehrer2
1Ferkauf Graduate School of Psychology, Yeshiva
University, Bronx, NY, USA
2Rutgers – The State University of New Jersey,
Piscataway, NJ, USA
13
B2
Maulion
pdm62@scarletmail.rutgers.edu
Effects of Heart Rate Variability Biofeedback on
Airway Inflammation
Patrick Maulion1, Milisyaris Aviles1, Jessica
Graves2, Frederick Wamboldt2, Shou-En Lu,1 Paul
Lehrer1
1Rutgers – The State University of New Jersey,
Piscataway, NJ, USA
2National Jewish Health, Denver, CO
D4
Raveensdran
esperanza.morales@nyu.edu
The Relationship between Acculturation,
Asthma Psychological Triggers, and Utilization of
Quick Relief Medication in Mexican and Puerto
Rican Families
Esperanza Morales Raveendran1, Kimberly
Arcoleo2, MPH, Jonathan Feldman1
1Ferkauf Graduate School of Psychology Yeshiva
University; New York, USA
2 Ohio State University College of Nursing,
Columbus, OH, USA
B7
Ritz
tritz@mail.smu.edu
Correcting respiratory sinus arrhythmia for
respiratory influences: Findings with an infant
stress paradigm
Thomas Ritz1, Michelle Bosquet Enlow2, Lucy
King2, Hannah Schreier3, Kelly Brunst3, Stefan M.
Schulz4, Rosalind J. Wright4
1 Southern Methodist University, Dallas, TX, USA
2 Boston Children's Hospital and Harvard Medical
School, Boston, MA, USA
3 Icahn School of Medicine at Mount Sinai, New
York, NY, USA
4 University of Wuerzburg, Wuerzburg, Germany
D2
Sandler
jonmsandler@gmail.com
Asthma-Related Death of a Loved One, Panic
Disorder, and Ataque de Nervios in Latino Adults
with Asthma
Jonathan M. Sandler, Jonathan M. Feldman
Ferkauf Graduate School of Psychology, Yeshiva
University, Bronx, NY, USA
14
D3
C2
Scheckner
The Effect of Parental Social Support and
Bari.Scheckner@psych.ferkauf.yu.e Acculturation on Childhood Asthma Control
du
Bari Scheckner,1 Kimberly Arcoleo, PhD3,
Jonathan M. FeldmanPhD1,2
1Ferkauf Graduate School of Psychology, Yeshiva
University, NY
2Department of Epidemiology and Population
Health, Albert Einstein College of Medicine, NY
3Ohio State University College of Nursing, OH
Schroijen
Mathias.Schroijen@ppw.kuleuven.
be
Assessing differential effects of fear and anxiety
to respiratory threat.
Mathias Schroijen1, Simona Fantoni1, Carmen
Rivera1, Bram Vervliet1, Koen Schruers12, Omer
Van den Bergh1 Ilse Van Diest1
1KU Leuven - University of Leuven, Leuven
Belgium.
2Maastricht University, the Netherlands.
Singer
spaceman792@live.com
Effects of heart rate variability biofeedback on
asthma symptoms
Michael Singer,1 Gabriel Pontipiedra,1 Kevin Ma,1
Nimesh Patel,1 Patrick Maulion,1 Milisyaris
Aviles,1 Jessica Graves, 2 Frederick Wamboldt,2
Shou-En Lu,1 Paul M Lehrer1
1Rutgers—The State University of New Jersey,
Piscataway, NJ,USA
2National Jewish Health, Denver, CO, USA
C3
Van Den Houte
Maaike.VanDenHoute@ppw.kuleu
ven.be
Low end-tidal PCO2 across stress-related
disorders: A transdiagnostic exploration of its
correlates
Maaike Van Den Houte, Katleen Bogaerts, Lukas
Van Oudenhove, Ilse Van Diest Omer Van den
Bergh
University of Leuven, Leuven, Belgium
B5
van Dixhoorn
dixhoorn@versatel.nl
Psychophysiological treatment of anxiety: does
the diagnosis matter?
Jan van Dixhoorn
Centre for breathing Therapy, Amersfoort and
Research Center Linnaeus Institute, Haarlem. The
B3
15
Netherlands
B6
Vaschillo
evaschil@rci.rutgers.edu
Resonance breathing affects hemodynamic
oscillations in the brain at 0.1 Hz
Evgeny Vaschillo,1 Jennifer F Buckman,1 Deena
Peyser 1 Sydney Heiss,1 Peter Barnas,1 Laura
Banu, 1 Alexander Puhalla, 1 Bronya Vaschillo,1
David Eddie,1 Suchismita Ray,1 Stephen Hanson,2
Catherine Hanson,2 Bharat Biswal,3 Marsha E
Bates1
1Rutgers – The State University of New Jersey,
Piscataway, NJ, USA
2Rutgers – The State University of New Jersey,
Newark, NJ, USA
3New Jersey Institute of Technology, Newark, NJ,
USA
C6
Vazquez
Asthma triggers in Latino adults with
comorbid asthma and panic disorder
kvazquez427@gmail.com
Karinna Vazquez, Jonathan Feldman
Yeshiva University, Ferkauf Graduate School of
Psychology, Bronx, NY, USA
C4
Walentynowicz
Marta.Walentynowicz@ppw.kuleu
ven.be
Retrospective memory for breathlessness and
pain.
Marta Walentynowicz,1 Ilse Van Diest,1 Filip
Raes,2 Omer Van den Bergh1
1Health Psychology, 2 Learning and Experimental
Psychopathology, University of Leuven, Leuven,
Belgium
C5
Wuyts
ruth.wuyts@ppw.kuleuven.be
The influence of respiratory dynamics on
relaxation and cardiorespiratory parameters
and the response to and recovery from mental
stress.
Ruth Wuyts, Elke Vlemincx, Ilse Van Diest, Omer
Van den Bergh
University of Leuven, Leuven, Belgium
16
ABSTRACTS (alphabetical order)
Child & parent symptom perception as predictors of asthma illness representations and
asthma control
Kimberly Arcoleo, PhD1 Arcoleo.1@osu.edu
Jonathan Feldman, PhD2
1
2
The Ohio State University, College of Nursing, Columbus, OH, USA
Ferkauf Graduate School of Psychology, Yeshiva University, Bronx, NY, USA
Background: Asthma remains a major public health problem despite advances in pharmacologic
management of the disease. Recognition of asthma symptoms and early warning signs is dependent upon
subjective perceptions of children and parents. Failure to detect asthma symptoms is associated with
poor asthma control. What is not known is how children’s and parents’ symptom perception influences
their asthma illness representations which are predictive of asthma control.
Methods: 1 year longitudinal study of 300 Mexican & Puerto Rican mothers & 300 children ages 5–12
w/asthma recruited from 2 school-based health centers & Breathmobile in Phoenix, AZ & 1 pediatric
asthma & allergy clinic in Bronx, NY. Interviews & child PFTs @ baseline and 3, 6, 9, & 12 months; medical
record reviews @ 12 months.
Results. Results from N=267 baseline interviews. SEM examined effects of sociodemographic
characteristics, parental depression, child and parent symptom perception, and asthma illness
representation on clinician rated asthma control by ethnicity. Results: The data fit the model well
(RMSEA=.02, CFI=.97, TLI=.93, Χ2=.39) and accounted for 22% of the variance in AIRS scores and 9% in
asthma control. Parents reporting higher depressive symptoms, living in poverty, lower education, and
higher panic and irritability had AIRS scores aligned with the lay model. There was no effect for children’s
symptom perception. AIRS scores congruent with the lay model and Puerto Rican ethnicity were
associated with poor asthma control. There was an indirect effect of parents’ education through AIRS on
asthma control.
Discussion: A window of opportunity exists when asthma patients can use bronchodilator medications to
prevent asthma exacerbations and maintain good control. Parents who have elevated depressive
symptoms, panic, and irritability may delay administration of medications resulting in adverse health
outcomes for their children. Interventions targeting medication adherence need to assess and treat
caregiver psychiatric disorders to achieve optimal outcomes.
17
Effect of Heart Rate Variability Biofeedback on Methacholine Airway Reactivity in a
Sample of Steroid Naïve Asthma Patients
Milisyaris Aviles-Velez, MS1 avilesmi@rwjms.rutgers.edu
Jessica Graves, MA2 Charles Irvin, PhD3 Frederick Wamboldt, MD2 Shou-En Lu, PhD4 Paul Lehrer, PhD1
1 Department
of Psychiatry, Rutgers -- Robert Wood Johnson Medical School, Piscataway, NJ, USA
Jewish Health, Denver, CO, USA
3 University of Vermont, Burlington, VT, USA
4 Rutgers – School of Public Health, Piscataway, NJ, USA
2 National
Background: Asthma is a global health problem affecting around 300 million individuals of all ages, ethnic groups
and countries. It is estimated that by 2025 the number of people living with asthma will increase by 100 million,
becoming a global health priority. There is an imperative need to investigate effective innovative, effective and low
cost treatments to manage this condition. The present study investigates the effects of HRV Biofeedback and EEG
music and relaxation on airways hyperesponsiveness-one of the characteristic features of asthma.
Method: This is an interim analysis of an ongoing two-center trial. The patients received 4 visits of screening and
asthma education where pulmonary function was assessed. Participants who met the inclusion criteria were given a
methacholine challenge test. Participants who had FEV1 PC 20 < 8 mg/ml of methacholine were randomized to
either HRV biofeedback or EEG music and relaxation training. The participants trained for 8 visits as well as at home
using a StressEreaser or an identical placebo unit for 40 minutes per day. At the final visit the patients had a posttest(what test?) methacholine challenge.
Results: Data from 39 patients was used in the final analysis. Using a matched T-test, the HRV biofeedback group
showed a significant decrease in airways hyperresponsiveness t(16) = 2.50, p =.0236. The EEG + music + Paced
Breathing Group did not show significant changes t(21) = -.81, p =.4283. A sign rank test also yeilded positive results
for the group receiving HRV biofeedback with a unidirectional hypothesis; one sided, p =.0279.
Discussion: Airway hyper-reactivity in asthmatics has previously been shown to be associated with abnormal
autonomic nervous system (ANS) control. In particular, the parasympathetic (vagal) component of the ANS appears
to be implicated in the pathogenesis of asthma. Methacholine is a drug that will affect the parasympathetic control.
The current results suggest that the HRV biofeedback may impact the regulatory systems of the ANS mediated by
the vagal nerve that control airway function. Moreover we suggest that HRV biofeedback may provide an effective,
non drug and low cost therapy for asthma that patients seek.
18
Respiratory kinematics of reflex and voluntary cough in healthy adults
Alexandra E. Brandimore, MA/CCC-SLP1,2 aessman@ufl.edu
Michelle S. Troche, PhD/CCC-SLP, 2 Paul W. Davenport, PhD,3 Karen W. Hegland, PhD/CCC-SLP 1
1Department
of Speech, Language, & Hearing Sciences, University of Florida, Gainesville, FL, USA
Brain Rehabilitation Research Center, Malcom Randall VA, Gainesville, Florida, USA
3 Department of Physiological Sciences, University of Florida, Gainesville, Florida, USA
2
Background: Voluntary cough (VC), or cough initiated on command, is dependent upon cortically
mediated mechanisms (e.g. cognitive functioning, intention). In contrast, reflex cough (RC) is a
brainstem-mediated sensorimotor response to a stimulus (i.e. penetrant/aspirant in the airway), that is
modified cortically, or volitionally in the awake human. There is evidence to suggest that physiological
differences exist between the RC and VC; however, the mechanistic and airflow differences between the
cough types are not fully understood. Therefore, the aims of this study were to determine the lung
volume, respiratory kinematic and airflow differences between RC and VC in healthy young adults.
Methods: Twenty-five participants (14 female; 18-29 years) were recruited for this study. Participants
were evaluated using respiratory inductance plethysmography calibrated with spirometry. Experimental
procedures included: 1) respiratory calibration (rest breathing, vital capacity maneuvers, and isovolume
maneuvers), 2) three sequential voluntary cough trials, and 3) three reflex cough trials induced with 200
µM capsaicin. Repeated measures ANOVA and linear regression were used to evaluate the differences
between RC and VC.
Results: Lung volume initiation (LVI; p=.003) and lung volume excursion (LVE; p<.001) were significantly
greater for VC compared to RC. The rib cage and abdomen significantly influenced LVI for VC (p<.001);
however, only the rib cage significantly impacted LVI for RC (p<.001). LVI significantly influenced peak
expiratory flow rate for VC (p=.029), but not RC (p=.610).
Discussion: Production of a RC results in significant lung volume, respiratory kinematic and airflow
differences compared to VC. These findings likely reflect the influence of a perceived urge-to-cough prior
to RC whereby detection of the sensory stimulus modifies motor aspects of the reflexive behavior.
Further understanding of the urge-to-cough and the differences between RC and VC in older adults and in
persons with dystussia (cough dysfunction) will be essential to facilitate the development of successful
cough treatment paradigms.
19
Immediate efficacy of a school-based intervention for urban adolescents with
undiagnosed asthma: a randomized control trial
Jean-Marie Bruzzese, PhD1 Jean-Marie.Bruzzese@nyumc.org
Amarilis Cespedes, MPH,1 Sharon Kingston, PhD,2 Beverley J. Sheares, MD, MS,3 Zhe Su, MS,1 Hossein
Sadeghi, MD,3 Meyer Kattan, MD,3 David Evans, PhD3
1NYU
School of Medicine, New York, NY, USA
College, Carlisle, PA, USA
3Columbia University College of Physicians and Surgeons, New York, NY, USA
2Dickinson
Background: Undiagnosed asthma has high prevalence and morbidity in adolescents. No intervention has
specifically targeted undiagnosed adolescents. This study tests the immediate efficacy of Asthma SelfManagement for Adolescents with Undiagnosed Asthma (ASMA-Undx), a school-based intervention to
help adolescents obtain a clinical evaluation and diagnosis, and manage their symptoms.
