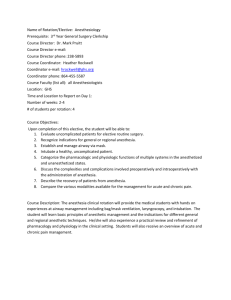
General Anesthesia (2)
advertisement

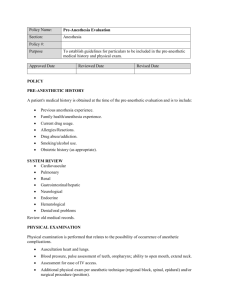
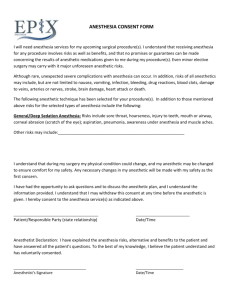
1 Florida Heart CPR* Anesthesia, General 2 hours GENERAL CONSIDERATIONS Anesthesia is the process by which a patient is rendered able to undergo surgery. Surgery was, of course, commonly performed before any means was available to spare the patient any part of the experience. It takes little imagination to realize that an unanesthetized person enduring a surgical wound will exhibit several things including the following: Evasive action Severe pain and emotional distress Maximum tension in skeletal muscles Massive increase in sympathetic tone causing sweating, tachycardia, and hypertension Vivid and unpleasant memory of the event forever The goals of anesthesia thus include the following: Anesthesia (lack of awareness of surrounding events) Akinesia (keeping the patient still to allow surgery to take place) Muscle relaxation (to enable access through muscles to bones and body cavities) Autonomic control (to prevent dangerous surges in hemodynamics) General anesthesia General anesthesia uses drugs given systemically to render the patient unaware of anything that is being done to or around him or her. It must be safe, not threatening or unpleasant to the patient, allow adequate surgical access to the operative site, and cause as little disturbance as possible to internal homeostatic mechanisms. A point worth noting is that general, as opposed to local or regional anesthesia, may not always be the best choice. The optimal technique for any given patient and procedure is selected by the anesthesiologist based on the following criteria: Advantages Makes no psychological demand of the patient Allows complete stillness for prolonged periods of time Facilitates complete control of the airway, breathing, and circulation Permits surgery to take place in widely separated areas of the body at the same time Florida Heart CPR* General Anesthesia 2 Can be used in cases of sensitivity to local anesthetic agent Can be administered without moving the patient from the supine position Can be adapted easily to procedures of unpredictable duration or extent Usually can be administered rapidly Disadvantages Requires the involvement of an extra set of healthcare providers Requires complex and costly machinery Requires some degree of preoperative patient preparation Usually associated with some degree of physiological trespass Carries the risk of major complications including death, myocardial infarction, and stroke Associated with less serious complications such as nausea/ vomiting, sore throat, headache, shivering, and delayed return to normal mental functioning Associated with malignant hyperthermia, a rare, inherited muscular condition in which exposure to some (but not all) general anesthetic agents results in acute and potentially lethal temperature rise, hypercarbia, metabolic acidosis and hyperkalemia A given patient’s risk for complications as a direct result of general anesthesia depends largely on his or her medical co-morbidities but is small. Anesthetic death rates of 1 per 10,000 generally are quoted, but most anesthesiologists believe that current advances in anesthesia monitoring such as pulse oximetry and capnography have made massive contributions to patient safety. Furthermore, it is an average figure incorporating both elective and emergency patients of all types of physical conditions. Minor complications occur at predicable rates even in previously healthy patients. The incidence of symptoms during the first 24 hours following ambulatory surgery is: <5% bleeding, vomiting, nausea; fever 5-15%; dizziness, headache, drowsiness, hoarseness >15%; sore throat (25%); and incisional pain (30%). PREPARATION FOR GENERAL ANESTHESIA Safe and efficient anesthesia practice requires certified personnel, appropriate drugs and equipment, and an optimized patient. These requirements need to be adapted to the context; no one would criticize a trauma surgeon attending a patient trapped in the wreckage of a motor vehicle accident for administering a bolus dose of intravenous (IV) ketamine at the roadside to amputate a limb and free the victim. Such a general anesthetic, given in an uncontrolled fashion by an individual with no anesthesia training, would be completely inappropriate for an elective surgical procedure. Florida Heart CPR* General Anesthesia 3 Minimum requirements Minimum infrastructure requirements for general anesthesia include a well-lit space of adequate size, a source of pressurized oxygen (either piped in or from cylinders) an effective suction device, and equipment to continuously monitor heart rate and rhythm, blood pressure, oxygen saturation, and temperature. Additional monitoring requirements exist in certain