Leptospirosis in wildlife and cats- Pilot study
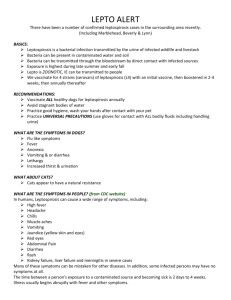
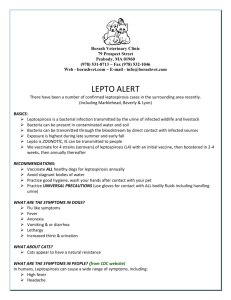
advertisement

UTRECHT UNIVERSITY Leptospirosis in wildlife and cats- Pilot study Research internship Supervisor New Zealand: Supervisor the Netherlands: Student: Peter Wilson Ruurd Jorritsma Mark van de Pol Abstract The studies presented in this paper are both studies about the role of Leptospirosis in animals in the (sub-) urban area. The first part is a pilot study on the prevalence of Leptospirosis in pest animals in the (sub-) urban area of Palmerston North which. Out of 36 caught animals (possums, hedgehogs, stoats, mice and rats) 6 were PCR positive (17%). Of the same 36 animals, 1 out of 7 (14%) urine samples were DNA positive and 6 out of 23 (26%) blood samples were seropositive for Leptospira spp. Three of the seropositive animals were positive for L. Hardjo, two were positive for L. Ballum, and one sample was positive for both serovars. The amount of animals though is insufficient to say something about the prevalence in the different species investigated, but there is already evidence of both L. and L. Ballum in pest animals living in the (sub)-urban area The second part of the studies was a pilot study on the prevalence of Leptospirosis in cats. A total of 180 cat serum samples was tested of which a total of 59 cats (32.7%) were positive for one or more serovars. L. Ballum was the serovar most found among the positive cats: 56 of the 180 tested cats had antibodies against L. Ballum (31,1%). It is likely that cats get in contact with leptospirosis due to contact with infected rodents, but to prove that, a more comprehensive study is needed. 1 General introduction Leptospirosisis a disease in animals and humans which is distributed worldwide and is mainly known because of the disease of Weil. Leptospira is an obligate aerobic spirochete bacteria of which 20 different serotypes and over 300 different serovars are known (Mansell & Benschop, 2014). Leptospirosis is a zoonosis, while no human-to-human transmission has ever been reported. Humans become most often infected with leptospirosis by direct contact with urine of infected animals or due to indirect contact, for example with water or soil contaminated with leptospires. The severity of the pathogen depends on the serovar, but also on the health status, age and immunological competence of the person. Symptoms can be mild: for example an influenza-like illness, but also very severe and leading to death (Adler & de la Peña Moctezuma, 2010). Approximately 10% of the severe infections with leptospires develop the Weil syndrome with symptoms of jaundice, acute kidney failure and pulmonary disease (Seguro & Andrade, 2013). Transmission is seen in both developing and industrialised countries and it is known that the incidence of infection in humans is higher in tropical regions than in regions with a moderate climate. The reported incidence rates are probably an underestimation (Bharti et al., 2003). Besides humans, leptospirosis is seen in all different kind of domesticated animals, like cats, dogs, cattle and swine, but also in wild animals like mice, rats and possums. Symptoms can vary strongly between species and individuals and include fever, renal and hepatic failure, but also pulmonary manifestations and reproduction failure. Almost every mammal has been shown to be able to act as a carrier of leptospires without showing clinical signs. This in contrast to humans, who suffer more often acute infections and almost never become carriers. It is also known that some species serve as a particular reservoir for certain leptospirosis serovars. For example, it is known that mice and the black rat can be carriers of L. Ballum (Adler & de la Peña Moctezuma, 2010; Mansell & Benschop, 2014). These mice and rats can harbor the leptospires in their kidneys and shed it into their environment, without showing clinical signs themselves (Adler & de la Peña Moctezuma, 2010). 2 Leptospirosis in wildlife and domesticated household cats. Pilot study Introduction and aim of this study In New Zealand, six serovars of leptospirosis are endemic of which L. Hardjo, L. Pomona and L. Ballum are the three serovars responsible for the majority of human cases, and L. Ballum being the serovar most identified in human cases in 2010 (Mansell & Benschop, 2014). Hathaway et al. (1981) performed a study on the prevalence of leptospirosis in free-living species in New-Zealand. They found the highest seroprevalence in possums, hedgehogs, ship rats, Norway rats and the house mouse, varying between 5% (Norway rats) and 56% (possums). Of the kidney cultures performed in this study, the prevalence