Methods: 399 urban, predominately Hispanic and African American adolescents with symptoms of
moderate to severe persistent asthma, but no diagnosis, were randomized to ASMA-Undx or a control
condition. ASMA-Undx consists of (1) an 8-week intervention delivered to students, which includes
referral to their medical providers and group and individual coaching sessions to learn how to care for
asthma; (2) an intervention for the students’ caregivers delivered via mail and phone to help them
support their child’s efforts; and (3) education for students’ medical providers via academic detailing.
Primary outcomes were the proportion of students who: saw a medical provider for an evaluation; were
diagnosed with asthma; and were prescribed medication. Secondary outcomes were steps taken to
prevent and to manage symptoms, and self-efficacy to care for asthma. Treatment groups were
compared using Generalized Linear Mixed Effects Models. Intent-to-treat analyses controlled for baseline
outcome values and asthma severity, and included random effects for schools.
Results: Relative to controls, ASMA-Undx students had significantly (P<.0001) higher odds of obtaining a
clinical evaluation (OR=5.00), of being diagnosed with asthma (OR=8.03), and of obtaining asthma
medication (OR=5.71). They had higher rates of taking steps to prevent symptoms (RR=1.19, P<.01) and
more confidence to care for asthma (RR=0.58, P<.0001).
Discussion: ASMA-Undx, the first intervention designed specifically for adolescents with undiagnosed
asthma, results in improvements in rates of adolescents who obtain a clinical evaluation and a diagnosis,
and improvements in asthma self-management. Future studies should consider the long-term impact of
ASMA-Undx on asthma control and urgent health care utilization.
20
Affective modulation of respiratory sensory gating: a mechanism for the emotionrelated overperception of respiratory sensations?
Cecile Chenivesse, MD, PhD1,2,3,4, cecile.chenivesse@psl.aphp.fr
Pei Ying Chan, PhD,5 Hsiu-Wen Tsai, PhD,1 Karen Wheeler-Hegland, PhD/CCC-SLP, 6 Erin Silverman, PhD,1
Andreas Von Leupoldt, PhD,7 Thomas Similowski, MD, PhD,2,3,4 Paul W Davenport, PhD1
1 Department
of Physiological Sciences, University of Florida, Gainesville, FL 32610, USA
Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Pneumologie et Réanimation
Médicale, 47-83 boulevard de l’hôpital, F-75013, Paris, France
3 Sorbonne Universités, UPMC Univ Paris 06, UMR_S 1158, Neurophysiologie Respiratoire Expérimentale et
Clinique, F-75005, Paris, France
4 INSERM, UMR_S 1158, Neurophysiologie Respiratoire Expérimentale et Clinique, F-75005, Paris, France
5 Department of Occupational Therapy, Chang Gung University, Taiwan
6 Department of Speech Language and Hearing Sciences, University of Florida, Gainesville, FL 32610, USA
7 Research group on Health Psychology, University of Leuven, Belgium
2 AP-HP,
Background. Some patients are symptom overperceivers because they perceive respiratory sensations
with a higher intensity than expected for the magnitude of the stimulus. Clinical observations suggest that
psychological factors might cause an increase in respiratory sensory perception. The cortical neural
modulation of respiratory sensory processing by emotion is poorly understood. We hypothesize that
emotion-related respiratory overperception may be due to a decrease in the respiratory-related evoked
potentials (RREP) sensory gating (RSG).
Methods. The RSG was compared between negative and neutral emotional conditions in healthy subjects.
Emotions were modulated by IAPS pictures. The RSG was assessed by the RREP elicited by paired
inspiratory occlusions. The RSG was calculated as the difference between the second (S2) and first (S1)
occlusions RREP N1 peak amplitude.
Results. Six males and seven females (34 years [23;46]) were studied. Negative pictures were rated with a
lower valence and a higher arousal than neutral pictures (p=0.001). Viewing negative pictures decreased
the RREP N1 amplitude elicited by the S1 (Negative N1 = -3.37 µV [-4.62;-1.37] versus Neutral N1 = -4.59
µV [-6.08;-1.36]; p=0.017). The RREP N1 amplitudes produced by the S2 were not significantly different
between Negative and Neutral. The N1 amplitude difference between S1 and S2 was significantly reduced
in the Negative condition (Negative = 3.73 µV [0;5.82] versus Neutral = 4.79 µV [3;6.20]; p=0.038).
Discussion. The reduction in the RREP N1 amplitude elicited by the S1 occlusion while viewing negative
pictures is likely related to a shift of subject’s attention toward the emotional stimulus to the detriment of
the respiratory sensory inputs. Thus, negative pictures produced a decrease in the RREP measure of RSG.
These results suggest that negative emotions may increase respiratory sensory information activating the
cortex by reduced RSG and may be associated with an overperception of respiratory stimuli.
21
Autonomic effects of heart rate variability in a study of patients with mild and moderate
asthma
Cornel Chiu1 cornelchiu@yahoo.com
Evgeny Vaschillo, PhD 1 Milisyaris Aviles, MS 1 Shireen Hamza, 1 Maria Katsamanis, PsyD 1 Frederick
Wamboldt, MD 2 Jessica Graves, MA, 2 Shou-En Lu, PhD,1 Paul Lehrer, PhD1
1Rutgers
– The State University of New Jersey, Piscataway, NJ, USA
Jewish Health, Denver, CO, USA
2National
Background. Heart rate variability biofeedback (HRV-BF) has previously been found efficacious for
treating asthma. In this preliminary analysis on data from steroid-naïve adult asthma patients from a twocenter clinical trial with steroid naïve adult subjects, we examined autonomic effects of HRV-BF compared
with a control condition comprising training to increase EEG alpha, listening to relaxing music, and
breathing at a relaxed rate (about 15 breaths/min).
Methods. Subjects were randomly divided into two groups: HRV-BF and a combination of EEG
biofeedback, paced breathing at a comfortable rate between 10-12 breaths per minute, and listening to
relaxing music. They received 6-10 sessions of training over a three-month period, with assigned daily
practice. Physiological data weres collected each session during three visitsspaced evenly during the trial.
In each session, physiological data were recorded during a five minute baseline (plain vanilla task),
followed by five minutes of,intervention (HRV-BF or EEG biofeedback plus breathing at a relaxed rate) and
then another 5-min baseline.
Results. Forty-seven participants in began the trial. In later sessions there were a decreased number of
participants because some had not yet completed the study. This discrepancy was taken into account to
prevent it from influencing the analysis. We analyzed heart rate, pulse transit time, respiration frequency,
and pulse amplitude, as well as oscillations in these measures in the high frequency (HF) (0.15-0.4 Hz),
low frequency (LF) (0.05-0.15 Hz), and very low frequency (VLF) (0.005-0.15 Hz) ranges. HRV biofeedback
patients slowed their breathing during paced breathing periods to about 6 times a minute, with large
increases in LF and total HRV, while patients in the relaxed breathing condition breathed about 15 times a
minute, with little change in HRV measures. Pulse transit time variability increased in the HRV BF group,
particularly in the VLF range, andboth mean and variability of pulse amplitude decreased.
Discussion. Participants adhered to the directions and performed HRV biofeedback correctly. Changes in
pulse transit time and pulse amplitude suggested that the HRV-BF procedure stimulates the alpha
sympathetic system, and the sympathetically-mediated vascular tone branch of the baroreflex system.
There is some evidence that the alpha sympathetic system may play a role in asthma, particularly
exercise-induced asthma. Further analysis and study is needed to determine whether these changes
mediate biofeedback-induced therapeutic changes in asthma.
22
Cumulative prenatal and early childhood stress associated with poor lung growth and reduced
exhaled nitric oxide in school-aged urban children.
Yueh-Hsui Mathilda Chiu1 (Rosalind J. Wright) rosalind.wright@mssm.edu
Wayne Morgan,2 Thomas Ritz, PhD,3 BA Coull 4, Robert O. Wright, 1 Rosalind J. Wright, MD MPH1
1Icahn
School of Medicine at Mount Sinai, New York, NY
of Arizona, Tuscon, AZ
3Southern Methodist Univesity, Dallas, TX
2University
Background. An important step toward identifying children at risk for chronic respiratory disorders is
characterizing mechanisms that lead to and maintain early predisposition.
Method We indexed pre- and postnatal maternal stress by a negative life events (NLEs) score (range 0-9)
assessed prenatally, in the first 2 years of the child’s life (early postnatal) and at lung function testing (7.0
± 0.9 years) (late postnatal) in the Asthma Coalition on Community, Environment, and Social Stress
(ACCESS) Project. Outcomes were diagnosed asthma and forced expiratory volume in one second (FEV1),
forced vital capacity (FVC) and the FEV1/FVC ratio as well as exhaled nitric oxide (eNO), a measure of
eosinophilic airway inflammation. We considered pre- and/or postnatal NLEs separately and concurrently
(all moderately correlated, r<0.5, p=0.01), by collapsing scores into low (0-2, <median) and high (≥3,
>median) groups and categorizing as low pre/low postnatal, high pre/low postnatal, low pre/high
postnatal, and high pre/high postnatal stress.
Results. Mothers with higher NLEs in both the pre- and early postnatal periods were most likely to have
children with asthma (n=502). Children of mothers with high NLEs in both pre- and early postnatal periods
had decreased FEV1 and FVC with a preserved ratio (n=150). Children born to mothers reporting high
NLEs across all 3 periods had lower eNO levels at the 7 year follow-up compared to children whose
mothers reported low NLEs across all three periods.
Discussion. These data suggest that reduced lung function in relation to early life stress may be due to
compromised lung growth starting in utero and that oxidative stress and non-eosinophilic inflammation
may have a central role.
23
Dysfunctional breathing- the significance of a multi-dimensional view for breathing retraining in asthma
Rosalba Courtney, DO breathandbody@optusnet.com.au
Southern Cross University, East Lismore NSW, Australia
Background. A growing number of studies suggest that various breathing retraining programs may be
helpful in asthma. The main therapeutic rational for most of these programs is the correction of
dysfunctional breathing (DB). DB has been reported in 29-64% of asthma sufferers and it is thought to
contribute to symptoms and interfere with asthma treatment, however its definition is vague. It is still
unclear which patients or which types of breathing dysfunction respond best to particular breathing
exercise or retraining regimes. One definition of dysfunctional breathing proposes that it might be
viewed practically as a multi-dimensional entity with 3 key dimensions, biochemical, biomechanical and
psychopsychological. This review looks at evidence for the importance of each of these dimensions of
breathing dysfunction for breathing retraining protocols for asthma.
Methods. Data bases Medline, Scopus Proquest, Cinhahl and the Cochran Library were searches for
articles discussing dysfunctional breathing, breathing therapy, breathing training and asthma. Additional
relevant articles were sourced from reference lists of articles retrieved through database searches.
Results. There is evidence for the importance of biochemical, biomechanical and psychophysiological
dimensions of dysfunctional breathing in asthma. Aggravation of asthma symptoms can occur due to
hyperventilation, inefficient and aberrant breathing patterns associated with neuromuscular factors such
as muscle tension and hyperinflation, conditioned breathing behaviors and a patient’s sense of the
congruence of their symptoms and perceived control. Breathing retraining protocols may impact on all
these factors. However, it appears that improvements in these parameters and overall improvement in
asthma is more likely to occur when they are specifically measured and targeted.
Discussion. Breathing retraining for asthma is more likely to be successful when it is targeted,
individualized, comprehensive and sufficiently intensive to produce measurable improvements in related
but also separate dimensions. Ideal breathing therapy should address hyperventilation, breathing
behaviors and psychophysiological factors.
24
Sensory Distraction via Cutaneous Stimulation Reduces Dyspnea in COPD Patients.
Phillip Cox, DO, pcox1@hmc.psu.edu
Ben Bartsch, MD, Philippe Haouzi, MD PhD
Penn State Hershey Medical Center, Division of Pulmonary and Critical Care Medicine
Rationale: We have recently reported that transcutaneous electrical neural stimulation (TENS) of the C3C5 dermatome alleviates the sensation of dyspnea in a patient with intractable dyspnea following a
herpes zoster eruption affecting the cervical dorsal roots. We postulated that the remarkable benefit of
this stimulation was to be accounted for by the specific blockade of unmyelinated fibers originating from
the diaphragm and/or more likely from unspecific “sensory” distraction, a phenomenon already described
with auditory or visual inputs. We sought to determine whether this unspecific “sensory” distraction
patients with chronic obstructive disease.
Methods: 23 Patients (18-83 years old, FEV1/FVC<70% predicted with FEV1 = 50.45±20.00%) performed 2
six-minute walk tests, separated by a 10-minute resting period. Heart rate, SpO2, and perceived level of
dyspnea were recorded every 30 second intervals using a modified Borg Index (0-10). Patients were
randomly assigned into one of three groups: control group (C), neck stimulation (N) or back stimulation
(B). During the first six-minute walk test no intervention was applied; during the second test, a TENS unit
was used to deliver via cutaneous electrodes the following stimulation (frequency of 80 Hz and pulse
width 50 microseconds) in the N and B groups, while the C group walked with no stimulation.
Results: In contrast to the C group, there was a significant decrease in mean Borg score in the second
bout of exercise in the 2 groups B+N (4.63 ±1.62 vs. 3.44 ±1.61, p<0.005). There was no influence of the
site of stimulation (B vs. N).
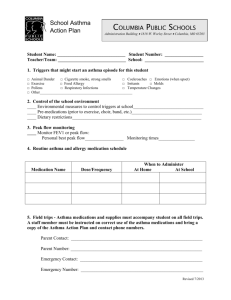
10
BORG
SCALE
8
6
4
2
W
Walk 1
W
2
1
0
Walk 2
Figure 1: Walk 1 without the TENS. Walk 2 with the TENS activated. BORG
scale 0-10 (0 meaning no dyspnea while 10 meaning maximum dyspnea.)
Conclusions: It is concluded that cutaneous stimulation involving large myelinated fibers significantly
reduces the level of dyspnea in patients with obstructive lung disease regardless of the region stimulated.
25
Heart rate variability biofeedback to reduce craving during treatment for substance use
disorders
David Eddie, MS daveddie@scarletmail.rutgers.edu [daveddie@scarletmail.rutgers.edu]
Chrys Kim, PsyD, Paul Lehrer, PhD, Erin Deneke, PhD., Marsha E. Bates, PhD
Rutgers – The State University of New Jersey, Piscataway, NJ, USA
Objectives: The present pilot study investigated the implementation feasibility, and efficacy for reducing
alcohol and drug craving, of a brief, 3-session heart rate variability biofeedback (HRV BFB) intervention
added to a traditional 28-day alcohol and drug use disorder inpatient treatment program.