jurisdictions. Beyond this, some equipment is needed to deliver the anesthetic agent. This may be as simple as needles and syringes if the drugs are to be given entirely IV, but in most circumstances this means the availability of a properly serviced and maintained anesthetic gas delivery machine. An array of routine and emergency drugs, including supplies of Dantrolene sodium (the specific treatment for malignant hyperthermia), airway management equipment, a cardiac defibrillator, and a recovery room staffed by properly trained individuals completes the picture. Preparing the patient The patient should be adequately prepared. The most efficient method is for the patient to be reviewed by the person responsible for giving the anesthetic well in advance of the surgery date. Persons without concomitant medical problems may need little more than a quick medical review and the opportunity to discuss anesthetic questions or concerns. Those with co-morbidity in general should be optimized for the procedure. Patients with diabetes, coronary artery disease, chronic bronchitis and emphysema, and other chronic aliments should be stable. The question of whether such a diseased state is under optimal control is usually a simple matter of good clinical judgment and can be determined by anyone who asks the appropriate questions. There are a few areas where anesthesiology review can predict and prevent major adverse events. Foremost amongst these is a careful examination of the patient's airway anatomy. Identification of one or more of these anomalies may indicate that management of the patient's airway might prove difficult under anesthesia. Airway management Possible or definite difficulties with airway management include the following: Small or receding jaw Prominent maxillary teeth Short neck Limited neck extension Poor dentition Florida Heart CPR* General Anesthesia 4 Tumors of the face, mouth, neck, or throat Facial trauma Interdental fixation Hard cervical collar Halo traction Various scoring systems have been created using orofacial measurements to predict difficult intubation. The most widely used is the Mallampati score, which identifies patients in whom the pharynx is not well visualized through the open mouth. High Mallampati scores predict difficult intubation with good but not perfect accuracy. Often, such histories describe factors such as prolonged postoperative vomiting or slow emergence, which, while important, do not cause undue concern for the patient at hand. Of much greater concern is a history of high temperature under anesthesia or any form of anesthesia complication that resulted in death or the necessity for intensive care. It may be necessary to obtain records from other institutions when suspicion of an adverse event is high but it is deemed necessary to plan a similar anesthetic technique again. Other requirements The necessity to come to the operating room with an empty stomach is well known to health professionals and the lay public alike. While aspiration of food or fluids into the lungs during anesthesia is a serious complication, do not forget that depriving the patient of fluid is not benign, particularly in the case of small children, thus strike a reasonable balance between safe anesthetic care and dehydration. Most anesthetists would agree that solid food should be avoided for 6 hours and clear fluids for up to 4 hours prior to the induction of anesthesia. With a few exceptions, patients should continue to take regularly scheduled medications up to and including the morning of surgery. There are obvious exceptions, including the following: Discontinue anticoagulants, including aspirin, in good time to avoid increased surgical bleeding. Avoid oral hypoglycemics on the day of surgery and manage blood glucose using IV dextrose and insulin. Metformin is an oral hypoglycemic agent that is associated with the development of profound and occasionally irreversible metabolic acidosis under general anesthesia. Discontinue it 2 weeks prior to the surgery date. Since monoamine oxidase inhibitors are associated with anesthetic drug interactions, discontinue them prior to surgery if possible. Florida Heart CPR* General Anesthesia 5 The extent of laboratory testing for the presurgical patient is the subject of ongoing debate within the anesthesia community. Previous regimens demanding standard blood-work profiles, ECGs, and chest radiographs on all surgical patients are now believed to be unnecessarily elaborate by most anesthesia professionals. The most efficient route is to have the anesthetist order his or her own tests. THE PROCESS OF ANESTHESIA Premedication: The first stage of a general anesthetic This stage, which is usually conducted in the surgical ward or in a preoperative holding area, is something of a throwback to the early days of ether and chloroform anesthesia