Child circumcision in the UK: A review of incidence and
advertisement

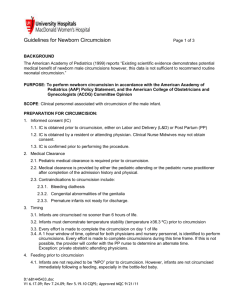
Child circumcision in the UK: A review of incidence and harms Laura MacDonald Summary A national survey of male circumcision incidence and harms has been undertaken by a member of the public, using the Freedom of Information Act 2000. The study – the first of its kind to be publishedcollates important data from NHS non-therapeutic child circumcision schemes including the cost and incidence of early and medium term adverse events. It also collates data on therapeutically-coded child circumcision in English hospitals, and on morbidity and mortality relating to the wider child circumcision marketplace. The survey reveals a disturbing gap between circumcision reality and rhetoric. Child circumcision harm is widespread, and serious harm may particularly affect those assumed to be the safest target: infants. Yet from thousands of A&E / GP follow ups, to hundreds of revision surgeries, to the deaths (4-5 recorded as linked to circumcision in 65 months), these impacts are going unreported. The lucrative private circumcision sector is minimally regulated and evidences some dangerous and dishonest practice; even some NHS mass circumcision schemes, which headlined quality assurance, fail to enforce service level agreements and breach guidelines on consent. Long term monitoring of male circumcision impact is absent, and there is no evidence of due diligence into the risk of future litigation or even the cost to the NHS of future treatments for urinary, psychological or sexual issues. Meanwhile, therapeutically-coded child circumcision is still significantly over-referred, bringing unnecessary costs in terms of both surgeries and treatment of complications. The health of children may not be traded for an illusion of cultural sensitivity nor to maintain a belief in medical infallibility. With non-therapeutic or dubiously-therapeutic circumcision affecting around 40,000 boys each year, it is time for a comprehensive national audit into the incidence and impact of this surgery. Only then can a full national debate begin. Background In the early 1990s against the background of the death of Boma Oruitemeka and reports of life threatening harms affecting over 100 boys per annum in Englandi, there were increasing calls for the NHS to offer non-therapeutic child circumcision (NTCC) as a safety measure. The issues highlighted include septicaemia, urinary tract infection, penile degloving, urethral fistula, embedded plastibell, haemorrhage requiring surgery and/or transfusion, lymphaditis, meningitis, osteomyelitis, septic arthritis, and bilateral femoral head necrosis; the patients included both neonates and older children ii iii iv . Page 1 of 18 In 1996 the first NHS scheme providing NTCC under local anaesthetic was launched, provided at cost v. Other schemes offering infant NTCC under local anaesthetic have followed, in a variety of settings, some with full fundingvi. Incidence of NTC (adults and children) as inpatient surgery has also grown: in the ten financial years to March 2010, NHS hospital episode statistics (HES) reports that there were 15,288 inpatient spells coded Z41.2 (routine or ritual male circumcision) in the age group 0-14, with 1,153 inpatient spells for routine circumcision in older teens and adults. If an average tariff of £500 is assumed over the years 2000-2010, £7.6 million in NHS funds was spent on NTC of under 15s in this period; and around £576,500 on the NTC of older males. All this activity - which adding inpatient and local clinic NT circumcisions may amount to 30,000 surgeries - was undertaken rather quietly, with Department for Health guidelines continuing to state that NTC should not be funded in the NHS. In England the rate of hospital performed NTC peaked in the financial year ending March 2009 with 1,854 operations on children and 142 on adults. By the financial year ending March 2012, as financial austerity measures took hold, the rate of inpatient NTC had dropped to 949 in children and 45 in adults. Directly comparable NTC incidence for Scotland has not been collected, however a scheme launched in October 2007 undertakes inpatient NTCC on infants aged 6-9 months across 4 regional centresvii: in the first 18 months of this scheme it circumcised 820 childrenviii. NHS Scotland has also advised that in the period April 2001-March 2008, it funded a total of 3,112 non therapeutic circumcisionsix so operations apparently funded on a case by case basis prior to the formal scheme. Assuming again an individual cost of around £500, and that child NTCC continued at an incidence of around 550 per annum, NHS Scotland may have spent £2 million on NTCC in the ten years years to March 2010. A further freedom of information request will be made to establish actual costs. Reports of harm have continued x xi xii xiii xiv xv and internationally, challenges to NTCC are growing xvi xvii xviii xix xx xxi . . In the UK, however, discussions about resourcing continue, with evidence emerging that some commissioners may lack awareness of the scale and/or the cost of the NTCC schemes they have been fundingxxii xxiii.. In some areas, rather than fund NTCC, commissioners may signpost to NTCC services which are considered safexxiv