HTAs performed
advertisement
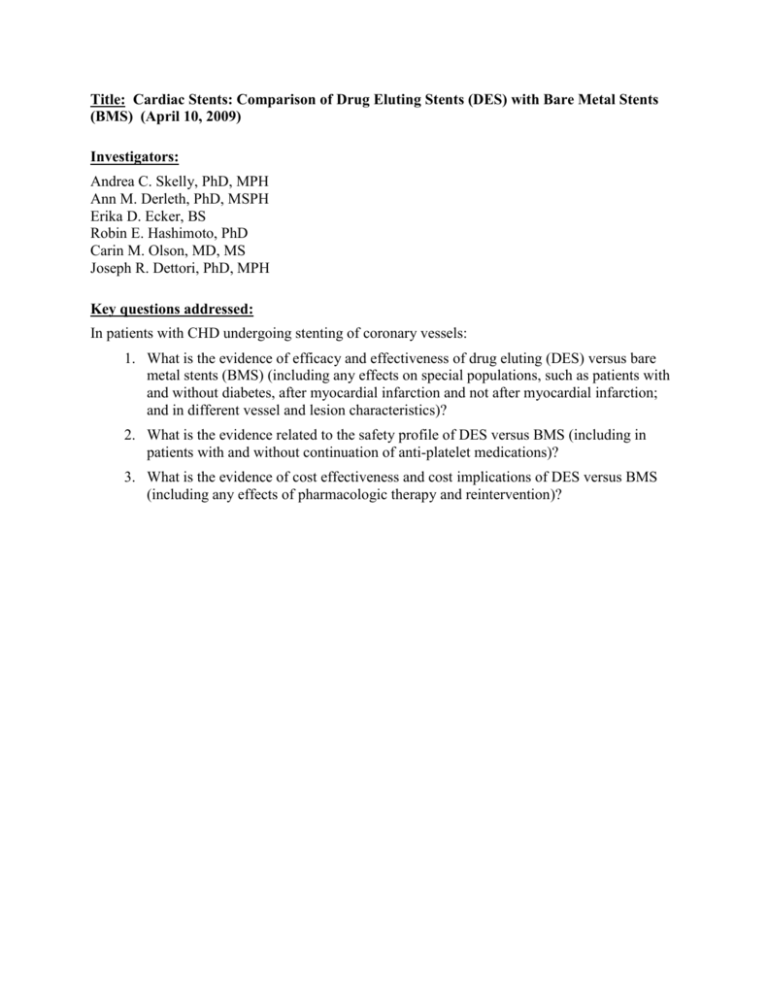
Title: Cardiac Stents: Comparison of Drug Eluting Stents (DES) with Bare Metal Stents (BMS) (April 10, 2009) Investigators: Andrea C. Skelly, PhD, MPH Ann M. Derleth, PhD, MSPH Erika D. Ecker, BS Robin E. Hashimoto, PhD Carin M. Olson, MD, MS Joseph R. Dettori, PhD, MPH Key questions addressed: In patients with CHD undergoing stenting of coronary vessels: 1. What is the evidence of efficacy and effectiveness of drug eluting (DES) versus bare metal stents (BMS) (including any effects on special populations, such as patients with and without diabetes, after myocardial infarction and not after myocardial infarction; and in different vessel and lesion characteristics)? 2. What is the evidence related to the safety profile of DES versus BMS (including in patients with and without continuation of anti-platelet medications)? 3. What is the evidence of cost effectiveness and cost implications of DES versus BMS (including any effects of pharmacologic therapy and reintervention)? Title: Artificial Disc Replacement (ADR) (August 26, 2008) Investigators: Joseph R. Dettori, PhD, MPH Andrea C. Skelly, PhD, MPH Robin E. Hashimoto, PhD Erika Ecker, BS Key questions addressed: 1. What is the evidence of efficacy and effectiveness of ADR compared with comparative therapies (including non-operative therapy; spinal fusion; other surgery)? 2. What is the evidence related to the ADR safety profile? (including device failure, reoperation) 3. What is the evidence of differential efficacy or safety issues amongst special populations (including but not limited to the elderly and workers compensation populations)? 4. What are the cost implications and cost effectiveness for ADR? Title: Total Knee Arthroplasty (Septemeber 15, 2010) Investigators: Joseph R. Dettori, PhD, MPH Erika Ecker, BS Daniel Norvell, PhD Robin Hashimoto, PhD Nora B. Henrikson, PhD, MPH Lisa Kercher, PhD, MPH, Kara McMullen, MPH Annie Raich, MS, MPH Key questions addressed: When used in adult patients: 1. What is the evidence of efficacy and effectiveness of using computer-navigated total knee arthroplasty (CN-TKA) compared with conventional TKA? Outcomes to consider: a. Primary: Clinical outcomes, Revision rates b. Secondary: Radiographic, other reported outcomes 2. What is the evidence of efficacy and effectiveness of partial knee arthroplasty compared with conventional TKA? Include consideration of: a. Unicompartmental b. Bicompartmental c. Bi-unicompartmental 3. Whatis the evidence of the safety of computer-navigated TKA or partial knee arthroplasty compared with standard total knee arthroplasty? Including consideration of: a. Adverse events type and frequency (mortality, major morbidity, other) b. Deep venous thrombosis 4. What is the evidence that TKA or partial knee arthroplasty has differential efficacy or safety issues in sub populations? Including consideration of: a. Gender b. Age c. BMI d. Diagnosis, including osteoarthritis versus rheumatoid arthritis e. Psychological or psychosocial co-morbidities f. Other patient characteristics or evidence based patient selection criteria g. Provider type, setting or other provider characteristics h. Payor or beneficiary type, including worker’s compensation, Medicaid, state employees i. Bilateral TKA (simultaneous or staged) 5. What is the evidence of cost implications and cost-effectiveness of computernavigated TKA or partial knee arthroplasty compared with knee joint arthroplasty? Title: Hip Surgery Procedures for Treatment of Femoroacetabular Impingement Syndrome (August 26, 2011) Investigators: Joseph R. Dettori, PhD, MPH Robin Hashimoto, PhD Erika Brodt, BS Key questions addressed: 1. Is there a consistent or agreed upon case definition for FAI? What is the evidence of reliability and validity of these case definitions? 