varied between 1637%. Possums were mostly infected by L. Balcanica, while of the rodents, L. Ballum was the isolate most identified. Of the hedgehogs only the serogroep Ballum was determined, but not the serovar. Four years before that research, Brockie (1977) already isolated L. Ballum in the ship rat, the Norway rat and the house mouse from dairy farms mainly in the North Island. He also found L. Copenhageni in the Norway rat. In a study by Hathaway & Blackmore (1981), the prevalence of L. Ballum in both black and brown rats were respectively 34% and 26%. There is some old literature about prevalences of leptospirosis in mice, rats, possums and hedgehogs in New Zealand. Whereas there is an increasing number of humans infected with L. Ballum (Mansell & Benschop, 2014), the question remains what the role of wildlife at the moment is in the epidemiology of human leptospirosis in the sub-urban area. Therefore, it is tried to catch as much animals as possible to collect their kidneys, blood and urine to gain more information about their infection status. The kidneys and urine will be used to search for the live leptospires and the blood samples will be used to search for antibodies against leptospirosis. The situation for domesticated house cats is a bit different. These animals are common pets in New Zealand and up to 1.4 million households keep them (MacKay et al., 2011). Different studies have been done in different countries to the prevalence of leptospiral antibodies in cats, varying between 4,8 and 35%. There is also evidence that cats are able to shed leptospires intermittently in their urine for several weeks after experimental infection. Although there have been some cases reported in the field of cats becoming ill of the bacteria, it is still thought that cats are resistant against the acute stage of leptospirosis (Rodriquez et al., 2012). In New Zealand, there has been a serological survey among cats as well. This study by Shophet (1979) showed the seroprevalence of 11 different serovars among 225 cats with a microscopic agglutination test (MAT). A total of 20 samples (8,8%) gave positive titres of which L. Copenhageni, L. Hardjo (both five), L. Ballum and L. Pomona (both four) were most determined serovars. While the study of Sophet (1979) is the latest research among cats in New Zealand, it is time to revisit this study to the infectious status of pet cats. It is still not known what the role of cats is in the epidemiology of human leptospirosis in New Zealand, despite the fact that they live in close contact with humans throughout this country. In contrast to the wildlife part of the study, it is not possible to gain the kidneys of these animals and perform a PCR and/or culture. Therefore, we try to collect blood samples of domesticated house cats to search for antibodies, which gives us an indication what serovar these cats come in contact with. It would also be interesting to compare the Leptospirosis serovars of domesticated house cats with the wildlife species. 3 Material and methods In order to catch possums in sub-urban areas, we used a total of ten steel possum cages of which five were hook- and the other five were plate cages for a period of four weeks. Some possums were caught by kill traps by the regional council and delivered for research to leptospirosis. For the collection of rats, we used five wooden, closed stoat cages. All cages were checked daily. Possum- and stoat traps were set out on different spots throughout the (sub-) urban part of the city Palmerston North. The bait used in the possum cages were apples (Cowen, 1987). The stoat cages were filled with bait containing apple and peanut butter to attract rats (Wilson et al., 2007). Once the animals were trapped alive, they were killed by carbondioxide (CO2) gas by putting the cage in a plastic bag and filling this bag with CO2. After killing, the animals were sexed and at least 2 ml of blood was collected immediately by heart puncture with a 21G 1 TW (0.8mm x 25 mm) BD PrecisionGlide™ Needle and a BD 10ml Syringe and put in a 10 ml BD Vacutainer Serum. If not enough blood could have been collected, the jugular vene was cut through and blood was caught in the 10 ml BD Vacutainer Serum directly. If possible, urine was collected also with a 21G 1 TW (0.8mm x 25 mm) BD PrecisionGlide™ Needle and a BD 10ml Syringe and put in a 10 ml BD Vacutainer®. The kidneys were taken out aseptically the same day and put in a transparent lock-zip plastic bag. After that, they were dissected following the protocol in appendix 1 resulting in a 1,5ml Eppendorf® cup with 800 μl dilution for the DNA extraction and one to three samples used for culturing the leptospires in a