xxv xxvi. The debate about NHS controlled or funded NTCC remains strikingly bare of empirical evidence regarding outcomes (although NHS involvement is presented as ensuring quality, while ‘using unaccredited services …may lead to increased health and psychological problems’ xxvii). The development of numerous NTC schemes with different characteristics offered medical authorities the opportunity to undertake a highly powered audit of outcomes in different age groups and with different techniques, training, delivery settings and service level contracts. No such research has been undertaken. Yet this data could have international relevance in the context of increasing promotion of infant NTC. It could evidence the health resource implications of its complications in the short, medium and long term, and importantly it could test the assumption that the earlier NTC is performed the safer it is [xxxv] xxviii (a Page 2 of 18 hypothesis challenged by the facts of neonatal anatomy/vulnerabilities, by the incidence of infant deaths xxix xxx xxxi xxxii, and also by evidence that mass adult NTC has low adverse effectsxxxiii xxxiv). NHS commissioner databases now provide the opportunity to extract detailed information on all NTCs performed and their follow up presentations, operations and treatments over multiple years, with a length of stay and cost attached to each episode: the data available now allows us even to assess the complications of the complications (in terms, for example, of presentations subsequent to corrective surgeries). Absent a national review, but against a background in which contractors of NHS NTCC services have cited significant rates of follow-up treatment xxxv [liv], NHS Choices tells parents that complications of circumcision are ‘rare’. The Medical Protection Society prefers the words ‘considerable’ and ‘common’xxxvi. A US review describes even a subset (late issues) as ‘common’xxxvii. One of those late issues (particularly linked to neonatal NTCCxxxviii) has been evidenced in one in five subjectsxxxix who were thought not to have issues. In the US, where one review suggests that infant circumcision might be responsible for as many as 117 child deaths per annumxl, the American Academy of Paediatrics (AAP) presents the risks as minimal xli in a report European Padiatrician have called culturally biased xlii and scientifically untenable [xx] In the UK, the impacts of limited or conflicting information on harms are increasingly clear; of 4 male circumcision-linked infant deaths known to have occurred between September 2006 and February 2012 (two performed by doctors, and all by experienced circumcisers) the details suggest that a better understanding of risk might have saved the lives of at least three boys. In the latest case, the parents of Goodluck Caubergs, who bled to death in 2010 from his circumcision wound, revealed in court that they did not ‘for one minute’ think that the procedure could cause harmxliii. Approach/methods/timeframe The study undertook to reveal the incidence of child morbidity and mortality in the UK today relating to circumcisions, particularly non therapeutic or dubiously therapeutic child circumcisions, and to compare this to information recorded by commissioners, and available to parents and the public. Data was extracted from hospital and commissioner databases via requests made between 2009 and 2013 under the provisions of the 2000 Freedom of Information Act (FOI). Initially supported by a health charity with an email address, laptop, and gift of data from an earlier, incomplete and unpublished FOI survey, it has been completed entirely independently. There were four main official sources of information: NHS trusts in England, Primary Care Trusts (NHS funders as was), the GMC as regulatory body, and local authority safeguarding teams in some areas of high incidence of circumcision. Limited data was also gathered from the Scottish NHS Information Services Division (ISD) and the Scottish government. Data from these sources was complemented by data and views gathered from a number of Page 3 of 18 other medical and authority sources, including the police, the pathology and coroners services, research and position papers, websites and polemic articles. Involving only one amateur researcher, and correspondence with almost 300 separate health institutions or boards, involving > 2,000 emails and > 500 separate datasets (some available only in pdf), it has been impossible to undertake a comprehensive analysis of all the information collated. Headline information is presented, along with some detailed information on series which by volume may be considered the most significant. All the data released under FOI provisions and accompanying correspondence will be made available to those paediatricians/urologists who have volunteered advice or interest, and also to the Care Quality Commission /another appropriate authority. RESULTS Incidence and cost of NHS funded NTCC Of 144 approached, 36 English PCTs confirmed that they funded one or more NTCCs in 2009. 76 stated they did not fund NTCC in 2009, and 32 provided no response; the zero returns and non-responses include areas where hospital data/other commissioner data suggests NTCs are funded. Of 36 PCTs which funded NTCC, 30 gave both number and cost: these PTCS funded 3,397 NTCCs at a total cost of £1,407,657. 