when drugs such as morphine and scopolamine routinely were given to make the inhalation of these highly pungent vapors more tolerable. The goal of this stage of the anesthesia process is to have the patient arrive in the operating room in a calm, relaxed frame of mind while causing minimal interference with breathing and cardiovascular status. For many patients, this step is either unnecessary or impractical because of the way in which patients are scheduled. Appropriate drug choices are morphine, lorazepam, diazepam, temazepam, and others. In anticipation of surgical pain, preemptive analgesics such as indomethacin or acetaminophen can be used. Where appropriate facilities are available, an excellent alternative is small doses of fentanyl and midazolam to be titrated IV by a nurse in the preoperative holding area. Drying agents occasionally are used to diminish oral secretions, but this is perhaps less of an issue than it once was. The patient is transferred to the operating table and baseline vital signs are obtained. Induction: The patient is ready for this stage, usually the most critical part of the anesthesia process. In many ways, induction of general anesthesia is analogous to an airplane taking off. It is the transformation of a waking patient into an anesthetized one. This can be achieved by IV injection of induction agents (drugs such as thiopental and propofol that work rapidly), by the slower inhalation of anesthetic vapors from a face mask, or a combination of both. For the most part, contemporary practice dictates that adult patients and most children be induced with IV drugs; inhaled inductions are reserved for uncooperative toddlers and special circumstances in adults. In addition to the induction drug, most patients receive an injection of narcotic analgesic. A wide range of synthetic and naturally occurring narcotics with different properties is available. Induction agents and narcotics work synergistically to put the patient to sleep. In addition, events that are about to occur, such as endotracheal intubation and incision of the skin, generally raise Florida Heart CPR* General Anesthesia 6 the blood pressure and heart rate. Narcotic helps preempt this undesirable response. The next step of the induction process is the securing of the airway. This may be a simple matter of manually holding the patient's jaw such that his or her natural breathing is unimpeded by the tongue or may demand the insertion of a prosthetic airway device such as a laryngeal mask airway or endotracheal tube. A variety of factors are considered when making this decision. The major issue is whether the patient requires an endotracheal tube. Indications for endotracheal intubation under general anesthesia include the following: o Potential for airway contamination (full stomach, gastroesophageal [GE] reflux, gastrointestinal [GI] or pharyngeal bleeding) o Surgical need for muscle relaxation o Predictable difficulty with endotracheal intubation or where anesthetist's access to the airway during the case will be difficult (lateral or prone position) o Surgery of the mouth or face o Prolonged procedure anticipated Not all surgery requires muscle relaxation. In this context, only the major muscle groups of the thorax and abdomen are considered. If surgery is taking place in these areas, then in addition to the induction agent and narcotic, an intermediate or long-acting muscle relaxant drug is given. This paralyzes muscles indiscriminately, including the muscles of breathing. Therefore, the patient's lungs must be ventilated under pressure, necessitating an endotracheal tube. Persons who for anatomic reasons are likely to be difficult to intubate are usually intubated electively at the beginning of the case. This prevents the situation where attempts are made to manage the airway with a lesser device, only for the anesthetist to discover that oxygenation and ventilation are inadequate. At that point during a surgical procedure it can be extraordinarily difficult, if not impossible, to intubate the patient quickly. Maintenance phase: At this point, the drugs used to initiate the anesthetic are beginning to wear off, and the patient must be kept anesthetized using a maintenance agent. For the most part, this refers to the delivery of anesthetic gases (more properly termed vapors) into the patient's lungs. These may be inhaled as the patient breathes himself or delivered under pressure by each mechanical breath of a ventilator. The maintenance phase is usually the most stable part of the anesthesia. However, it is important to understand that anesthesia is a continuum of different depths. A level of anesthesia that is satisfactory for surgery to the skin of an extremity, for example, would be inadequate for manipulation of the bowel. Appropriate levels of anesthesia must be chosen both