Methods: Forty-eight young adult men received either treatment as usual (TAU) plus three sessions of
HRV BFB training over three weeks, or TAU only. Participants receiving HRV BFB training were instructed
to practice daily using a hand-held HRV BFB device.
Results: HRV BFB training was well tolerated by participants and supported by treatment staff.
Participants receiving TAU + HRV BFB demonstrated a greater, medium effect size reduction in alcohol
and drug craving compared to those receiving TAU only, although this difference did not reach statistical
significance. Hierarchical regression analyses of residual craving change scores yielded significant group
by HRV interaction effects wherein baseline levels of HRV were predictive of changes in craving only in
the TAU group: Lower baseline levels of HRV were associated with increases in craving from start to end
of treatment, whereas higher baseline HRV levels were associated with greater decreases in craving by
the end of treatment. In the TAU + HRV BFB group, however, there was no such association. That is, HRV
BFB appeared to dissociate individual differences in baseline HRV levels from changes in craving.
Conclusions and Implications: Given that alcohol and drug craving often precipitate relapse, HRV BFB
merits further study as an adjunct treatment to ameliorate craving experienced by persons with alcohol
and drug use disorders.
26
Rhinitis symptoms and asthma control in urban children with asthma and allergic rhinitis
Robin S. Everhart, PhD,1 reverhart@vcu.edu
Sheryl J. Kopel, MSc,2 Cynthia A. Esteban, MSN, MPH, 2 Elizabeth L. McQuaid, PhD,2 Gregory Fritz, MD,2
Robert Klein, MD,2 & Daphne Koinis-Mitchell, PhD2
1 Virginia
Commonwealth University, Department of Psychology, Richmond, VA USA,
Children’s Research Center, Alpert Medical School, Brown University, Providence, RI USA
2 Bradley/Hasbro
Background: Asthma and allergic rhinitis (AR) are common, comorbid conditions in children. Rhinitis
symptoms have the potential to exacerbate asthma in children and interfere with children’s daily
functioning. Limited research has considered the effect of rhinitis symptoms on asthma control among
urban children with asthma and AR from diverse backgrounds.
Methods: Study participants included 227 children with asthma and AR (ages 7 to 9) and their caregivers
from African American (32% of families), Latino (51%), and non-Latino white (NLW; 17%) backgrounds.
Caregivers and children completed interview-based assessments and a clinician evaluation, as well as
three, 4-week periods of daily monitoring to track asthma and rhinitis symptoms across one academic
year.
Results: The mean proportion of days with rhinitis symptoms was higher in children with poorly controlled
asthma (Asthma Control Test scores ≤ 19) as compared to children with well controlled asthma
(t(225)=2.49, p=.014). Within groups, days with rhinitis symptoms differed across asthma control in
African American children (t(74)=2.29, p=.025); African American children with poorly controlled asthma
had higher symptom days (M=.31, SD=.24) as compared to children with well controlled asthma (M=.20
days, SD=.19). Level of asthma control also differed in children of the sample based on their level of
rhinitis symptoms. Children above the mean number of rhinitis symptom days had a lower level of asthma
control (M=19.34, SD=4.28) than children with fewer rhinitis symptoms (M=20.36, SD=2.54; t(225)=2.45,
p=.015).
Discussion: Findings suggest that rhinitis symptoms may worsen asthma control among urban children
with both asthma and AR. In particular, African American children with poorly controlled asthma in this
sample experienced increased rhinitis symptoms. Clinicians may wish to highlight the importance of
treating rhinitis symptoms in conjunction with asthma during recommendations to urban caregivers of
children with both asthma and AR.
27
Psychological treatment of comorbid asthma and panic disorder in Latino adults: Results
from a randomized controlled pilot study
Jonathan M. Feldman, PhD1 JFeldman@aecom.yu.edu
Lynne Matte, PhD,1 Alejandro Interian, Ph.D,2 Paul M. Lehrer, Ph.D,3 Bari Scheckner, MA,1 Dara Steinberg,
PhD,1 Shou-En Lu, Ph.D,4 Anu Kotay, PhD,5 Sumita Sinha, MD,5 Chang Shim, MD6
1Ferkauf
Graduate School of Psychology, Yeshiva University 2VA New Jersey Healthcare System 3Rutgers Robert Wood Johnson Medical School University 4Rutgers -Environmental and Occupational Health
Sciences Institute 5 Montefiore Medical Center/Albert Einstein College of Medicine 6 Jacobi Medical
Center/Albert Einstein College of Medicine
Background: Confusion between panic and asthma symptoms can result in serious errors in selfmanagement of both disorders. An intervention was designed with the following elements:
differentiation between panic and asthma symptoms, cognitive behavioral therapy (CBT) for panic
disorder (PD), asthma education, and heart rate variability biofeedback. This treatment was culturally
adapted for Latino participants. The purpose of this study was to examine the preliminary efficacy of this
intervention compared with music and relaxation therapy (MRT), which included paced breathing at
resting respiration rates.
Methods: The sample consisted of 53 Latino adults with asthma and PD between the ages of 19 to 68
years old (M = 43.4 ± 12.9). Puerto Rican participants comprised the main ethnic group (81.1%).
Participants were recruited from outpatient clinics at hospitals in the Bronx, NY. PD was assessed with the
Structured Clinical Interview for DSM-IV. Participants were randomly assigned to either the CBT or MRT
group for 8 weekly sessions. The Panic Disorder Severity Scale (PDSS), the Clinical Global Impression (CGI),
and the Asthma Control Questionnaire (ACQ) were administered by an interviewer, who was blind to
treatment condition.
Results: Approximately half of the participants in both the CBT (n = 16) and MRT (n = 16) groups were
treatment responders on the CGI at 3 month follow-up (CBT = 56.2%, MRT = 50.0%). Participants showed
improvements on the PDSS from baseline (CBT = 2.2, MRT = 2.4) to 3-month follow-up (CBT = 1.3, MRT =
1.5) and the ACQ (CBT and MRT = 25% increase in well controlled) in both groups. No between group
difference was found between CBT and MRT on panic or asthma control. The attrition rate was high in
both groups (CBT = 41%, MRT = 38%).
Conclusions: Both CBT and MRT may be efficacious treatments for comorbid asthma-PD, although
additional research is needed due to the small sample size, high attrition rate, and lack of between-group
differences on preliminary analyses.
28
Psychological and physiological effects of exposure to inhaled environmental toxins and
irritants
Nancy Fiedler, PhD nfiedler@eohsi.rutgers.edu
Environmental and Health Sciences Institute, Rutgers – The State University of New Jersey, Piscataway, NJ,
USA
Background: Respiratory symptoms such as shortness of breath and chest tightness are common
symptoms among community-dwelling individuals exposed to inhaled environmental toxins even at
concentrations not expected to produce respiratory distress. Discerning a dose response relationship
among chemical exposures, respiratory symptoms, and objective measures of respiratory function
requires precise measurement of chemical exposure conditions in conjunction with assessment of
respiratory function which can most effectively be accomplished with controlled exposures.
Methods: Our controlled exposure laboratory at the Rutgers Environmental and Occupational Health
Sciences Institute has conducted controlled exposures to methyl tertiary butyl ether (MTBE) (N= 12
MTBE sensitives; 19 healthy controls), hydrogen sulfide (N= 74 healthy subjects), diesel vapors (N= 12 ill,
19 healthy Gulf war veterans), and mixtures of volatile organic compounds (N= 130 healthy female
subjects) at environmentally relevant concentrations. In repeated measures designs, symptom
questionnaires, psychophysiologic responses relevant to the exposures, and computerized tests of
cognitive function are administered at baseline prior to exposure onset, at several points during exposure,
and immediately following exposure. After controlling for baseline responses at each exposure session,
subject responses during filtered air or low exposure conditions are compared to health effects assessed
during and after exposure to increasing concentrations of the toxicant.
Results: Odor unpleasantness, anxiety, cognitive and respiratory symptoms were significantly increased
immediately following the onset of exposure to hydrogen sulfide and diesel vapors. Immediately
following exposure to diesel vapors, veterans diagnosed with Gulf war illness exhibited greater
respiratory variability, systolic blood pressure, and a significant decline in end-tidal CO2 relative to healthy
Gulf war controls, indicating a hyperventilation response to exposure. Relative to controls, ill Gulf War
veterans also exhibited hyporeactivity in response to a computerized task of vigilance. Relative to filtered
air, exposure to VOC mixtures with or without ozone among healthy female subjects did not result in
significantly different symptoms, reduced cognitive performance or changes in lung function. Although
individuals reporting sensitivity to MTBE reported significantly greater total symptoms than healthy
controls during the highest exposure condition (15% MTBE), no differences in respiration rate or other
psychophysiologic responses were observed.
Conclusion: Although respiratory symptoms are frequently reported in response to chemical exposures,
changes in respiratory function are not demonstrated among otherwise healthy individuals. In our
laboratory, the most compelling respiratory effect was observed among subjects who were chronically ill
and this effect was associated with hyperventilation and anxiety. Future studies of responses among
individuals at risk for respiratory symptoms such as asthmatics may be more fruitful in understanding
community responses to chemical exposures.
29
A pilot study of brief heart rate variability biofeedback to reduce craving in
young adult men receiving inpatient treatment for substance use disorders
David Eddie, M.S.
Chrys Kim, PsyD,1 Paul Lehrer, PhD, 1 Erin Deneke, PhD, 2 Marsha E. Bates, PhD1
1Rutgers
2
– The State University of New Jersey, Piscataway, NJ, USA
Caron Treatment Centers, Wernersville PA, USA
Objectives: The present pilot study investigated the implementation feasibility, and efficacy for reducing
alcohol and drug craving, of a brief, 3-session heart rate variability biofeedback (HRV BFB) intervention
added to a traditional 28-day alcohol and drug use disorder inpatient treatment program.
Methods: Forty-eight young adult men received either treatment as usual (TAU) plus three sessions of
HRV BFB training over three weeks, or TAU only. Participants receiving HRV BFB training were instructed
to practice daily using a hand-held HRV BFB device.
Results: HRV BFB training was well tolerated by participants and supported by treatment staff.
Participants receiving TAU + HRV BFB demonstrated a greater, medium effect size reduction in alcohol
and drug craving compared to those receiving TAU only, although this difference did not reach statistical
significance. Hierarchical regression analyses of residual craving change scores yielded significant group
by HRV interaction effects wherein baseline levels of HRV were predictive of changes in craving only in
the TAU group: Lower baseline levels of HRV were associated with increases in craving from start to end
of treatment, whereas higher baseline HRV levels were associated with greater decreases in craving by
the end of treatment. In the TAU + HRV BFB group, however, there was no such association. That is, HRV
BFB appeared to dissociate individual differences in baseline HRV levels from changes in craving.
Conclusions and Implications: Given that alcohol and drug craving often precipitate relapse, HRV BFB
merits further study as an adjunct treatment to ameliorate craving experienced by persons with alcohol
and drug use disorders.
30
The effect of slow diaphragmatic breathing on heart beat event related potentials (HEPs)
Richard Gevirtz, PhD rgevirtz@alliant.edu
California School for Professional Psychology,San Diego, CA, USA
Background. Recent reviews have shown that biofeeedback techniques that use slow abdominal
breathing can reduce anxiety and depression to a greater extent than relaxation interventions. Although a
number of mechanisms may mediate this effect, based on recent findings using an implanted vagal nerve
stimulator, a likely candidate is vagal afferent activity into the NTS and projected to Broadman area 25.
Methods. To test this hypothesis, we have conducted studies that look at the effect of various maneuvers
on the heartbeat evoked potential (HEP). The HEP is an event-related EEG response that is triggered by
the R-wave of the ECG. The results of two studies are presented that demonstrate that the HEP is
affected by both short term and long term slow breathing interventions.
Discussion. We speculate that this effect is mediated by the vagal afferent pathway.
31
Activation of chemosensors in the lung stimulates breathing
Juan Guardiola, MD, Jerry Yu, BM, PhD jerry.yu@louisville.edu
Robely Rex VA Medical Center and Pulmonary Medicine, University of Louisville, Louisville, KY, USA
Background: Breathing pattern is under the control of the central nervous system (CNS), which is
regulated by feedback information in the lung via the vagus nerve (Lee and Yu, 2014; Comprehensive
Physiol 4:287-324). Hyperpnea and tachypnea are common respiratory pattern in a variety of pulmonary
diseases such as asthma, pneumonia, chronic obstructive pulmonary disease, pulmonary embolism, adult
respiratory distress syndrome, and left heart failure. Therefore, we hypothesize that chemical mediators
released into the lung during pulmonary diseases stimulate chemosensitive afferents (chemosensors) in
the vagus nerve, which in turn alters the CNS activity and then breathing pattern.
Methods: To test this hypothesis, we examined neural activities of vagal chemosensors (unmyelinated
(histamine, bradykinin, and 5-HT), cytokines (TNF-α and IL-1β), and chemosensor activators (H2O2,
hypertonic saline and oleic acid) in open-chest and mechanically-ventilated rabbits. In a separate group of
rabbits, we examined respiratory pattern (assessed from the integrated phrenic efferent neurogram) in
response to the stimulating agents.
Results: We found that these testing agents stimulated chemosensitive afferents vigorously. Furthermore,
these agents stimulated breathing. For example, injection of hypertonic saline (0.1 ml 8.1% NaCl) or H2O2
rate (61±10% and 43±8%, respectively, n=30) of phrenic neuroengram, indicating hyperpnea and
tachypnea. This chemically mediated hyperpnea and tachypnea disappeared after bilateral vagotomy.
Discussion: Our results support that chemosensors in the vagus nerve is a common pathway for lung-brain
communication during pulmonary diseases. Since hyperpnea and tachypnea cause hyperventilation,
which increases work of breathing therefore promotes ventilatory failure during pulmonary diaseases,
activation of chemosensors could be detrimental.