Ellinghausen-McCullough-Johnson-Harris (EMJH) medium (appendix 1). Until the 18th of February 2015, one culture per fresh kidney sample was used and from the 19th of February 2015 the dilution of three cultures per fresh kidney sample was used, as written in the appendix. These cultures can be read for 13 weeks before being discarded, because of the slow growth of this bacteria (Adler & de la Peña Moctezuma, 2010). The collected urine samples were submitted to DNA extraction following the protocol included in the QIAamp DNA mini kit (QIAGEN, Germany). The DNA extraction of all the kidney samples was performed with use of the High Pure PCR Template Preparation Kit (Roche, Mannheim, Germany) following the manufacturer’s instructions. Only 160 μl out of the total 800 μl of every kidney sample was used. The 640 μl leftover was put back in the -80°C freezer being held as a back-up sample. This resulted in final kidney DNA samples of 200 μl each to be used for the PCR. The wildlife blood samples were within four hours after collection centrifuged in a Heraeus multifuge 1S-R centrifuge at 3000 rpm for 10 minutes to separate the serum from the red blood cells. After centrifugation, the blood was stored in the -5°C fridge for a maximum of 10 days. For the domesticated house cats, we used a total of 180 serum samples from the New Zealand Veterinary Pathology (NZVP) laboratories. These samples were sent to the NZVP for all different kind of reasons, both sick and healthy animals. All samples were used, so no samples were discarded because of hemolysed serum or other reasons. Of all the collected blood samples, three masterplates were made to use for the Microscopic Agglutination Test (MAT): one for the wildlife samples and two for the domesticated house cat samples. The protocol for the preparation of the masterplate can be found in appendix 2. The MAT was performed as described by Cole et al. (1973). The collected blood samples 4 were investigated for the presence of antibodies against the four most common serovars in New Zealand: L. interrogans serovar , Pomona and Copenhageni and L. borgpetersenii serovar Ballum. The cut-off titre of ≥48 was used for differentiation between negative and positive seroprevalence (Dreyfus, 2013). Results After the trapping period of four weeks, a total of seventeen mature possums were collected. Four of them were caught by a kill trap and thirteen of the possums were caught by live traps. Of the total of seventeen possums caught dead or alive, eight possums were carrying a juvenile possum with them. One juvenile possum was caught alone (without the mother) in a live trap. Animal Amount Possum adult 17 Besides the possums, a total of three stoats, five hedgehogs, one mouse and one rat were caught dead or alive (table 1). All birds Possum juvenile 9 in the traps were released immediately. Data on the performed Hedgehog 5 tests and the location where the different species were caught Stoat 3 can be found in appendix 4. Figure 1 shows the locations where Rat 1 one or more animals where caught (green balloon) or the spots Mouse 1 where no animals were caught (red balloon). Total 36 We were able to collect kidney samples of all caught animals. Table 1. Animals caught during study Blood samples were collected from 23 animals and a total of 7 urine samples were collected. Figure 1. Locations in Palmerston North where one or more cages were put down during the collecting period 5 Figure 1. Global distribution of the household cat samples investigated PCR kidney samples Of the 36 kidney samples taken during the four weeks of trapping, six animals were positive in the PCR, which was confirmed using PFGE (figure 3). Figure 3. Results of positive PCR results for the pulsed-field gel electrophoresis PCR urine samples Of the seven urine samples collected, one sample was found positive with the PCR, which was confirmed during PFGE (figure 3). 6 Kidney cultures Of the kidneys cultured, two were positive: one hedgehog and one possum. The hedgehog was positive for L. Ballum and the possum for L. Hardjo. Microscopic Agglutination Test Of the 23 wild animals of which blood was collected, six animals (26%) of which five possums and one hedgehog had one or more positive titres with a cut-off titre of ≥48 (Fang, 2014). One hedgehog was positive for L. Ballum (1:192). One possum was also positive for L. Ballum, but with a lower titre of 1:48. Another possum was also positive for L. Ballum with a titre of 1:48, but this animal had also a positive titre of 1:768 for L. Hardjo. Three possums were positive for L. Hardjo as well with titres of respectively 1:768, 1:1536 and 1:192. There are no positive titres found of the serovars Copenhageni and Pomona (table 2). Titre 