Physiology 25 [5-11
advertisement
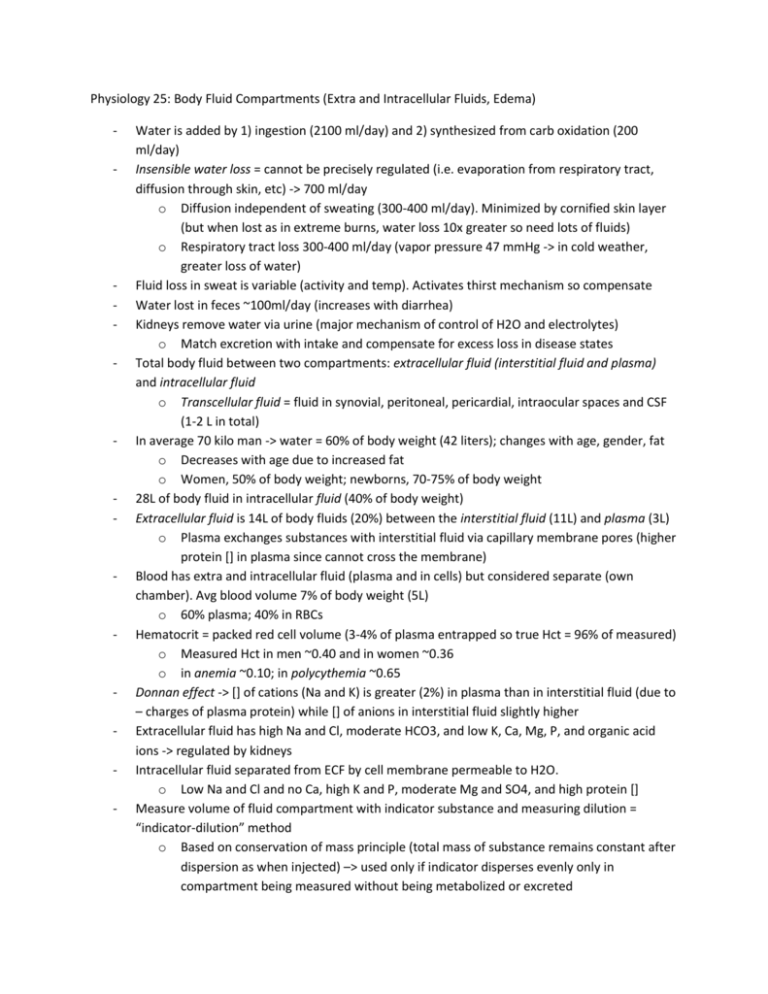
Physiology 25: Body Fluid Compartments (Extra and Intracellular Fluids, Edema) - - - - - - - Water is added by 1) ingestion (2100 ml/day) and 2) synthesized from carb oxidation (200 ml/day) Insensible water loss = cannot be precisely regulated (i.e. evaporation from respiratory tract, diffusion through skin, etc) -> 700 ml/day o Diffusion independent of sweating (300-400 ml/day). Minimized by cornified skin layer (but when lost as in extreme burns, water loss 10x greater so need lots of fluids) o Respiratory tract loss 300-400 ml/day (vapor pressure 47 mmHg -> in cold weather, greater loss of water) Fluid loss in sweat is variable (activity and temp). Activates thirst mechanism so compensate Water lost in feces ~100ml/day (increases with diarrhea) Kidneys remove water via urine (major mechanism of control of H2O and electrolytes) o Match excretion with intake and compensate for excess loss in disease states Total body fluid between two compartments: extracellular fluid (interstitial fluid and plasma) and intracellular fluid o Transcellular fluid = fluid in synovial, peritoneal, pericardial, intraocular spaces and CSF (1-2 L in total) In average 70 kilo man -> water = 60% of body weight (42 liters); changes with age, gender, fat o Decreases with age due to increased fat o Women, 50% of body weight; newborns, 70-75% of body weight 28L of body fluid in intracellular fluid (40% of body weight) Extracellular fluid is 14L of body fluids (20%) between the interstitial fluid (11L) and plasma (3L) o Plasma exchanges substances with interstitial fluid via capillary membrane pores (higher protein [] in plasma since cannot cross the membrane) Blood has extra and intracellular fluid (plasma and in cells) but considered separate (own chamber). Avg blood volume 7% of body weight (5L) o 60% plasma; 40% in RBCs Hematocrit = packed red cell volume (3-4% of plasma entrapped so true Hct = 96% of measured) o Measured Hct in men ~0.40 and in women ~0.36 o in anemia ~0.10; in polycythemia ~0.65 Donnan effect -> [] of cations (Na and K) is greater (2%) in plasma than in interstitial fluid (due to – charges of plasma protein) while [] of anions in interstitial fluid slightly higher Extracellular fluid has high Na and Cl, moderate HCO3, and low K, Ca, Mg, P, and organic acid ions -> regulated by kidneys Intracellular fluid separated from ECF by cell membrane permeable to H2O. o Low Na and Cl and no Ca, high K and P, moderate Mg and SO4, and high protein [] Measure volume of fluid compartment with indicator substance and measuring dilution = “indicator-dilution” method o Based on conservation of mass principle (total mass of substance remains constant after dispersion as when injected) –> used only if indicator disperses evenly only in compartment being measured without being metabolized or excreted - - - - - - - - - o Volume B = (Volume A * [A]) / [B] Radioactive water (tritium, 3H2O) or heavy water (deutirum, 2H2O) used to measure total body water -> dilution principle o Can also use antipyrine (penetrates cell membranes and distributes uniformly) ECF volume estimated using radioactive Na, Cl, or iothalamate, thiosulfate ion, and inulin (do not penetrate cell membrane so remain in ECF) o Radioactive Na may diffuse into cells in small amount so ECF volume measurement aka sodium space or inulin space Intracellular volume = Total body water – Extracellular volume Measure plasma volume using 125I-albumin or Evans blue dye (aka T-1824; binds plasma proteins) -> remain in vascular system after injection Interstitial fluid volume = ECF volume – Plasma volume If plasma volume and hematocrit value known, calculate: total blood volume = plasma volume/(1 – Hct) o Can also measure via radioactively labeled (51Cr) RBCs ECF distribution determined by hydrostatic