32
Respiratory disease and executive functioning among adults in the United States
Alice Grinberg, MA, EdM 1 alice.grinberg@gmail.com
Renee Goodwin, PhD, MPH 1, 2
1 Department
of Psychology, City University of New York (CUNY), Flushing, New York,
11367, USA
2 Department of Epidemiology, Mailman School of Public Health, New York, New York, USA
Background: The goal of the current study was to investigate the relationship between
respiratory disease and impairments in neuropsychological functioning among adults in the
United States.
Method: Data were drawn from the Midlife Development of the United States (MIDUS), a
nationally-representative survey of adults in the United States (N=3259). Ordinary least squares
were used to estimate the relationship between respiratory disease and various
neuropsychological measures. Analyses were run separately for adults below and at/above the
age of 50, adjusting for demographic characteristics and various measures of physical and mental health,
including body mass index (BMI), history of a heart attack, stroke, or diabetes, history of smoking
cigarettes, a current diagnosis of Major Depressive Disorder (MDD), and ratings on a self-reported
measure of quality of life (i.e., Activities of Daily Living).
Results: After controlling for demographic characteristics and health status, respiratory disease
was associated with significant declines in executive functioning compared to those without
respiratory disease. Adults with respiratory disease 50 years and older were at significantly
greater risk for executive decline than those 50 years and older without respiratory disease. There was no
association among adults younger than 50 years old.
Discussion: Adults with respiratory disease may be at increased risk for declines in executive
functioning later in life. If these findings are replicated, screening and preventive interventions
aimed at preventing cognitive decline in people with respiratory disease may be advantageous
33
The effect of expiratory muscle strength training (EMST) on urge-to-cough in stroke
patients
Karen W. Hegland, PhD/CCC-SLP 1 kwheeler@ufl.edu
Michelle S. Troche, PhD/CCC-SLP,1 Floris Singletary, MS/CCC-SLP,2 Paul W. Davenport, PhD3
1Department
of Speech, Language, and Hearing Sciences
University of Florida
2Brooks Rehabilitation Clinical Research Center
Jacksonville, FL, USA
3Department of Physiological Sciences
University of Florida
Background: Disordered swallowing following stroke is common, but typically resolves within the first
month post-stroke. However, aspiration pneumonia continues to be a leading cause of death in the 5
years post-stroke. The urge-to-cough (UtC) provides a measure of respiratory sensation related to an
irritating airway stimulus. Evidence suggests that blunted UtC ratings relate to airway protection deficits
in patients with neurologic disease. The goal of this study was to determine the effect of a respiratorybased rehabilitation paradigm on the UtC of participants post stroke.
Method Twelve participants with a history of ischemic stroke within the previous 12 months were
recruited for this study. Baseline tasks included maximum expiratory pressure (MEP) measurement and a
cough challenge to three trials of 200 μM capsaicin. Following each capsaicin presentation participants
rated the UtC on a modified Borg scale. The same measures were repeated following 5 weeks of EMST. A
repeated measures analysis of variance was used to determine whether there were significant differences
for UtC and MEP pre and post EMST.
Results: At baseline, all participants demonstrated a blunted UtC to 200 μM capsaicin when compared to
previously published data on healthy adults. Following 5 weeks of EMST, UtC increased from an average
of 2.67 to 3.95. MEP also increased by an average of 30cmH2O post training.
Discussion: The results of our study show that UtC is blunted in post-stroke patients, and that a
respiratory strength training paradigm improves both expiratory muscle strength and the UtC sensation in
response to cough inducing stimuli. This may relate to positive pressure in the upper airway and
subsequent sensory stimulation that occurs during the EMST task. This is an important finding given that
the perception of UtC is a critical component in the generation of an effective cough response to aspirate
material.
34
Let’s talk about asthma and vocal cord dysfunction
Charles Irvin, PhD Charles.irvin@uvm.edu
University of Vermont, Burlington, VT, USA
Asthma is a common chronic lung disorder for which there are well-codified diagnostic criteria and treatment
schemes. On the other hand vocal cord dysfunction (VCD) is a frequent syndrome that can be mistaken for asthma
but where the diagnostic criteria are ill defined and treatment is largely based on expert opinion. Vocal cord
dysfunction (VCD) can occur with or without asthma but in either case these patients present a difficult diagnostic
challenge. Failure to recognize VCD is important as it leads to unnecessary treatment and contributes to patient
morbidity. The neural control and innervation of the larynx is complex and multiple factors have been identified
that lead to abnormal adduction and airflow limitation. Unfortunately, the literature on this disorder is largely
made up of small studies and anecdotal communications. Diagnosis is difficult and little agreement exists as to the
best approach. Laryngoscopy is held to be the gold standard but inspiratory flow volume loops can be helpful and
are not invasive. A myriad of treatments have been proposed for VCD including drugs (e.g. racemic epipherine),
treatment of post nasal drip, GERD, botox, hypnotherapy, biofeedback but the most commonly used treatment is
speech pathology therapy. Further investigations into the causes, natural history and in particular better, validated
diagnostic approaches are needed. Assessment of treatment effectiveness is clearly necessary. Accordingly, the
causes and cures for VDC provide a rich opportunity for research.
35
The impact of harmfulness information on urge-to-cough during citric-acid inhalation.
Thomas Janssens, PhD, Thomas.Janssens@ppw.kuleuven.be
Sarah Brepoels, MA, Lieven Dupont, MD, PhD & Omer Van den Bergh, PhD
KU Leuven (University of Leuven), Belgium
Background: The cough reflex is an automatic reflex, but it can be modulated by a conscious effort to
augment or suppress cough. Furthermore, evidence is emerging that cough reflexes are modulated by
other forms of top-down cortical control. In this experiment, we investigated the role of perceived
harmfulness on cough reflex sensitivity. Due to the defensive nature of the cough reflex, we hypothesized
that an increase in perceived harmfulness would increase cough reflex sensitivity and associated urge-tocough.
Methods: Healthy participants (n=39) Received information that the substance they were to inhale was
harmless (natural citric acid), or potentially harmful (a potent agrochemical). Subsequently, they
participated in a two-step cough challenge test, using dosimeter controlled citric acid inhalations. First,
the dose eliciting at least three coughs (C3) was determined. Subsequently, participants received
repeated presentations of the C3 dose, a subthreshold dose of citric acid and placebo.
Results: C3 thresholds were not influenced by harmfulness information, but only 27/39 participants
reached C3. During repeated citric acid presentations, the group that received information that the cough
inducing substance was a potentially harmful chemical showed a greater urge-to-cough compared to the
group that was told that the cough-inducing substance was natural citric acid (F(1,24) = 10.15, p < .01).
Cough frequency was not influenced by the harmfulness information.
Conclusion: Our findings show that harmfulness information is an important factor in the perception of
urge-to-cough and suggests that a reduction of perceived harmfulness may be a beneficial symptom relief
strategy in individuals that suffer from an increased urge-to-cough.
36
Prevalence of anti-inflammatory medication use in asthma patients
Karenjot Kaur1 karenjot.kaur@rutgers.edu,
Milisyaris Aviles, MS,2 Varsha Kurup,1 Frederick Wamboldt, MD,3 Shou-En Lu, PhD,4 Paul Lehrer, PhD5
1 Rutgers
– The State University of New Jersey, New Brunswick, NJ, USA
Department of Psychiatry, Rutgers -- Robert Wood Johnson Medical School, Piscataway, NJ, USA
3National Jewish Health, Denver, CO, USA
4 School of Public Health, Rutgers – The State University of New Jersey
2
Background. Asthma is an inflammatory disease which causes heightened airway irritability, and has
intermittent symptoms precipitated by viral infections, cold air, exercise, pollutants, and psychological
stress. The National Institute for Health recommends the use of Albuterol, inhaled steroids, and oral
steroids for asthma control. Literature suggests that 50% of asthma patients do not use inhaled steroids
as recommended. This study sought to recruit these patients in order to give them an alternative to the
use of inhaled steroids despite having asthma exacerbations.
Methods. The patients were recruited through posters, advertisements, and medical referrals which
emphasized the need for non-smoking and non-steroid using patients. Information on patients’ asthma
was collected through surveys, questionnaires, and physiological testing.
Results. A large percentage of subjects was excluded from the study for not meeting criteria; exclusion
rates were high. The excluded subjects’ responses in the collected data were analyzed to determine the
major exclusion criteria. A sample of 530 self-proclaimed, non-smoking adult asthma patients, who were
excluded from the study (50 were included), was used in this assessment. Through data observation, it
was found that approximately 20% of these subjects, were either currently or previously heavy smokers.
Other patients were excluded for having very mild asthma symptoms, or only seasonal symptoms. A
majority of excluded subjects, approximately 30%, were using inhaled steroids, despite the study
advertising the need for non-users.
Discussion. We verified that smoking is a hindrance in asthma prevention and treatment and found that
more individuals use inhaled steroids than suggested by the literature. This recommended use of inhaled
steroids may have been due to geographic location, with several of the Central New Jersey subjects
having easy access to medical care and drugs. These subjects may also have been less afraid of the side
effects of inhaled steroids, suggesting their increased medical access and availability.
37
Breath, beats, and behavior: applied psychophysiology, stress management, and
behavioral medicine
Paul Lehrer, PhD Lehrer@rwjms.rutgers.edu
Rutgers – Robert Wood Johnson Medical School, Piscataway, NJ, USA
This talk reviews 45 years of psychophysiological research at Rutgers, and related research from around
the world.
Stress can produce dysregulation in various body systems. We review research on various forms of
stress-related autonomic dysfunction, including parasympathetic as well as sympathetic overactivity and
symptomatology.
Changes in various parameters of respiration are important for normal regulation. They typically occur
during exposure to stress. These include changes in bronchial tone, tidal volume, respiratory drive, and
total ventilation. They often occur in the form of yawning and sighing. In normal function, respiratory
changes aid in regulating acid base balance in the blood and adaption to exercise, altitude, air pollution,
and changes in respiratory resistance. They also may affect autonomic regulation. Data on laboratory
stressors are reviewed. Stress-related respiratory changes often produce a mismatch between physical
demand for oxygen and respiration. Such effects can lead to respiratory dysregulation, and produce a
host of physical and emotional symptoms, often mediated by hyperventilation. These may include
headache, dyspnea, chest pain, muscle tension, performance decrements, confusion, and panic.
Breathing slowly at about six breaths/min is a therapeutic intervention that may have powerful effects in
combatting various sources of respiratory dysregulation. It protects against hyperventilation while
maintaining oxygen saturation, prevents asthma exacerbations, and, through its effects on the baroreflex
system, improves cardiovascular and emotional regulation. Yogis and Sherpas are often observed to
breathe with this pattern, as do Zen monks. Data from a current trial suggest that it decreases airway
reactivity to methacholine among asthma patients. It targets the parasympathetic system, and appears to
stimulate parasympathetic regulatory components in cardiovascular regulation. These effects appear to
be maximized when heart rate variability biofeedback is included as a way to teach optimal patterns of
slow breathing, where resonance characteristics of the baroreflex system are stimulated, and gas
exchange is maximized. Combinations of psychophysiological techniques may be particularly helpful for
patients with multiple somatic symptoms and a pattern of somatization.
38
Heart rate variability biofeedback: its role in asthma therapeutics
Paul Lehrer, PhD1 Lehrer@rwjms.rutgers.edu
Frederick Wamboldt, MD,2 Evgeny Vaschillo, PhD,3 Charles Irvin, PhD,4 Milisyaris Aviles, MS,1 Jessica
Graves, MA,2 Shou-En Lu, PhD5
1Department
of Psychiatry, Rutgers – Robert Wood Johnson Medical School, Piscataway, NJ, USA
Jewish Health, Denver, CO, USA
3Center for Alcohol Studies, Rutgers – The State University of New Jersey, Piscataway, NJ, USA
4University of Vermont, Burlington, VT, USA
5School of Public Health, Rutgers – The State University of New Jersey
2National
Background. Previous research found the heart rate variability biofeedback (HRVB) allowed decreases in
asthma medication, while producing improved pulmonary function, a reduction in asthma symptoms, and
a complete elimination of asthma exacerbations. However, no mediators for this effect were found.
Method. In the current study we tested the effects of biofeedback on airway reactivity to methacholine
and exhaled nitric oxide, to determine whether the pathway may be autonomic or anti-inflammatory, and
whether HRVB can be used as a substitute or complement to steroid medication. We also assessed effects
of treatment on HF, LF, and VLF HRV, as well as these frequency ranges in pulse transit time and pulse
amplitude, as indirect measures of vascular tone effects.
Results. Here we present preliminary data on partial results from this two center trial.
Fifty-five steroid-naïve adult patients with mild or moderate asthma were given either HRVB or a
relaxation control, involving EEG alpha biofeedback, paced breathing at 15 breaths/min, and listening to
relaxing music. Although we thus far have not found significant effects on resting levels of pulmonary
function, we found a significant improvement on the methacholine challenge test only for the HRVB
group. We also found a significant increase in LF and VLF pulse transit time variability, as well as a
decrease in finger pulse amplitude, and increases in LF HRV. No effects were found for exhaled nitric
oxide.
Discussion. The results suggest that HRVB may be useful as a supplement to steroids, but not as a
substitute. The decrease in reactivity to methacholine suggests modulation of reactivity of airway smooth
muscles by increased baroreflex strength, a known effect of HRVB. The autonomic effects suggest
increased baroreflex activity in both the heart rate and vascular tone closed loops of the baroreflex
system.
39
Nicotine withdrawal severity moderates the relation between panic disorder status and physiological stress
reactivity
Teresa M. Leyro, Ph.D. 1 teresa.leyro@rutgers.edu
Michael J. Zvolensky, Ph.D. 2
1
Rutgers – The State University of New Jersey, Piscataway, NJ, USA
University of Houston, Houston, TX, USA
2
Background: Smoking onset is significantly and prospectively linked to the development of Panic Disorder (PD),
placing these individuals at greater risk for more intense panic-relevant psychopathology and poorer smokingrelated outcomes. Nicotine withdrawal is one mechanism that may explain this relationship; for example, smokers
with PD may over-attend to somatic sensations associated with nicotine withdrawal and may misinterpret them as
threatening. We examined whether nicotine withdrawal moderates the relation between PD and panic reactivity
via assessment of expired tidal levels of CO2 (ETCO2) to a laboratory challenge.
