C2015_Worksheet_ALS_Vasopressors in cardiac
advertisement

C2015 ALS_Vassopressors in cardiac arrest_220912
WORKSHEET for Evidence-Based Review of Science for Emergency Cardiac Care
Worksheet author(s)
Laurie MORRISON and Clifton CALLAWAY and Steve LIN
Date Submitted for review 20 October 2012 Reviewed by Taskforce
Dallas Nov 2014 Resubmitted for E3 and GRADE review Dec 31 2014
formatting changes January 2 2015.
Clinical question.
In adult patients in cardiac arrest (asystole, pulseless electrical activity, pulseless VT and VF) (OHCA)[P], does the use of vasopressors
(epinephrine, norepinephrine, others) or combination of vasopressors [I], compared with not using drugs (or a standard drug regime)(C), improve
outcomes (eg ROSC, survival)[O]?
Population: Adults in cardiac arrest (asystole, pulseless electrical activity, pulseless VT and VF) (OHCA / IHCA)
Intervention: vasopressors
Comparison: no drugs /standard drug regime/ different drug dosage/ combination of drugs
Outcomes:
ROSC (important 5)
Survive with ROSC to ED Arrival (Important 6)
Survive to 24 hours post ED Arrival (Critical 7)
Survival to hospital discharge (Critical 8)
Neurologically intact survival (Critical 9)
Is this question addressing an intervention/therapy, prognosis or diagnosis: Intervention
State if this is a proposed new topic or revision of existing worksheet: Revision [http://circ.ahajournals.org/site/C2010/ALS-D-023B.pdf/]
Conflict of interest specific to this question
Do any of the authors listed above have conflict of interest disclosures relevant to this worksheet?
Dr Cliff Callaway is an author on one of the RCTs reviewed in this worksheet. Both authors are funded by the NIH to participate in the ROC consortium and
are designing an RCT to evaluate the therapeutic dosage of epinephrine in OHCA.
Search strategy
SEARCH STRATEGY for RCTs
Database: Ovid MEDLINE(R) <1946 to April Week 1 2012>, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations <April 16, 2012>
This search was not updated due to time constraints and the relatively small chance that an RCT involving Epinephrine and Placebo would have been
published without the knowledge of the taskforce..
Search Strategy:
-------------------------------------------------------------------------------1 exp Heart Arrest/ (29918)
2 cardiac arrest.tw. (17150)
3 cardiovascular arrest.tw. (43)
4 heart arrest.tw. (530)
5 cardiopulmonary arrest.tw. (1331)
6 cardiopulmonary resuscitation.mp. (12991)
7 asystole.mp. (2449)
8 pulseless electrical activity.mp. (387)
9 Advanced Cardiac Life Support.mp. (1212)
10 ACLS.tw. (696)
11 Ventricular Fibrillation/ (14018)
12 or/1-11 (56270)
13 exp Epinephrine/ (110644)
14 exp Vasopressins/ (32578)
15 (Epinephrine or vasopressin* or adrenaline).tw. (70364)
16 Injections, Intravenous/ (74860)
17 or/13-16 (236047)
18 double-blind method/ or random allocation/ or single-blind method/ (193111)
19 random*.mp. (753836)
20 placebo*.mp. (153201)
21 or/18-20 (818302)
22 12 and 17 (2745)
23 limit 22 to randomized controlled trial (105)
24 21 and 22 (477)
25 23 or 24 (477)
26 limit 22 to meta analysis (5)
27 limit 22 to "reviews (best balance of sensitivity and specificity)" (311)
28 25 or 26 or 27 (738)
29 remove duplicates from 28 (735)
C2015 ALS_Vassopressors in cardiac arrest_220912
30
31
32
33
limit 29 to animals (386)
limit 30 to humans (92)
30 not 31 (294)
29 not 32 (441)
***************************
Database: Embase Classic+Embase <1947 to 2012 Week 15>
Search Strategy:
-------------------------------------------------------------------------------1 exp heart arrest/ (41597)
2 cardiac arrest.tw. (24481)
3 cardiovascular arrest.tw. (56)
4 heart arrest.tw. (595)
5 cardiopulmonary arrest.tw. (1676)
6 heart ventricle fibrillation/ (24087)
7 exp asystole/ (3640)
8 or/1-7 (68348)
9 exp adrenalin/ (108478)
10 exp vasopressin/ (31144)
11 (Epinephrine or vasopressin* or adrenalin*).tw. (103790)
12 or/9-11 (168570)
13 8 and 12 (4813)
14 limit 13 to randomized controlled trial (121)
15 double blind procedure/ (112829)
16 exp randomization/ (58015)
17 single blind procedure/ (15729)
18 random*.tw. (739312)
19 placebo*.mp. (292567)
20 or/15-19 (961590)
21 13 and 20 (599)
22 limit 13 to (meta analysis or "systematic review") (59)
23 limit 13 to "reviews (best balance of sensitivity and specificity)" (779)
24 14 or 21 or 22 or 23 (1281)
25 remove duplicates from 24 (1264)
26 limit 25 to embase (1162)
27 limit 26 to (animals or animal studies or (ape or cat or cattle or chicken or dog or "ducks and geese" or goat or guinea pig or "hamsters and gerbils" or
horse or monkey or mouse or "pigeons and doves" or "rabbits and hares" or rat or sheep or swine)) (302)
28 limit 27 to human (32)
29 27 not 28 (270)
30 26 not 29 (892)
Database: EBM Reviews - Cochrane Central Register of Controlled Trials <April 2012>, EBM Reviews - Cochrane Database of Systematic Reviews <2005 to
March 2012>, EBM Reviews - Database of Abstracts of Reviews of Effects <1st Quarter 2012>, EBM Reviews - Cochrane Methodology Register <2nd Quarter
2012>, EBM Reviews - Health Technology Assessment <2nd Quarter 2012>
Search Strategy:
-------------------------------------------------------------------------------1 exp Heart Arrest/ (849)
2 cardiac arrest.tw. (984)
3 cardiovascular arrest.tw. (2)
4 heart arrest.tw. (83)
5 cardiopulmonary arrest.tw. (59)
6 cardiopulmonary resuscitation.mp. (645)
7 asystole.mp. (143)
8 pulseless electrical activity.mp. (25)
9 Advanced Cardiac Life Support.mp. (103)
10 ACLS.tw. (47)
11 Ventricular Fibrillation/ (410)
12 Ventricular Fibrillation.tw. (680)
13 or/1-12 (2454)
14 exp Epinephrine/ (3928)
15 exp Vasopressins/ (976)
16 (Epinephrine or vasopressin* or adrenalin*).tw. (6034)
17 or/14-16 (8124)
C2015 ALS_Vassopressors in cardiac arrest_220912
18
13 and 17 (146)
***************************
In addition, we hand searched bibliographies of previous systematic reviews and the 2010 update of ILCOR Consensus Statement and Treatment
Recommendations for advanced life support. We also searched online resources such as BestBETS (available at http://www.bestbets.org/) and the first
200 hits of Google ScholarTM. Ongoing clinical trials and unpublished studies were searched using the following sites: http://www.clinicaltrials.gov,
http://www.controlledtrials.com, and http://www.centerwatch.com. Non-English titles, abstracts, and manuscripts were translated and evaluated for
inclusion. Industrial contacts and first authors in each of the selected studies were contacted to ask for unpublished trials and none were identified.
• State inclusion and exclusion criteria
Included all randomized controlled trials examining the use of vasopressors in adult cardiac arrest. Excluded studies neonatal studies, paediatric studies,
animal studies and studies that did not specifically address the PICO question. Excluded studies only published in abstract form, unless accepted for
publication.
• Number of articles/sources meeting criteria for further review:
There were 1190 potential citations identified by the literature search after the duplicates were deleted. Of these, we identified 14 RCTs eligible for inclusion.
The details of study selection including reasons for exclusion are outlined in the figure 1. The kappa values ranged from 0.88 to 1.00 at the hierarchical
selection of titles, abstracts and full manuscripts. The 14 included RCTs comprised of 2,246 patients (range, 40-3327 patients) in nine countries. All studies
were published in English
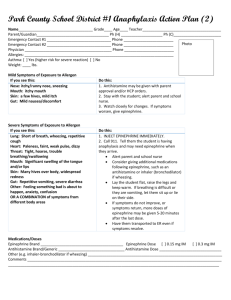
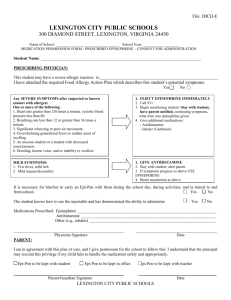
Figure 1. Flow chart of study selection process.