1:48 1:96 1:192 1:384 1:768 1:1536 Total Hardjo 0 0 1 0 2 1 4 Ballum 2 0 1 0 0 0 3 Copenhageni 0 0 0 0 0 0 0 Pomona 0 0 0 0 0 0 0 Table 2. Titre results of the Microscopic Agglutination Test of the wildlife animals caught during the study Of the 180 household cat serum samples investigated, 59 samples (32,7%) were positive for one or more leptospirosis serovars on the MAT (table 3). Two cats (1,1%) had a positive titre of L. Hardjo with both a titre of 1:48. One cat had a positive titre of L. Pomona of 1:384 (0,6%). Eight cats (4,4%) had a positive titre of L. Copenhageni of which five cats had a titre of 1:48, two of 1:96 and one of 1:768. The serovar Ballum was with 56 positive MAT results the serovar most common in the cats investigated (31,1%). The titres varied between 1:48 up to 1:3072. The global results can be found in table 3, the more comprehensive results can be found in appendix 5. Titre 1:48 1:96 1:192 1:384 1:768 1:1536 1:3072 Total Hardjo 2 0 0 0 0 0 0 2 Ballum 18 18 7 6 4 2 1 56 Pomona 0 0 0 1 0 0 0 1 Copenhageni 5 2 0 0 1 0 0 8 Table 3. Titre results of the Microscopic Agglutination Test performed on cats from namely the Northern Island Of the 180 cats, six cats were positive for two serovars of which five were positive for the combination of L. Ballum and L. Copenhageni and one cat was positive for L. Ballum and L. Pomona. 7 Of the 180 cats, one cat was positive for three serovar, namely L. Hardjo, L. Ballum and L. Copenhageni. Wildlife combinations As can be seen in table 4, there are animals with more than one positive result for different tests. Of the six positive MAT results, there were three animals with just a positive MAT and the other three animals also had a positive PCR result. One of those three animals even had a positive culture on top of that. The other positive culture was combined with a positive kidney and urine PCR, but without a positive MAT. There are two animals with just a positive kidney PCR. The serovar involved in these individuals couldn’t be determined. Combinations found # of animals serovars Only positive MAT Positive MAT+ positive kidney PCR Positive MAT+ positive kidney PCR + positive culture Positive kidney PCR Positive kidney PCR + positive urine PCR+ positive culture 3 2 1 2 1 2x L. Ballum 1x L. Hardjo 2x L. Hardjo 1x L. Hardjo 2x unknown 1x L. Ballum Table 4. Overview of the combinations of positive test results found in the wildlife study 8 Conclusion and discussion In this study there have been a total of three weeks of trying to catch rats around people’s houses. Only two hedgehogs (of which one was released by the householder) were caught during 60 trapnights. So this trapping at individuals’ houses barely provided any animals for receiving data. It is more useful to put the traps down at places with high rat densities, as seen in the study of Wilson et al. (2007), where 31 rats in 100 trapnights were caught. It also can be that the wooden stoat cages are not good for capturing rats. Wilson et al. (2007) found that more rats are caught in cage traps than in Elliot traps. Elliot traps are closed traps and look more like the stoat traps than the cage traps do. Wildlife The MAT performed on the wildlife serum samples collected, shows that some animals captured for this research have been in contact with L. Ballum and some with L. Hardjo. L. Hardjo is antigenetically indistinguishable from L. Balcanica using MAT without further testing (Hathaway et al., 1978a). Because previous research showed that L. Balcanica is often present in possums, instead of L. Hardjo, it is likely that this is the case here as well, but this was not possible to perform in our laboratory (Hathaway et al., 1981). Hathaway et al. (1981) also found most positive serum samples in possums for both the Ballum and Hebdomadis serogroup (where both L. Hardjo and L. Balcanica belong to). They also found the highest seroprevalence of L. Ballum in hedgehogs, of which also the only positive hedgehog out of five was positive for in this research. That none of the animals have been found positive for L. Copenhageni and L. Pomona suggests that these serovars play a minor role in wildlife epidemiology in the sub-urban area. But more research should be done to the real prevalences of leptospirosis in the five species investigated in this study in which the results of this study can be used or added. The good thing is that a lot of tests in individual animals are combined and that most of these animals were relatively fresh, which makes investigation easier and more reliable: DNA and antibodies are not degraded yet and for the culture, live leptospires are needed. Household cats As can be seen in table 3 and appendix 5, antibodies against