Method: Using a between-subjects design, 58 nicotine-dependent smokers with and without PD were randomly
assigned to refrain from smoking for at least 12 hours, or to smoke as usual, prior to participating in a 4-minute
10% carbon dioxide-enriched air (CO2) biological challenge, during which ETCO2 was continually indexed.
Results: Participants were 58 adult smokers (M =19.7 cigarettes daily, SD = 8.0), and 36.2% met criteria for current
PD. Self-reported nicotine withdrawal and PD status (via diagnostic interview) did not interact to predict pre- to
post-challenge change in ETCO2. However, higher levels of nicotine withdrawal and positive PD status interacted to
predict greater physiological reactivity to the challenge as indexed by ETCO2 levels measures in response to, and
recovery from, the challenge over time (Time2 x PD status x nicotine withdrawal: t=-2.08, p<.05).
Discussion: The current findings are the first to experimentally demonstrate that greater self-reported nicotine
withdrawal interacts with PD status to predict greater physiological reactivity to, and slower recovery, from a CO2
laboratory stress provocation, as indexed via ETCO2. These findings suggest subjective nicotine withdrawal severity
may exacerbate physiological panic reactivity in smokers with panic psychopathology. In addition, they suggest the
need for further inquiry into physiologically relevant clinical intervention targets, such as ETCO2, for the treatment
of smokers with co-occurring panic psychopathology.
40
Effects of heart rate variability biofeedback on airway inflammation
Patrick Maulion1, pdm62@scarletmail.rutgers.edu
Milisyaris Aviles, MS,1 Jessica Graves, MA,2 Frederick Wamboldt, MD,2 Shou-En Lu, PhD,1 Paul Lehrer,
PhD1
1Rutgers – The State University of New Jersey, Piscataway, NJ, USA
2National Jewish Health, Denver, CO
Background: An underlying process in asthma is considered to be airway inflammation that increases
airway irritability. Most asthma patients are therefore treated with anti-inflammatory drugs, primarily
inhaled steroids, which are taken as ‘controller’ medications, to prevent exacerbations, even when the
patient is asymptomatic. However a large proportion of asthma patients are nonadherent to steroid
treatment, primarily because of cost and fear of side effects. Heart Rate Variability Biofeedback (HRV-BF)
is a non-pharmacological breathing therapy in which individuals are instructed to breathe at the rate
determined by the resonance frequency of the baroreflex system, approximately 6 times a minute.
Previous studies showed that HRV-BF improves airway function, decreases symptoms, allows less
medication use, and prevents asthma exacerbations. The goal of this study was to see if HRV-BF
decreases airway inflammation as measured by fractional exhaled nitric oxide (eNO).
Methods: This is an interim analysis of a two-center clinical trial that is still ongoing. The study included
80 steroid naïve patients who were randomized into either HRV-BF (N = 36) or a combination of EEG
biofeedback, paced breathing at a relaxed rate (~15 breaths/minute), and listening to relaxing musicrelaxation (N = 44). After a one-month run-in with asthma education, patients were given 6=10 sessions
of training. Measures of eNO were taken at pre, mid and post treatment. The Aerocrine NIOX MINO
System was used, following the manufacturer’s protocol. Data were analyzed using an ANOVA with a
repeated measures design, through the SAS GLM program. The log transformation was used on parts per
billion (ppb) eNO in order to normalize data.
Results: Neither group showed a significant change in log eNO during the study, with no differences
between groups.
Means and s.d.’s of log eNO
Group
HRV-BF
Music EEG
Beginning of Tx
3.50 ± 0.76
3.80 ± 0.91
Mid Tx
3.52 ± 0.86
3.68 ± 0.91
End of Tx
3.60 ± 0.75
3.73 ± 0.93
Discussion: HRV-BF did not have a significant impact on eNO. Although other data show that HRV-BF has
a potential for treating asthma, the path does not appear to be through decreasing airway inflammation.
HRV-BF may thus function as a complement to treatment with inhaled steroids, not as an alternative.
41
Psychiatric symptoms, bronchodilator response, and symptom magnification in Latino
children with asthma
Elizabeth L. McQuaid, PhD1, elizabeth_mcquaid@brown.edu
Nicole R. Nugent, PhD,1 Daphne Koinis-Mitchell, PhD,1 Ronald Seifer, PhD,1 Glorisa Canino, PhD,2 Gregory
K. Fritz, MD1
1Bradley/Hasbro
2Behavioral
Children’s Research Center, Alpert Medical School, Brown University, Providence, RI.
Sciences Research Institute, University of Puerto Rico, Medical Sciences Campus, San Juan, PR
Background: Stress and psychiatric symptoms may affect bronchodilator responsivity (BDR) in asthma,
particularly among Latinos. Our prior data suggest that Latino children with asthma are more likely to
overestimate lung function compromise (symptom magnification; SM). In this study, we investigate
symptoms of anxiety and panic, and their relationship to BDR and SM among Latino children with asthma.
Methods: 382 Latino children with asthma (ages 7-15) living in PR (n=242) and RI (n = 140; 59 PR and 81
DR) completed the BDR protocol involving pre-post bronchodilator reversibility. BDR was defined as:
([post-bronchodilator FEV1 – pre-bronchodilator FEV1]/pre-bronchodilator FEV1) x 100. A subset of 246
children also completed five weeks of our standard symptom perception protocol involving serial
subjective and objective lung function assessments. The degree of SM for each child was quantified using
our Asthma Risk Grid. The DISC Predictive Scales, Youth Report (Y-DPS) were used to assess symptoms of
anxiety and panic. Multivariate modeling was used to examine anxiety and panic symptoms in relation to
BDR and SM, controlling for age, gender, smoke exposure, income, and site.
Results: Controlling for relevant covariates, children with significant symptoms of panic and anxiety had a
reduction in BDR of 2.0% (p < .05) compared to those without symptoms. Multivariate analyses did not
reveal associations between anxiety or panic and SM; however, covariates of child sex, site, and income
remained predictors of SM.
Discussion: In our sample of Latino children, psychological symptoms had modest associations with
impaired BDR, but not with SM. Factors associated with chronic disadvantage, many of which occur in
combination, likely contribute to symptom perception in this group.
42
Pilot study of hypoventilation treatment on anxiety in patients with asthma
Alicia E. Meuret, PhD1, ameuret@mail.smu.edu
David Rosenfield, PhD,1 Ashton M. Steele, MA,1 Mark. M. Millard, MD,2 Thomas Ritz, PhD1
1Southern
2Baylor
Methodist University, Dallas, Texas, USA
University Medical Center, Dallas, Texas, USA
Background: There is a high prevalence of anxiety in patients with asthma. Research suggests that anxiety
exacerbate asthma symptoms and health care utilization and, conversely, asthma symptoms and
medication may complicate anxiety treatment. Effective, non-pharmacological interventions to improve
anxiety in asthma are needed. A marker common to both is hyperventilation which has been linked to
adverse effects on lung function, symptoms, and well-being in asthma and fear in anxiety sufferers. We
determined whether reducing hyperventilation improves anxiety in patients with comorbid anxiety and
asthma.
Methods: 120 adult patients with asthma, aged 20-65, English- or Spanish-speaking, were enrolled in an
NIH-funded 4-week, 5 session training. Patients were randomly-assigned to receive capnometry-assisted
respiratory training (CART) for raising PCO2 or feedback in slowing of respiratory rate (SLOW) to improve
asthma symptoms and lung function. Anxiety was not directly targeted.
Results: Twenty-six patients met criteria for clinically relevant anxiety levels (HADS, anxious mood ≥8).
Anxiety symptoms (measured by ASI, PANAS negative items, and HADS-A) were substantially reduced in
the high anxiety patients receiving CART (effect size d=1.30 for ASI, d=.52 for PANAS, and d=.62 for HADSA), while they remained stable in the SLOW condition. Further, the Anxiety by Treatment by Time
interactions were significant for all three anxiety outcomes (ps<.05), with the advantage of CART over
SLOW on improvement in anxiety being greater for high than for low anxiety patients. In addition, while
high anxiety participants in the SLOW condition had decreasing quality of life over the course of the study,
high anxiety participants in CART maintained their quality of life over time, and were equivalent to the
low anxiety patients.
Conclusions: Brief training in reducing overbreathing by means of raising PCO2 led to significant and
sustained reductions in both asthma and anxiety symptoms. The findings lend support for PCO 2 as a
critical factor for anxiety reduction in asthma.
43
Management of psychological comorbidities in females with copd in a rural healthcare
setting
Sarah Miller, PhD, RN1 sarahmilleruf@gmail.com
Erin Silverman, PhD2, 3, 4, Belinda Fleming, PhD, ARNP1
1
University of Memphis, Memphis, TN;
of Physiological Sciences, University of Florida, Gainesville, FL
3North Florida South Georgia Veteran’s Health System, Malcom Randall VAMC
4Rehabilitation Outcomes Research Center – Malcom Randall VAMC, Gainesville, FL
2Department
Background & Purpose. The purpose of this study was to investigate the management of, factors related
to, and prevalence of psychological comorbidities in adults with chronic obstructive pulmonary disease
(COPD) in a rural healthcare setting.
Methods. A retrospective chart analysis of all adults with a COPD diagnosis (ICD 496.0) seen within a rural
setting from December 1, 2010 to May 31, 2010 was utilized. A total of 232 charts were randomly
selected for complete analysis. The following variables were examined: gender; presence of psychological
comorbidity diagnoses (anxiety, depression); physiological comorbidities; the number of controller
breathing medications, anxiolytics, and antidepressants prescribed; access to healthcare and insurance;
smoking history; BMI; age; FEV1% of predicted; and FEV1/FVC% of predicted.
Results Females were more likely (p=<.001) to have a current psychological comorbidity and related
prescription. However, there was no screening process, and medical management was responsive rather
than preventative or supportive. Females reported psychological manifestations while reporting their
chief complaint, but males did not. FEV1% and FEV1/FVC% of predicted scores were associated with the
presence of anxiety & depression. The majority of patients (92%) had a physiological comorbidity, of
which hypertension (81.8%), diabetes mellitus (43%) and congestive heart failure (32%) were most
prevalent. The presence of a physiological comorbidity was related to the presence of a psychological
comorbidity. There were no significant relationships in healthcare access and psychological comorbidity
diagnosis, but patients with self-pay (no insurance) were less likely to comply with spirometry orders.
Discussion & Clinical Implications In clinical practice, early screening and psychological evaluation will
identify women with COPD who are at higher risk for anxiety and depression. Females with COPD
demonstrate increased physical and psychological burden from their disease, yet there is no specialized
treatment plan to screen and address this population. NICE guideline 91 highlights the importance of
early identification of patients with a chronic health condition, such as COPD, who are at increased risk for
depression and functional impairment (NICE, 2014). The guidelines address disease-associated mood
fluctuations, loss of pleasure in activities, pain, functional impairment and disability that can increase the
risk of depression and anxiety. Early recognition, supportive care and treatment can ease the burden of
psychological comorbidities in patients with COPD. This presentation will compare and contrast existing
recommendations for patient management with new recommendations based upon this current data.
44
The relationship between heart rate variability, depression, and anxiety: baseline
findings from a randomized controlled trial of a panic disorder intervention for latino
adults with asthma
Tanya Oken, BA.1 okentt@gmail.com
Jonathan M. Feldman, PhD,1 Paul Lehrer, PhD2
1Ferkauf Graduate School of Psychology, Yeshiva University, Bronx, NY, USA
2Rutgers – The State University of New Jersey, Piscataway, NJ, USA
Background: Reduced HRV is implicated in mood and anxiety disorders. The aim of this study is to explore
the relationship between depression and panic disorder (PD) on HRV in asthmatics.
Methods: Psychiatric diagnoses were determined by structured clinical interview (SCID). Baseline
psychophysiological recordings for 46 female participants with PD and asthma were analyzed in 5-min
epochs of time. Time and Frequency bands were set according to established standards. Natural log
transformations of the LF, HF, and RMSDD index, were included as HRV outcome measures. Respiration
and participant age were included as covariates. The Beck Depression Inventory (BDI) and Panic Disorder
Severity Scale (PDSS) were used as measures of depression and PD.
Results: 47.9% (N=22) of participants met SCID criteria for a current depressive disorder. Hierarchical
regressions revealed that the BDI (M=23.48, SD=12.12) and PDSS (M=16.52, SD=4.13) were not significant
predictors of HRV as measured by log transformed LF (M=2.26, SD= .76), HF (M=2.21, SD= .88), and
RSMDD (M=1.36, SD= .40), and were excluded from analyses. Age (M=43.61, SD=12.05) and respiration
(M=16.08, SD=4.09) explained 31.1% of the variance in LF (R2 = .311, F (2, 38)=8.59, p < .01), 28.9% of the
variance in HF (R2 = .289, F (2, 38)=7.92, p < .01), and 19% of the variance in RSMDD (R2 = .19, F (2,
38)=4.47, p < .05). Age was a significant predictor of HF (β = -.45, p < .01), LF (β = -.43, p < .01), and
RSMDD (β = -.44, p < .01). Respiration significantly predicted HF (β = -.30, p < .05) and LF (β = -.53, p= .01),
but not RSMDD (β = -.03, p > .05).
Discussion: When controlling for age and respiration, the PDSS and BDI did not explain the variance in
baseline HRV for participants with PD and asthma.
45
The relationship between acculturation, asthma psychological triggers, and utilization of
quick relief medication in Mexican and Puerto Rican families
Esperanza Morales Raveendran, PhD1 esperanza.morales@nyu.edu
Kimberly Arcoleo, PhD, MPH, 2 Jonathan Feldman, PhD1
1Ferkauf
2Ohio
Graduate School of Psychology Yeshiva University; New York, USA
State University College of Nursing, Columbus, OH, USA
Objective: The present study examined the association between caregivers’ level of acculturation,
psychological triggers of asthma, and use of children’s quick relief asthma medication.