2. What are the expected treatment outcomes of hip surgery for FAI? Are there validated instruments related to hip surgery outcomes? Has clinically meaningful improvement in outcomes been defined for FAI? 3. What is the evidence of efficacy and effectiveness of hip surgery (open or arthroscopic) compared with no surgery for FAI? Including consideration of short-term and long-term: • Need of or time to total hip arthroplasty • Development or progression of osteoarthritis • Impact on function, pain, range of motion, quality of life, activities of daily living and return to work 4. What is the evidence of the safety of hip surgery for FAI compared with no surgery? Including consideration of: • Revision/re-operation rates • Adverse events type and frequency (peri-operative, fractures, nerve damage, mortality, other major morbidity) 5. What is the evidence that hip surgery for FAI compared with no surgery has differential efficacy or safety issues in sub populations? Including consideration of: • Gender • Age • Psychological or psychosocial comorbidities • Baseline functional status: e.g. type of deformity, extent of osteoarthritis or cartilage damage • Other patient characteristics or evidence-based patient selection criteria • Provider type, setting or other provider characteristics • Payer/beneficiary type: including worker’s compensation, Medicaid, state employees 6. What evidence of cost implications and cost-effectiveness of hip surgery compared with no surgery exists for FAI? Including consideration of: • Costs (direct and indirect) and cost effectiveness • Short-term and long-term Title: Microprocessor-controlled Lower Limb Prostheses (October 12, 2011) Investigators: Nora B. Henrikson, PhD, MPH Brian J. Hafner, PhD Joseph R. Dettori, PhD, MPH Daniel C. Norvell, PhD Annie Raich, MPH Erika D. Brodt, BS Andrea C. Skelly, PhD MPH Key questions addressed: When used in patients living with lower limb loss: 1. What are the expected treatment outcomes of use of microprocessorcontrolled lower limb prosthetics? Are there validated instruments related to measurement of outcomes of this technology? Has clinically meaningful improvement in outcomes been defined for use of this technology? 2. What is the evidence of efficacy and effectiveness of microprocessorcontrolled lower limb prosthetics? Including consideration of validated tools to measure both short term and long term outcomes: a. Energy and cognitive requirements of ambulation b. Impact on ambulation: daily step frequency; estimated step distance; performance on level or varied surfaces; stopping and standing safely, adaptation to different walking speeds, with estimation of number of falls c. Patient perception; QOL; impact on activities of daily living; work; work performance 3. What is the evidence about the safety microprocessor-controlled lower limb prosthetics? Including consideration of: a. Adverse events type and frequency (mortality, other major morbidity) b. Equipment failure, equipment longevity, reoperation c. Ulcers, infections, falls, etc. 4. What is the evidence that microprocessor-controlled lower limb prosthetics has differential efficacy or safety issues in sub populations? Including consideration of: a. Gender b. Age c. Psychological or psychosocial co-morbidities d. Baseline functional status using instruments such as Medicare’s Orthotics and Prosthetics K levels of function. e. Other patient characteristics or evidence based patient selection criteria such as stump length and BMI f. Provider type, setting or other provider characteristics g. Payor/ beneficiary type: including worker’s compensation, Medicaid, state employees 5. What evidence of cost implications and cost-effectiveness of microprocessorcontrolled lower limb prosthetics? Including consideration of: a. Costs (direct and indirect) and cost effectiveness b. Short term and long term c. Ongoing maintenance and replacements for the prosthetic Title: Osteochondral Allograft/Autograft Transplantation (OAT) (October 17, 2011) Investigators: Andrea C. Skelly, PhD, MPH Erika D. Ecker, BS Jeannette M. Schenk‐Kisser, PhD, MS Barbara C. Leigh, PhD, MPH Annie Raich, MS, MPH With assistance from: Robin E. Hashimoto, PhD Jeffrey T. Hermsmeyer, BA Key questions addressed: When used in patients with cartilage damage: 1. What is the case definition of a patient suitable for OATS/mosaicplasty surgery, and are there measures of reliability and validity for case identification? a. What are the maximum, minimum, and optimum size (volume) of the damage that is suitable for repair using OATS/mosaicplasty? b. What are the maximum and optimum number of lesions that can be repaired in a single OATS/mosaicplasty procedure? c. Are there other considerations that make OATS/mosaicplasty suitable or unsuitable (age, mobility, comorbidities, BMI)? d. Is there a distinction between OATS and mosaicplasty, and a related case definition difference between the two? e. Is there a distinction between cases where autograft versus allograft OATS/mosaicplasty is preferable? 2. What are the expected treatment outcomes of OATS/mosaicplasty, and are there validated instruments and scores to measure clinically meaningful improvement? 3. What is the evidence of efficacy and effectiveness of OATS/mosaicplasty (open or arthroscopic)? Including consideration of short term and long term: a. Delay or avoidance of progression to osteoarthritis b. Impact on function, pain, range of motion, quality of life, activities of daily living and return to work c. Longevity of treatment effect d. Need for continuing and/or subsequent intervention e. Need for extended or continuing physical therapy f. Recovery time considering harvest site recovery issues g. Differential results from multiple versus single grafts, patterning for multiple grafts (linear arrangement versus circular arrangement) h. Differential results between allograft and autograft procedures i. Differential results between open and arthroscopic procedures j. Differential results in centers of excellence 4. What is the evidence of the safety of OATS surgery? Including consideration of: a. Adverse events type and frequency (peri-operative, cartilage plug detachment, cartilage rejection, graft fit, harvest site issues, development of fibrocartilage, mortality, other major morbidity such as DVT, deep infection, and excessive intraarticular bleeding) b. Revision/re-operation rates (if not addressed in efficacy) 5. What is the evidence that OATS surgery has differential efficacy or safety issues in sub populations? Including consideration of: a. Gender b. Age c. Psychological or psychosocial co-morbidities d. Baseline functional status: e.g. type of injury or lesion, extent of cartilage damage, specific damage site size, number of damage sites e. Other patient characteristics or evidence based patient selection criteria, especially comorbidities of diabetes and high BMI f. Provider type, setting or other provider characteristics g. Payor/ beneficiary type: including worker’s compensation, Medicaid, state employees 6. What is the evidence of cost implications and cost-effectiveness for OATS/mosaicplasty? Including consideration of: a. Costs (direct and indirect) and cost effectiveness b. Short term and long term Title: Hip Resurfacing (October 03, 2009) Investigators: Robin Hashimoto, PhD Joseph R. Dettori, PhD, MPH Nora B. Henrikson, PhD, MPH Erika Ecker, BS Jeff Hermsmeyer, BS Key questions addressed: Hip Resurfacing is an alternative surgery to total hip replacement (THR). When used as an alternative in patients where total hip replacement is indicated: 1. What’s the evidence of efficacy and effectiveness of hip resurfacing? 2. What is the evidence about the safety profile for hip resurfacing? 3. What is the evidence that the use of hip resurfacing improves clinical outcomes compared to conventional total hip replacement? 