for the planned procedure and for its various stages. In complex plastic surgery for example, a considerable Florida Heart CPR* General Anesthesia 7 period of time may elapse between the time that the induction of anesthetic is complete and the skin is incised. o During the period of skin preparation, urinary catheter insertion, and marking out incision lines with a pen, the patient should not be receiving any noxious stimulus. This requires a very light level of anesthesia, which must be converted rapidly to a deeper level just before the incision is made. As the case progresses, the level of anesthesia is altered to give the minimum amount necessary to ensure adequate anesthetic depth. This is achieved more through art than science. o If muscle relaxants have not been used, inadequate anesthesia is easy to spot. The patient will move, cough, or pupillary obstruct his airway if the anesthetic is too light for the stimulus being given. o If muscle relaxants have been used, then clearly the patient is unable to demonstrate any of these phenomena. In these patients, the anesthesiologist must rely on careful observation of autonomic phenomena such as hypertension, tachycardia, sweating, and capillary dilation to decide that the patient requires a deeper anesthetic. o This requires experience and judgment. It is from failure to recognize such signs that tragic and highly publicized cases of awareness under anesthesia are caused. o Excessive anesthetic depth, on the other hand, is associated with decreased heart rate and blood pressure, and, if carried to extremes, can jeopardize perfusion of vital organs or be fatal. Short of these serious misadventures, excessive depth results in slower awakening and more side effects. As the surgical procedure draws to a close, the patient's emergence from anesthesia is planned. Experience and close communication with the surgeon enable the anesthesiologist to predict the time at which the application of dressings and casts will be complete. o In advance of that time, anesthetic vapors have been decreased or even switched off entirely to allow time for them to be excreted by the lungs. o Excess muscle relaxation is reversed using specific drugs and adequate long-acting narcotic analgesic to keep the patient comfortable in the recovery room. o If a ventilator has been used, the patient is restored to breathing by himself and as anesthetic drugs dissipate, the patient wakes up. o Waking up is not synonymous with removal of the endotracheal tube or other artificial airway device. This is only performed when the patient has regained sufficient control of his or her airway reflexes. ANESTHESIA DRUGS IN COMMON USE There are a number of choices for every aspect of anesthetic care and the way in which Florida Heart CPR* General Anesthesia 8 they are sequenced probably depends more on the personal preference of the person administering them. Induction agents For 50 years, the most commonly used induction agents were rapidly acting, water-soluble barbiturates such as thiopental, methohexital, and thiamylal. These drugs are still commonly in use today, have an enormous record of safety and reliability, and also are economical. More recently, propofol, a nonbarbiturate intravenous anesthetic, has displaced barbiturates in many anesthesia practices. o The use of propofol is associated with less postoperative nausea and vomiting and a more rapid, clear-headed recovery. o In addition to being an excellent induction agent, it can be given by slow IV infusion instead of vapor to maintain the anesthesia. o Among its disadvantages are the facts that it often causes pain on injection, and it is prepared in a lipid emulsion, which if not handled using meticulous aseptic precautions, can be a medium for rapid bacterial growth. Anesthesia also can be induced by inhalation of a vapor. This is a common and useful technique in uncooperative children and in some special circumstances. Halothane and Sevoflurane are the most commonly used drugs for this purpose. Traditional narcotic analgesics Morphine, meperidine, and hydromorphone are widely used in anesthesia as well as in emergency rooms, surgical wards, and obstetric suites. In addition, anesthesia providers have at their disposal a range of synthetic narcotics, which in general cause less fluctuation in blood pressure and are shorter acting. These include fentanyl, sufentanil, alfentanil, and remifentanil. Remifentanil is the newest drug in this class and has such a short duration of action that it must be given as a continuous infusion. Muscle relaxants come in many varieties Succinylcholine, a rapid-onset, short-acting depolarizing muscle relaxant, is the drug of choice when rapid muscle relaxation is needed. o For decades, anesthetist have used it extensively despite a number of predictable and unpredictable adverse