Method: 263 Mexican and Puerto Rican children between ages 5 and 12 with physician-diagnosed asthma
and their caregivers were recruited from two distinct locations: Phoenix, Arizona and the Bronx, New
York. The dyads completed structured interviews using the Stephenson Multigroup Acculturation Scale
(SMAS) and Asthma Trigger Inventory (ATI). Use of quick relief medication data were gathered by
attaching counting devices called Dosers to the child’s quick-relief metered dose inhalers.
Results: Pearson’s correlations found no significant relationships between psychological triggers of
asthma, ethnic society immersion level of acculturation, r (263)= -.06, p=.34 nor dominant society
immersion level of acculturation r (263)= -.08, p=.20. Additional Pearson’s correlation between reported
psychological triggers and use of quick relief asthma medication r (235)= .08, p=.21 revealed no significant
relationship. An independent t-test revealed no between group differences between Puerto Ricans
(M=.40, SD= .57) and Mexicans on reported psychological triggers of asthma (M= .49, SD=.63, p=.26) t(
261) =1.07. Puerto Rican caregivers scored higher on the dominant society immersion subscale (M=3.40,
SD=.44, p<.001) than Mexican caregivers (M=2.98, SD=.40, p=.90). Lastly, a hierarchical linear regression
was used to examine the proportion of variance of quick relief medication use explained by reported
psychological triggers after controlling for acculturation level. Psychological asthma triggers were not a
predictor of quick relief medication use ( =-.061, p=.36).
Discussion: Puerto Ricans caregivers have a higher level of acculturation than Mexican caregivers. There
was no relationship between reported psychological triggers, ethnicity and use of quick relief medication.
These findings are not consistent with previous research showing that acculturation may play a role in
asthma health outcomes.
46
Correcting respiratory sinus arrhythmia for respiratory influences: Findings with an
infant stress paradigm
Thomas Ritz, PhD1 tritz@mail.smu.edu
Michelle Bosquet Enlow, PhD,2 Lucy King BA,2 Stefan M. Schulz PhD3, and Rosalind J. Wright, MD, MPH4
1
Southern Methodist University, Dallas, TX, USA
Boston Children's Hospital and Harvard Medical School, Boston, MA, USA
3. University of Wuerzburg, Wuerzburg, Germany
4 Icahn School of Medicine at Mount Sinai, New York, NY, USA
2
Background. The amplitude of respiratory sinus arrhythmia (RSA) can be increased by slower and deeper
breathing independent of vagal activity. This effect is well-documented in adults and correction
procedures have been devised to control for this confound. However, less is known about the role of
respiratory pattern influences in infant RSA. We recently found evidence for the usefulness of respiratory
corrections in a smaller study using an infant stress paradigm.
Method. The present study sought to replicate these findings in a larger sample (N=181). Infants were
administered the Still Face Test, in which they are confronted with their mother terminating interaction
and maintaining a neutral face for 2 min, followed by a 2-min reunion phase with re-established
interaction. Two sequences of this test were administered unless infants became too distressed by the
first sequence. Typically, decreases in RSA would be expected during the challenge phase of the test.
However, results showed that infants’ respiration rate decreased and tidal volume increased at the same
time, which can mask the expected effects in RSA.
Results. Normalization of RSA by tidal volume and within-individual correction for respiration rate
substantially improved the demonstration of RSA attenuation during stress, for both infants completing
one and infants completing two sequences of the test.
Discussion. In conclusion, studies of infant RSA can substantially benefit from respiratory correction
procedures that control for respiration rate and tidal volume.
47
Hypoventilation training in asthma: Results from a capnometry-assisted breathing
training trial
Thomas Ritz, PhD1 tritz@mail.smu.edu
David Rosenfield, PhD,1 Ashton M. Steele, MA,1 Mark. M. Millard, MD,2 Alicia E. Meuret, PhD1*
1Southern
2Baylor
Methodist University, Dallas, Texas, USA
University Medical Center, Dallas, Texas, USA
Background. Hyperventilation has been associated with adverse effects on lung function, symptoms, and
well-being in asthma. We examined the effects of adjunctive breathing training aimed at raising end-tidal
carbon-dioxide levels (PCO2) on asthma symptoms and pathophysiology.
Method. 120 adult asthma patients were enrolled in a randomized-controlled trial to receive biofeedback
training for either raising PCO2 (capnometry-assisted respiratory training, CART) or slowing respiratory
rate (SLOW). Interventions consisted 5 sessions over 4-weeks with twice daily home training assignments.
The primary outcomes were asthma control, PCO2, and diurnal PEF variability. Secondary outcomes
included asthma symptoms, medication use, spirometric lung function, respiratory resistance, airway
inflammation, airway hyperreactivity, and quality of life.
Results. CART, but not SLOW patients achieved sustained increases in PCO2 throughout treatment and
follow-up. Significant improvements were found across most outcome measures in both groups, including
aspects of lung function and airway hyperreactivity tested by methacholine challenge. CART patients
showed lower respiratory resistance during therapy and superiority in long-term symptom reduction at 6month follow-up.
Discussion. Thus, breathing training aimed at raising PCO2 or slowing respiration rate leads to sustained
improvements in asthma symptoms and lung function. Raising PCO2 resulted in greater benefits in aspects
of lung function and long-term symptoms.
48
Asthma-Related Death of a Loved One, Panic Disorder, and Ataque de Nervios in Latino Adults with
Asthma
Jonathan M. Sandler, MA jonmsandler@gmail.com
Jonathan M. Feldman, PhD
Ferkauf Graduate School of Psychology, Yeshiva University, Bronx, New York, USA
Background: Research has demonstrated high co-occurrence of asthma and panic disorder (PD) in the
general population, as well as the role that psychosocial stressors play in such comorbidity. Yet less is
known about the relationship between asthma and the Latino culture-bound syndrome of ataque de
nervios. This study therefore investigated correlations between the self-reported death of a loved one
due to asthma and the prevalence of PD and ataque de nervios in a Latino sample of adults with asthma.
Methods: Data originated from a randomized controlled trial in which Latino adults (N = 490) were
recruited from outpatient hospital clinics in the Bronx, New York. Diagnosis of PD was determined by the
Patient Health Questionnaire (PHQ), while lifetime history of ataque de nervios was based upon selfreport. Participants were also administered the Asthma Trigger Inventory (ATI).
Results: Chi-square analysis revealed a significant association between self-reported asthma-related
death of a loved one and ataque de nervios [X2(1) = 10.6, p = .001]. Participants reporting asthma-related
deaths also scored significantly higher on the psychological trigger subscale of the ATI (M = 1.66, SD =
1.00) than did those not reporting such deaths (M = 1.40, SD = 0.98), t(428) = -2.51, p = .012, and
significantly lower on perceived ability to control ATI triggers (M = 1.45, SD = 0.91) than did those not
reporting such deaths (M = 1.64, SD = 0.91), t(413) = 2.03, p = .043. Self-reported asthma-related death of
a loved one was not associated with PD [X2(1) = 0.94, p = .33].
Discussion: These findings suggest the clinical importance of assessing for family history of asthma-related
deaths in Latino patients with asthma and ataque de nervios, as such history may negatively impact
perceived vulnerability to psychological triggers of asthma and perceived control of asthma triggers in
general.
49
Assessing differential effects of fear and anxiety to respiratory threat.
Mathias Schroijen1 Mathias.Schroijen@ppw.kuleuven.be
Simona Fantoni,1 Carmen Rivera,1 Bram Vervliet,1 Koen Schruers,1,2 Omer Van den Bergh, PhD,1 Ilse Van
Diest, PhD1
1KU
Leuven - University of Leuven, Belgium.
University, the Netherlands.
2Maastricht
Background: When respiratory sensations engage the behavioral defensive system (interoceptive threat),
it is hypothesized that two functionally distinct states, namely fear and anxiety may ensue. Each of which
are thought to play a prominent role in the etiology of panic disorder (Bouton et al., 2001). A first study
(N= 48) aimed to validate the difference between anxiety and fear towards a respiratory threat. A second
study (N= 17) aimed to explore whether fear and anxiety may differentially influence perceptual
sensitivity and response bias towards respiratory sensations.
Method: In both studies, a modified version of the NPU-threat test (Schmitz & Grillon, 2012) was used
with a respiratory aversive stimulus. Participants breathed through a tube during three experimental
conditions: a neutral condition without respiratory threat (N), a predictable (P) and an unpredictable (U)
respiratory threat condition. A breathing occlusion, making it briefly impossible to breathe, served as the
respiratory threat stimulus and was signaled by a visual signal cue in the P or unrelated to the cue in the U
condition. Startle blink responses, electrodermal activity, respiration and heart rate were measured. In
the second study, a Signal Detection Task (SDT-task) was added to this modified NPU-test. Participants
had to categorize one out of two inspiratory resistive loads as the lighter or the stronger one during each
of the three conditions (N, P, U).
Results and Discussion: The first study showed that both fear and anxiety-potentiated startle responses
were successfully elicited by predictable and unpredictable respiratory threat, respectively. Furthermore,
inter-individual differences in fear of suffocation importantly moderated the fear-potentiated, but not the
anxiety-potentiated startle. Perceptual outcomes of the SDT-task in the second study will also be
discussed
50
The effect of parental social support and acculturation on childhood asthma control
Bari Scheckner, MA1 Bari.Scheckner@psych.ferkauf.yu.edu
Kimberly Arcoleo, PhD, MPH,3 Jonathan M. Feldman, PhD1,2
1Ferkauf
Graduate School of Psychology, Yeshiva University, NY
of Epidemiology and Population Health, Albert Einstein College of Medicine, NY
3Ohio State University College of Nursing, OH
2Department
Background: There exists large ethnic disparities in asthma among Latino children; Puerto Ricans (PR) are
disproportionately affected, while Mexicans have the lowest prevalence and morbidity. Disparities are
poorly understood, however, acculturation and social support are suggested to influence asthma control
among children. This study investigated the relationship between acculturation, social support, and
asthma control among PR and Mexican children and their caregivers.
Methods: Primary caregiver-child dyads (N=267) of PR (n=79) and Mexican (n=188) descent were
recruited from clinics at two inner-city hospitals in Bronx, NY and three clinics in Phoenix, AZ. Children
were 5-12 years of age and had a confirmed asthma diagnosis. Dyads completed measures of social
support, acculturation and asthma control. Logistic regression was used for analysis.
Results: Mexican children had better asthma control than PR children (p<.001). PR caregivers were more
acculturated than Mexican caregivers (p<.05); however, acculturation did not predict control. Across
Latino subgroups caregivers’ total level of social support predicted better asthma control among children
(p<.05), and support received from family and friends each independently predicted better control
(p<.05).
Discussion: Results suggest that social support reduces some of the burden associated with asthma
management enabling caretakers to better control their children’s asthma. For example, caregivers who
perceive greater support may have greater self-efficacy regarding their ability to manage these
difficulties, and they may practically have more assistance in doing so (e.g., family/friends to babysit,
multiple sources of financial assistance). The lack of an association between acculturation and control
may be an artifact of the ethnic communities in which this study was conducted, which may limit
pressures for acculturation. Alternatively, however, research in this area is limited and existing studies
widely vary in their measurement of acculturation, making it difficult to generalize across studies.
51
Assessment of dystussia in TBI
Erin Silverman, PhD1,2,3 epearson@ufl.edu
Sarah Miller, PhD, RN,4 Christine Sapienza, PhD,5 Paul W. Davenport, PhD1
1Department
of Physiological Sciences, University of Florida, Gainesville, FL
Florida South Georgia Veteran’s Health System, Malcom Randall VAMC); 3(Rehabilitation
Outcomes Research Center – RORC, Malcom Randall VAMC, Gainesville, FL); 4(University of Memphis,
Memphis, TN); 5 (Jacksonville University, Jacksonville, FL)
2(North
Background: Symptoms associated with traumatic brain injury (TBI) may include airway compromise in
the form of impaired cough or dystussia. The presence of impaired cough places an individual at
increased risk for uncompensated aspiration. Aspiration is very common in individuals with TBI and
typically takes the form of silent (aspiration followed by no cough response) in almost half of all
individuals with TBI (Terre & Meari, 2007). Cough function and urge to cough have .D.
been studied in a number of cohorts including healthy controls, Parkinson’s Disease, stroke, and
Amyotrophic Lateral Sclerosis, however there has been no systematic investigation of these functions in
those with TBI. Personal communication with physicians and rehabilitation staff at Walter Reed Army
Medical Center has revealed that issues relating to airway compromise in many individuals with TBI and
that these issues persist even following discharge from medical facilities. Therefore the central aim of this
project was to quantify and describe various physiological aspects of airway compromise, including cough
impairment, in those with TBI.
Methods: A capsaicin cough challenge was administered to three individuals who had sustained a TBI
within the preceding 5 years. Global severity ratings were obtained in the form of Montreal Cognitive
Assessment (MOCA) and Rancho Los Amigos (RLAS) scores. Participants were administered a
randomized block series of capsaicin and saline solution at the following concentrations (µM): 0, 50,
100, 200, and 500. Each concentration was administered 3 times for a total of 15 administrations via a
standard respiratory facemask connected to a nebulizer. Cough responses were recorded by
pneumotachograph and the cough airflow signal was digitized and recorded onto a desktop computer
(Chart, ADInstruments). Cough counts were obtained following each capsaicin solution administration.
Participants were also instructed to rate their urge to cough using a modified Borg scale where 1 equals
no urge and 10 equals maximum urge. Cough counts and urge to cough ratings were compared to data
previously obtained from healthy normal control subjects.
Results: Significant differences were observed relative to number of coughs and urge to cough. TBI
patients coughed less and had a lower urge to caugh.
Discussion: These results show apparent differences in cough response including urge to cough in
participants with TBI compared with existing data obtained from healthy controls. Clinical and
rehabilitation considerations are discussed within the context of these findings.