1,519 were performed as inpatient surgeries, representing 45% of the total. In 2009 NTCCs performed under local anaesthetic in primary care or clinic settings ranged in cost from £55£284 (mean £155), and NTCCs performed under general anaesthetic in secondary care cost in the range £500-£1,074 (mean £781).The numbers of NTCCs contracted by PCTs ranged from 1 to 1,068. Eight PCTs across England funded more than 150 NTCCs in 2009; five mainly or only in clinic settings under local anaesthetic, and two only in secondary care under local anaesthetic. The top six commissioned schemes (by volume) were selected for further analysis, particularly the largest, PCT1, which in the seven financial years to March 2012 funded a total of 8,212 NTCCs via GP contractors at a total cost of £757,125. Emergency presentations and admissions post NTC The first attempt to generate data on circumcision harms asked hospital trust to search emergency triage records for the word ‘circumcision’ and reveal those cases (with details to assist in removing irrelevant ones, such as those referencing a need for circumcision). This exercise generated 282 case histories of circumcision issues in A&E in 2009 across 46 trusts (of 127 interrogated). It also generated, from one children’s hospital (which I call H1), an audited series of child presentations in A&E (N=104). This verified data included the breakdown of presenting issues, which demonstrates how crude data on post circumcision presentations may under-represent actual issues: Issue Page 4 of 18 No of patients Bleeding 37 Swelling Dressing 17 15 Dysuria 6 Blister/Spots 5 Discharge Infection 4 4 Soreness 4 Pain 3 Allergic reaction 2 Rash 1 Cough/Pyrexia 1 Diarrhoea + Vomiting/Fever Crying/Decreased oral intake 1 1 Injury Constipation 1 1 Post op complications Not specified 1 TOTAL: 104 Of the above children, 24 (23%) were admitted to ward or held for a period of observation: 14 in total were observed; ten were admitted for treatment. The length of stay was revealed for 9 admissions to ward: it ranged from 1-4 days (mean 2.4 days): these can be assumed to be serious or life threatening cases. Information on the place of circumcision was refused and the surgery denominator cannot be established. However, this hospital operates in a sprawling conurbation in which there were several NTCC schemes. In 2009 the main two commissioners of NTCCs in H1’s catchment area performed 1,424 NTCs following which there were 92 gross episodes of presentation in A&E within 30 days (of which around 75% may be assumed to be relevant). Given this fact, and that 64 children in the series are age 0, it is reasonable to assume that at least half the complications in this audit may reference NHS NTC. Further responses suggest that H1 believes the results are of particular relevance to NTCC commissioners – the hospital revealed (somewhat reluctantly) that the decision to undertake the audit followed from clinical concerns about circumcision care. H1 reports that its concerns were shared with local NHS commissioners, although (as of early 2013) no response had been received. The wider results from this FOI exercise (282 emergency cases presented by 46 trusts) have limited utility: representing not just a subset of English acute trusts (around 1/3) but also even within this, a small subset of post circumcision A&E presentations. The exercise relies on operator choice of language, and even spelling; in some potentially important areas hospital databases were inadequate, proving unable to generate any more than those emergency cases which resulted in admission. Later Page 5 of 18 interrogations which asked trusts to review their own emergency presentations by proven methods (database queries using the unique patient ID as pivot) suggest that even where trusts were able to fully interrogate triage records using the method suggested (free text searching for ‘circumcision’), the results could represent as little as ¼ of actual emergency cases of circumcision harm. Extrapolation of the above issues suggests that total A&E presentations post CC across England, are likely to exceed 2,000 per annum. Across this whole exercise (including H1 and 46 other trusts), 85 (28%) of 303 circumcision related A&E cases with disposal information are described as having resulted in admission or a transfer to another hospital. While the data suggest that overall an infant seen in A&E post may be slightly less likely to be admitted than an older child, it appears to show that where admission in age 0 does occur those issues may be more likely to be drastic and resource intensive. Although a fraction of the national picture ,the cases of admission included three age 0 infants transferred for specialist treatment for circumcision haemorrhage/shock. Incidence of inpatient TC, and readmissions As a complement to the above, and to demonstrate whether too many unnecessary therapeutic circumcisions are being performed (particularly in children)xliv, the 127 trusts interrogated regarding A&E data were also asked to reveal their incidence of circumcision in 2009 and 2011, with breakdown by age group (0-4, 5-9, 10-17, and 18+), and primary diagnosis. Most were also asked to reveal readmissions to hospital within 