the serovar Ballum are by far most found among the household cats investigated. L. Hardjo, L. Pomona and to a lesser extend L. Copenhageni play a minor role in this species. Rodriguez et al. (2014) found that outdoor access and hunting lifestyles are significant risk factors for seropositivity in cats. It is known that the serovar most common in black rats and mice is L. Ballum (Mansell & Benschop, 2014) and that is exactly the same serovar most found among cats in this study. It is likely that cats get in contact with leptospirosis due to contact with infected rodents, although there is no information available of these cats about their hunting lifestyle or outdoor access. When we compare the results of the household cats to the study of Sophet (1979), there is a big difference in the percentage of total cats positive, but also of cats with positive antibodies against L. Ballum. Although his study is not for 100% comparable with this study (he used a cut-off value of ≥24 and with two positive serovars in the same cat, he only marked the highest titre as being positive), a difference of incidence for L. Ballum of 1,77% versus 31,1% is a big difference and suggests a higher presence of L. Ballum in the environment of humans. This is in correlation with the fact that in 2010, L. Ballum was the serovar most identified among human cases (Mansell & Benschop, 2014). 9 There is not much information available of the cats investigated. It is known that antibodies against leptospirosis are more common in outdoor cats and in known hunters (Rodriguez et al., 2014) but all information available of the cats used in this investigation was (often) a short history. There was also no urine available to investigate for live leptospires, which could provide more information about the shedding status of the individual. The study of Rodriguez et al., (2014) is therefore more comprehensively, because there was more information available about the cats due to a questionnaire for the owner. For a follow-up of this research, it would be useful to combine urine samples with blood samples to gain a more complete view of the shedding status of the cats. Also, the questionnaire for owners used in the study of Rodriguez et al., (2014) about the behavior of their cat would be useful to gain more information about the behavior of infected and non-infected cats to find any risk factors. The cut-off titre for the MAT of ≥48, which has been used by both Dreyfus (2013) and Fang (2013) is a bit arbitrary. A human case will be confirmed for example when the person has a titre of 400 or higher (World Health Organisation, 2011). Often, a cut-off value of 100 and higher is considered indicative for infection (Fang, 2013). On the other hand it has been seen that cattle in New Zealand which were actively shedding, sometimes did have lower MAT titres (in this case of L. Hardjo) than ≥100 (Mackintosh et al. 1980; Ellis et al. 1986) so it’s not clear what the ideal cut-off titre has to be. That is why is chosen for the same cut-off titre as Dreyfus (2013) and Fang (2014). Another tool for confirmation of an infection with leptospirosis is a fourfold or greater rise of the MAT titre (Fang, 2013). In that case, it is possible to distinguish between animals with a low titre. The animals with a low titre in the acute phase will show an incline of the MAT titre, while the animals with a low titre and a past infection will not show a rise and might even show a decline. With only a single titre available of the 23 wildlife animals and 180 cats used for this research, nothing can be said about the phase of infection of the animals with lower titres. So for a follow up study, it would be useful to collect paired titres when possible because that provides more information. As can be seen in appendix 4, two possums and one hedgehog are positive for both the MAT and the PCR on the kidneys. These MAT titres vary between 1:192 and 1:1536 and in all cases they were positive MAT results for L. Hardjo. The PCR method is a really sensitive and specific method, but the disadvantage is that it is not possible to differentiate between different serovars (O’Keefe, 2002). While these MAT results correspond with a positive PCR result, it is likely that the PCR tested positive on L. Hardjo. The one possum that was positive for MAT, kidney PCR and kidney culture showed the presence of L. Hardjo in the culture and antibodies against this same serovar, so these test results match with each other. That is why the combination of tests is relevant. With only the PCR, it is known that leptospires are present, but it is unknown what serovar is involved. With only the MAT, it is known that the individual has been in contact