4. Is there evidence of differential efficacy or safety issues with use of hip resurfacing? 5. What is the evidence of cost implications and cost effectiveness of hip resurfacing? Title: Spinal Cord Stimulation (July 23, 2010) Investigators: Robin Hashimoto, PhD Joseph R. Dettori, PhD, MPH Nora B. Henrikson, PhD, MPH Lisa Kercher PhD, MPH Key questions addressed: Spinal cord stimulators are surgically implanted devices used to deliver electrical stimulation to the spinal cord to treat pain. When used in adult patients with chronic pain (neuropathic) who have failed alternative therapies: 1. What is the evidence of efficacy and effectiveness of spinal cord stimulation? Including consideration of: a. Short-term and long-term outcomes b. Impact on Function, Pain, Quality of life c. Other reported measures including: use of pain medications and opiods, return to work; intensity and duration of use 2. What is the evidence of the safety of spinal cord stimulation? Including consideration of: a. Adverse events type and frequency (mortality, major morbidity, other) b. Revision and removal rates including loss of paresthesia (if not addressed in efficacy) c. Infections d. Lead migration e. Technical malfunctions (e.g., early battery failure, broken leads) 3. What is the evidence that spinal cord stimulation has differential efficacy or safety issues in subpopulations? Including consideration of: a. Gender b. Age c. Psychological or psychosocial co-morbidities d. Diagnosis or pain type e. Other patient characteristics or evidence based patient selection criteria f. Provider type, setting or other provider characteristics g. Health care system type, including worker’s compensation, Medicaid, state employees 4. What evidence of cost implications and cost-effectiveness of spinal cord stimulators? Including consideration of: a. Costs (direct and indirect) in short term and over expected duration of use b. Replacement Title: Spinal Injections (March 10, 2011) Investigators: Robin Hashimoto, PhD Annie Raich, MPH Erika Ecker, BS Nora B. Henrikson, PhD, MPH Leslie Wallace, MPH Joseph R. Dettori, PhD, MPH Roger Chou, MD Key questions addressed: Spinal injections are used to treat chronic back or neck pain with or without radiculopathy when more conservative care has not provided relief. Spinal injections include epidural injections, facet joint injections, medial branch blocks, sacroiliac joint injections, and intradiscal steroid injections. When used in adult patients with chronic back or neck pain: 1. What is the evidence of efficacy and effectiveness of spinal injections? Including: a. Short term and long term measures, including measures related to: repeated spinal injections multilevel spinal injections bilateral vs. unilateral spinal injections b. Impact on clinically meaningful physical function and pain, c. Impact on quality of life, patient satisfaction d. Opiod use, return to work and any other reported surrogate measures 2. What is the evidence of the safety of spinal injections? Including: a. Adverse event type and frequency (mortality, major morbidity, other) b. Dural or arachnoid puncture; c. Infection; d. Epidural or intradural hematoma e. Allergic reaction f. Nerve or spinal cord injury g. Artery/vein damage/puncture h. Arachnoiditis 3. What is the evidence that spinal injections have differential efficacy or safety issues in sub populations? Including consideration of: a. Gender b. Age c. Psychological or psychosocial co-morbidities d. Diagnosis or time elapsed from fracture e. Other patient characteristics or evidence based patient selection criteria f. Provider type, setting or other provider characteristics g. Payor/ beneficiary type: including worker’s compensation, Medicaid, state employees 4. What evidence of cost implications and cost-effectiveness of spinal injections? Including: a. Direct costs over short term and over expected duration of effect b. Comparative costs Title: Glucose