1190 citations retrieved from
literature search
884 irrelevant citations
excluded
306 relevant citations screened for
abstract retrieval
282 abstracts excluded:
266 not RCTs
1 pediatric
15 not specified intervention
24 manuscripts retrieved for
detailed evaluation
10 manuscripts excluded:
6 not RCTs
4 not specified intervention
14 RCTs included for analysis:
1 – Epinephrine vs. Placebo
1 – Epinephrine vs. Vasopressin
6 – Standard dose vs. High dose epinephrine
6 – Epinephrine vs. Vasopressin/Epinephrine
Here are the search strings for the re-run of the Vasopressors for cardiac arrest search, but limited to observational studies (prospective cohort,
before and after, propensity, retrospective) since 2010:
PubMed
113 results
C2015 ALS_Vassopressors in cardiac arrest_220912
((((((("Heart Arrest"[Mesh] OR "cardiac arrest"[TIAB] OR "cardiovascular arrest"[TIAB] OR "heart arrest"[TIAB] OR "asystole"[All Fields]
OR "pulseless electrical activity"[All Fields] OR "Advanced Cardiac Life Support"[All Fields] OR "ACLS"[TIAB] OR "Ventricular
Fibrillation"[Mesh:noexp] OR "cardiopulmonary resuscitation"[All Fields] OR "cardiopulmonary arrest"[TIAB]) AND ("Epinephrine"[Mesh]
OR "Vasopressins"[Mesh] OR ("Epinephrine"[TIAB] OR "vasopressin*"[TIAB] OR "adrenaline"[TIAB]) OR "Injections,
Intravenous"[Mesh:noexp])))) AND (((Prospective[TIAB] OR prospectively[TIAB] OR nonrandomized[TIAB] OR observational[TIAB] OR
propensity[TIAB] OR population-based[TIAB] OR retrospective[TIAB] OR registry[TIAB] OR registries[TIAB] OR cohort[TIAB] OR
matched[TIAB] OR "Registries"[Mesh:NoExp] OR "Epidemiologic Studies"[Mesh] OR "Matched-Pair Analysis"[Mesh] OR "Observational
Study" [Publication Type] OR "Observational Study as Topic"[Mesh]))))) AND 2010:2030[dp])
Embase
365 results
'heart arrest'/exp OR 'cardiac arrest':ab,ti OR 'cardiovascular arrest':ab,ti OR 'heart arrest':ab,ti OR 'cardiopulmonary arrest':ab,ti OR 'heart
ventricle fibrillation'/exp AND ('adrenalin'/exp OR 'vasopressin'/exp OR epinephrine:ab,ti OR vasopressin*:ab,ti OR adrenalin*:ab,ti) AND
(prospective:ab,ti OR prospectively:ab,ti OR nonrandomized:ab,ti OR observational:ab,ti OR propensity:ab,ti OR 'population based':ab,ti OR
retrospective:ab,ti OR registry:ab,ti OR registries:ab,ti OR cohort:ab,ti OR matched:ab,ti OR 'clinical study'/de OR 'case control study'/exp OR
'comparative study'/exp OR 'controlled study'/exp OR 'observational study'/exp OR 'cohort analysis'/exp OR 'longitudinal study'/de OR
'retrospective study'/exp OR 'prospective study'/exp OR 'register'/exp) AND (2010:py OR 2011:py OR 2012:py OR 2013:py OR 2014:py) NOT
('animal'/exp NOT 'human'/exp) AND [english]/lim AND [embase]/lim
There is no need to revise the Cochrane search string as I did not use any study design limits.
Cochrane
([mh "Heart Arrest"] or "cardiac arrest" or "cardiovascular arrest":ti,ab or "heart arrest":ti,ab or "asystole":ti,ab or "pulseless electrical
activity":ti,ab or "Advanced Cardiac Life Support":ti,ab or "ACLS":ti,ab or [mh ^"Ventricular Fibrillation"] or "cardiopulmonary
resuscitation":ti,ab or "cardiopulmonary arrest":ti,ab or "Ventricular Fibrillation":ti,ab) and ([mh Epinephrine] or [mh vasopressin] or
(Epinephrine or vasopressin* or adrenalin*):ti,ab)
Due to time constraints these were not filtered through SEERS or GRADE however EVREVs reviewed
1: Hagihara A, Hasegawa M, Abe T, Nagata T, Wakata Y, Miyazaki S. Prehospital
epinephrine use and survival among patients with out-of-hospital cardiac arrest.
JAMA. 2012 Mar 21;307(11):1161-8. doi: 10.1001/jama.2012.294. PubMed PMID:
22436956.
2: Nakahara S, Tomio J, Nishida M, Morimura N, Ichikawa M, Sakamoto T.
Association between timing of epinephrine administration and intact neurologic
survival following out-of-hospital cardiac arrest in Japan: a population-based
prospective observational study. Acad Emerg Med. 2012 Jul;19(7):782-92. doi:
10.1111/j.1553-2712.2012.01387.x. PubMed PMID: 22805628.
3: Nakahara S, Tomio J, Takahashi H, Ichikawa M, Nishida M, Morimura N, Sakamoto
T. Evaluation of pre-hospital administration of adrenaline (epinephrine) by
emergency medical services for patients with out of hospital cardiac arrest in
Japan: controlled propensity matched retrospective cohort study. BMJ. 2013 Dec
10;347:f6829. doi: 10.1136/bmj.f6829. PubMed PMID: 24326886; PubMed Central
PMCID: PMC3898161.
4: Hayashi Y, Iwami T, Kitamura T, Nishiuchi T, Kajino K, Sakai T, Nishiyama C,
Nitta M, Hiraide A, Kai T. Impact of early intravenous epinephrine administration
on outcomes following out-of-hospital cardiac arrest. Circ J. 2012;76(7):1639-45.
Epub 2012 Apr 5. PubMed PMID: 22481099.
5: Goto Y, Maeda T, Goto YN. Effects of prehospital epinephrine during
out-of-hospital cardiac arrest with initial non-shockable rhythm: an
observational cohort study. Crit Care. 2013 Sep 3;17(5):R188. [Epub ahead of
print] PubMed PMID: 24004456; PubMed Central PMCID: PMC3840562.
C2015 ALS_Vassopressors in cardiac arrest_220912
Characteristics of included RCT studies (alphabetical)
Epinephrine vs Placebo
First author Jacobs, Year 2011, 1138
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
All adult OHCA
1 mg epinephrine bolus dosages
placebo
ROSC, survival to discharge
Australian Prehospital Trial
Adult OHCAs (N= 534); Age, mean y ± SD, 64.3 ± 17.5 (Epi) and 64.9 ± 17.4 (placebo)
VF/pVT 43.8% (Epi) and 48.1% (placebo), PEA 33.5% (Epi) and 26.7% (placebo), asystole
22.8% (Epi) and 25.2% (placebo)
Witnessed 53.7% (Epi) and 58.0% (placebo);
Bystander CPR 52.9% (Epi) and 49.2% (placebo)
Stopped prematurely secondary to enrolment delay due to lack of provider support for the
trial
Epinephrine SD vs Vasopressin SD
First author Mukoyamo Year 2009, 755
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Vasopressin 40 IU up to 4 doses
Epinephrine 1 mg
ROSC, Survival to discharge
Japanese Emergency Department Trial
Adult OHCAs (N=336); Age, mean y ± SD, 63.7 ± 18.6 (Epi) and 66.9 ± 15.2 (Vaso)
VF 25.3% (Epi) and 23.0% (Vaso), PEA 13.9% (Epi) and 14.6% (Vaso), asystole 60.8%
(Epi) and 62.4% (Vaso)
Witnessed 45.6% (Epi) and 43.3% (Vaso);
Bystander CPR 16.5% (Epi) and 14.0% (Vaso)
Epinephrine SD vs Epinephrine HD
First author Brown, Year 1992, 1051
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Epinephrine 0.2 mg/kg single does
Epinephrine 0.02 mg/kg
ROSC , Survival to hospital discharge
US Prehospital Trial
Adult OHCAs (N=1280); Age, mean y ± SD, 66 ± 15 (SDE) and 66 ± 15 (HDE)
VF/pVT 50% (SDE) and 45.9% (HDE), PEA 18.4% (SDE) and 20.5% (HDE), asystole
31.7% (SDE) and 33.6% (HDE)
Witnessed 39% (SDE) and 36% (HDE) , unwitnessed 61% (SDE) and 64% (HDE);
Bystander CPR 24% (SDE) and 23% (HDE)
First author Callaham, Year 1992, 2667
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Epinephrine 1mg (SDE) (n=260),
15mg (HDE) (n=286) or NE 1mg (n=270), up to 3 doses
ROSC, Survival to DC
US Prehospital Trial
Adult OHCAs (N=816); Age, mean y ± SD, 65 ± 19 (SDE) and 66 ± 18 (HDE)
VF/pVT 24.4, PEA 28.8, asystole 46.8 of total study population
C2015 ALS_Vassopressors in cardiac arrest_220912
Witnessed 63 (SDE) and 63 (HDE); Bystander CPR 22 (SDE) and 29 (HDE)
First author Choux, Year 1995, 3
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Epinephrine 5 mg up to 15 doses
Epinephrine 1 mg
French MICU Prehospital Trial
Adult OHCAs (N=536); Age, mean y ± SD, 62 ± 19 (SDE) and 59 ± 18 (HDE)
VF 16 (SDE) and 18 (HDE), PEA 9 (SDE) and 10 (HDE), asystole 75 (SDE) and 72 (HDE)
Witnessed vs non witnessed and bystander CPR rates not reported by cohort
First author Gueugniaud, Year 1998, 1595
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Epinephrine 5 mg
Epinephrine 1 mg
ROSC, Survival to Discharge
French and Flemish MICU Prehospital Trial
Adult OHCAs (N=3327); Age, mean y ± SD, 67±15 (SDE) and 65±15 (HDE)
VF 15.9 (SDE) and 18.0 (HDE), PEA 9.5 (SDE) and 9.5 (HDE), asystole 74.6 (SDE) and
72.5 (HDE)
Witnessed 78.6 (SDE) and 79.1 (HDE);Bystander CPR: 9.3 (SDE) and 10.3 (HDE)
First author Sherman, Year 1997, 242
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Epinephrine 0.1 mg/kg up to 4 doses
Epinephrine 0.01 mg/kg
ROSC, Survival to DC
US Emergency Department Trial
Adult OHCAs (N=140); Age, mean y ± SD, 68±14 (SDE) and 65±14 (HDE)
VF 16 (SDE) and 31 (HDE), asystole 84 (SDE) and 69 (HDE)
Witnessed 74 (SDE) and 59 (HDE); Bystander CPR rates not reported
First author Stiell, Year 1992, 1045
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Epinephrine 7 mg up to 5 doses
Epinephrine 1 mg
ROSC, Survival to DC
Canadian Emergency Department Trial
Adult OHCAs (n=335) and in-hospital cardiac arrests (n=315); Age, mean y±SD, 67±15
(SDE) and 66±15
Rhythms other than VFVT not included
Witnessed and non witnessed and bystander CPR rates
Epinephrine SD vs Epinephrine/Vasopressin in Combination
First author Callaway, Year 2006, 1316
Methods
Participants
Interventions
Comparisons