30/90 days (some others were asked a different secondary question; which followed on from issues identified in the phase 1 research). Across 113 hospital trusts which provided data for 2009 and 2011 overall circumcision declined by 1,589 operations in the period. This decrease is partly accounted for by decreased funding for NTC, however some significant reductions in incidence are also seen in hospitals which may not have funded NTC previously. A declining in incidence of circumcision was seen at 73 trusts; reductions ranged from 2-334, with 23 reporting a total decrease of 50 or more operations. Analysis of this trust grouping shows adult (defined as age 18+) circumcision incidence in the range 0341, and child (defined as 0-17) circumcision incidence ranging from 1-359. Mean incidence of adult circumcision by trust is 104 circumcisions, with 53 trusts performing fewer than this number. Mean incidence of child circumcision by trust is 73 (although this includes a significant number of NTCs). 835 NTCCs are identified across this dataset, and 25 adult NTCs, (although some trusts did not report numbers). 90 hospital trusts (71% of those interrogated) reported both an age breakdown in child circumcisions and an age breakdown of diagnosis; this shows 1,552 TCs in age 0-4 (a mean of 17.2 per trust). 12 trusts in the dataset (13%) performed more than twice this number, while 9 trusts performed 40 or more TCs in age 0-4. This is significant as a BAPS advise that TC is ‘virtually never necessary’ in this age groupxlv. Page 6 of 18 Therapeutic circumcision rates in age 5-9 affects 2,282 boys across the above trust group; incidence is high as 111 in one hospital trust in one year. There is evidence of continuing high level concern about the issue of unnecessary male circumcisons; Royal College of Surgeons draft guidance suggests that doctors in both primary and secondary care institutions need to learn to distinguish rare pathological phimosis from physiological phimosis (i.e. developmental normality) xlvi. One respondent in this study (‘H2’) was found on further research to have undergone investigation by a commissioner 12 years previouslyxlvii, due to ‘disproportionately high’ TCs, particularly in the age 0-4. H2 has since reduced the rate in this age group by around 2/3, but in 2011 it still had the second highest incidence of therapeutic circumcision in under 9s in England, with 145 operations performed. Generalised circumcision admissions It has not been possible to analyse all the data on readmissions post circumcision generated by this survey, and a mistake in requesting ‘returns to urology’ rather than more open readmission parameters initially invalidated some returns. Despite this, good information on readmissions post inpatient surgeries in 26 secondary care institutions has been generated, and analysed. A simple method to find relevant readmissions relating to circumcision is to search for readmission diagnosis codes beginning T81 (complications of a procedure); some hospitals use these diagnoses as default parameters to generate readmission rates, often to 30 days. Readmission data reviewed in this study, which includes the diagnosis for the original surgery, and readmission diagnosis coding up two levels, over a time period of up to 91 days, suggests T81/30 day parameters may not reveal the real incidence of issues likely to be linked to circumcision. Analysis of relevant readmissions (n=100) in 30 day of CC at 26 trusts shows that readmission rates vary significantly (0-15%), with mean incidence of 3.8%. Increasing the time frame to to 90 days post surgery increases the mean relevant readmission rate to 4.3%. Most child circumcision complications occur within two weeks of the operation, and length of stay ranges from a few hours in observation to 4 days in a hospital bed. A small series which includes the cost of each spell of readmission suggests that early CC readmissions may cost an average of £971 per child. Importantly, a detailed analysis of presentations subsequent to surgery at H2 (a hospital with persistent high rates of TCC) revealed the highest rates of follow up presentations in the children least likely to require a TC. H2 revealed both relevant A&E presentations and readmissions in 2009 (N=20), and readmissions in 2011 (N=8). In 2009, 20/239 under 16s subject to TC returned with haemorrhage or infection within 91 days, with half readmitted:an emergency presentation rate of 8.5%, and admission rate of 4.2%. In 2011 relevant readmissions in 30 days of TC occurred in 8 children (4.3%). The rate of Page 7 of 18 readmission in under 5s is higher - 8% (4 of 50); an age group denominator is not available for 2009 data however 0-4s are also disproportionately represented in the 2009 readmissions: 7/10 relevant cases. The information generated confirms that unnecessary TCC is still a significant resource drain for the NHS. Assuming 1,000 unnecessary TCCs are undertaken per annum by the NHS at a cost of £700 per operation; and that the rate of readmission (acknowledging a high proportion of under 5s) is 5% and the average cost per readmission is £971, the tariff for these unnecessary interventions and their complications requiring readmission would be almost £750,000 in one year. This is without calculating the cost of follow-up A&E, or primary care presentations which may affect 22%xlviii, or the risk of litigation relating to poorly informed consent. Treatment of complications subsequent to NTC PCTs which performed NTCC in 2009 were asked a range of associated questions about subsequent A&E presentations, early follow-up admissions, and longer term follow-up admissions for urological surgery. The A&E data generated is particularly crude (A&E databases frequently record no searchable information on presenting issue), however patterns of presentation suggest a strong correlation between NTCC and presentation in A&E. A&E presentations in 4 weeks post NTC in 2011 across 3 NHS NTCC schemes PCT2 PCT6 TOTAL NTCCs PCT1 368 197 1,168 Episodes in A&E in 7 days of NTC Episodes in A&E 8-14 days of NTC Episodes in A&E 15- 21 days of NTC 32 5 2 28 11 8 27 11 22 Episodes in A&E 22-28 days of NTC 1 7 14 40 54 74 Episodes in A&E within 4 weeks At PCT2 (which performs mainly plastibell opreations in a clinic setting) there were 40 spells in A&E in 4 weeks of NTCC which affected 37 patients (10% of NTCC subjects); 32 of these spells (8.7% of all NTCCs) occurred in week one post NTCC. At PCT6, 54 spells in A&E in 4 weeks of NTCC affected 48 patients (24.3% of the total NTCC subjects), with 14.2% presenting in A&E in week one following NTCC. Clearly some spells are not related: but the pattern of presentation is revealing. At PCT2, 11 patients (3%) presented in A&E on the same day as their circumcision. At PCT6 (which conducts only inpatient operations on older infants/children) average time to presentation in hospital is longer but presentations are greater in number , although the cases appear less serious. The differences in rates of A&E presentations may reflect the nature of the schemes and follow up arrangements, the ease of access to a local A&E department, and also, possibly, advice given to parents about risks. Evidence suggests that PCT2’s NTCC delivery contractors may have seen one or more NTCC issues become life threatening due to delay in seeking treatment. If this is indeed the case, it is theorized that this could Page 8 of 18 have resulted in an increased emphasis to parents about risks, which might explain a high rate of very early presentation. PCT5, a commissioner which funds inpatient NTCC only, performed its own analysis of A&E data, which did not include a weekly breakdown as above. 22 patients presented in A&E within 30 days of circumcision (8.7%), of these PCT5 advises that 17 are probably or certainly NTC complications , using an estimate of 75% relevancy for those A&E presentations without diagnosis data (9 of 22 cases). The 17 patients seen in A&E with what is believed to be an NTCC adverse effect would represent 6.7% of the total NTCCs in this year. PCTs 1-4 use local contractors to deliver NTC schemes on infants aged up to 3 months under local anaesthetic. Each scheme is subject to a detailed service level agreement with explicit monitoring/audit requirements including follow up by telephone, and reporting of early post-operative issues. At PCT1 for example, GP circumcisers are contractually bound to submit a return in seven days of the end of each month, with a record of adverse events associated with treatment, and referrals into secondary care. Despite this, PCT1 responded to an initial question about recording of NTCC outcomes with, “The Trust records episodes or numbers of procedures undertaken. No other data is collected.” On challenge, PCT1 responded, “[we] are informed by the GP if any patients were sent to A&E but the trust does [sic] know if this was as a result of a complication. Therefore [we] cannot answer this question.” Asked to generate A&E data via database query, PCT1 revealed (as above) that within seven days of the operation 2.3% of NTCC subjects presented in A&E, and by the end of week 4 post circumcision, 74 were seen in A&E (6.3%), however the number of primary care follow-up issues remains unknown. PCT4 contracted the same circumcisor as PCT1, however it appears to have failed to enforce auditing requirements. In answer to a question about complications following the 2009/10 cohort of infant NTCCS (n=269) PCT3 responded that ‘no information is available’. Challenged, the commissioner approached its contractor, who advised that there were “0 adverse incidents and 0 referrals into secondary care”. By contrast, at PCT3, which in 2009 reported a similar level of NTCC (N=290), the contractor reported 16 patients requiring follow-up for issues within 7 days (5.5%); 10 of whom presented to the GP (with 8 given treatment) and 6 who were referred to A&E (it is not known whether others visited A&E without a referral). PTC4’s response lacks credibility and its apparent failure to monitor performance of its NTC programme seems particularly surprising, considering that it was implemented against the protestations of local doctors who cited the inherent clinical risks of circumcision.xlix Admissions post NHS NTCC Most NHS NTCs are performed in the age group <3 months. This is a period in which the immune system is compromised, the foreskin and glans are one structure, and loss of only 68 ml of blood (easily hidden Page 9 of 18 in a modern nappy) threatens survivall li. A further issue to consider in reviewing secondary care presentations post NTCC is that most of these operations occur in communities in which child health may be already poorer than averagelii. 4 of the 8 PCTs which funded 150 or more NTCs in 2009 provided high quality data showing admissions within 30 or 90 days post NTC either in 2009 or 2011 or both. It appears that before the question was asked, none of these PCTS had officially recorded this data. The best dataset generated comes from the largest commissioner of NTCC, and includes unique (encrypted) patient ID (to reveal repeat presentations), number of days between NTCC and admission, primary and secondary diagnosis for the admission, primary and secondary procedures, total length of stay, and total cost of the spell. Although the figures cannot be fully verified without review of patient notes, this level of details allows a high degree of certainty about the cases which are very likely to represent circumcision complications. In financial year 2011-12, 1,359 NTCs commissioned by PCT1 using plastibell were followed in 30 days by 64 episodes of admission, with length of stay of 0-12 days, and a total of £65,162. From the range of diagnoses it is clear that most of these cases may be unrelated. However, 9 episodes representing 9 patients are likely to represent NTCC complications. This includes 8 episodes coded with T81 or T792 primary diagnosis, indicating complications of a procedure or a secondary haemorrhage. These cases all occurred in 0-15 days of NTC, the length of stay ranged from 0-2 days (mean 0.75 days) and three of the subjects underwent a revision procedure during their spell. One additional case of UTI occurred, which is likely to be relevantliii and which resulted in an admission of one day. These spells cost an average of £950 each. They represent 0.59% of the NTCs performed and all are potentially life threatening complications, particularly the five infants (0.36% of the NTCs) for which the admission lasted 1 day or more. However these are unlikely to represent the only complications: many additional episodes would merit analysis, including cases of early presenting septicaemia. Two series which make for useful comparison are PCT2 and PCT6, both of which provided information on admissions following NTC in 2011. PCT2 commissioned mainly plastibell circumcisions on boys aged < 3 months, with a handful of inpatient operations; PCT6 offers NTCC only as inpatient surgery, under general anaesthetic, on children aged 6 months or older. PCT6 provided data on readmission episodes (N=41) post NTC (N=368) occurring in up to 90 days: these affected 36 patients in total. 24 episodes affecting 23 boys (11.7%) seem relevant. Of 24 relevant readmissons, 20 patients were aged 0-4 and 3 were aged 5-9. 21 patients (10.7%) underwent admission within 1-12 days of NTCC with a diagnosis of T81 or Z71.1 (feared complaint). One presented twice in week 6 post NTC with a T81 issue, and one patient presented in week 12 with dysuria. All relevant admissions in this series were daycase admissions. PCT2 shows a rate of readmission of 3.6% in 90 days which is much lower than PCT6, but data suggest cases may be more serious. In 90 days post circumcision there were 32 admission episodes representing 28 patients (7.6% of original patients); 12 episodes are deemed relevant (although the number of Page 10 of 18 patients cannot be identified). Admissions of one day affected five patients (1.4% of total NTCs). Four infants underwent a follow up operation within 3 days of NTCC (1.1%). PCT2 separately provided information showing that the cost of admissions for early complications of its NTCC programme was £9,592 across 12 cases: an average cost of £799 per patient. Longer term Adverse Effects post NHS NTCC Urological issues post neonatal NTC may take years to present, and may sometimes not be identified even where serious secondary urinary system damage has occurred [xxxvi]. Despite this, there is no evidence of any systematic monitoring of this issue among NTCC subjects in the NHS: NHS Scotland did not have any information readily available, and suggested a charge of over £5,000 to source it. Some English commissioners were able to extract the information from databases but there is no data to suggest that this had been used as part of any quality monitoring or improvement. PCT1 extracted detailed multi-year incidence rates of urological surgeries undertaken April 2006February 2012, following NTCCs performed between March 2006 and September 2012 (5.5 years) No of Patients treated No Of Admissions Cost 2005-06 0 0 2006-07 2 £3,545.34 2007-08 1 £1,184.37 2008-09 2 £5,595.48 2009-10 6 £6,941.35 2010-11 6 £9,405.85 2011-12 5 £5,676.29 TOTALS 22 £32,348.68 The overall incidence of follow up urological procedures is low at 0.27% but many episodes are serious and resource intensive: 13 surgeries were performed as a day case admission, but nine children underwent a hospital spell of 1-2 days. Some issues may not be relevant, and the dataset requires expert review however the even initial analysis raises several concerns. The first is that the diagnoses reveal a number of infants being treated for congenital issues which are generally considered a contraindication to infant NTCC, and which according to the service specification should have been excluded. The dataset also shows operations for urethral stricture (costing from £761-£788) occurring up to 3.8 years post NTCC. This issue may present over a decade after NTCC, showing that even were the scheme to stop now, resourcing of reparative procedures will be required for years into the future. Yet the Page 11 of 18 wording of PCT1’s response suggests they are unaware of this late presenting issue, although it is strongly linked to infant NTCC[xxxvi] liv., and may be the commonest complication overalllv. Limited other data is available on long term presentations: where it has been provided the denominator is not always clear, making further analysis difficult. PCT3 (which refused full data on all follow-up urological surgeries) did provide information on re-circumcisons performed between 2005 and 2011 (11 of 1,492). At 0.7% this rate is more than double the total rate of urological surgeries at PCT1, although if referencing cosmetic repeats it seems low (one London survey recorded an NTCC repeat rate of 7.5%lvi). Revision surgery of all types merits further research. The failure to include cosmetic revisions as an adverse effect in a recent metal analysis of NTCC harm is difficult to justify on scientific or ethical groundslvii. Repeat NTCCs are likely to affect a significant number of children, and, often performed under general anaesthetic, they bring new narcotic risks in addition to the post-operative issues of bleeding and infection - which may themselves cause further readmissionslviii. The child’s pain and distress cannot be discounted, nor the risk of functional damage from repeated excisions to the genitals. In Africa, re-circumcision has been shown to be associated with scarring, a longer healing time and a loss of penile sensitivity lix . Deaths In addition to four acknowledged deaths from haemorrhage or infection between September 2006 to February 2012, in February 2007 in London, an unanaesthetised ritual circumcision was followed within minutes by cardiac arrest, which led to child’s death some days laterlx. Against a background in which circumcision without pain relief has been shown to be associated with severe and persistent painlxi, a significant rise in heart ratelxii ,cortisollxiii, and incidence of serious apnealxiv, post mortem linked the trauma and the collapse. However the Crown Prosecution Service refused the case, and it was heard at inquest almost 3 years later, with a verdict of SIDS. Despite evidence that circumcision is still often performed without pain relieflxv [liv]lxvi, and expert commentary at the Moshe inquest that unanaesthetised male circumcision has the potential to cause death by traumalxvii, no action has been taken to regulate this issue in the UK. By comparison, Sweden made pain relief compulsory in all circumcision a decade agolxviii. The Jewish Medical Association openly admits that its circumcisers use no anaesthetic, preferring only ‘sweet liquid’ . Anecdotal evidence suggests that this is a euphemism for alcohollxix lxx, and that circumcisers are conscious of the public relations issues around admitting that alcohol is routinely used to quieten children during circumcisionlxxi. With anecdotal evidence suggesting that circumcision deaths may have occurred without publicitylxxii, attempts were made to investigate death rates through FOI requests made to a small series of local council safeguarding teams in areas of high NTCC incidence. This generated information on the death of Page 12 of 18 one infant with an infection which post mortem apparently linked to a recent circumcision, to the extent that police initially investigated the doctor’s practice. However a safeguarding group advised subsequently that it felt the death was not related. It cannot be established whether the death is relevant or not, although details appear to suggest a similarity in its details and handling to a case which occurred in the course of a controversial neonatal circumcision experiment in Africalxxiii. This data reveals an apparent need for further investigation to establish whether male circumcision deaths are being investigated with the same rigour as other unexpected deaths. Information, consent, commissioning and regulation Limited consent information was given as part of this project, but information reviewed suggests that doctors routinely fail to give information on the many functions of the prepuce[xxi] lxxiv lxxv, nor circumcision’s risk of future sexual difficulties including a partner’s dyspareunia lxxvilxxvii lxxviii lxxix lxxx lxxxi. They may even fail to mention the issues particular to foreskin ablation in infancy, although this has resource implications. A&E data suggests that a significant number of parents bring a child to A&E with what is a normal circumcision wound; parents often have no understanding that in early infancy, far from being a simple snip, circumcision must begin with a forceful degloving of the glanslxxxii. In any non-therapeutic operation, a full patient understanding of the risks is particularly important. With the basic legality of circumcision by proxy consent being increasingly questioned lxxxiiilxxxiv, and evidence that adults may be willing to sue for NTCClxxxv, the need for full disclosure is overwhelming. It is also important that NHS NTCC schemes follow