Monitoring: Self-monitoring in individuals with insulin dependent diabetes, 18 years of age or under (January 14, 2011) Investigators: Andrea C. Skelly, PhD, MPH Jeannette M. Schenk Kisser, PhD, MS Jennifer A. Mayfield, MD, MPH Carin M. Olson, MD, MS Erika D. Ecker, BS With assistance from: Ellen Van Alstyne, MS Nora B. Henrikson, PhD, MPH Key questions addressed: For patients 18 years of age or under with insulin requiring diabetes mellitus: 1. What is the evidence of efficacy and effectiveness of self-glucose monitoring? Including consideration of: a. Achieving target A1C levels b. Maintaining target A1C levels c. In conjunction with provider specific report cards for target (e.g. under 7/over 9) d. Reduce hospitalizations or acute episodes of diabetic ketoacidosis, hyperglycemia and hypoglycemia e. Reduce microvascular complications (retinopathy, nephropathy, neuropathy) f. Reduce Mortality g. Effect on medication or nutritional management h. Quality of life 2. What is the evidence on optimal or improved efficacy or effectiveness of glucose monitoring based on frequency or mode (continuous versus self-monitoring) of testing? 3. What is the evidence of the safety of glucose monitoring? Including consideration of: a. Adverse events type and frequency (mortality, major morbidity, other) 4. What is the evidence that glucose monitoring has differential efficacy or safety issues in subpopulations? Including consideration of: a. Gender b. Age (differential within the 18 and under population) c. Psychological or psychosocial co-morbidities d. Other patient characteristics or evidence based patient selection criteria e. Provider type, setting or other provider characteristics f. Health care payer type, including worker’s compensation, Medicaid, state employees 5. What is the evidence of cost implications and cost-effectiveness of self-glucose monitoring? Including consideration of: a. Costs (direct and indirect) in short term and over expected duration of use b. Estimates of costs saved by preventing morbid events Title: Electrical Nerve Stimulation for the Treatment of Pain (November 13, 2009) Investigators: Jocelyn M. Weiss, PhD, MPH Andrea C. Skelly, PhD, MPH Nora Henrikson, PhD, MPH Lisa Kercher, PhD, MPH Joseph R. Dettori, PhD, MPH With assistance from: Erika D. Ecker, BS Key questions addressed: When used to treat persons with pain: 1. What’s the evidence of efficacy and effectiveness of ENS? 2. What is the evidence about the safety profile for ENS? 3. What is the evidence that the use of ENS units improve clinical outcomes? 4. Is there evidence of differential efficacy or safety issues with use of ENS? 5. What is the evidence of cost implications and cost effectiveness of ENS? Title: Vertebroplasty, Kyphoplasty and Sacroplasty (November 4, 2010) Investigators: Barbara C. Leigh, PhD, MPH Andrea C. Skelly, PhD, MPH Nora B. Henrikson, PhD, MPH Lisa Kercher, PhD, MPH, Megan Skinner, BA, MPH Key questions addressed: When used in patients with spinal pain due to vertebral fracture: 1. What is the evidence of efficacy and effectiveness of vertebroplasty, kyphoplasty or sacroplasty? Including consideration of: a. Short-term and long-term outcomes b. Impact on function, pain, quality of life c. Other reported measures including: use of pain medications and opioids, return to work 2. What is the evidence of the safety of vertebroplasty, kyphoplasty or sacroplasty? Including consideration of: a. Adverse events type and frequency (mortality, major morbidity, other) b. Revision/re-operation rates (if not addressed in efficacy) 3. What is the evidence that vertebroplasty, kyphoplasty or sacroplasty has differential efficacy or safety issues in sub populations? Including consideration of: a. Gender b. Age c. Psychological or psychosocial co-morbidities d. Diagnosis or time elapsed from fracture e. Other patient characteristics or evidence based patient selection criteria