with a certain serovar, but nothing can be said about the actual infection status of that individual. If animals are positive for both PCR and MAT, the serovar can be determined and it is known that that animal is actually shedding the bacteria. That the combination of tests performed provides more information is also seen in the case of Hedgehog 44. The serovar, L. Ballum, has been determined based on the positive culture, despite of the absence of a positive MAT. Besides this positive culture, this hedgehog was positive on the PCR for both the urine and kidney. The explanation of the fact that three PCR positive animals didn’t have a corresponding MAT titre is that it can be that the infection is too acute and that no antibodies against leptospires are produced yet. Fang (2014) did research to the comparison of both urine and kidney PCR results and the seroprevalence of 10 the same individuals in cows and sheep. He found out that approximately 40% of the seropositive animals had a positive PCR for both urine and kidney and that approximately 3% of the seronegative animals had a positive PCR result for their urine or kidney. It is possible that three animals caught in this study were in the acute phase of infection, but this would be a coincidence. Another explanation for a negative MAT result, in combination with a positive PCR result is that the MAT is not specific enough, but Adler & de la Peña Moctezuma (2010) state that the MAT is a highly specific and sensitive method, so this theory is unlikely as well. Perhaps, the study of Fang (2014) in sheep and cows cannot be extrapolated to wildlife. In short: a high prevalence of L. Ballum has been found in domesticated house cats. In wildlife, both L. Ballum and L. Hardjo have been isolated. The majority of human cases are caused by L. Ballum, L. Hardjo and L. Pomona (Mansell & Benschop, 2014). Although it is still unclear what the exact role of both domesticated house cats and wildlife is in the epidemiology of humans, the information obtained by this research is indicative that both groups might play a role in the epidemiology of at least L. Ballum and L. Hardjo. 11 Appendix 1. Protocol for kidney dissection 1. Weight the kidneys together at the weighting scale and write down the weight of the kidneys together. 2. Turn the fume cupboard on and take the kidneys to the fume cupboard. 3. Take for each kidney sample one (and from the 19th of February three) bottle(s) containing the Ellinghausen-McCullough-Johnson-Harris (EMJH) medium out of the fridge and leave it at room temperature for at least 30 minutes. 4. Undo the kidney of its capsule with your forceps. 5. Take a total amount of 10 grams (estimated) of the kidneys and drench it with Ethanol 70% above a funnel and flask. If the kidneys weight less than 10 grams, then take both entire kidneys. 6. Flame the kidneys with the Bunsen burner for a few seconds until the entire surface is egally grey/brown. 7. Put the kidneys in a Stomacher® bag and add an amount of 5 ml per gram kidney, with a maximum of 50 ml 0,01M Phosphate Buffer Saline (PBS). 8. Put the Stomacher® bag in the Colworth stomacher 400 (AJ Seward Ltd, London, United Kingdom) and wait for 1 minute. If the total amount of kidneys is <2 grams, crush the kidneys for at least 1 minute manually with a blunt object until they are well crushed. 9. Take the Stomacher bag out of the Colworth stomacher 400 and see if the kidneys are well crushed. 10. If they are not well crushed enough, repeat step 7 & 8. 11. Take an 1,5 ml Eppendorf cup (Raylab, Auckland, New Zealand) for each sample and write the sample number on top. 12. Put 800 μl of fluid out of the bag into the destinated Eppendorf cup using a Gilson Pipetman P200. 13. Put the 1,5 ml Eppendorf cup in the -20°C freezer 14. Label each EMJH medium with Mark, species, animal number, date and dilution. 15. Put 100 μl of fluid out of the bag into an EMJH medium (dilution 0) using a Gilson Pipetman P200. 16. From the 19th of February: take 100 μl of fluid out of the EMJH medium dilution 0 and put it in a new EMJH medium (dilution -1) and repeat this step one more time for the dilution -2. 17. Put the EMJH medium in the 38°C 18. Discard the Stomacher® bags. 12 Appendix 2. Protocol for preparation of a masterplate 1. Centrifuge all the samples in numbered vacutainers at 3000rpm for 10min in a Heraeus multifuge 1S-R centrifuge. 2. Determine in which well of the Greiner Bio One microplate (REF 655161) you want to put which sample (from vacutainers) and write this down on the Masterplate-paper. 3. Fill the wells for the vacutainer samples with 150μl sterile saline with a Gilson Pipetman L Multi 20 μl-300 μl pipet. 