Pharmacy Residency Rotation Summary | Interior Health
advertisement

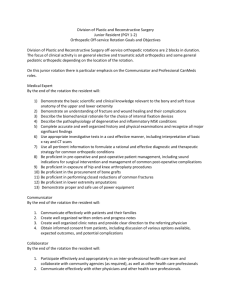
Interior Health Pharmacy Practice Residency Program
Rotation Name
Rotation Location
Preceptor: Name
Title
Contact Information (email, phone, pager)
Description
[Include a description of the hospital, services provided, type of rotation (ie. core or elective, inpatient
or outpatient), the description the unit/ward, clinic(s) that the resident will be working in, the types of
team members that the resident will be interacting with to provide care, and the types of learning
experiences (eg. learn what it is like to work in an ambulatory care clinic, learn about specific disease
states common in these clinics).]
Example Description: Kelowna General Hospital is a 341-bed tertiary care referral hospital that provides
specialty and sub-specialty care to approximately 300,000 people in the Okanagan Valley. The hospital
is affiliated with the University of British Columbia as a clinical academic teaching site. The medicine
rotation is a core rotation in the Interior Health Pharmacy Practice Residency Program and will take
place on the Medical Teaching Unit (MTU) at Kelowna General Hospital. The MTU is a ten-bed acute
adult internal medicine unit and is a key learning environment for medical residents and students. The
MTU is staffed by an attending physician, a senior internal medicine resident, junior residents, medical
students and a pharmacist. In addition, nurses, physiotherapists, occupational therapists, social workers
and other allied health professionals work closely with this team to provide patient care. The resident
will integrate into the MTU and work as part of a multi-disciplinary team to provide patient care. The
resident will be exposed to a wide variety internal medicine-related diseases and pharmacotherapy
throughout this four week rotation.
Goals and Objectives
{Note: these are standard for all rotations and must be included in all direct
patient care rotation summaries}
Goal 1:
Objectives:
Develop and integrate the knowledge required to provide direct patient care as a member
of the interprofessional team.
The resident will be able to:
1. Relate knowledge of the pathophysiology, risk factors, etiology and clinical presentation of
medical conditions, including symptoms, physical assessment data, relevant diagnostics, and
laboratory findings to patient-specific clinical findings to make appropriate, patient-specific drug
therapy recommendations. (CPRB 3.1.4.e)
2. Relate knowledge of pharmacology, pharmacokinetics, pharmaceutics, and evidence-based
therapeutics pertaining to medication therapy to patient-specific clinical findings to make
appropriate, patient-specific drug therapy recommendations. (CPRB 3.1.4.e)
3. Acquire and utilize knowledge of safe medication practices to manage and improve medication
use for patients. (CPRB 3.2.5)
Goal 2:
Demonstrate the necessary pharmaceutical care skills to provide direct patient care as a
member of the interprofessional team.
Objectives:
The resident will be able to:
4. Place a high priority on, and be accountable for, selecting and providing care to patients who are
most likely to experience drug therapy problems. (CPRB 3.1.3)
5. Establish a respectful, professional and ethical relationship with the patient and their caregivers.
(CPRB 3.1.4.a)
6. Gather relevant patient information by conducting a patient interview and from all other
appropriate sources. (CPRB 3.1.4.c.d)
7. Develop a prioritized medical problem list and describe the current active issues that are
responsible for the patient’s hospitalization or clinic visit. (CPRB 3.1.4.e)
8. Identify, prioritize and justify patient-specific drug therapy problems. (CPRB 3.1.4.b)
9. Identify goals of therapy and advocate for the patient in meeting their health-related needs and
their desired goals of therapy. (CPRB 3.1.2)
10. Identify, prioritize, assess and justify all reasonable therapeutic alternatives and discuss the
advantages and disadvantages of each alternative, considering efficacy, safety, patient factors,
administration issues and cost. (CPRB 3.1.4.e)
11. Develop, justify and communicate patient-specific recommendations for all identified drug
therapy problems. (CPRB 3.1.4.e.f)
12. Design and implement monitoring plans and plans for continuity of care that accommodate new
or changing information and provide patient education and continuity of care. (CPRB 3.1.4.g.h)
13. Proactively communicate healthcare issues, recommendations and care plans verbally to the
appropriate team members and the patient. (CPRB 3.1.4.f.i, 3.2.4.c)
14. Proactively document healthcare issues, recommendations and care plans, as appropriate in the
health care record. (CPRB 3.1.4.e.f.i, 3.2.4.b.c)
15. Effectively respond to medication- and practice-related questions and educate others in a timely
manner, utilizing a systematic literature search and critical appraisal skills and appropriate
means of communication (verbal or written, as appropriate). (CPRB 3.5.1.a.b.c.d.e)
Goal 3:
Demonstrate the attitudes and behaviours that are hallmarks of a practice leader and
mature professional.