f. Provider type, setting or other provider characteristics g. Payer/beneficiary type: including worker’s compensation, Medicaid, state employees 4. What is the evidence of cost implications and cost-effectiveness of vertebroplasty, kyphoplasty and sacroplasty? Including consideration of: a. Costs (direct and indirect) in the short term and over expected duration of use b. Revision/re-operation (if not addressed in efficacy) Title: On- and Off-label Uses of rhBMP-2 or rhBMP-7 for Spinal Fusion (February 14, 2012) Investigators: Robin Hashimoto, PhD Annie Raich, MPH Emily Yoder, BA Kara McMullen, MPH Joseph R. Dettori, PhD MPH With assistance from Nora B. Henrikson, PhD MPH Erika D. Brodt, BS Andrea Skelly, PhD MPH Key questions addressed: When used in patients undergoing spinal fusion: 1. What are the expected treatment outcomes of primary single or multilevel lumbar or cervical spinal fusion for degenerative disc disease (DDD), and of revision posterolateral lumbar spinal fusion in compromised patients (i.e., osteoporosis, smoking, diabetes)? Are there validated instrument related to outcomes in patients undergoing these procedures? Has clinically meaningful improvement in outcomes been defined in these patient populations? 2. Compared with spinal fusion using ICBG or alternative bone graft substitutes, what is the evidence of efficacy and effectiveness of: • rhBMP-2 (InFUSE) for on-label lumbosacral spine fusion in patients with DDD? • rhBMP-7 (OP-1) for on-label revision posterolateral lumbar spine fusion in compromised (e.g., osteoporosis, smoking, diabetes) patients? • rhBMP-2 (InFUSE) for off-label lumbosacral spine fusion? • rhBMP-7 (OP-1) for off-label lumbosacral spine fusion? • rhBMP-2 (InFUSE) for off-label cervical spine fusion? • rhBMP-7 (OP-1) for off-label cervical spine fusion? Including consideration of perioperative outcomes (including length of surgery) as well as short term and long term: • impact on function, pain, radiographic fusion, patient satisfaction, quality of life, activities of daily living and return to work • other reported measures. 3. What is the evidence of the safety of on- or off-label use of rhBMP-2 or rhBMP-7 for spinal fusion compared with spinal fusion using ICB alternative bone graft substitutes? Including consideration of: • Short- and long term adverse events and complications type and frequency (pain, donor site morbidity, resorption/osteolysis, heterotopic bone formation, graft subsidence, graft migration, dysphagia or respiratory difficulties, elevated antibody responses BMPs or collagen, wound complications (infection, hematoma, seroma, or dehiscence), local or systemic toxicity, mispositioned graft, neurological complications, retrograde ejaculation, urogenital complications, allergic reactions, mortality, other major morbidity. • Revision/re-operation rates 4. What is the evidence that on- or off-label use of rhBMP-2 or rhBMP-7 for spinal fusion compared with spinal fusion using ICBG or alternate graft substitutes has differential efficacy or populations? • Gender • Age • Baseline functional or pain status • Comorbidities (including but not limited to tobacco use, alcohol use, psychological or psychological) • Other patient characteristics or evidence-based patient criteria • Provider type, setting or other provider characteristics • Payor/beneficiary type: including worker’s compensation, Medicaid, state employees 5. What evidence of cost implications and cost-effectiveness of on- or off-label use of rhBMP-2 or rhBMP-7 exists? Including consideration of: • Costs (direct and indirect) and cost effectiveness • Short term and long term Title: Coronary Artery Calcium Scoring (CACS) as a Diagnostic Test for Detection of Coronary Artery Disease (September 4, 2009) Investigators: Andrea C. Skelly, PhD, MPH Erika D. Ecker, BS Nora B. Henrikson, PhD, MPH Carin M. Olson, MD, MS Annie L. Raich, MS, MPH Ellen M. Van Alstyne, MS Joseph R. Dettori, PhD, MPH Biostatistics assistance from Margaret S. Pepe, PhD, MS Daryl Morris, MS Key questions addressed: Cardiac calcium scoring uses a CT to check for the buildup of calcium in plaque on the coronary arteries. When used to diagnose persons with suspected coronary artery disease (CAD): 1. What are the test characteristics, PPV (positive predictive value), NPV (negative predictive value), sensitivity and specificity, or coronary artery calcium scoring (CACS) compared with the reference standard of coronary angiography for the diagnosis of CAD or other established diagnostic tests for CAD. What is the evidence to describe the reliability (i.e., test-retest, intra-reader, inter-reader performance) of CACS compared with the evidence about the reference standard or other diagnostic tests for CAD? 2. What is the safety of CACS? 3. What is the evidence that CACS influences clinical decision making and improves patient clinical outcomes (e.g. mortality)? 4. What is the evidence that CACS may perform differently in special populations (e.g. women, diabetic populations)? 5. What evidence of cost implications and cost-effectiveness for CACS compared with other diagnostic tests? Title: Effectiveness of Upright MRI for Evaluation of Patients with Suspected Spinal or Extra-spinal Joint Dysfunction (May 11, 2007) Investigators: Andrea C. Skelly, MPH, PhD Elya Moore, MS, PhD Joseph R. Dettori, MPH, PhD Key questions addressed: Each of the key questions was addressed with respect to the following abnormalities/conditions: Suspected degenerative spondylolisthesis (>25% slip) Suspected spinal stenosis (moderate/severe central stenosis (>1/3 canal), lateral recess stenosis (displacing or compressing nerve root, disc extrusion) Radicular pain (moderate /severe central stenosis, lateral recess stenosis, nerve root compression, disc extrusion) Non-specific spine pain (moderate/severe central stenosis, lateral recess stenosis, nerve root compression, disc extrusion) Extra-spinal joint pain/function loss (e.g narrowing, musculoskeletal only) 1. What is the evidence to describe the concordance (i.e., ability to detect clinically important findings associated with known conditions) of upright MRI compared with currently available diagnostic testing (e.g., standard MRI +/- loading, CT myelogram+/- upright, plain films [flexion and extension], discography, operative findings) in patients (including appropriate sub-populations) with conditions 1-5 above. If a reference standard is available for any of these conditions, what are the test characteristics, PPV (positive predictive value), NPV (negative predictive value), sensitivity and specificity, of upright MRI compared with standard diagnostic testing? 2. What is the evidence to describe the reliability (i.e., test-retest, intra-reader, interreader performance) of upright MRI and how does this reliability compare with available diagnostic testing in patients with 1-5? 3. What is the evidence to describe the diagnostic impact (i.e., effect on additional diagnostic testing, effect on limiting the differential diagnosis) of upright MRI compared with available diagnosis testing in patients with conditions 1-5? 4. What is the evidence to describe the therapeutic and patient impact (i.e., effect on treatments received, efficiency of moving from diagnostic testing to treatment, outcomes [pain, function, adverse events] of test-directed treatment [operative and non-operative]) of upright MRI compared with available diagnostic testing in patients with conditions 1-5, (e.g., what is the likelihood that positive upright MRI findings accurately predicts favorable outcome following test-directed treatment?) 5. What is the evidence that upright MRI in the acute setting is more effective (diagnostic and therapeutic impact) than available diagnostic testing in the subacute/delayed setting in patients with conditions 1-5?