and colloid osmotic forces across capillaries o Fluid distribution between ECF and ICF determined by osmotic effect of Na, Cl and electrolytes across cell membrane (remain isotonic via H2O osmosis) Osmosis is net diffusion of water across a selectively permeable membrane from high [water] to lower [water] o Higher the solute [] the lower the water []; water diffuses from low solute [] to high solute [] o Rate of diffusion of water = rate of osmosis Osmoles (osm) = total number of osmotically active particles in solution (not molar []) o 1 osm = 1 mol (6.02 x 1023) of solute particles (if a molecule dissociates into 2, 1 mol/L = 2 osm/L; dissociates into 3, 1 mol/L = 2 osm/L) o Usually use milliosmole (mOsm) Osmolality = osmoles per kilogram of water Osmolarity = osmoles per liter of solution o Two terms almost synonymous in dilute solutions Van’t Hoff’s law (calculate osmolarity and osmotic pressure of a solution) -> 1% solution means 1g/mL (molarity). Molarity divided by molecular weight = mol/L. Multiply by Osm = osm/L (osmolarity) o Osmotic coefficient corrects for deviations in predictions 80% of osmolarity of ECF is from Na and Cl ions; 50% of osmolarity of ICF from K o Total osmolarly of each compartment ~300 mOsm/L (plasma is 1 mOsm/L greater from osmotic effect of plasma protein) Corrected Osmolar activities = take into account interionic attractions which may cause decrease in “activity” For each mOsm [] gradient of Impermeant solute (will not permeate cell membrane), 19.3 mmHg osmotic pressure exerted -> forces that move water across membrane Isotonic solution = ECF impermeant solute same as ICF (~282 mOsm/L) - - - - - o Ex. 0.9% NaCl or 5% glucose Hypotonic solution = impermeant solute <282 mOsm/L in ECF than ICF -> cell swelling o Ex. <0.9% NaCl Hypertonic solution = impermeant solute >282 mOsm/L in ECF than ICF -> cell shrinking o Ex. >0.9% NaCl Isosmotic = solutions with osm same as cell Hyperosmotic and hypo-osmotic = solutions with higher or lower osmolarity than ECF Rapid movement of H2O corrects imbalances quickly (but equilibrium not met quickly -> takes 30 mins for osmotic equilibrium after drinking water) Water moves rapidly across cell membranes (osm of ECF and ICF equal) Cell membranes almost completely impermeable to solutes (osm constant unless solutes added or lost to ECF) Effects of saline solutions to ECF: o Hypertonic solutions added cause rise in osmolarity of both compartments and increase in EC volume o Isotonic solutions cause increase in EC volume o Hypotonic solution causes ECF osmolarity to decrease and IC and EC volumes to increase Calculation of fluid shifts and osmolarities (hypertonic saline) -> o calculate volume, [], and mOsm in each compartment o Calculate total mOsm added to ECF and values instantly after infusion o Calculate volumes and [] occurring after osmotic equilibrium IV solutions administered to provide nutrition to people (glucose, AA, and homogenized fat solutions) o Adjusted to isotonicity; after metabolized, excess H2O remains (dilute urine) so only nutrients added Plasma Na concentration (evaluates pts fluid status) o When <142 mEq/L = hyponatremia; when > 142 mEq/L = hypernatremia Causes of hyponatremia = excess water or loss of NaCl -> rapid change causes cell swelling (brain cell edema and neurological symptoms of headache, nausea, lethargy, and disorientation, herniation) but if slower, electrolytes and solutes go from cells to ECF to attenuate o Hyponatremia-dehydration -> diarrhea, vomiting, diuretics overuse, Addison’s disease (low aldosterone) o Hyponatremia-overhydration -> excessive ADH secretion o If IV fluids used too rapidly to correct -> demyelination. Avoid by limiting to <10-12 mmol/L/day and <18 mmol/L/48 hours Causes of hypernatremia = excess sodium or water loss -> cell shrinkage (less consequences because intense thirst