4. Take 30μl of the serum/supernatant from the vacutainer with a Gilson Pipetman Classic™ P200 pipet and put it in the right well with the saline. 5. Take the rest of the serum/supernatant with a Gilson Pipetman Classic™ P200 pipet and put it in a backup sample tube. 6. Write the sample number on the lid of the backup sample tube, and on the tube itself: Mark, sample number, date. 7. Put Parafilm “M” (Pechiney Plastic Packaging, Chicago, IL, USA) on top of the Greiner Bio One microplate (REF 655161) and put the lid on the microplate. 8. Put the Greiner Bio One microplate (REF 655161) in a zip-lock bag and close the ziplock bag. 9. Put the zip-lock bag in the -20°C freezer. 10. Put the backup sample tubes from step 13 in a backup sample box. 11. Name the backup sample box: Mark 1 Lepto 2015. Write down which backup samples are in which backup sample box. 12. Put the backup sample box in the freezer (-80°C). 13. Discard the used and empty vacutainers. 13 Appendix 3. Total list of trap dates, locations, type of cages and animals caught 11-Feb 12-Feb 13-Feb 6 Plate cage 7 Plate cage 4 Plate cage 5 Plate cage 3 Hook cage 1 Hook cage 2 Hook cage 108 Atawhai rd 108 Atawhai rd 108 Atawhai rd 108 Atawhai rd 7 Fernwood rd 118 Clifton cr 42 The Strand P x x x x x P P x x x*** x P P C x x*** x x x P x x B x x 13 Stoat trap 11 Stoat trap 12 Stoat trap 10 Stoat trap Stoat trap 8 Plate cage/ kill 9trap 66 Pahiatua st 50A Lockhart av 50A Lockhart av 50A Lockhart av 50A Lockhart av 50A Lockhart av x x x x x x x x x x x x x x x x x P (KT) x x x x x x (KT) 8 Plate cage 6 Plate cage 7 Plate cage 4 Plate cage 5 Plate cage 3 Hook cage 1 Hook cage 2 Hook cage 108 Atawhai rd 108 Atawhai rd 108 Atawhai rd 108 Atawhai rd 108 Atawhai rd 108 Atawhai rd108 Atawhai rd 66 Pahiatua st H x x x H x P P H * x P x x x x x x x** x B x x 13 Stoat trap 11 Stoat trap 12 Stoat trap 10 Stoat trap 9 Stoat trap 50A Lockhart av 50A Lockhart av 50A Lockhart av 50A Lockhart av 50A Lockhart av x x x x H* x x x x H x x x x x 17-Feb 18-Feb 19-Feb 20-Feb 12 Hook cage 156 Aokautere drive x x x x*** 8 Kill Trap 66 Pahiatua st x x x x 11 Plate cage 9 la Lena gr x x x x 6 Plate cage 7 Plate cage 4 Hook cage 5 Plate cage 3 Hook cage 1 Hook cage 2 Hook cage 108 Atawhai rd Acacia Birch 3c Acacia Birch 3c Acacia Birch 3c 7 Fernwood rd 118 Clifton cr 42 The Strand x x P x x x x B x x x x x x P x P x x x x B x x x x x x 10 Plate cage 9 la Lena gr x P x H* 24-Feb 25-Feb 26-Feb 27-Feb 4. Stoat trap 5. Stoat trap 1. Stoat trap 2. Stoat trap 3. Stoat trap 5 Newland crt 5 Newland crt 5 Newland crt 5 Newland crt 5 Newland crt x x x x x x x x x x x x x x x x x x x x x x x x x 9 Kill Trap 122 Atawhai rd x x P x 27-Feb 2-Mar 3-Mar 4-Mar 5-Mar x= empty P= Possum H= Hedgehog H*= Hedgehog released by householder St= Stoat B= Bird KT= Kill Trap *= cage disappeared x**= cage sabotaged with flour x***= cage closed, bait gone, no animal 14 Appendix 4. Comprehensive list of animals caught, tests performed and test results 15 Appendix 5. Comprehensive results of positive (≥48) MAT titres cats Hardjo Ballum Pomona Copenhageni Age Gender District P15000804 1:96 15Y C Whanganui P15000819 1:384 16Y F South Taranaki P15000842 1:96 6Y S Wellington City P15000850 1:96 16Y M Gisborne P15000897 1:1536 16Y S Wellington City P15000898 1:48 15Y C Whanganui P15000919 1:768 9Y C Central Hawkes Bay P15000928 1:96 13Y C Kapiti Coast P15000943 1:384 15Y M South Taranaki P15000954 1:48 12Y S Tasman 1:3072 16Y C Wellington City P15001055 1:1536 14Y C Porirua City P15001059 1:96 12Y C Porirua City P15001070 1:96 16Y S Porirua City P15001072 1:48 14Y S Porirua City P15001104 1:96 13Y C New Plymouth P15001202 1:48 15Y U Kapiti Coast P15001205 1:48 14Y C Porirua City P15001220 1:768 1:96 9Y C Wellington City P15001226 1:48 1:48 9Y S Wellington City P15001234 1:48 18Y S Palmerston North P15001238 1:48 13Y C Horowhenua P15001265 1:768 15Y F Manawatu P15001288 1:192 14Y M Hastings 1:24 13Y S Porirua City P15001302 1:192 8Y F Wellington City P15001305 1:48 14Y S Kapiti Coast P15001353 1:768 13Y F Lower Hutt City P15001359 1:384 P15001366 1:96 P15000989 P15001299 1:24 1:48 1:96 14Y C Marlborough 1:48 UN S Horowhenua P15001369 1:48 16Y F Gisborne P15001376 1:48 4Y S Porirua City P15001404 1:192 5Y C Palmerston North P15001416 1:192 3M C Whanganui P15001426 1:96 11Y S Wellington City P15001433 1:192 UN U Wellington City P15001436 1:192 15Y C Wellington City P15001444 1:96 4Y M South Taranaki P15001450 1:96 13Y S Wellington City P15001519 1:96 9Y C Palmerston North P15001538 1:384 13Y M Hastings P15001539 1:48 16Y F Kapiti Coast 1:24 1:384 1:24 16 P15001550 1:96 P15001554 13Y M Porirua City 1:48 17Y F Wellington City P15001566 1:48 9Y M Hastings P15001612 1:48 13Y C Wellington City P15001615 