52
Effects of heart rate variability biofeedback on peak expiratory flow rates in steroid-naïve
patients with mild or moderate asthma
Michael Singer1 spaceman792@live.com
Gabriel Pontipiedra,1 Kevin Ma,1 Nimesh Patel,1 Patrick Maulion,1 Milisyaris Aviles, MS,1 Jessica Graves,
MA,2 Shou-En Lu, PhD,1 Frederick Wamboldt, MD,2 Paul M. Lehrer, PhD 1
1Rutgers—The
State University of New Jersey, New Brunswick and Piscataway, NJ, USA2National Jewish
Health, Denver, CO, USA
Background. Asthma is a chronic disease of the airways, it has varying severity and symptoms but typically
presents with increased airway reactivity to irritants. As of now, there is no cure for asthma, although
medications can alleviate exacerbations and symptoms. Inhaled corticosteroids are usually prescribed as
controller medication, but studies have shown low rates of adherence, primarily because of cost or fear of
adverse side effects. The goal of this study is to evaluate the effectiveness of heart rate variability
biofeedback (HRV-BF) as a supplement or alternative to corticosteroid use. Previous research has found
that HRV-BF allows patients to take less asthma medication, while alleviating symptoms, improving
pulmonary function, and preventing exacerbations
Method. This is an interim analysis of data from an ongoing two-center trial. Eighteen subjects were
assigned to a group receiving HR-BF, and 21 to a group receiving a combination of EEG alpha biofeedback,
listening to relaxing music, and paced breathing at a relaxed rate (10-12 breaths/min) (EEG+). Training
lasted approximately 4 months, with 6-10 sessions of training and assigned daily home practice. Subjects
took daily morning and evening home peak flow measures on a Piko peak flow meter. We calculated the
mean and standard deviation of daily AM peak flow values for approximately each month in the study.
Fourteen subjects in HRV-BF and 7 in EEG+ had completed the last study week at the time these data
were analyzed.
Results. Preliminary data analysis showed a significant increase across both groups in peak expiratory flow
mean and a decrease in standard deviation of peak expiratory flow values in both groups. However there
were no differences between groups.
Discussion. Results suggest that both our placebo and experimental conditions produced improvements in
asthma condition. Paced breathing at a relaxed rate may help asthma as much as breathing at resonance
frequency for measures of peak flow. Relationship with other variables may determine the pathways of
action for each of the methods.
53
Deep brain stimulation and airway protection in Parkinson’s disease
Michelle S. Troche, PhD/CCC-SLP,1 michi81@PHHP.UFL.EDU
Karen W. Hegland, PhD/CCC-SLP,1 Alexandra E. Brandimore, MA/CCC-SLP,1 Michael Okun, MD,2 Paul W.
Davenport, PhD3
1Department
of Speech, Language, and Hearing Sciences
University of Florida, Gainesville, FL, USA
2Department of Neurology and Neurosurgery
University of Florida, Gainesville, FL, USA
3Department of Physiological Sciences
University of Florida, Gainesville, FL, USA
Background: Deep brain stimulation (DBS) surgery into the subthalamic nucleus (STN) and the globus
pallidus interna (GPi) is quickly becoming the management option of choice for persons with Parkinson’s
disease (PD). Despite this, the effects of DBS on swallowing and cough function are understudied, which
is problematic given aspiration pneumonia is a leading cause of death in PD. The goal of this study was to
compare the effects of STN vs. GPi DBS on swallowing and cough outcomes in PD.
Method(s): Twenty-five participants with mild to moderate PD who were undergoing DBS were recruited
for this study. Study procedures were completed before surgery and six months post-DBS surgery.
Participants completed a capsaicin challenge with three randomized blocks of 0, 50, 100 & 200 μM
capsaicin. Following each presentation, participants rated their UTC using a modified Borg scale.
Sensitivity of the participant to the cough stimulus was measured as the log–log relationship of capsaicin
concentration and UTC. Participants completed a videofluoroscopic evaluation of swallowing and
swallowing safety was evaluated using the penetration-aspiration scale.
Result(s): There was no significant difference in age, disease duration, or PD severity between STN and
GPi DBS groups. Participants who received GPi DBS maintained swallowing safety outcomes, while
participants who received STN DBS worsened. Preliminary results identified blunted UTC in the STN
group as compared with the GPi group. These findings correlated with swallowing severity.
Discussion: Understanding the differential effects of STN vs. GPi DBS on cough and swallowing outcomes
provides interesting insight regarding the neural underpinnings of airway protection. Additionally,
identifying the effects of DBS on airway protection is important and timely as DBS continues to develop as
a primary management option; especially considering that aspiration pneumonia is a leading cause of
morbidity and death in the PD population.
54
Symptom perception and affect: A theoretical account
Omer Van den Bergh, PhD Omer.VandenBergh@ppw.kuleuven.be
KU Leuven - University of Leuven, Health Psychology, Leuven, Belgium
High trait negative affectivity (NA) persons tend to report symptoms that are poorly or unrelated to
physiological dysfunction, both when healthy and ill. This relationship is also found, but less robustly, for
high state NA. Most of the evidence on this relationship is correlational precluding interpretation of
causal mechanisms. In the past decade, we have investigated this relationship in an experimental way
through symptom inductions in the laboratory. We will present a review of studies and propose a simple
set of assumptions about mechanistic processes that can account for most findings. We propose that high
NA persons possess an over-reactive evaluative system leading to predominantly processing affectivemotivational aspects of a somatic experience at the expense of sensory-perceptual details. As a result,
they develop somatic memory representations that are characterized by poor sensory-perceptual detail
and are dominated by affective-motivational memory codes. Combined with deficient cognitive control,
these assumptions are able to explain why and when high trait NA persons show poor correspondence
between physiological dysfunction and self-reported symptoms, why they tend to be polysymptomatic
and fail to show a normal retrospective bias (e.g. peak-end effect) in symptom reports, and why they are
easily amenable to report symptoms in response to (associatively) learned and natural negative affective
cues in the absence of physiological dysfunction. Clinical implications of this perspective are discussed.
55
Low end-tidal PCO2 across stress-related disorders: A transdiagnostic exploration of its
correlates
Maaike Van Den Houte, MA1 Maaike.VanDenHoute@ppw.kuleuven.be
Katleen Bogaerts, PhD, 1 Lukas Van Oudenhove, PhD, 2 Ilse Van Diest, 1 PhD,
Omer Van den Bergh, PhD1
1Health
2Clinical
Psychology, University of Leuven, Leuven, Belgium
and Experimental Medicine, University of Leuven, Leuven, Belgium
Background. Low end-tidal PCO2 (PetCO2) and slow recovery from hyperventilation provocation is
frequently observed in panic disorder. On the other hand, in respiratory medicine the term chronic
hyperventilation is used to label patients with low PetCO2 and compromised recovery. Regardless of
diagnostic controversies about differences and overlap, low PetCO2 may possibly be considered a
transdiagnostic marker of psychophysiologic stress response occurring in a large variety of patients with
stress-related disorders. The aim of this study was to explore possible correlates of PetCO 2 across
different stress-related disorders.
Method. A convenience sample of 106 outpatients with stress-related complaints, psychological disorders
with a strong somatic component and functional disorders performed a capnography test (2-minute
baseline; 5 deep sighs, 2-minute recovery; voluntary hyperventilation followed by 2 minutes of recovery).
Patients filled out questionnaires measuring various personality variables, subjective physical complaints,
psychiatric complaints and quality of life. Diagnostic information was available for 64 patients.
Results. Mean baseline PetCO2 for the whole sample was low (34,93 mmHg, SD= 3,97 mmHg). Low
baseline PetCO2 was associated with slower recovery from provocation, but not with recovery from
sighing. Mean baseline PetCO2, PetCO2 right after challenge or recovery rates did not differ between
diagnostic groups. None of the physiological measures correlated with trait questionnaires.
Conclusion. As expected, low PetCO2 was associated with slower physiological recovery from voluntary
hyperventilation. However, low levels of PetCO2 and slow recovery were not exclusively characteristic for
patients suffering from panic disorder, nor was it associated with questionnaires measuring aspects of
panic disorder. These results suggest that instead of being specific to panic disorder, low PetCO 2 and slow
recovery might be a marker for stress-related disorders in general. Because of low sample sizes of the
diagnostic groups, these data should be interpreted with caution.
56
Indirect regulation of breathing: a detour may be fastest
Jan van Dixhoorn, MD, PhD dixhoorn@versatel.nl
Centre for breathing Therapy Amersfoort and Research Center Linnaeus Institute, Haarlem
Background. Direct breathing regulation implies a goal-directed strategy to change specific aspects of
breathing: frequency, pauses, volume, ETCO2, resonance to heart rate, location etc. An alternative option
is indirect regulation, which consists of strategies to modify determinants of breathing. The majority of
instructions that we use are indirect forms of regulation. We use two main determinants: mental
(direction of attentional focus) and mechanical (posture). The presentation will show how this is done and
its effect on breathing movement and subjective sensation.
Method. A recording was made of five experienced practitioners, executing a simple movement, while
sitting on a flat, horizontal surface (a stool), looking straight ahead, feet in front of the knees, hands on
the upper legs. They moved front and back a little, while focusing on the shift of weight in the sitting
bones, for about one minute. Before and after, breathing movement was assessed manually (MARM) and
subjective changes afterwards were noted.
Results. The videos show an increased coordination between lumbar spine and chest bone, as well as
improved balance of the head. Subjects noted to sit more firm and straight, to feel more freedom in the
neck and more involvement of breathing in the chest. MARM showed an increase in the upper line
(p<0.05) and a lesser decrease in the lower line (ns), resulting in a larger area of breathing movement.
Discussion. An indirect procedure is a feasible option for breathing regulation.
57
Psychophysiological treatment of anxiety: does the diagnosis matter?
Jan van Dixhoorn, MD, PhD1 dixhoorn@versatel.nl
A Mataheru2, R Overbeek2, M Scheffers2
1Centre
for breathing Therapy Amersfoort en Research Center Linnaeus Institute, Haarlem, The
Netherlands
2 Windesheim College, Zwolle, The Netherlands
Background. In experimental studies it has been shown that psychophysiological treatment can be
effective in patients with anxiety disorder (Meuret, 2008) or with somatisation disorder (Katsamanis,
2011). In this observational study, we investigated whether patients with mainly anxiety complaints but
without a DSM-IV diagnosis responded differently from patients with a DSM-IV diagnosis.
Method. Patients with anxiety as their main complaint were selected from an existing database,
containing subjects who were referred for breathing and relaxation therapy from 2006-2011. They were
255 subjects, 205 did not have a DSM-IV diagnosis (148 women, 57 men) and 50 subjects (36 women, 14
men) did. Outcome was assessed clinically (good effect, limited effect, no effect) and by way of two
checklists, Nijmegen Questionnaire (NQ) and the General Distress Questionnaire (GDQ).
Results. Good clinical effect was present in 52% of patients without diagnosis and in 37% of patients with
diagnosis. Initial NQ scores were slightly higher for patients with diagnosis, statistically not significant, but
initial GDQ scores were significantly higher. Both groups improved on both questionnaires, both highly
significant (p<0.001). However, effect sizes were higher for patients without diagnosis (NQ: 1,0; GDQ:
1,0), than for those with diagnosis (NQ: 0,59; GDQ: 0,80). As a result the questionnaires normalized for
more patients without diagnosis, than for those with diagnosis.
Discussion. Although patients with DSM-IV diagnosis had higher scores and smaller reductions after
treatment, the differences were relatively small and both groups did benefit significantly. Differences
were greatest in general distress.
58
Resonance breathing affects hemodynamic oscillations in the brain at 0.1 Hz
Evgeny Vaschillo, PhD1 evaschil@rci.rutgers.edu
Jennifer F Buckman,PhD,1 Deena Peyser,BA,1 Sydney Heiss, 1 Peter Barnas, 1 Laura Banu,1 Alexander
Puhalla,1 Bronya Vaschillo, MD,1 David Eddie,MS,1 Suchismita Ray, PhD,1 Stephen Hanson, PhD,2 Catherine
Hanson, PhD,2 Bharat Biswal, PhD,3 Marsha E Bates, PhD1
1Center
for Alcohol Studies, Rutgers – The State University of New Jersey, Piscataway, NJ, USA
– The State University of New Jersey, Newark, NJ, USA
3New Jersey Institute of Technology, Newark, NJ, USA
2Rutgers
Background: The positive effects of resonance breathing (0.1 Hz; ~6 breaths-per-minute [6P]) on
cardiovascular functions and clinical symptoms have been well-documented, yet little is known about
functional brain responses during resonance breathing. The present study investigated hemodynamic
oscillation in the whole brain during 6P by simultaneously assessing electrocardiogram (ECG), respiration,
and the BOLD response using functional magnetic resonance imaging (fMRI).
Methods: Participants (n = 22, 9 females, ages 18-25) completed two 5-minute tasks: a baseline task and a
6P breathing task in a 3T Siemens Trio scanner. During baseline, participants completed a low-demand
task. During 6P, participants breathed at a rate of approximately 0.1 Hz by following a visual pacer. ECG
and respiration data were collected using Biopac MRI-compatible ECG electrodes and thoracic breath
belt. Time series fMRI BOLD data were extracted using FSL 5.0.5. Power spectra were estimated using a
Fourier transformation in WinCPRS (Absolute Aliens Oy, Finland).
Results: During the baseline task, there was substantial variability between participants in the power
spectra of hemodynamic oscillations in the brain. During the 6P task, robust peaks were observed at 0.1
Hz in the brain stem and cerebellum. Peaks at 0.1 Hz were also observed for most participants in the
amygdala, and anterior cingulate, frontal medial, and insular cortices during 6P. In addition, one
participant who did not perform 6P properly also did not demonstrate any discernible resonance
breathing effects in these brain regions.
Discussion: We observed hemodynamic oscillations at 0.1 Hz in multiple brain regions during resonance
breathing. These data provide the first step towards better understanding how respiration affects brain
hemodynamics and how resonance breathing potentially may contribute to positive clinical outcomes.
59
Sigh to restore respiratory variability. proposed mechanism.
Evgeny Vaschillo, PhD evaschil@rci.rutgers.edu
Bronya Vaschillo, MD, Jennifer Buckman, PhD, Sydney Heiss, Marsha Bates, PhD
Center of Alcohol Studies, Rutgers University, New Jersey, USA
Background: Prior studies showed that a sigh is a respiratory maneuver associated with stressful events,
negative emotions, unpleasant thoughts, as well as with cognitive loading and sustained attention.