but hypothalamic lesions impair thirst sense and age may alter mental status) o Hypernatremia –dehydration -> inability secrete ADH (diabetes insipidus) or renal insensitivity to ADH (nephrogenic diabetes insipidus), dehydration (prolonged sweating) o Hypernatremia-overhydration -> excessive aldosterone secretion (balanced by H2O retention along with Na) - - - - - - - o Correct with hypo-osmotic NaCl or dextrose solutions slowly in chronic cases Edema = presence of excess fluid in body tissues (mainly in ECF) o Intracellular Edema -> hyponatremia, depressed metabolic systems of tissues, lack of adequate cell nutrition (ischemia), inflammation (increasing permeability) o Extracellular Edema -> abnormal leakage from plasma to interstitial spaces, failure of lymphatics (lymphedema) Most common cause = excessive capillary fluid filtration Capillary filtration rate = Kf x (Pc-Pif – πc + πif) o Increased Kf, Pc, or decreased πc can increase filtration rate Lymphedema can cause edema because proteins not removed drawing fluid out o Occurs with infection = filaria nematodes (Wuchereria bancrofti) (spread from person to person by mosquitoes) -> elephantiasis or hydrocele o Can occur in cancer or surgery (mastectomy) Increased Pc -> excess retention of Na and H2O (kidney failure, mineralocorticoid excess), high venous P and venous constriction (heart failure, venous obstruction, failure of venous pumps by paralysis, immobilization or valve failure), decreased arteriolar resistance (excess heat, insufficient sympathetics, vasodilators) Decreased πc -> nephrotic syndrome (proteinuria), protein loss from burns or wounds, failure to produce proteins (liver cirrhosis, malnutrition) Increased Kf -> immune reactions with histamine, toxins, bacterial infection, vitamin (C) deficiency, ischemia, burns Blockage of lymph -> cancer, infections, surgery, congenital absence/abnormality of lymphatics Heart failure -> raises venous pressure causing high capillary filtration, BP falls (kidney retains fluid and Na and renin-angiotensin II system activation) causing edema o In L heart failure -> pulmonary edema Decreased kidney excretion of Na and H2O -> so remains in blood increasing interstitial fluid volume (extracellular edema) and hypertension o Ex. glomerulonephritis Decreased plasma proteins reduce πc increasing capillary filtration o Ex. nephrotic syndrome (proteinuria), cirrhosis of the liver (which also compresses abdominal venous drainage -> ascites) 3 safety factors to prevent edema (total = 17 mmHg of safety): o Low compliance of interstitium when interstitial fluid P is negative Adds slight suction to hold tissue together (normally -3 mmHg so gives 3 mmHg of safety factor) and allows sufficient capillary filtration Fluid in interstitium is in gel form (proteoglycan meshwork) -> prevents fluid from flowing easily and offers elastic resistance to compression. Without gel -> free fluid in tissues causing pitting edema o Nonpitting edema from tissue cells swelling or when interstitium clotted with fibrinogen - - Proteoglycan filaments act as “spacer” between cells allowing rapid diffusion of nutrients, electrolytes, and cell waste products (but preventing too easy of flow) o Lymph flow increase 10-50 fold Carries away large amounts of fluid and proteins maintaining (-) interstitial pressure. Safety factor ~7mmHg o Washdown of interstitial fluid protein [] Increased lymph flow removes proteins from interstitium preventing further edema. Safety factor ~7 mmHg Potential spaces = pleural, pericardial, peritoneal, and synovial cavities o Fluid in adjacent capillaries diffuses in and proteins collect so lymphatics remove them and return to circulation o Edema fluid in potential space = effusion (from lymph blockage or excess capillary filtration) In the abdomen = ascites o Normal fluid pressure in potential spaces = negative