1:48 15Y C Kapiti Coast P15001624 1:384 14Y S Porirua City P15001628 1:96 1:24 17Y C Wellington City P15001695 1:48 1:24 13Y F Manawatu P15001723 1:96 10Y C Wellington City P15001728 1:48 18Y S Central Hawkes Bay P15001795 1:96 9Y F Manawatu P15001813 1:384 10Y S Wellington City P15001817 1:48 11Y C Kapiti Coast P15001819 1:48 13Y S Wellington City P15001821 1:192 10Y C Wellington City P15001823 1:96 1:768 14Y C Wellington City 1:96 1:48 5Y M South Taranaki P15001829 M= F= C= S= U= 1:48 1:24 Male Female Male castrated Female speyed Unknown 17 Literature Adler, B., & de la Peña Moctezuma, Alejandro. (2010). Leptospira and leptospirosis. Veterinary Microbiology, 140(3-4), 287-96. doi:10.1016/j.vetmic.2009.03.012 Bharti, A., Nally, J., Ricaldi, J., Matthias, M., Diaz, M., Lovett, M., . . . Vinetz, J. (2003). Leptospirosis: a zoonotic disease of global importance. The Lancet Infectious Diseases, 3(12), 757-71. Brockie, R. E. (1977). Leptospiral infections of rodents in the North Island. New Zealand veterinary journal, 25(4), 89-96. Cowan, P. E. (1987). The influence of lures and relative opportunity for capture on catches of brushtail possums, Trichosurus vulpecula. New Zealand journal of zoology, 14(2), 149-161. Dreyfus, A. (2013). Leptospirosis in humans and pastoral livestock in New Zealand. PhD thesis, Massey University, Palmerston North, New Zealand. Ellis, W. A., Songer, J. G., Montgomery, J., & Cassells, J. A. (1986). Prevalence of Leptospira interrogans serovar in the genital and urinary tracts of non-pregnant cattle. The Veterinary Record, 118(1), 11-13. Faine, S., Adler, B., Bolin, C. & Perolat, P. (1999). Leptospira and Leptospirosis, 2nd edn. Melbourne: MedSci. Fang, F. (2014). Leptospirosis diagnostics and exposure at the human and animal interface in New Zealand. PhD thesis, Massey University, Palmerston North, New Zealand. Haake, D., & Levett, P. (2015). Leptospirosis in humans. Current Topics in Microbiology and Immunology, 387, 65-97. doi:10.1007/978-3-662-45059-8_5 Hartmann, K., Egberink, H., Pennisi, M. G., Lloret, A., Addie, D., Belák, S., ... & Horzinek, M. C. (2013). Leptospira Species Infection in Cats ABCD guidelines on prevention and management. Journal of feline medicine and surgery, 15(7), 576-581. Hathaway, S. C., & Blackmore, D. K. (1981). Ecological aspects of the epidemiology of infection with leptospires of the ballum serogroup in the black rat (rattus rattus) and the brown rat (rattus norvegicus) in new zealand. The Journal of Hygiene, 87(3), 427-36. Hathaway, S. C., Blackmore, D. K., & Marshall, R. B. (1981). Leptospirosis in free-living species in New Zealand. Journal of Wildlife Diseases, 17(4), 489-96. 18 Hathaway, S.C. (1978). Leptospirosis in free-living animals in New Zealand, with particular reference to the possum (Trichosurus Vulpecula). PhD thesis, Massey University, Palmerston North, New Zealand. Mackintosh, C. G., Marshall, R. B., & Broughton, E. (1980). The use of a -pomona vaccine to prevent leptospiruria in cattle exposed to natural challenge with Leptospira interrogans serovar . New Zealand Veterinary Journal, 28(9), 174-177. MacKay, J., & NZCAC (New Zealand Companion Animal Council Incorporated). (2011). Companion animals in New Zealand. Mansell, C., & Benschop, J. (2014). Leptospirosis is an important multi-species zoonotic disease in New Zealand. New Zealand Medical Journal, 127(1388), 5-8. O'Keefe, J. S. (2002). A brief review on the laboratory diagnosis of leptospirosis. New Zealand Veterinary Journal, 50(1), 913. Rodriguez, J., Blais, M., Lapointe, C., Arsenault, J., Carioto, L., & Harel, J. (2014). Serologic and urinary PCR survey of leptospirosis in healthy cats and in cats with kidney disease. Journal of Veterinary Internal Medicine, 28(2), 284-93. doi:10.1111/jvim.12287 Rodriguez, J., Lapointe, C., Carioto, L., & Harel, J. (2012). Feline leptospirosis: A serologic and urinary pcr survey in healthy cats and in cats with kidney disease. Philadelphia: J.B. Lippincott. Seguro, A., & Andrade, L. (2013). Pathophysiology of leptospirosis. Shock, 39 Suppl 1, 17-23. doi:10.1097/SHK.0b013e31828fae49 Shophet, R. (1979). A serological survey of leptospirosis in cats. New Zealand Veterinary Journal, 27(11), 236-6. doi:10.1080/00480169.1979.34662 Wilson, D. J., Efford, M. G., Brown, S. J., Williamson, J. F., & McElrea, G. J. (2007). Estimating density of ship rats in New Zealand forests by capture-mark-recapture trapping. New Zealand Journal of Ecology, 31(1), 47. World Health Organization (2011). Report of the Second Meeting of the Leptospirosis Burden Epidemiology Reference Group. 62 http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&gid=19163&Itemid=2518 (accessed September 2013), Geneva 19