RCT unblinded
Adult OHCA
Vasopressin 40IU or placebo after 1 mg initial dose of epinephrine (unblinded), single dose
Epinephrine 1 mg
C2015 ALS_Vassopressors in cardiac arrest_220912
Outcomes
Notes
ROSC, Survival to DC
US Prehospital Trial
Adult OHCAs (N=325); Age, mean y ± SD, 65 ± 17 (Epi) and 66 ± 17 (Epi/Vaso)
VF/AED shock 26 (Epi) and 29 (Epi/Vaso), PEA 23 (Epi) and 22 (Epi/Vaso), asystole 51
(Epi) and 50 (Epi/Vaso)
Witnessed 55 (Epi) and 48 (Epi/Vaso); Bystander CPR: 35 (Epi) and 31 (Epi/Vaso)
First author Ducros, Year 2011, 453
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT unblinded
Adult OHCA Witnessed
Vasopressin 40 IU or placebo or nitro after one dose open label Epinephrine for three doses
then open label SD epinephrine as per ACLS
Epinephrine 1mg
ROSC, Survival to DC
French MICU Prehospital Trial
Adult OHCAs (N=44); Age, mean y ± SE, 60 ± 4 (Epi) and 56 ± 4 (Epi/Vaso)
VF 0 (Epi) and 14 (Epi/Vaso), PEA 50 (Epi) and 21 (Epi/Vaso), asystole 50 (Epi) and 64
(Epi/Vaso)
All OHCA witnessed and received CPR by Firefighters prior to EMS arrival
First author Gueugniaud, Year 2008, 21
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
epinephrine 1mg and Vasopressin 40IU, up to 2 doses
Epinephrine 1 mg and placebo
ROSC, Survival to discharge
French MICU Prehospital trial
Adult OHCAs (N= 2894); Age, mean y ± SD, 62 ± 15 (Epi) and 61 ± 15 (Epi/Vaso)
VF 9.3 (Epi) and 9.2 (Epi/Vaso), PEA 8.3 (Epi) and 7.7 (Epi/Vaso), asystole 82.4 (Epi) and
83.1 (Epi/Vaso)
Witnessed 76.1 (Epi) and 74.3 (Epi/Vaso);
Bystander CPR 26.0 (Epi) and 27.7 (Epi/Vaso)
First author Lindner, Year 1997, 535
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA in VF only
Vasopressin 40 IU as a single dose followed by open label epinephrine SD as per ACLS
Epinephrine 1 mg
ROSC, survival to DC
German, Prehospital Trial
Adult OHCAs (N=40); Age, mean y ± SE, 66 ± 4 (Epi) and 64 ± 3 (Epi/Vaso)
VF only
Witnessed 60 (Epi) and 65 (Epi/Vaso);
Bystander CPR 25 (Epi) and 20 (Epi/Vaso)
First author Ong, Year 2012, 953
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Vasopressin 40 IU as a single dose followed by open label epinephrine SD as per ACLS
Epinephrine 1 mg
ROSC, survival to DC
Singapore, Emergency Department trial
Adult OHCAs (N=727); Age, mean y ± SD, 64.9 ± 15.4 (Epi) and 64.6 ± 14.2 (Epi/Vaso)
VF/pVT 8.5 (Epi) and 7.0 (Epi/Vaso), PEA 20.4 (Epi) and 17.6 (Epi/Vaso), asystole 67.4
(Epi) and 70.9 (Epi/Vaso)
C2015 ALS_Vassopressors in cardiac arrest_220912
Witnessed 75.1 (Epi) and 70.9 (Epi/Vaso);
Bystander CPR 14.2 (Epi) and 16.6 (Epi/Vaso)
First author Wenzel, Year 2004, 105
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT
Adult OHCA
Vasopressin 40IU up to two doses
Epinephrine 1 mg
ROSC, survival to DC
Austrian Emergency Department Trial
Adult OHCA (N=1186); Age, mean y ± SD, 65.9 ± 14.2 (Epi) and 66.5 ± 14.4 (Epi/Vaso
VF 41.7 (Epi) and 37.9 (Epi/Vaso), PEA 13.7 (Epi) and 17.7 (Epi/Vaso), asystole 44.6 (Epi)
and 44.5 (Epi/Vaso)
Witnessed 79.7 (Epi) and 76.8 (Epi/Vaso);
Bystander CPR 17.9 (Epi) and 18.8 (Epi/Vaso)
Characteristics of included Excluded RCT studies deemed of interest
(alphabetical)
First author Olasveengen, Year 2009, 2222
Methods
Participants
Interventions
Comparisons
Outcomes
Notes
RCT (Excluded)
All adult OHCA
No intravenous (no drugs)
SDE and ALS care
Survival to Discharge, Survival at one year, Functional survival using CPC, hospital
admission with ROSC, Quality of CPR
Adult OHCAs (851) where 95 eligible not randomized, and 45 in the no intravenous group
and 74 in the intravenous group were post randomization exclusions.
No significant difference in utstein criteria across groups (randomization was kind)
C2015 ALS_Vassopressors in cardiac arrest_220912
And Observational Studies Selected by EvREVs
Study
Subjects
Date
N
One-Month Survival
CPC 1-2
Hagihara 2012
JAMA
“Epi vs. None”
OHCA
20052008
417,188
Propensity
Matched:
26,802
VF: 15.4% vs. 21.3%
NonVF: 3.8% vs. 3.4%
Propensity Matched:
5.1% vs. 7.0%
VF: 6.1% vs.
NonVF: 0.6%
Propensity Ma
1.3% vs. 3.1%
Nakahara 2012
“Early Epi?”
Witnessed
OHCA
20072008
49,165
VF: 28.2% vs. 17.7%
NonVF: 4.7% vs. 2.8%
VF: 13.9% vs.
NonVF: 0.9%
Nakahara 2013
BMJ
“EMS Epi?”
Witnessed
OHCA
20072010
96,079
Propensity
Matched for
Duration:
22,096
VF: 16.5% vs. 28.8%
NonVF: 3.9% vs. 4.2%
Propensity Matched:
VF: 17.0% vs. 13.4%
NonVF: 4.0% vs. 2.4%
VF: 6.9% vs.
NonVF: 0.6%
Propensity Ma
VF: 6.6% vs. 6
NonVF: 0.7%
Hayashi 2012
“EMS Epi?”
OHCA with
Advanced
EMS
20072009
3,161
13.5% vs. 12.0%
VF: 29.8% vs. 36.2%
NonVF: 9.3% vs. 8.1%
4.1% vs. 6.1%
VF: 14.1% vs
NonVF: 1.5%
Goto 2013
“Epi x Rhythm?”
OHCA of
cardiac
cause
20092010
209,577
VF: 15.4% vs. 27.0%
NonVF: 3.0% vs. 18.7%
VF: 7.0% vs.
NonVF: 0.59 v
C2015 ALS_Vassopressors in cardiac arrest_220912
Risk of bias in individual RCT studies
All studies, alphabetical
Lack of
Blinding
Incomplete
accounting of
patients or
outcomes
Low
High – 67 pts
(11%) post
randomization
excl
Unclear – no
mention
Low
Low
Sequence
Generation
Lack of
Allocation
concealment
SDE vs. Placebo
Jacobs 2011,
1138
Low
SDE vs. Vasopressin
Mukoyama
2009, 755
Unclear – not
stated
SDE vs. HDE
Brown
1992, 1051
Callaham
1992, 2667
Selective
outcome
reporting
Other Biases
Outcomes to
which these
assessments
apply
Overall risk of
bias for
outcome(s) for
study**
Low
High – 989
consecutive cases, of
which 601 randomized
(unexplained) & trial
terminated early due to
lack of enthusiasm by
providers
All outcomes
High
Unclear – no
mention
High – 37%
post
randomization
exclusion
Unclear –
attributed to
post
randomization
exclusion
Low
All outcomes
High
Low
Low
Low
Low
Low
none
Low
Low
Low
Low
Low
Low
none
Low
Low
Survival to
discharge
Moderate
Low
Choux
1995, 3
Low
Low
Low
Low
High - No
reported data
survival to
discharge – at 6
mo. available
Gueugniaud
1998, 1595
Low
Low
Low
Low
Low
Low
none
Low
All outcomes
Moderate
Sherman
1997, 242
Low
Low
Low
Low
Low
High - higher
proportion of VF
patients and lower
proportion of asystole
in HDE
Stiell
1992, 1045
Low
Low
Low
Low
Low
Low
none
Low
Low
none
Low
SDE vs. Epinephrine and Vasopressin
Callaway
2006, 1316
Low
Low
Low
Low
Low
C2015 ALS_Vassopressors in cardiac arrest_220912
Sequence
Generation
Lack of
Allocation
concealment
Lack of
Blinding
Incomplete
accounting of
patients or
outcomes
Selective
outcome
reporting
Other Biases
Outcomes to
which these
assessments
apply
Overall risk of
bias for
outcome(s) for
study**
SDE vs. Epinephrine and Vasopressin cont’d from page 1
Ducros
2011,453
Gueugniaud
2008, 21
Low
Low
Lindner 1997,
535
Low
Ong
2012, 953
Unclear –
randomization
attributed to
‘trial
statistician’ –
missing
details
Wenzel 2004,
105
Low
Low
Low
Low
High – Fallout
prior to
endpoints due
to ROSC (19)
and (6) IV
access
Low
Unclear –
poorly
described –
uses
‘unaware’
but no details
provided
Low
Low
Low
All outcomes
Moderate
Low
High – Needs a
consort diagram
to confirm
consecutive case
enrolment
All Outcomes
Moderate
Low
Low
Survival to DC
High
Low
High – poor
protocol
compliance –
included 88
randomized
patients who met
criteria for
exclusion
All outcomes
High
Low
Low
Low
Low
Low
High - broke
blinding after
hospital
admission
but unlikely
to affect
outcome
Low
High –
combined
Survival to
DC with alive
at 30 days or
which ever
came first
High – 33
randomized
patients
missing study
drug so not
included –
distribution
across groups
unknown
High - higher
proportion of PEA
patients in Epi group
and higher proportion
of VF patients in
VasoEpi gp
All outcomes
High
*For all: risk of bias = Low/Unclear/High
1. Lack of allocation concealment: Those enrolling patients are aware of the group (or period in a crossover trial) to which the next enrolled patient will be allocated (major problem in ‘‘pseudo’’ or ‘‘quasi’’ randomized trials with allocation by day of week, birth date,
chart number, etc)
2. Lack of blinding: Patient, care givers, those recording outcomes, those adjudicating outcomes, or data analysts are aware of the arm to which patients are allocated (or the medication currently being received in a crossover trial)
3. Incomplete accounting of patients and outcome events: Loss to follow-up and failure to adhere to the intention-to-treat principle in superiority trials; or in noninferiority trials, loss to follow-up, and failure to conduct both analyses considering only those who
adhered to treatment, and all patients for whom outcome data are available
4. Selective outcome reporting bias: Incomplete or absent reporting of some outcomes and not others on the basis of the results
5. Other limitations: Stopping early for benefit. Use of unvalidated outcome measures (e.g., patient-reported outcomes). Carryover effects in crossover trial. Recruitment bias in cluster-randomized trials
** Overall risk of bias of study = Low, Moderate or High
“Low” risk of bias if most or all key criteria listed above are met, and any violations are not crucial.