Vlemincx and colleagues (2010 – 2013) found that a sigh can restore the structure of respiratory
variability after disruption by psychological strain and hypothesized that normalization of respiration
reduces stress and counteracts emotionality. The present study builds on these findings by suggesting a
mechanism by which sighing restores respiratory variability.
Method: ECG, respiration, and beat-to-beat blood pressure were collected in 24 young healthy
participants during a baseline, 0.1 Hz paced breathing, and 0.02 Hz paced sighing (10 sighs, 1 sigh/50
seconds, with normal breathing interspersed) tasks.
Results: Each sigh induced a powerful, but temporally constrained effect on blood pressure (BP), RRI, and
pulse transit time (PTT, a measure of vascular tone) that gradually faded over ~50 s. Each sigh provoked
an average change of 14.5(1.4) mmHg in systolic BP, 7.3(0.4) mmHg in diastolic BP, 106.9(12.4) ms in RRI,
and 8.7(1.0) ms in PTT.
Discussion: The affected cardiovascular functions are known to participate in homeostatic processes that
control stress and emotions through the baroreflex. We suggest that the observed changes in BP, RRI, and
PTT induced by a sigh occur due to activation of the afferent neural outflow from the baroreceptors. This
afferent traffic serves as a broad inhibitory force on subcortical and cortical processing and, as such, can
mitigate emotional and psychological strain. These results thus provide preliminary evidence that a sigh’s
ability to “reset” the respiratory system is provided by the baroreflex mechanism. According to this
hypothesis, a sigh alters cardiovascular functions, which activate the afferent stream of the baroreflex.
This afferent activation promotes neural inhibition to reduce stress and emotional arousal. This
psychological benefit then serves to restore respiratory variability.
60
Asthma triggers in Latino adults with comorbid asthma and panic disorder
Karinna Vazquez, MA kvazquez427@gmail.com
Jonathan Feldman, PhD
Ferkauf Graduate School of Psychology, Yeshiva University, Bronx, NY, USA
Background: Asthma has been linked to a higher prevalence of panic disorder (Carr, Lehrer, & Hochron,
1992; Carr, Lehrer, Rausch, & Hochron, 1994) and this comorbidity occurs more often in Latinos than in
other ethnic groups (Dumanovsky & Matte, 2007; Lehrer, Feldman, Giardino, Song, & Schmaling, 2002;
Rose, Mannino, & Leaderer, 2006). The aim of the current study was to examine differences in asthma
triggers between Latino asthma patients with panic disorder versus Latino asthma patients without panic
disorder. It was expected that Latino asthma patients with panic disorder would endorse a higher
frequency of asthma triggers than those without panic disorder.
Methods: Participants in this study included 302 (227 English-speaking and 75 Spanish-speaking) selfreported, adult asthma patients of Latino descent who were screened to assess eligibility for the asthma
and panic disorder treatment study. This study examined asthma triggers using the Asthma Trigger
Inventory (ATI), a structured, self-report instrument for the assessment of asthma triggers (Ritz, Steptoe,
Bobb, Harris, & Edwards, 2006). The PRIME-MD Patient Health Questionnaire (PHQ): Panic Screening
Questions was used to assess if participants exhibited panic disorder symptoms. The Structured Clinical
Interview for DSM-IV (SCID-I) and the Panic Disorder Severity Scale (PDSS) were used to confirm the
diagnosis and assess the severity of panic disorder.
Results: The results showed that participants with panic disorder reported a significantly higher frequency
of psychological, physical activity, pollutant, and infection asthma triggers than participants without panic
disorder controlling for age, gender, and language of interview. The results also found that participants
with panic disorder reported a significantly higher impact of asthma triggers on their daily functioning
than participants without panic disorder.
Discussion: The findings suggest that asthma triggers may have a greater impact on Latino asthma
patients with panic disorder than Latino asthma patients without panic disorder. Interventions can be
developed to help patients learn how to avoid or control triggers that have a higher prevalence in Latino
asthma patients with panic disorder.
61
The effect of sighs on self-reported relief and physiological muscle tension
Elke Vlemincx, PhD elke.vlemincx@ppw.kuleuven.be
Ilse Van Diest, PhD, Omer Van den Bergh, PhD
Research Group on Health Psychology, University of Leuven
Background. Research in both animals and humans has shown an important correlation between sighs
and relief. However, the proposed resetting properties of sighs suggest that sighs cause relief. The current
experiment aimed to compare the causal effect of sighs versus breath holds on psychological and
physiological relief.
Method. A previously established paradigm alternating transitions to certain safety (predicting that no
aversive stimulus would occur) with transitions to danger (predicting that an aversive stimulus would
occur) was used, which has been shown to increase spontaneous sigh rates. Three blocks of 40 trials were
presented. In the first block, no breathing instructions were given. In Blocks 2 and 3, participants (N=35)
were instructed to either take a deep breath (‘sigh’) or to postpone their next inspiration for two seconds
('breath hold') during transitions in 20 trials. Continuously, surface electromyography of the Frontalis was
measured and participants rated how relieved they felt using a dial. Self-reported relief and physiological
tension were compared five seconds before and after each sigh (defined as a breath in the ‘sigh’ block
with a volume at least twice as large as the mean volume during Block 1) and each breath hold (defined as
a breath in the ‘breath hold’ block with an expiratory pause longer than two seconds which was not a
sigh).
Results. Results show that (1) self-reported relief following a sigh was higher than before a sigh, (2) selfreported relief following a sigh was higher than following a breath hold, and (3) self-reported relief did
not change before and after breath holds. In addition, physiological tension decreased following a sigh,
but did not decrease following a breath hold.
Discussion. These results suggest that a sigh relieves, both psychologically and physiologically, and
therefore support the hypothesis that sighs function as psychological and physiological resetters.
62
Neural processing of short-term habituation and sensitization to dyspnea
Andreas von Leupoldt, PhD 1,2 andreas.vonleupoldt@ppw.kuleuven.be
Roland W Esser 2, MMatthias Gamer 2, Christian Büchel2, Maria Cornelia Stoeckel2
1
Research Group Health Psychology, University of Leuven, Leuven, Belgium
of Systems Neuroscience, University Medical Center Hamburg-Eppendorf, Hamburg,
Germany
2Department
Background Both habituation and sensitization to dyspnea might impact the course of the underlying
disease. This study examined neural processes involved in short-term habituation and sensitization to
experimentally induced dyspnea.
Methods Forty six healthy volunteers underwent twenty blocks of inspiratory resistive loaded breathing
with parallel acquisition of fMRI-data. We alternately presented loads inducing severe dyspnea (dyspnea
condition) and loads that were just noticeable (baseline condition). Each condition was cued for 6s
(anticipation period) and lasted 24s (dyspnea period). After each block ratings of dyspnea intensity and
unpleasantness were obtained. We compared data from the second (“late”) half with data from the first
(“early”) half of the experiment.
Results Approximately two thirds of the volunteers showed increased intensity and/or unpleasantness
ratings (indicating “sensitization”) during the second half of the experiment as compared to the first half.
The remaining third showed similar or decreased ratings (indicating “habituation”). For the anticipation
period, we observed a significant negative correlation of delta intensity and unpleasantness ratings with
the late vs. early [cue dyspnea vs. cue baseline] contrast in the periaqueductal gray (PAG). A positive
correlation of delta unpleasantness ratings was found with bilateral anterior insula. For the dyspnea
period, we observed a negative correlation of delta intensity and unpleasantness ratings with the late vs.
early [dyspnea vs. baseline] contrast in the rostral anterior cingulate cortex (rACC). A positive correlation
of delta unpleasantness ratings was found with right anterior insula.
Discussion An increasing recruitment of PAG and rACC during the anticipation (PAG) and perception
(rACC) of dyspnea seems to result in short-term habituation in perceived intensity and unpleasantness of
dyspnea. In contrast, an increasing recruitment of anterior insula during the anticipation and perception
of dyspnea seems to underlie a short-term sensitization process that is limited to the perceived affective
unpleasantness of dyspnea.
63
How is breathlessness remembered by patients with Medically Unexplained Dyspnea?
Marta Walentynowicz, MA1 Marta.Walentynowicz@ppw.kuleuven.be
Katleen Bogaerts, PhD,1 Linda Stans, MA,3 Ilse Van Diest, PhD,1 Filip Raes, PhD,2 Omer Van den Bergh,
PhD1
1Health
Psychology, University of Leuven, Leuven, Belgium
and Experimental Psychopathology, University of Leuven, Leuven, Belgium
3Pneumology Department, University Hospital Gasthuisberg, University of Leuven, Belgium.
2 Learning
Background. Retrospective reports of breathlessness serve as an important source of information for
clinicians. Several biases may influence memory for symptoms, but little information exists on how
breathlessness episodes are encoded and remembered by persons reporting breathlessness unrelated to
physiological dysfunction. In the present study we investigated whether memory for experimentally
induced breathlessness episodes in patients with medically unexplained dyspnea (MUD) differed from
that of matched healthy controls.
Method Female MUD patients (N=22) and matched healthy controls (N=22) participated in two trials of a
rebreathing paradigm, resulting in a progressive increase in PCO2, ventilation and breathlessness. Order
of the trials was counterbalanced across participants. Dyspnea ratings were collected at three moments:
(1) continuously during symptom induction, (2) after the experiment, (3) after 2 weeks. Respiratory
parameters were measured continuously during the trials. State NA, PA and anxiety were evaluated at
baseline and after every trial.
Results Both rebreathing trials resulted in higher concurrent dyspnea ratings as well as increased minute
ventilation among patients compared to controls. Retrospective overestimation (compared to concurrent
measurement) was observed in both groups. However, no increase in overestimation was observed
across a two week time frame and no interaction with Group was found. Compared to baseline ratings,
dyspnea induction resulted in higher anxiety and lower PA ratings in the patient group, while state NA
remained on similar level.
Discussion The findings show that retrospective dyspnea reports are biased in a similar way in both
patients and healthy controls. Since overreporting in the patient group was found across all measurement
occasions, starting from online ratings, it suggests that biases in that group may operate predominantly
during symptom perception/memory encoding. Those findings, together with the lack of increase in
overestimation over time, could inform future clinical interventions tackling symptom overestimation.
64
Retrospective memory for breathlessness and pain.
Marta Walentynowicz, MA1 Marta.Walentynowicz@ppw.kuleuven.be
Ilse Van Diest, PhD,1 Filip Raes, PhD,2 Omer Van den Bergh, PhD1
1Health
Psychology, University of Leuven, Leuven, Belgium
and Experimental Psychopathology, University of Leuven, Leuven, Belgium
2Learning
Background. Patient reports and questionnaire data on symptoms mostly rely on retrospective memory.
Comparisons of concurrent (through experience sampling) and retrospective reports typically have no
control over actual experiences. Also, individual differences in retrospective symptom reporting after
experimental symptom inductions have not been systematically investigated. In the present study, we
investigated retrospective memory for two experimentally induced symptoms, namely breathlessness
and pain, in high (HSR) and low habitual symptom reporters (LSR).
Method. Healthy women (N=48; 24HSR/24LSR) participated in (a) two trials of a rebreathing paradigm,
leading to a gradual increase in PCO2, ventilation and breathlessness, and (b) two trials of a modified cold
pressor task. Dyspnea and pain inductions were administered in two separate sessions and participants
were counterbalanced across eight trial orders. Dyspnea and pain ratings were collected at four times: (1)
continuously during symptom induction, (2) after each trial, (3) after the experiment, and (4) after 2
weeks. State NA and state anxiety were measured after every trial.
Results. Dyspnea induction resulted in higher state NA and anxiety than pain induction. Retrospective
evaluations were overall higher than concurrent evaluations, but differences between dyspnea and pain
emerged. While retrospective dyspnea ratings were equally overestimated by both groups, the recalled
pain ratings were higher in HSR than in LSR. Moreover, a further increase in overestimation over time was
only found for breathlessness ratings in HSR.
Discussion. Our results show that even though retrospective evaluations of both breathlessness and pain
are distorted, the type of bias clearly differs between the symptoms. The findings suggest the relevance
of unpleasantness of the experience for memory processes, such that in less aversive inductions
individual differences play a more pronounced role. Moreover, the observed increase of dyspnea
overestimation over time is important for diagnostic assessment based on symptom reporting.
65
The influence of respiratory dynamics on relaxation and cardiorespiratory parameters
and the response to and recovery from mental stress.
Ruth Wuyts, MA ruth.wuyts@ppw.kuleuven.be
Elke Vlemincx, PhD, Ilse Van Diest, PhD, Omer Van den Bergh, PhD
Health Psychology, University of Leuven, Leuven, Belgium
Background. Whereas slow and regular breathing instructions are often included in relaxation training,
the clinically validated effects of breathing techniques on various stress-related disorders are not well
understood. From a dynamic systems perspective, healthy breathing is characterized by complex
variability balancing correlated and random variability components, while a lack of structured variability
or too much random variability is indicative of unhealthy breathing and decreased system sensitivity to
changing environmental demands. In this study we investigated the effect of slow regular and normal
regular breathing on subjective relaxation, cardiorespiratory parameters and physiological stressreactivity.
Methods. A slow regular (8 bpm) and normal regular (14 bpm) breathing pattern was induced in each
subject (N = 23) by means of auditory pacing. Respiratory and cardiovascular parameters were
continuously recorded using the LifeShirt System. After each breathing pattern a mental stressor was
introduced followed by a recovery period. Subjective relaxation in response to the breathing patterns was
assessed, and total respiratory variability and structured variability of respiratory parameters were
indexed by the coefficient of variation (CV) and autocorrelation (AR) respectively. Cardiorespiratory
parameters were assessed in response to and recovery of the mental stressor.
Results. Mean respiratory rate (RR) showed pacing was successful. Subjective relaxation was higher during
slow regular breathing then during normal regular breathing. Structured variability of RR decreased
during both breathing exercises, and this was not compensated by increased structured variability in
respiratory volume parameters. Changes in parameters of respiratory variability and heart-rate-variability
in response to the stressor and recovery thereof will be further addressed.
Discussion. Whereas slow regular breathing increased subjective relaxation, both breathing exercises did
not promote healthy breathing. Further results will help to resolve conflicting conceptions about healthy
breathing and treatment practices.
66