effects associated with its use. o The search for a drug that replicates its onset and offsets speed without its adverse effects is the holy grail of muscle relaxant research. Other relaxants have durations of action ranging from 15 minutes to more than 2 hours. Older drugs in this class were often associated with changes in heart rate or blood pressure, but the newer ones are devoid of these adverse properties. Florida Heart CPR* General Anesthesia 9 Muscle relaxants generally are excreted by the kidney, but some preparations are broken down by plasma enzymes and can be used safely in partial or complete renal failure. Pancuronium is an established drug that is still in widespread use because of its low cost and familiarity, especially in intensive care units; rocuronium, mivacurium, and cisatracurium are more likely to be used by contemporary anesthesiologists. Anesthetic vapors These are highly potent chlorofluorocarbons, which are delivered from precision vaporizers directly into the patient's inhaled gas stream. They may be mixed with nitrous oxide, a much weaker but nonetheless useful anesthetic gas. The prototype of modern anesthetic vapors is halothane. It has an unparalleled track record of safety and efficacy, although it is associated with rare but devastating hepatic necrosis to a greater extent than other agents. In the 1980s, it was displaced by isoflurane and enflurane, agents that were cleared from the lungs faster and thus were associated with more rapid anesthetic emergences. In the late 1990s, 2 new vapors have become very popular, desflurane and sevoflurane. These drugs are much more maneuverable than their predecessors and are associated with much more rapid emergence. There is intense commercial interest in anesthesia drug research, and it seems inevitable that new and better drug products will be introduced continuously for many years to come. REFERENCES Nash PG, Cullen BF, Stoelting RK (eds.): Clinical Anesthesia. 2nd ed. Philadelphia: JB Lippincott 1992. Chung F: Recovery pattern and home-readiness after ambulatory surgery. Anesth Analg 1995 May; 80(5): 896-902 Davies JM, Pagenkopf D, Todd K: Comparison of selection of preoperative laboratory tests: the computer vs the anaesthetist. Canadian Journal of Anaesthesia 1994; 41: 1156-60 Franks NP, Lieb WR: Molecular and cellular mechanisms of general anaesthesia. Nature 1994 Feb 17; (6464): 607-14 Stack CG, Rogers P, Linter SP: Monoamine oxidase inhibitors and anaesthesia. A review. Br J Anaesth 1988 Feb; (2): 222-7 Florida Heart CPR* General Anesthesia 10 Florida Heart CPR* General Anesthesia Assessment 1. An unanesthetized person enduring a surgical wound will exhibit several things including the following: a. Severe pain and emotional distress b. Maximum tension in skeletal muscles c. Massive increase in sympathetic tone causing sweating, tachycardia, and hypertension d. All of the above 2. The goals of anesthesia include: a. Akinesia b. Muscle relaxation c. Autonomic control d. All of the above 3. Anesthetic death rates of ____ generally are quoted, but most anesthesiologists believe that current advances in anesthesia monitoring such as pulse oximetry and capnography have made massive contributions to patient safety. a. 1 per 100 b. 1 per 10,000 c. 1 per 500 d. 1 per 5,000 4. Safe and efficient anesthesia practice requires: a. certified personnel b. appropriate drugs and equipment c. optimized patient d. all of the above 5. Possible or definite difficulties with airway management include the following: a. Facial trauma b. Poor detention c. Hard cervical collar d. All of the above 6. Most anesthetists would agree that solid food should be avoided for __ hours and clear fluids for up to __ hours prior to the induction of anesthesia. a. 6 hours/ 4 hours b. 12 hours/12 hours c. 12 hours/ 24 hours d. 6 hours /10 hours Florida Heart CPR* General Anesthesia 11 7. With a few exceptions, patients should continue to take _____up to and including the morning of surgery. a. Vitamins b. Regularly scheduled medications c. Aspirin d. Water 8. In many ways, induction of general anesthesia is analogous to an airplane taking off. It is the transformation of a waking patient into an anesthetized one. a. Falling asleep b. An airplane taking off c. An airplane landing d. None of the above 9. At this point, the drugs used to initiate the anesthetic are beginning to wear off, and the patient must be kept anesthetized using a maintenance agent. a. Induction b. Maintenance phase c. Premedication phase d. Latent phase 10. Anesthesia also can be induced by_____. This is a common and useful technique in uncooperative children and in some special circumstances. Halothane and Sevoflurane are the most commonly used drugs for this purpose. a. Mouth b. Inhalation of a vapor c. IV d. Injection Florida Heart CPR* General Anesthesia