“Moderate” risk of bias if have a crucial limitation in one criterion or some limitations in multiple criteria, sufficient to lower the confidence in the estimate of effect.
“High” risk of bias if have a crucial limitation in one or more criteria, sufficient to substantially lower the confidence in the estimate of effect.
C2015 ALS_Vassopressors in cardiac arrest_220912
C2015 ALS_Vassopressors in cardiac arrest_220912
Initial Evidence Profile Tables
Outcome
No of studies
Author Year 1st page
Study
Design
Risk of
bias*
Indirectness*
Imprecision*
Other**
Quality of
evidence for
outcome***
Not applicable
to single trial
No serious
indirectness
Serious
imprecision
Not applicable
to single trial
Low
Not applicable
to single trial
No serious
indirectness
Serious
imprecision
Not applicable
to single trial
Low
Not applicable
to single trial
No serious
indirectness
Very Serious
imprecision
Not applicable
to single trial
Low
Not applicable
to single trial
No serious
indirectness
Very Serious
imprecision
Not applicable
to single trial
Low
Inconsistency*
SDE vs Placebo
ROSC
Important 5
Alive at Admission
Important 6
Survival to
Discharge
Critical 8
Survival to
Discharge with CPC
1 or 2
Critical 9
1
Jacobs 2011,1138
RCT
1
Jacobs 2011,1138
RCT
1
Jacobs 2011,1138
RCT
1
Jacobs 2011,1138
RCT
Very
Serious
limitation
Very
Serious
limitation
Very
Serious
limitation
Very
Serious
limitation
SDE vs Vasopressin
ROSC
Important 5
Alive at Admission
Critical 7
Survival to
Discharge
Critical 8
Survival to
Discharge with CPC
1 or 2
Critical 9
1
Makoyamo
2009, 755
RCT
1
Makoyamo 2009, 755
RCT
1
Makoyamo 2009, 755
RCT
1
Makoyamo 2009, 755
RCT
Very
Serious
Limitation
Very
Serious
Limitation
Very
Serious
Limitation
Very
Serious
Limitation
Not applicable
to single trial
No serious
indirectness
Serious
imprecision
Not applicable
to single trial
Low
Not applicable
to single trial
No serious
indirectness
Serious
imprecision
Not applicable
to single trial
Low
Not applicable
to single trial
No serious
indirectness
Serious
imprecision
Not applicable
to single trial
Low
Not applicable
to single trial
No serious
indirectness
Serious
imprecision
Not applicable
to single trial
Low
No serious
indirectness
No serious
imprecision
Undetected
High
SDE vs HDE
ROSC
Important 5
6
Brown 1992, 1051
Callaham 1992, 2667
Choux 1995, 3
Gueugniaud 1998, 1595
Sherman 1997, 242
Stiell 1992, 1045
RCT
No Serious
Limitation
No serious
inconsistency
C2015 ALS_Vassopressors in cardiac arrest_220912
Alive at Admission
Important 6
4
Brown 1992, 1051
Callaham 1992, 2667
Choux 1995, 3
Gueugniaud 1998, 1595
RCT
No Serious
Limitation
No Serious
Limitation
No serious
indirectness
No serious
imprecision
Undetected
High
C2015 ALS_Vassopressors in cardiac arrest_220912
Outcome
No of studies
Author Year 1st page
Survival to Discharge
Critical 8
5
Brown 1992, 1051
Callaham 1992, 2667
Gueugniaud 1998, 1595
Sherman 1997, 242
Stiell 1992, 1045
2
Callaham 1992, 2667
Gueugniaud 1998, 1595
Study
Design
Risk of
bias*
Inconsistency*
Indirectness*
Imprecision*
Other**
Quality of
evidence for
outcome***
SDE vs HDE cont’d from previous table
Survival to Discharge
with CPC 1 or 2
Critical 9
RCT
Serious
limitation
No serious
inconsistency
No serious
indirectness
Serious
imprecision
Undetected
Moderate
RCT
Serious
limitation
No serious
inconsistency
No serious
indirectness
Serious
imprecision
Undetected
Moderate
No serious
imprecision
Undetected
High
No serious
imprecision
Undetected
High
Serious
imprecision
Undetected
Moderate
Serious
imprecision
Undetected
Moderate
SDE vs Epinephrine Vasopressin Combination
ROSC
Important 5
Alive at Admission
Important 6
Survival to Discharge
Critical 8
Survival to Discharge
with CPC 1 or 2
Critical 9
6
Callaway 2006, 1316
Ducros 2011,453
Gueugniaud 2008, 21
Lindner 1997, 535
Ong 2012, 953
Wenzel 2004, 105
5
Ducros 2011,453
Gueugniaud 2008, 21
Lindner 1997, 535
Ong 2012, 953
Wenzel 2004, 105
5 (as above)
RCT
Serious
limitation
No serious
inconsistency
No serious
indirectness
RCT
Serious
limitation
No serious
inconsistency
No serious
indirectness
RCT
Very
Serious
Limitation
No serious
inconsistency
No serious
indirectness
3
Very
Gueugniaud 2008, 21
No serious
No serious
RCT
Serious
Ong 2012, 953
inconsistency
indirectness
Limitation
Wenzel 2004, 105
* Classification across all studies for each outcome for: Risk of Bias/Inconsistency/Indirectness/Imprecision
No serious limitations: Most information is from studies at low risk of bias. Do not downgrade
Serious limitations: Most information is from studies at moderate risk of bias. Rate down one level
Very serious limitations: Most information is from studies at high risk of bias. Rate down two levels
** Classification across all studies for each outcome for Publication Bias: Undetected or Strongly suspected
*** Quality of Evidence across included studies for outcome: High, Moderate, Low, Very Low
C2015 ALS_Vassopressors in cardiac arrest_220912
Summary of Findings Table (Single Trial OR)
Single Dose Epinephrine versus Placebo
Jacobs, 2011
Outcome
ROSC
Survival to admission
Survived to DC
Survival with CPC 1-2
SDE
Events Total
64
272
69
272
11
272
9
272
Placebo
Events Total
22
262
34
262
5
262
5
262
OR (95% CI)
3.4 (2.0, 5.6)
2.3 (1.4, 3.6)
2.2 (0.7, 6.3)
GRADE
Quality of the Evidence
Comments (see tables)
Low
Low
Low
Low
Stopped Early, perhaps
many pot eligible not
randomized and Post
Rand exclusion.
GRADE
Quality of the Evidence
Comments
Single Dose Epinephrine versus Vasopressin
Makoyama 2009
Outcome
ROSC
Survival to admission
Survived to DC
Survival with CPC 1 or 2
SDE
Events Total
42
158
32
158
6
158
0
158
Vasopressin
Events Total
51
178
30
178
10
178
4
178
OR (95% CI)
1.1 (0.7, 1.8)
0.8 (0.5, 1.4)
1.5 (0.5, 4.2)
Low
Low
Low
Low
Methods unclear,Post Rand Excl
C2015 ALS_Vassopressors in cardiac arrest_220912
Summary of Findings Table (Meta-Analyses by Outcome)
Single Dose Epinephrine versus High Dose Epinephrine
ROSC – GRADE HIGH
Survival to arrive at ED – GRADE HIGH
Survival to discharge – GRADE MODERATE
C2015 ALS_Vassopressors in cardiac arrest_220912
Survival to discharge with CPC of 1 or 2 – GRADE MODERATE
SDE
HDE
Favours high dose
HDE
Summary of Findings Table (Meta-Analyses by Outcome)
Epinephrine versus Epinephrine and Vasopressin in Combination
ROSC – GRADE HIGH
Survival to admission – GRADE HIGH
Favours standard dose
C2015 ALS_Vassopressors in cardiac arrest_220912
Survival to discharge – GRADE MODERATE
Survival to discharge with CPC of 1 or 2– GRADE MODERATE
EPI
Vaso/Epi
Favours Vaso/Epi
Favours Epi
C2015 ALS_Vassopressors in cardiac arrest_220912
REVIEWER’S FINAL COMMENTS AND ASSESSMENT OF BENEFIT / RISK:
CONSENSUS ON SCIENCE:
Loaded onto Seers and pasted below
Placebo vs Epinephrine
For all four long term (critical) and short term (important) outcomes, we found one underpowered trial that provided low quality evidence comparing SDE to placebo
(Jacobs, 2001, 1138). Among 534 subjects, there was uncertain benefit or harm of SDE over placebo for the critical outcomes of survival to discharge [RR 2.12, 95% CI
0.75-6.02, p=0.16] and good neurological outcome defined as CPC of 1-2 [RR 1.73, 95% CI 0.59-5.11, p=0.32]. However, patients who received SDE had higher rates of
the two important outcomes of survival to admission [RR 1.95, 95% CI, 1.34-2.84, p=0.0004] and ROSC in the prehospital setting [RR 2.80, 95% CI 1.78-4.41, p<0.00001]
compared to those who received placebo.
SDE vs Vasopressin
We found a single RCT (Mukoyama 2009; 755) n=336 that compared multiple doses of Standard Dose Epinephrine (SDE) with multiple doses of Standard Dose
Vasopressin in the Emergency Department after OHCA. The trial had a high rate of bias as much of the methodology is unclear and there was a 37% post randomization
exclusion. The primary outcome measure was CPC score of 1 or 2 however neither the sample size estimate nor power calculation were included in the paper. There were
no significant differences in either critical outcomes of survival to discharge with neurological outcome as defined as Cerebral Category Performance Score of 1 or 2 (RR
0.68, 95% CI 0.25–1.82, p = 0.44) or survival to discharge (RR 0.68, 95% CI 0.25–1.82, p = 0.44) or the important outcome of ROSC (RR 0.93, 95% CI 0.66–1.31, p =
0.67).
SDE vs HDE* all these high or moderate quality trials were downgraded by the TF based on age of the trials < 1999
For the critical outcome of survival to hospital discharge with a good CPC score of 1 or 2 we found 2 RCTs comparing standard dose epinephrine (SDE) with high dose
epinephrine (HDE) (Callaham 1992, 2667; Gueugniaud 1998, 1595 low quality) n=1920 and cumulative relative risk (RR) did not demonstrate any survival to discharge
with a good CPC score advantage with HDE with a RR of 1.2 95% CI of 0.74, 1.96.
For the critical outcome of survival to hospital discharge we found 5 RCTs comparing standard dose epinephrine (SDE) with high dose epinephrine (HDE) (Brown 1992,
1051; Callaham 1992, 2667; Gueugniaud 1998, 1595; Sherman 1997, 242; Stiell 1992, 1045; low quality) n=2859 and cumulative RR did not demonstrate any survival to
discharge advantage with HDE with a RR of 0.97 with 95% CI of 0.71, 1.32.
For the important outcome of survival to hospital admission we found 4 RCTs comparing SDE with HDE (Brown 1992, 1051; Callaham 1992, 2667; Gueugniaud 1998,
1595;Choux 1995,3; Moderate quality) n=2882 and the cumulative RR demonstrated a survival to hospital admission advantage with HDE with a RR of 1.15 with 95% CI
of 1.0, 1.32.
For the important outcome of return of spontaneous circulation (ROSC) we found 6 RCTS comparing SDE with HDE (Brown 1992, 1051; Callaham 1992, 2667; Choux
1995, 3; Gueugniaud 1998, 1595; Sherman 1997, 242; Stiell 1992, 1045; Moderate quality) n=3130 and the cumulative RR demonstrated a ROSC advantage with HDE
with a RR of 1.17 (95% CI 1.03, 1.34)
Epinephrine vs Epinephrine and Vasopressin in Combination Therapy
For the critical outcome of survival to hospital discharge with CPC of 1 or 2 we found 3 RCTs (Gueugniaud 2008, 21; Ong 2012, 953; Wenzel 2004, 105 moderate quality)
N=2402 comparing standard dose epinephrine (SDE) with vasopressin epinephrine combination therapy demonstrated no superiority with vasopressin epinephrine
combination (RR of 1.32 95% CI of 0.88 and 1.98).
For the critical outcome of survival to hospital discharge we found 5 RCTs (Ducros, 2011, 453; Gueugniaud 2008, 21; Lindner 1997, 535;Ong 2012, 953; Wenzel 2004, 105
moderate quality) n=2438 comparing SDE to vasopressin and epinephrine combination therapy did not demonstrate superiority with vasopressin and epinephrine
combination therapy in survival to discharge [RR 1.12, 95% CI 0.84-1.49, p=0.45]
For the important outcomes of survival to admission we found 5 RCTs (Ducros, 2011, 453; Gueugniaud 2008, 21; Lindner 1997, 535;Ong 2012, 953; Wenzel 2004, 105
high quality) n=2438 demonstrating no significant differences in survival to hospital admission with vasopressin epinephrine combination therapy (0.88, 95% CI 0.73-1.06,
p=0.17)
C2015 ALS_Vassopressors in cardiac arrest_220912
For the important outcomes of return of spontaneous circulation (ROSC) we found 6 RCTs (Callaway 2006, 1316; Ducros, 2011, 453; Gueugniaud 2008, 21; Lindner 1997,
535;Ong 2012, 953; Wenzel 2004, 105 high quality) demonstrating no ROSC advantage with vasopressin epinephrine combination therapy with RR 0.96, 95% CI 0.891.04, p=0.31.
Conclusion
TREATMENT RECOMMENDATION (including direction, quality of evidence and strength of evidence grade*):
GRADE assignment for Strength of Recommendation = WEAK
GRADE assignment for Strength of Evidence = High for early outcomes and Low for survival
Loaded onto Seers and pasted below
Placebo vs Epinephrine
Treatment Recommendation
Given the observed benefit in short term outcomes, we suggest SDE be administered to patients in cardiac arrest.(weak recommendation, low quality)
Value and Preferences Statement:
In making this statement, we place value on the short-term outcomes of ROSC and survival to admission, and our uncertainty about the absolute effect on
survival and neurological outcome.
SDE vs Vasopressin
Treatment Recommendation:
We suggest against initiating vasopressin as a substitution for epinephrine in the treatment in cardiac arrest. (weak recommendation, low quality)
Values and Preferences Statement:
The recommendation considers the fact that vasopressin is widely used now, and the available data do not indicate any reason to change practice.
SDE vs HDE
Treatment Recommendation:
Despite the high quality evidence that HDE improves short term outcomes when compared to SDE, we recommend against the routine use of HDE in
cardiac arrest treatment.(strong recommendation, moderate quality)
Value and Preferences Statement:
In making this statement, we noted that multiple high and moderate quality trials failed to demonstrate an improvement the critical outcomes of survival and
neurological outcome. The absolute magnitude of effects of HDE vs. SDE on ROSC are much less than the difference in SDE vs. Placebo. These HDE
studies were performed in the 1990’s since when care and outcomes have changed dramatically, making it hard to interpret the relevance of these results
when compared with current care.
Epinephrine vs Epinephrine and Vasopressin in Combination Therapy
Treatment Recommendation:
We suggest against adding vasopressin to standard dose epinephrine during cardiac arrest. (weak recommendation, moderate quality)
Value and Preferences Statement:
In making this recommendation, we considered it distracting and costly to add a drug that has no evidence of additional benefit for patients.
We also have no reason to withdraw this drug if the drug is currently in use.
Knowledge gap for all Vasopressor PICOs
Dose response and placebo-controlled efficacy trials are needed to evaluate the use of any vasopressor in adult and pediatric cardiac arrest.
C2015 ALS_Vassopressors in cardiac arrest_220912
Acknowledgements:
Justin Wagner University of Western Ontario, Prakeshkumar Shah University of Toronto, Joseph Beyene University of Toronto
* Strength of Recommendation
Strong: the desirable effects of an intervention clearly outweigh the undesirable effects, or clearly do not.
For patients—most people in your situation would want the recommended course of action and only a small proportion would not; request discussion if the intervention is
not offered
For clinicians—most patients should receive the recommended course of action
Weak: the trade-offs are less certain—either because of low quality evidence or because evidence suggests that desirable and undesirable effects are closely
balanced.
For patients—most people in your situation would want the recommended course of action, but many would not
For clinicians—you should recognise that different choices will be appropriate for different patients and that you must help each patient to arrive at a management decision
consistent with her or his values and preferences
Strength of Evidence Grade Definition
High: We are very confident that the true effect lies close to that of the estimate of the effect
Moderate: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially
different.
Low: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect.
Very low: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect.
C2015 ALS_Vassopressors in cardiac arrest_220912
Citation List
Included studies (with abstracts)
Brown, C. G., D. R. Martin, P. E. Pepe, H. Stueven, R. O. Cummins, E. Gonzalez and M. Jastremski (1992). "A comparison of
standard-dose and high-dose epinephrine in cardiac arrest outside the hospital. The Multicenter High-Dose Epinephrine Study
Group." N Engl J Med 327(15): 1051-1055.
BACKGROUND: Experimental and uncontrolled clinical evidence suggests that intravenous epinephrine in doses higher
than currently recommended may improve outcome after cardiac arrest. We conducted a prospective, multicenter study comparing
standard-dose epinephrine with high-dose epinephrine in the management of cardiac arrest outside the hospital. METHODS: Adult
patients were enrolled in the study if they remained in ventricular fibrillation, or if they had asystole or electromechanical
dissociation, at the time the first drug was to be administered to treat the cardiac arrest. Patients were randomly assigned to
receive either 0.02 mg of epinephrine per kilogram of body weight (standard-dose group, 632 patients) or 0.2 mg per kilogram
(high-dose group, 648 patients), both given intravenously. RESULTS: In the standard-dose group 190 patients (30 percent) had a
return of spontaneous circulation, as compared with 217 patients (33 percent) in the high-dose group; 136 patients (22 percent) in
the standard-dose group and 145 patients (22 percent) in the high-dose group survived to be admitted
Callaham, M., C. D. Madsen, C. W. Barton, C. E. Saunders and J. Pointer (1992). "A randomized clinical trial of high-dose
epinephrine and norepinephrine vs standard-dose epinephrine in prehospital cardiac arrest." JAMA 268(19): 2667-2672.
OBJECTIVE: To determine the relative efficacy of high- vs standard-dose catecholamines in initial treatment of prehospital
cardiac arrest. DESIGN: Randomized, prospective, double-blind clinical trial. SETTING: Prehospital emergency medical
system of a major US city. PATIENTS: All adults in nontraumatic cardiac arrest, treated by paramedics, who would receive
epinephrine according to American Heart Association advanced cardiac life support guidelines. INTERVENTIONS: Highdose epinephrine (HDE, 15 mg), high-dose norepinephrine bitartrate (NE, 11 mg), or standard-dose epinephrine (SDE, 1
mg) was blindly substituted for advanced cardiac life support doses of epinephrine. MAIN OUTCOME MEASURES:
Restoration of spontaneous circulation in the field, admission to hospital, hospital discharge, and Cerebral Performance
Category score. RESULTS: Of 2694 patients with cardiac arrests during the study period, resuscitation was attempted on
1062 patients. Of this total, 816 patients met study criteria and were enrolled. In the entire cardiac arrest population, 63% of
the survivors were among the 11% of patients who were defibrillated by first responders. The three drug treatment groups
were similar for all independent variables. Thirteen percent of patients receiving HDE regained a pulse in the field vs 8% of
those receiving SDE (P = .01), and 18% of HDE patients were admitted to the hospital vs 10% of SDE patients who were
admitted to the hospital (P = .02). Similar trends for NE were not significant. There were 18 survivors; 1.7% of HDE patients
and 2.6% of NE patients were discharged from the hospital compared with 1.2% of SDE patients, but this was not significant
(P = .37; beta = .38). There was a nonsignificant trend for Cerebral Performance Category scores to be worse for HDE (3.2)
and NE patients (3.7) than for SDE patients (2.3) (P = .10; beta = .31). No significant complications were identified. Highdose epinephrine did not produce longer hospital or critical care unit stays. CONCLUSIONS: High-dose epinephrine
significantly improves the rate of return of spontaneous circulation and hospital admission in patients who are in prehospital
cardiac arrest without increasing complications. However, the increase in hospital discharge rate is not statistically
C2015 ALS_Vassopressors in cardiac arrest_220912
significant, and no significant trend could be determined for neurological outcome. No benefit of NE compared with HDE
was identified. Further study is needed to determine the optimal role of epinephrine in prehospital cardiac arrest.
Callaway, C. W., D. Hostler, A. A. Doshi, M. Pinchalk, R. N. Roth, J. Lubin, D. H. Newman and L. J. Kelly (2006). "Usefulness of
vasopressin administered with epinephrine during out-of-hospital cardiac arrest." Am J Cardiol 98(10): 1316-1321.
Vasopressin administration has been suggested during cardiopulmonary resuscitation, and a previous clinical trial has
suggested that vasopressin is most effective when administered with epinephrine. Adult subjects (n = 325) who received >
or =1 dose of intravenous epinephrine during cardiopulmonary resuscitation for nontraumatic, out-of-hospital cardiac arrest
were randomly assigned to receive 40 IU of vasopressin (n = 167) or placebo (n = 158) as soon as possible after the first
dose of epinephrine. The rate of return of pulses was similar between the vasopressin and placebo groups (31% vs 30%),
as was the presence of pulses at the emergency department (19% vs 23%). No subgroup appeared to be differentially
affected, and no effect of vasopressin was evident after adjustment for other clinical variables. Additional open-label
vasopressin was administered by a physician after the study drug for 19 subjects in the placebo group and 27 subjects in
the vasopressin group. Results were similar if these subjects were excluded or were assigned to an actual drug received.
Survival duration for subjects admitted to the hospital did not differ between groups. In conclusion, vasopressin administered
with epinephrine does not increase the rate of return of spontaneous circulation.
Choux, C., P. Y. Gueugniaud, A. Barbieux, E. Pham, C. Lae, P. Y. Dubien and P. Petit (1995). "Standard doses versus repeated
high doses of epinephrine in cardiac arrest outside the hospital." Resuscitation 29(1): 3-9.
Among all of the cathecolamines used for cardiac arrest treatment, epinephrine injection during cardio-pulmonary
resuscitation is currently the most powerful means of enhancing effectiveness; however, deliberations about the optimal
dosage have recently become intense. In the SAMU of Lyon (F), we conducted a double blind prospective randomized study
over an 18-month period, comparing repeated standard-dose epinephrine (1 mg) and repeated high-dose epinephrine (5
mg) in the management of cardiac arrest outside the hospital. Five-hundred thirty-six patients were enrolled with 265 in the
standard-dose group and 271 in the high-dose group; both groups are globally similar. One-hundred eighty-one (33.8%)
patients returned to spontaneous circulation (R.O.S.C.); 85 in the standard-dose group (32%) and 96 in the high-dose group
(35.5%). One-hundred nineteen patients (22.2%) were admitted; 54 in the standard-dose group (20.4%) and 65 in the highdose group (24%). At 6 months nine patients (7.6%) were alive; three patients from the standard-dose group (5.5%) and six
from the high-dose group (9.2%). We never noticed cardiac or neurologic adverse effects with the high doses. The results of
this study are not statistically significant, but we observed a marginal trend towards repeated 5 mg epinephrine doses. A
large French multicentre study is now necessary.
Ducros, L., E. Vicaut, C. Soleil, M. Le Guen, P. Gueye, T. Poussant, A. Mebazaa, D. Payen and P. Plaisance (2011). "Effect of the
addition of vasopressin or vasopressin plus nitroglycerin to epinephrine on arterial blood pressure during cardiopulmonary
resuscitation in humans." J Emerg Med 41(5): 453-459.
BACKGROUND: Infusion of a vasopressor during cardiopulmonary resuscitation (CPR) in humans increases end
decompression (diastolic) arterial blood pressure, and consequently increases vital organ perfusion pressure and survival.
Several vasoactive drugs have been tested alone or in combination, but their hemodynamic effects have not been
C2015 ALS_Vassopressors in cardiac arrest_220912
investigated clinically in humans. STUDY OBJECTIVE: We tested the hypothesis that epinephrine (1 mg) co-administered
with vasopressin (40 IU) +/- nitroglycerin (300 mug) results in higher diastolic blood pressure than epinephrine alone.
STUDY DESIGN: A prospective, randomized, double-blinded controlled trial in the prehospital setting. The study included 48
patients with witnessed cardiac arrest. Patients received either epinephrine alone (E alone) or epinephrine plus vasopressin
(E+V) or epinephrine plus vasopressin plus nitroglycerin (E+V+N). A femoral arterial catheter was inserted for arterial
pressure measurement. OUTCOME MEASURES: The primary end point was diastolic blood pressure during CPR, 15 min
after the first drug administration (T = 15 min). RESULTS: After exclusions, a total of 44 patients were enrolled. Diastolic
blood pressures (mm Hg) at T = 15 min were not statistically different between groups (median [interquartile range]: 20 [10],
15 [6], and 15 [13] for E alone, E+V, and E+V+N, respectively. The rate of return of spontaneous circulation was 63% (n =
10) in the epinephrine group, 43% (n = 6) in the epinephrine plus vasopressin group, and 36% (n = 5) in the triple therapy
group (NS). CONCLUSIONS: Addition of vasopressin or vasopressin plus nitroglycerin to epinephrine did not increase
perfusion blood pressure compared to epinephrine alone in humans in cardiac arrest, suggesting the absence of benefit in
using these drug combination(s).
Gueugniaud, P. Y., P. Mols, P. Goldstein, E. Pham, P. Y. Dubien, C. Deweerdt, M. Vergnion, P. Petit and P. Carli (1998). "A
comparison of repeated high doses and repeated standard doses of epinephrine for cardiac arrest outside the hospital. European
Epinephrine Study Group." N Engl J Med 339(22): 1595-1601.
BACKGROUND: Clinical trials have not shown a benefit of high doses of epinephrine in the management of cardiac arrest.
We conducted a prospective, multicenter, randomized study comparing repeated high doses of epinephrine with repeated
standard doses in cases of out-of-hospital cardiac arrest. METHODS: Adult patients who had cardiac arrest outside the
hospital were enrolled if the cardiac rhythm continued to be ventricular fibrillation despite the administration of external
electrical shocks, or if they had asystole or pulseless electrical activity at the time epinephrine was administered. We
randomly assigned 3327 patients to receive up to 15 high doses (5 mg each) or standard doses (1 mg each) of epinephrine
according to the current protocol for advanced cardiac life support. RESULTS: In the high-dose group, 40.4 percent of 1677
patients had a return of spontaneous circulation, as compared with 36.4 percent of 1650 patients in the standard-dose group
(P=0.02); 26.5 percent of the patients in the high-dose group and 23.6 percent of those in the standard-dose group survived
to be admitted to the hospital (P=0.05); 2.3 percent of the patients in the high-dose group and 2.8 percent in the standarddose group survived to be discharged from the hospital (P=0.34). There was no significant difference in neurologic status
according to treatment among those discharged. High-dose epinephrine improved the rate of successful resuscitation in
patients with asystole, but not in those with ventricular fibrillation. CONCLUSIONS: In our study, long-term survival after
cardiac arrest outside the hospital was no better with repeated high doses of epinephrine than with repeated standard
doses.
Gueugniaud, P. Y., J. S. David, E. Chanzy, H. Hubert, P. Y. Dubien, P. Mauriaucourt, C. Braganca, X. Billeres, M. P. ClotteauLambert, P. Fuster, D. Thiercelin, G. Debaty, A. Ricard-Hibon, P. Roux, C. Espesson, E. Querellou, L. Ducros, P. Ecollan, L.
Halbout, D. Savary, F. Guillaumee, R. Maupoint, P. Capelle, C. Bracq, P. Dreyfus, P. Nouguier, A. Gache, C. Meurisse, B.
Boulanger, C. Lae, J. Metzger, V. Raphael, A. Beruben, V. Wenzel, C. Guinhouya, C. Vilhelm and E. Marret (2008). "Vasopressin
and epinephrine vs. epinephrine alone in cardiopulmonary resuscitation." N Engl J Med 359(1): 21-30.
C2015 ALS_Vassopressors in cardiac arrest_220912
BACKGROUND: During the administration of advanced cardiac life support for resuscitation from cardiac arrest, a
combination of vasopressin and epinephrine may be more effective than epinephrine or vasopressin alone, but evidence is
insufficient to make clinical recommendations. METHODS: In a multicenter study, we randomly assigned adults with out-ofhospital cardiac arrest to receive successive injections of either 1 mg of epinephrine and 40 IU of vasopressin or 1 mg of
epinephrine and saline placebo, followed by administration of the same combination of study drugs if spontaneous
circulation was not restored and subsequently by additional epinephrine if needed. The primary end point was survival to
hospital admission; the secondary end points were return of spontaneous circulation, survival to hospital discharge, good
neurologic recovery, and 1-year survival. RESULTS: A total of 1442 patients were assigned to receive a combination of
epinephrine and vasopressin, and 1452 to receive epinephrine alone. The treatment groups had similar baseline
characteristics except that there were more men in the group receiving combination therapy than in the group receiving
epinephrine alone (P=0.03). There were no significant differences between the combination-therapy and the epinephrineonly groups in survival to hospital admission (20.7% vs. 21.3%; relative risk of death, 1.01; 95% confidence interval [CI],
0.97 to 1.05), return of spontaneous circulation (28.6% vs. 29.5%; relative risk, 1.01; 95% CI, 0.97 to 1.06), survival to
hospital discharge (1.7% vs. 2.3%; relative risk, 1.01; 95% CI, 1.00 to 1.02), 1-year survival (1.3% vs. 2.1%; relative risk,
1.01; 95% CI, 1.00 to 1.02), or good neurologic recovery at hospital discharge (37.5% vs. 51.5%; relative risk, 1.29; 95% CI,
0.81 to 2.06). CONCLUSIONS: As compared with epinephrine alone, the combination of vasopressin and epinephrine
Jacobs, I. G., J. C. Finn, G. A. Jelinek, H. F. Oxer and P. L. Thompson (2011). "Effect of adrenaline on survival in out-of-hospital
cardiac arrest: A randomised double-blind placebo-controlled trial." Resuscitation 82(9): 1138-1143.
Background: There is little evidence from clinical trials that the use of adrenaline (epinephrine) in treating cardiac arrest
improves survival, despite adrenaline being considered standard of care for many decades. The aim of our study was to
determine the effect of adrenaline on patient survival to hospital discharge in out of hospital cardiac arrest. Methods: We
conducted a double blind randomised placebo-controlled trial of adrenaline in out-of-hospital cardiac arrest. Identical study
vials containing either adrenaline 1:1000 or placebo (sodium chloride 0.9%) were prepared. Patients were randomly
allocated to receive 1. ml aliquots of the trial drug according to current advanced life support guidelines. Outcomes
assessed included survival to hospital discharge (primary outcome), pre-hospital return of spontaneous circulation (ROSC)
and neurological outcome (Cerebral Performance Category Score - CPC). Results: A total of 4103 cardiac arrests were
screened during the study period of which 601 underwent randomisation. Documentation was available for a total of 534
patients: 262 in the placebo group and 272 in the adrenaline group. Groups were well matched for baseline characteristics
including age, gender and receiving bystander CPR. ROSC occurred in 22 (8.4%) of patients receiving placebo and 64
(23.5%) who received adrenaline (OR = 3.4; 95% CI 2.0-5.6). Survival to hospital discharge occurred in 5 (1.9%) and 11
(4.0%) patients receiving placebo or adrenaline respectively (OR = 2.2; 95% CI 0.7-6.3). All but two patients (both in the
adrenaline group) had a CPC score of 1-2. Conclusion: Patients receiving adrenaline during cardiac arrest had no
statistically significant improvement in the primary outcome of survival to hospital discharge although there was a
significantly improved likelihood of achieving ROSC. (copyright) 2011 Elsevier Ireland Ltd.
Lindner, K. H., B. Dirks, H. U. Strohmenger, A. W. Prengel, I. M. Lindner and K. G. Lurie (1997). "Randomised comparison of
epinephrine and vasopressin in patients with out-of-hospital ventricular fibrillation." Lancet 349(9051): 535-537.
C2015 ALS_Vassopressors in cardiac arrest_220912
BACKGROUND: Studies in animals have suggested that intravenous vasopressin is associated with better vital-organ
perfusion and resuscitation rates than is epinephrine in the treatment of cardiac arrest. We did a randomised comparison of
vasopressin with epinephrine in patients with ventricular fibrillation in out-of-hospital cardiac arrest. METHODS: 40 patients
in ventricular fibrillation resistant to electrical defibrillation were prospectively and randomly assigned epinephrine (1 mg
intravenously; n = 20) or vasopressin (40 U intravenously; n = 20) as primary drug therapy for cardiac arrest. The endpoints
of this double blind study were successful resuscitation (hospital admission), survival for 24 h, survival to hospital discharge
and neurological outcome (Glasgow coma scale). Analyses were by intention to treat. FINDINGS: Seven (35%) patients in
the epinephrine group and 14 (70%) in the vasopressin group survived to hospital admission (p = 0.06). At 24 h, four (20%)
epinephrine-treated patients and 12 (60%) vasopressin-treated patients were alive (p = 0.02). Three (15%) patients in the
epinephrine group and eight (40%) in the vasopressin group survived to hospital discharge (p = 0.16). Neurological
outcomes were similar (mean Glasgow coma score at hospital discharge 10.7 [SE 3.8] vs 11.7 [1.6], p = 0.78).
INTERPRETATION: In this preliminary study, a significantly larger proportion of patients created with vasopressin than of
those treated with epinephrine were resuscitated successfully from out-of-hospital ventricular fibrillation and survived for 24
h. Based upon these findings, larger multicentre studies of vasopressin in the treatment of cardiac arrest are needed.
Mukoyama, T., K. Kinoshita, K. Nagao and K. Tanjoh (2009). "Reduced effectiveness of vasopressin in repeated doses for patients
undergoing prolonged cardiopulmonary resuscitation." Resuscitation 80(7): 755-761.
INTRODUCTION: The efficacy of repeated administration of vasopressin alone during prolonged cardiopulmonary
resuscitation (CPR) remains unconfirmed. This study was conducted to estimate the effectiveness of the repeated
administration of vasopressin vs. epinephrine for cardiopulmonary arrest (CPA) patients receiving prolonged CPR.
METHODS: We conducted a prospective randomized controlled study on patients who experienced out-of-hospital CPA.
The patients were randomly assigned to receive a maximum of four injections of either 40IU of vasopressin (vasopressin
group) or 1mg of epinephrine (epinephrine group) immediately after emergency room (ER) admission. Patients who
received vasopressors before ER admission or suffered non-cardiogenic CPA were excluded after randomization.
RESULTS: In total, 336 patients were enrolled (vasopressin group, n=137; epinephrine group, n=118). No differences were
found between these groups (vasopressin group vs. epinephrine group) in the rates of return of spontaneous circulation
(ROSC) (28.7% vs. 26.6%), 24-h survival (16.9% vs. 20.3%), or survival to hospital discharge (5.6% vs. 3.8%). In a
subgroup analysis by the Fisher's exact test, the rate of ROSC was higher in the vasopressin group than in the epinephrine
group, among the patients whose arrests were witnessed (48.1% vs. 27.8%, p=0.010) or who received bystander CPR
(68.0% vs. 38.5%, p=0.033). When the independent predictors of ROSC were calculated in the subgroup analysis, however,
vasopressin administration (Odds ratio: 0.87-0.28) did not affect the outcome. CONCLUSIONS: This is the first report of a
possible vasopressin-alone resuscitation without additional epinephrine. However, repeated injections of either vasopressin
or epinephrine during prolonged advanced cardiac life support resulted in comparable survival.
Ong, M. E. H., L. Tiah, B. S. H. Leong, E. C. C. Tan, V. Y. K. Ong, E. A. T. Tan, B. Y. Poh, P. P. Pek and Y. Chen (2012). "A
randomised, double-blind, multi-centre trial comparing vasopressin and adrenaline in patients with cardiac arrest presenting to or in
the Emergency Department." Resuscitation 83(8): 953-960.
C2015 ALS_Vassopressors in cardiac arrest_220912
Objective: To compare vasopressin and adrenaline in the treatment of patients with cardiac arrest presenting to or in the
Emergency Department (ED). Design: A randomised, double-blind, multi-centre, parallel-design clinical trial in four adult
hospitals. Method: Eligible cardiac arrest patients (confirmed by the absence of pulse, unresponsiveness and apnea) aged
>16 (aged > 21 for one hospital) were randomly assigned to intravenous adrenaline (1. mg) or vasopressin (40. IU) at ED.
Patients with traumatic cardiac arrest or contraindication for cardiopulmonary resuscitation (CPR) were excluded. Patients
received additional open label doses of adrenaline as per current guidelines. Primary outcome was survival to hospital
discharge (defined as participant discharged alive or survival to 30 days post-arrest). Main results: The study recruited 727
participants (adrenaline = 353; vasopressin = 374). Baseline characteristics of the two groups were comparable. Eight
participants (2.3%) from adrenaline and 11 (2.9%) from vasopressin group survived to hospital discharge with no significant
difference between groups (p= 0.27, RR = 1.72, 95% CI = 0.65-4.51). After adjustment for race, medical history, bystander
CPR and prior adrenaline given, more participants survived to hospital admission with vasopressin (22.2%) than with
adrenaline (16.7%) (p= 0.05, RR = 1.43, 95% CI = 1.02-2.04). Sub-group analysis suggested improved outcomes for
vasopressin in participants with prolonged arrest times. Conclusions: Combination of vasopressin and adrenaline did not
improve long term survival but seemed to improve survival to admission in patients with prolonged cardiac arrest. Further
studies on the effect of vasopressin combined with therapeutic hypothermia on patients with prolonged cardiac arrest are
needed. (copyright) 2012 Elsevier Ireland Ltd.
Sherman, B. W., M. A. Munger, G. E. Foulke, W. F. Rutherford and E. A. Panacek (1997). "High-dose versus standard-dose
epinephrine treatment of cardiac arrest after failure of standard therapy." Pharmacotherapy 17(2): 242-247.
STUDY OBJECTIVE: To assess the efficacy of high-dose epinephrine (HDE) compared with standard-dose epinephrine
(SDE) in emergency department patients in cardiac arrest after SDE failed to improve asystole or ventricular fibrillation.
DESIGN: Prospective, multicenter, blinded, controlled trial. SETTING: Eight academic center emergency departments.
PATIENTS: One hundred forty patients treated for cardiac arrest. MEASUREMENTS AND MAIN RESULTS: Primary
outcomes were either improvement in cardiac rhythm or return of spontaneous circulation (ROSC). Of the 140 patients
enrolled, 78 received HDE and 62 received SDE. Of the 34 patients with ventricular fibrillation, 3 were resuscitated with HDE
and 2 with SDE (p = 0.60). Of those with asystole, ROSC occurred in 12 of HDE and 5 of SDE recipients (p = 0.11). No
patient had return of significant neurologic function and none survived to hospital discharge. Overall, there was no
advantage to HDE after failure of SDE. CONCLUSION: Our results are similar to those of controlled clinical trials comparing
HDE with SDE in cardiac arrest.
Stiell, I. G., P. C. Hebert, G. A. Wells, K. L. Vandemheen, A. S. L. Tang, L. A. J. Higginson, J. F. Dreyer, C. Clement, E. Battram, I.
Watpool, S. Mason, T. Klassen and B. N. Weitzman (2001). "Vasopressin versus epinephrine for inhospital cardiac arrest: A
randomised controlled trial." Lancet 358(9276): 105-109.
Background: Survival rates for cardiac arrest patients, both in and out of hospital, are poor. Results of a previous study
suggest better outcomes for patients treated with vasopressin than for those given epinephrine, in the out-of-hospital setting.
Our aim was to compare the effectiveness and safety of these drugs for the treatment of in-patient cardiac arrest. Methods:
We did a triple-blind randomised trial in the emergency departments, critical care units, and wards of three Canadian
teaching hospitals. We assigned adults who had cardiac arrest and required drug therapy to receive one dose of
C2015 ALS_Vassopressors in cardiac arrest_220912
vasopressin 40 U or epinephrine 1 mg intravenously, as the initial vasopressor. Patients who failed to respond to the study
intervention were given epinephrine as a rescue medication. The primary outcomes were survival to hospital discharge,
survival to 1 h, and neurological function. Preplanned subgroup assessments included patients with myocardial ischaemia or
infarction, initial cardiac rhythm, and age. Findings: We assigned 104 patients to vasopressin and 96 to epinephrine. For
patients receiving vasopressin or epinephrine survival did not differ for hospital discharge (12 [12%] vs 13 [14%],
respectively; p=0.67; 95% Cl for absolute increase in survival -11.8% to 7.8%) or for 1 h survival (40 [39%] vs 34 [35%];
p=0.66; -10.9% to 17.0%); survivors had closely similar median mini-mental state examination scores (36 [range 19-38] vs
35 [20-40]; p=0.75) and median cerebral performance category scores (1 vs 1). Interpretation: We failed to detect any
survival advantage for vasopressin over epinephrine. We cannot recommend the routine use of vasopressin for inhospital
cardiac arrest patients, and disagree with American Heart Association guidelines, which recommend vasopressin as
alternative therapy for cardiac arrest.
Wenzel, V., A. C. Krismer, H. R. Arntz, H. Sitter, K. H. Stadlbauer and K. H. Lindner (2004). "A comparison of vasopressin and
epinephrine for out-of-hospital cardiopulmonary resuscitation." N Engl J Med 350(2): 105-113.
BACKGROUND: Vasopressin is an alternative to epinephrine for vasopressor therapy during cardiopulmonary resuscitation,
but clinical experience with this treatment has been limited. METHODS: We randomly assigned adults who had had an outof-hospital cardiac arrest to receive two injections of either 40 IU of vasopressin or 1 mg of epinephrine, followed by
additional treatment with epinephrine if needed. The primary end point was survival to hospital admission, and the
secondary end point was survival to hospital discharge. RESULTS: A total of 1219 patients underwent randomization; 33
were excluded because of missing study-drug codes. Among the remaining 1186 patients, 589 were assigned to receive
vasopressin and 597 to receive epinephrine. The two treatment groups had similar clinical profiles. There were no significant
differences in the rates of hospital admission between the vasopressin group and the epinephrine group either among
patients with ventricular fibrillation (46.2 percent vs. 43.0 percent, P=0.48) or among those with pulseless electrical activity
(33.7 percent vs. 30.5 percent, P=0.65). Among patients with asystole, however, vasopressin use was associated with
significantly higher rates of hospital admission (29.0 percent, vs. 20.3 percent in the epinephrine group; P=0.02) and hospital
discharge (4.7 percent vs. 1.5 percent, P=0.04). Among 732 patients in whom spontaneous circulation was not restored with
the two injections of the study drug, additional treatment with epinephrine resulted in significant improvement in the rates of
survival to hospital admission and hospital discharge in the vasopressin group, but not in the epinephrine group (hospital
admission rate, 25.7 percent vs. 16.4 percent; P=0.002; hospital discharge rate, 6.2 percent vs. 1.7 percent; P=0.002).
Cerebral performance was similar in the two groups. CONCLUSIONS: The effects of vasopressin were similar to those of
epinephrine in the management of ventricular fibrillation and pulseless electrical activity, but vasopressin was superior to
epinephrine in patients with asystole. Vasopressin followed by epinephrine may be more effective than epinephrine alone in
the treatment of refractory cardiac arrest.
C2015 ALS_Vassopressors in cardiac arrest_220912
Excluded studies (and why excluded)
There were 10 excluded at full manuscript stage (Figure 1): 6 were not RCT and 4 were not the pre-specified intervention.
Carvolth et al.,
1995
Not randomized
Kleinschmidt S,
2004
Commentary, German
Linder et al.,
1991
Wrong interventions
Lindner KH, Ahnefeld FW, Grünert A. Epinephrine versus norepinephrine in prehospital
ventricular fibrillation. The American Journal of Cardiology. 1991;67(5):427-8.
Linder et al.,
1991
Unable to separate outcomes
between OHCA and IHCA
Linder, 1993
Review
Lindner KH, Ahnefeld FW, Prengel AW. Comparison of standard and high-dose adrenaline in
the resuscitation of asystole and electromechanical dissociation. Acta Anaesthesiologica
Scandinavica. 1991;35(3):253-6.
Lindner KH. Adrenergic agonist drug administration during cardiopulmonary resuscitation.
Critical care medicine. 1993;21(9 SUPPL):S324-S5.
Lipman et al.,
1993
IHCA population
Olasveengen et
al., 2009
Indirect interventions and unable to
calculate Epinephrine and placebo
effect
Not randomized
Polglase et al.,
1994
Carvolth RD. Comparison of high-dose epinephrine versus standard-dose epinephrine in adult
cardiac arrest in the prehospital setting. Prehospital and Disaster Medicine. 1996;11(3):21922.
Kleinschmidt S. Vasopressin versus adrenaline in the therapy of preclinical cardiopulmonary
arrest. Anaesthesist. 2004;53(6):579-80.
Lipman J, Wilson W, Kobilski S, Scribante J, Lee C, Kraus P, et al. High-dose adrenaline in
adult in-hospital asystolic cardiopulmonary resuscitation: a double-blind randomised trial.
Anaesthesia & Intensive Care. 1993;21(2):192-6.
Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug
administration during out-of-hospital cardiac arrest: a randomized trial. JAMA.
2009;302(20):2222-9.
Polglase RF, Parish DC, Camp B. Prehospital administration of high-dose epinephrine.
American Journal of Emergency Medicine. 1994;12(6):688-9.
Woodhouse et
al., 1995
Unable to separate outcomes
between OHCA and IHCA
Woodhouse SP, Cox S, Boyd P, Case C, Weber M. High dose and standard dose adrenaline do
not alter survival, compared with placebo, in cardiac arrest. Resuscitation. 1995;30(3):243-9.
Worster et al.,
2005
Commentary
Worster A, Upadhye S, Fernandes CMB. Vasopressin versus epinephrine for out-of-hospital
cardiopulmonary resuscitation. Canadian Journal of Emergency Medicine. 2005;7(1):48-50.