Objectives:
The resident will be able to:
16. Demonstrate responsibility for his or her own learning, through the refinement and
advancement of critical thinking, scientific reasoning, problem-solving, decision-making, time
management, communication, self-directed learning, teamwork and interprofessional skills.
(CPRB 3.4.1)
17. Demonstrate commitment to the profession, collaboration and cooperation with other
healthcare workers, and an understanding of the role of the pharmacist in the interprofessional
team in the improvement of medication use for patients. (CPRB 3.1.1, 3.2.2, 3.3.3)
Rotation-Specific Objectives [sample information provided]
1. Demonstrate a clear understanding of the following internal medicine-related diseases, including
the pathophysiology, clinical presentation, therapeutics and associated pharmacotherapy for the
following diseases (other disease states or therapeutic topics may also be discussed, depending on
the interests of the resident)through therapeutic discussions, patient care activities, and discussion
of relevant therapeutic controversies:
Heart Failure, chronic stable angina, stroke, anemia, renal failure, alcohol withdrawal,
atrial fibrillation, hypertension, diabetes (type I and type II), venous thromboembolism,
electrolyte disturbances, sodium and water balance, community and hospital-acquired
pneumonia, COPD and asthma, skin and soft tissue infections, liver disease
Resident’s Own Objectives
The resident will identify several of his/her own objectives for the rotation. These should be
documented in their ePortfolio and discussed at the beginning of the rotation and assessed at
evaluation points during the rotation.
1.
2.
3.
Required Activities [sample information provided]
The resident will:
1. Provide pharmaceutical care to all assigned patients on the MTU. The resident’s patient load will be
determined based on the resident’s previous experience and comfort in an internal medicine
setting. The patient load will be modified at the discretion of the preceptor.
2. Conduct medication histories for all patients under his/her care.
3. Provide discharge medication counselling and patient education for all patients under his/her care
(when appropriate).
4. Provide seamless care for patients transferred to other wards or who are discharged from hospital,
by liaising with other clinical pharmacists, physicians, community pharmacists, family physicians, BC
PharmaCare, as appropriate.
5. Attend all patient care rounds with your team.
6. Attend morning report for case discussions with your team.
7. Attend weekly Ground Rounds (Wednesday 0800-0900) if topic is of interest to the rotation.
8. Meet with the preceptor briefly every morning to triage and select patients for work-up.
9. Meet with the preceptor for approximately 1-2 hours per day in the afternoon to discuss patients
and clinical topics or controversies as they arise.
10. Discuss all written notes and recommendations with the preceptor prior to implementation, unless
previously arranged with the preceptor.
11. Prepare for 2-3 therapeutic topic discussions per week with the preceptor by completing any
assigned pre-readings and reviewing any associated pharmacotherapy or therapeutics.
12. Prepare and deliver one journal club or case presentation for the pharmacy staff at pharmacy
education rounds.
Communication Expectations [sample information provided]
1. The resident will discuss all written notes with the preceptor prior to placing them in the health
record. The resident will photocopy all written notes for later review by the preceptor.
2. The resident will discuss all recommendations with the preceptor prior to implementation.
3. The resident will notify the preceptor in advance of any off-site activities and absences during the
rotation.
Preceptor Responsibilities [sample information provided]
The preceptor will:
1. Meet with the resident at the beginning of the rotation to discuss the goals and objectives of the
rotation and work with the resident to develop a schedule for all rotation-specific activities and
therapeutic discussions.
2. Introduce the resident to the MTU team, the medicine ward, the pharmacists, nurses and other
health professionals that the resident will be working with.
3.
Meet with the resident briefly every morning to triage and select patients for work-up.
4. Meet with the resident daily in the afternoon to discuss and review all patients under the resident’s
care.
5. Discuss clinical and therapeutic topics with the resident at least 2-3 times per week
6. Be available to the resident in person or by phone at all times during the rotation.
7. Assist the resident in selecting their topic for journal club/case presentation and will schedule dates
for the journal club/presentation.
8. Provide informal feedback to the resident on their performance on a daily basis and will conduct a
written or verbal mid-point evaluation and a formal written and verbal final evaluation with the
resident.
Required Equipment
[eg. calculator, lab coat]
Evaluation Processes
1. The resident will receive a formative evaluation at the mid-point of the rotation. This evaluation will
take into account the rotation-specific objectives and the resident’s own objectives.
2. The resident will receive a summative evaluation at the end of the rotation. This evaluation will take
into account the rotation-specific objectives and the resident’s own objectives.
3. The resident will receive continuous feedback throughout the rotation and this will be considered
part of the evaluation process.
4. The resident will evaluate both the preceptor and the rotation.
5. The preceptor and resident will discuss their respective evaluations in a face-to-face manner.
Required Reading
[Include citations for any readings that you would like the resident to do before or during the rotation.
Alternatively, these can also be provided to the resident on the first day of their rotation (eg. as a
citation or pdf) or throughout the rotation if more appropriate]
Before Rotation:
During Rotation: