Implementing Care Planning at Nottingham Renal and Transplant Unit
advertisement
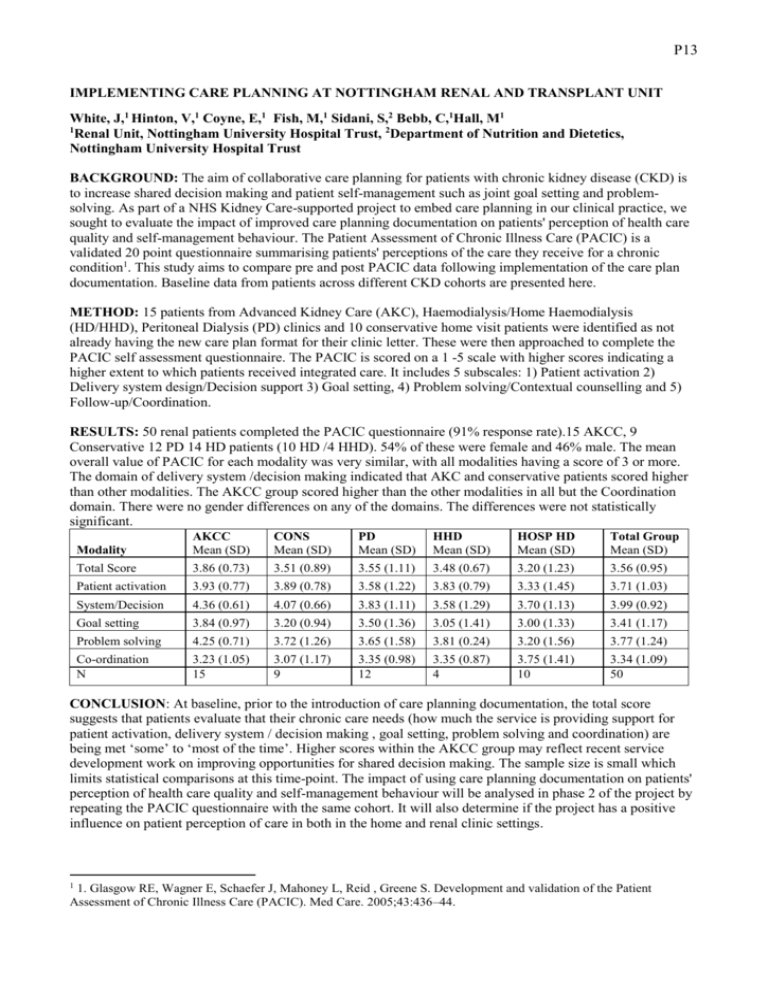
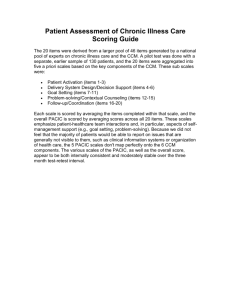
P13 IMPLEMENTING CARE PLANNING AT NOTTINGHAM RENAL AND TRANSPLANT UNIT White, J,1 Hinton, V,1 Coyne, E,1 Fish, M,1 Sidani, S,2 Bebb, C,1Hall, M1 1 Renal Unit, Nottingham University Hospital Trust, 2Department of Nutrition and Dietetics, Nottingham University Hospital Trust BACKGROUND: The aim of collaborative care planning for patients with chronic kidney disease (CKD) is to increase shared decision making and patient self-management such as joint goal setting and problemsolving. As part of a NHS Kidney Care-supported project to embed care planning in our clinical practice, we sought to evaluate the impact of improved care planning documentation on patients' perception of health care quality and self-management behaviour. The Patient Assessment of Chronic Illness Care (PACIC) is a validated 20 point questionnaire summarising patients' perceptions of the care they receive for a chronic condition1. This study aims to compare pre and post PACIC data following implementation of the care plan documentation. Baseline data from patients across different CKD cohorts are presented here. METHOD: 15 patients from Advanced Kidney Care (AKC), Haemodialysis/Home Haemodialysis (HD/HHD), Peritoneal Dialysis (PD) clinics and 10 conservative home visit patients were identified as not already having the new care plan format for their clinic letter. These were then approached to complete the PACIC self assessment questionnaire. The PACIC is scored on a 1 -5 scale with higher scores indicating a higher extent to which patients received integrated care. It includes 5 subscales: 1) Patient activation 2) Delivery system design/Decision support 3) Goal setting, 4) Problem solving/Contextual counselling and 5) Follow-up/Coordination. RESULTS: 50 renal patients completed the PACIC questionnaire (91% response rate).15 AKCC, 9 Conservative 12 PD 14 HD patients (10 HD /4 HHD). 54% of these were female and 46% male. The mean overall value of PACIC for each modality was very similar, with all modalities having a score of 3 or more. The domain of delivery system /decision making indicated that AKC and conservative patients scored higher than other modalities. The AKCC group scored higher than the other modalities in all but the Coordination domain. There were no gender differences on any of the domains. The differences were not statistically significant. Modality AKCC Mean (SD) CONS Mean (SD) PD Mean (SD) HHD Mean (SD) HOSP HD Mean (SD) Total Group Mean (SD) Total Score 3.86 (0.73) 3.51 (0.89) 3.55 (1.11) 3.48 (0.67) 3.20 (1.23) 3.56 (0.95) Patient activation 3.93 (0.77) 3.89 (0.78) 3.58 (1.22) 3.83 (0.79) 3.33 (1.45) 3.71 (1.03) System/Decision 4.36 (0.61) 4.07 (0.66) 3.83 (1.11) 3.58 (1.29) 3.70 (1.13) 3.99 (0.92) Goal setting 3.84 (0.97) 3.20 (0.94) 3.50 (1.36) 3.05 (1.41) 3.00 (1.33) 3.41 (1.17) Problem solving 4.25 (0.71) 3.72 (1.26) 3.65 (1.58) 3.81 (0.24) 3.20 (1.56) 3.77 (1.24) Co-ordination N 3.23 (1.05) 15 3.07 (1.17) 9 3.35 (0.98) 12 3.35 (0.87) 4 3.75 (1.41) 10 3.34 (1.09) 50 CONCLUSION: At baseline, prior to the introduction of care planning documentation, the total score suggests that patients evaluate that their chronic care needs (how much the service is providing support for patient activation, delivery system / decision making , goal setting, problem solving and coordination) are being met ‘some’ to ‘most of the time’. Higher scores within the AKCC group may reflect recent service development work on improving opportunities for shared decision making. The sample size is small which limits statistical comparisons at this time-point. The impact of using care planning documentation on patients' perception of health care quality and self-management behaviour will be analysed in phase 2 of the project by repeating the PACIC questionnaire with the same cohort. It will also determine if the project has a positive influence on patient perception of care in both in the home and renal clinic settings. 1 1. Glasgow RE, Wagner E, Schaefer J, Mahoney L, Reid , Greene S. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Med Care. 2005;43:436–44.