COTM0115 - California Tumor Tissue Registry
advertisement

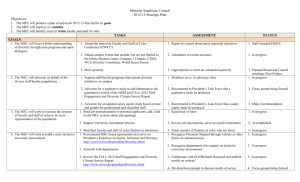
“A 13 y/o Boy with a Posterior Maxillary Nodule” California Tumor Tissue Registry’s Case of the Month CTTR COTM Vol. 17:4 January, 2015 www.cttr.org A 13year-old boy presented with a left posterior maxillary nodule which had developed over a two year period. The excised 2 x 2 x 1.5 cm oval, lobular nodule had a dark-red to pink-gray cut surface. Microscopically, it consisted of polygonal cells with eccentric nuclei and clear or mucincontaining cytoplasm that were admixed with nests of cells with eosinophilic cytoplasm, intercellular bridges and basal cells (Figs. 1 and 2). Pools of extracellular mucin were also seen. The cells failed to show mitotic figures and had only minimal nuclear atypia (Fig. 3). The nodule involved maxillary bone (Fig. 4). Diagnosis: Central/intraosseous Mucoepidermoid Carcinoma of Maxilla Tae Hun Kim, MSIV and Donald R. Chase, M.D. Department of Pathology and Human Anatomy, Loma Linda University Medical Center, Loma Linda, California California Tumor Tissue Registry, Loma Linda, California Mucoepidermoid carcinoma (MEC) is the most common malignant salivary gland tumor. It occurs in both minor and major salivary glands with a predominance in the latter, especially the parotid gland. MEC can rarely occur in sites that are normally devoid of salivary gland tissue, e.g. the mandible and maxilla. The term central or intraosseous MEC is utilized for these cases. Central MEC is a rare tumor with an estimated incidence rate of 2-4% of all MEC. Like traditional MEC, central MEC affects females more than men. It is more common in the molar regions of the mandible than the maxilla. The clinical presentation varies from asymptomatic individuals with an incidental nodule on radiologic evaluation to symptomatic individuals with swelling, pain, facial asymmetry, or trismus. Radiology usually demonstrates a well-circumscribed unilocular/multilocular radiolucent nodule with evidence of bony destruction. The exact origin of central MEC is unknown. Some authors proposed that it originates from ectopic salivary gland tissue, while others thought that it develops from existing odontogenic cysts. The latter theory is favored because metaplastic cells have been seen CTTR’s COTM January, 2015 Page 1 in odontogenic lesions. Half of central MEC are associated with cyst(s) or unerupted tooth, and other neoplasms have been shown the develop from odontogenic cysts. Histologically, central MEC is similar to that of low-grade MEC. It consists of mucous, epidermoid, and basal cells invading in nests and solid sheets. Pleomorphism is absent or minimal. Immunohistochemically, central MEC are positive for keratin (CK7 and CK14) and mucin markers (MUC1, MUC2, MUC4, MUC5AC, and MUC5B). Central MEC can also demonstrate the MAML2 gene rearrangement. Accepted criteria for the diagnosis of central MEC includes: Presence of intact cortical plates Radiologic evidence of bony destruction Exclusion of another primary tumor Histopathological confirmation Detectable intracellular mucin Brookstone and Huvos proposed a staging system for central MEC: Stage I – Intact cortical bone without clinical bony expansion Stage II – Intact cortical bone with clinical bony expansion Stage III – Cortical bone perforation, breakdown of overlying periosteum, or nodal spread The differential diagnosis includes: Glandular odontogenic cysts – Locally aggressive developmental cyst that occurs mostly in the mandible with an anterior predilection; cyst lined by stratified squamous epithelium, cuboidal, or columnar ciliated cells. Small microcysts and clusters of mucous cells can also be present. Because of its histologic similarity with central MEC, invasive growth, negative immunohistochemical staining of Maspin (expressed in MEC), and genetic abnormality are helpful in distinguishing these entities. Keratocystic odontogenic tumor – Parakeratinized stratified squamous epithelium with uniform thickness. No mucous cells are present. Adenosquamous carcinoma – Central MEC does not have anaplastic nuclear features or squamous cell carcinoma in-situ. Metastatic lesions to mandible/maxilla – Presence of primary tumor elsewhere in body Central MEC may be treated by either conservative or aggressive surgical resection. Recurrence rates are up to 40% and 13% for conservative and aggressive resections, respectively. Less than 10% of central MEC cases present with metastatic disease. CTTR’s COTM January, 2015 Page 2 Suggested Reading: Brookstone MS, Huvos AG. Central salivary gland tumors of the maxilla and mandible: a clinicopathologic study of 11 cases with an analysis of the literature. J Oral Maxillofac Surg. 1992; 50:229-36. Moghadam SA, Moghadam FA. Intraosseous mucoepidermoid carcinoma: Report of Two Cases. J Dent. 2014; 15(2): 86-90. Rosai J. Rosai and Ackerman’s Surgical Pathology, 10th ed. Edinburgh, Mosby, 2011; 831-832. Spoorthi BR, Rao RS, Rajashekaraiah PB, Patil S, Venktesaiah SS, Purushothama P. Predominantly cystic central mucoepidermoid carcinoma developing from a previously diagnosed dentigerous cyst: case report and review of the literature. Clin Pract. 2013 Jun 20;3(2)e19. Wenig B. Atlas of Head and Neck Pathology, 2nd ed: Philadelphia, Saunders/Elsevier, 2008; 615622. CTTR’s COTM January, 2015 Page 3