Module # 31 Thrombocytopenia
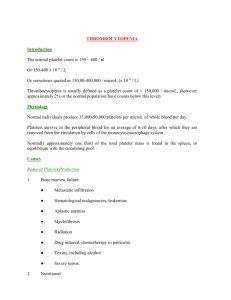
advertisement
Facilitator Version Module # 31 Thrombocytopenia Created by Dr. Mary Lacy July 2014 Objectives: 1. To understand the mechanisms of thrombocytopenia 2. To identify the most common causes of outpatient and inpatient thrombocytopenia 3. To understand how and when to treat thrombocytopenia References: 1. Gauer RL, Braun MM. Thrombocytopenia. Am Fam Physician. 2012;85(6):612-622. 2. Arnold DM, Lim W. A rational approach to the diagnosis and management of thrombocytopenia in the hospitalized patient. Semin Hematol. 2011;48(4):251-258. 3. Arnold DM, Nazi I, Warkentin TE, et al. Approach to the diagnosis and management of drug-induced immune thrombocytopenia. Transfus Med Rev. 2013;27(3):137-145. 4. Wong EY, Rose MG. Why does my patient have thrombocytopenia? Hematol Oncol Clin North Am. 2012;26(2):231-252, vii. 5. MKSAP 16 Case You are called by the ER for admission of a 49 year-old man with sepsis. The patient has never been admitted to the hospital but you have access to a few of his outpatient primary care visits from over the years. The records clue you into his history of alcohol and intravenous drug use. Labs performed by his primary care physician showed a platelet count of about 120,000 per μL on several occasions. What are the major mechanisms of thrombocytopenia? - Increased Destruction o Immune-mediated o Non-immune mediated Decreased Production Sequestration Dilutional Pseudothrombocytopenia (platelet clumping) What signs and symptoms to patients with isolated thrombocytopenia report? When do these signs and symptoms develop? - - Petechia/Purpura Mucosal bleeding o Epistaxis – if prolonged, this may be predictor of more severe bleeding risk o Wet Purpura – hemorrhagic blisters on mucous membranes can be predictor of more severe bleeding risk o GI/GU bleeding The platelet count that patient develop symptoms depends on the cause and function of the remaining platelets, but a general rule of thumb is that increased risk for severe bleeding occurs at platelet counts <10,000. ITP, for example, is associated with less bleeding risk for any given platelet count because the circulating platelets are typically younger, larger, and more effective. What are the major considerations in gathering a patient history that could point to a cause for thrombocytopenia? - Medical History: Cirrhosis, Easy bleeding/bruising Medications: Anti-epileptics, Antibiotics (more acute exposure typically) Labs: Other cell lines (MDS, Lymphoproliferative disorder), Liver function (occult cirrhosis) Social History: Risk factors for B12 or folate deficiency, Alcohol use, Tonic water/Quinine ingestion, Risk factors for Hepatitis or HIV Family history: Congenital thrombocytopenias (rare) If work up is negative, consider ITP as diagnosis of exclusion. On further investigation, you realize that your patient had isolated stable thrombocytopenia. HIV and hepatitis panels were negative. B12 and folate levels were normal. Liver function tests including albumin and INR were normal. The cause was presumed to be secondary to his chronic alcohol use causing bone marrow suppression (increased production). No abdominal imaging was performed to assess for splenomegaly (sequestration) or early cirrhosis. You learn more about his current presentation and suspect sepsis secondary to a soft tissue infection in an area of injection drug use. On examination, he has extreme tenderness as well as erythema of his right thigh. He has no other medical history and is on no medications. You admit him to the hospital and prescribe IV vancomycin. You also prescribe an opiate for his pain and subcutaneous heparin for venous thromboembolism prophylaxis. Initial Vitals/Labs: HR 110, BP 110/75, T 388, RR 16 CBC: WBC 16, Hct 35, Plt 98 BMP: Na 132, K 3.8, Cl 100, HCO3- 23, BUN 20, Cr 0.8 The degree of thrombocytopenia is acutely worsened from his baseline. What is the differential diagnosis for our acutely ill patient’s thrombocytopenia? - - Sepsis can lead to decreased production secondary to bone marrow suppression as well as platelet consumption. Disseminated intravascular coagulation (DIC) is critical to consider in any patient with thrombocytopenia and sepsis and causes thrombocytopenia by increased destruction. Infections leading to thrombocytopenia can accomplish this by immune-mediated destruction or decreased production. Many classic infections leading to thrombocytopenia are viral (HIV, HCV, EBV, CMV), though E. coli O157:H7 is associated with HUS and helicobacter pylori infection can cause a secondary ITP. Medications can also lead to increased destruction or decreased production. On presentation, our patient claimed to have no medications so this is an unlikely cause. Dilution related to massive transfusion or fluid resuscitation. You find that labs were drawn prior to any fluid administration in the ED. What work up would you pursue for this patient’s thrombocytopenia? What abnormalities would you expect if this patient had DIC? - Labs: high PT/INR, PTT, FDP, D-dimer; low fibrinogen Peripheral blood smear: schistocytes, low platelets What are the causes and complications of DIC? How do you treat it? - Complications: Bleeding and thrombosis. Ultimately DIC can cause multi-organ dysfunction related to hemorrhage and microthrombi. Causes: Sepsis, Trauma, Malignancy, Obstetric complications Treatment: o Treat the underlying condition o Otherwise, treatment is primarily targeted towards complications of DIC: If active bleeding: Fibrinogen > 100mg/dL (cryoprecipitate) INR < 1.5 (FFP Platelets > 50,000 Heparin for patients with predominantly thrombotic complications is generally reserved for chronic, compensated DIC DIC is a condition of thrombocytopenia that can be associated with thrombosis. What other classic causes of thrombocytopenia can result in thrombosis? - Thrombotic thrombocytopenic purpura Heparin-inducted thrombocytopenia Anti-phospholipid syndrome Your patient’s laboratory results return for the work-up of his thrombocytopenia: - INR 1.2 (0.8-1.2), PTT 35s (25-35s), fibrinogen 600mg/dL (200-400mg/dL) Peripheral blood shows low platelets without schistocytes Your patient doesn’t have DIC. Unfortunately, his pain continues to escalate and seems out of proportion to your exam. You re-examine him and decide to call general surgery to evaluate for necrotizing fasciitis. His antibiotics are broadened and he is transferred to the general surgery team. On day 7 of his admission you are called by the general surgery team to take the patient back on your service. His last trip to the OR was 3 days prior and he has been narrowed to IV vancomycin for MRSA in his operative cultures. He continues on opiates and subcutaneous heparin for VTE prophylaxis. He was incredibly lucky and his infection has stabilized, but his platelets have dropped to 8,000 (other cell lines are stable). His coagulation studies are normal. He has petechiae in dependent areas and reports a nosebleed that stopped with direct pressure. Your first thought is HIT secondary prolonged heparin exposure. How would you calculate the probability of HIT in our patient? How do you diagnose and treat HIT? - 4T’s score is the most extensively studied. It has a high NPV for low-probability scores and is very sensitive. The PPV is limited and the diagnosis needs laboratory confirmation. If HIT is suspected based on intermediate or high-probability score, heparin should be stopped. Treatment is with argatroban (parenteral, hepatic metabolism) or bivalirudin (parenteral, primarily renal clearance). Fondaparinux (subcutaneous) is also often used, though off-label. - Laboratory confirmation of diagnosis: Heparin-Platelet Factor 4-Ab ELISA for initial screening. If positive, send a serotonin release assay (SRA). Our patient has a low probability for HIT, which suggests that you should look for other causes. What is the most likely cause of our patient’s thrombocytopenia? Drug-induced immune thrombocytopenia (DITP) secondary to vancomycin is the most likely cause of his thrombocytopenia. DITP is characterized by exposure to a common offending agent, onset within 5-10 days, and nadir <20,000 (which is not characteristic of HIT). Other medications encountered in the hospital that have been shown to cause DITP include: TMP/SMX, beta-lactams, acetaminophen, rifampin, carbamazepine, phenytoin, and GPIIb/IIIa inhibitors. Of note, the DITP caused by GPIIb/IIIa inhibitors occurs within hours of first drug exposure. The mechanism of linezolid and valproic acid induced thrombocytopenia is bone marrow suppression. Of note, if there was a report of blood transfusions in our patient, post-transfusion purpura would be a consideration. How would you treat our patient? What if he needed another invasive procedure? Treatment is withdrawal of the drug and standard platelet transfusions for platelets less <10,000 or active bleeding. Our patient should receive platelets secondary to his platelet count less than 10,000. If our patient needed to return to the OR, the standard platelet threshold is 50,000. CNS and ocular procedures require platelet counts >100,000. Central lines can be performed with platelets > 20,000. Steroids and IVIG are sometimes tried for drug-induced ITP. These are first-line treatments in primary ITP, which cannot effectively be ruled out in this clinical scenario. There is no evidence of their benefit in DITP. Fortunately, your patient does not need to return to the OR. Over the next week, his platelets recover with withdrawal of vancomycin. He is able to discharge from the hospital. MKSAP 16 Questions: Hematology & Oncology: Question 5 (Transfusion thresholds - C) Hematology & Oncology: Question 23 (ITP treatment - E) Hematology & Oncology: Question 55 (TTP diagnosis - D) Hematology & Oncology: Question 68 (HIT treatment - A)