recommended practice and common lawlxxxvi in seeking dual parental consent: at least one scheme does not. Complications information may be confused, dishonest, or just hidden. One GP circumcision clinic advises “Bleeding …is rare … significant bleeding requiring a review may be needed in less than 10% of babies”lxxxvii Another GP circumcisor advertises on his home page that “complications are minimal and less than 1%”, but elsewhere reveals that as measured by just two issues – infection, and haemorrhage requiring surgical follow-up, the real incidence is 3- 4%. This clinic is recommended by the local PCT/safeguarding Board despite evidence of substantial harm to one childlxxxviii. Invited to share their auditing of his and other local circumcisors outcomes, the Safeguarding Board refusedlxxxix. Manchester’s quality assurance scheme is unusual in the UK, and would make for useful further analysis could its managers be persuaded to co-operate with a subsequent review. It is underpinned by the idea that child circumcision safety over the long term can be promoted by free market principles– because being an NHS quality assured circumcisor will drive market share [xii]. The earning potential of this sector is acknowledged. One clinic, advertising as ‘the UK’s leading circumcision male circumcision clinic’, promotes opportunities for doctors to set up and run satellite operations, calling this “a fantastic opportunity for a self-starter”xc . A marketing strategy document Page 13 of 18 suggests a total market of 50-60,000 UK NTCCs per annum, but warns that local GPs are ‘competitive’ about the income potential, and advises that any new local clinic will require a “continuous marketing campaign” to attract parental customxci. This paper assumes more conservatively that NTCC is likely to affect at minimum 40,000 British boys each year, based on census data which shows over 3.3 million adherents to the faiths in which NTCC is practiced. Dubious TCC may affect at least a further 1,000. The General Medical Council (GMC) has revealed that 20 circumcision complaints against 14 doctors were investigated in the 3 year period ending December 2012. In this period two GPs were suspended. Overall were 54 separate allegations, of which the majority concerned clinical care. This appears to represent an increase on previous yearsxcii, although as the information is extracted via free text search it might still represent an underestimation. The GMC states it does not know how many doctors have been investigated in relation to an NTCC death. One case involving the former Head of the Islamic Medical Association does appear in details of Fitness to Practice hearing, however the GMC has been at pains to declare the doctor not responsible, citing the death as, ‘simply an unfortunate consequence of the procedure’xciii Discussion “It is a curious fact that one of the operations most commonly performed in this country [the UK] is also accorded the least critical consideration. In order to decide whether a child's foreskin should be ablated the normal anatomy and function of the structure at different ages should be understood; the danger of conserving the foreskin must then be weighed against the hazards of the operation, the mortality and after-effects of which must be known. Though tens of thousands of infants are circumcised each year in this country, nowhere are these essential data assembled. “ Douglas Gairdner, The Fate of the Foreskin xciv, 1949 Gairdner’s evidence of serious morbidity and mortality from circumcision, and his urging that doctors recognise normal anatomical development and function, resulted in the leaders of the newly formed NHS refusing to fund routine circumcision. Today the situation is reversed, and tens of thousands of boys have been subjected to an NHS circumcision with neither medical indication nor personal consent. NHS justifications for this, from the claim that forced circumcision is ‘culturally sensitive’ to the idea that it is an ‘essential health requirement’xcv of some ethnic/faith groups, lack moral and intellectual rigour. The revelation that further boys (and parents) are misled into unnecessary surgery, because some doctors cannot recognise normal sexual anatomy, is equally shaming. Page 14 of 18 Underlying much NTC, in the NHS and elsewhere, is the idea that where circumcision is to be performed, it is best done early, because it is more dangerous in adultsxcvi. This claim goes unreferenced, because it is without evidence. Mass NTC in Africa has brought new clarity to the issues around the age-related safety of NTC in comparable settings: experiments show that though the range of complication measures post adult NTC may be wider (often including pain, and subject perception), surgical adverse events may still be more numerous and/or more significant in neonates [xxxii] [xxxi]xcvii xcviii xcix . The trials have also shown that adult NTC can be performed under local anaesthetic in a matter of minutes. This week’s approval of PrePexc and early indications from its clinical trialsci raises the potential that adult NTC will only become simpler and safer cii Against this background, UK medical authorities should urgently review circumcision practice and harms in the UK, and make a judgement on future policy which considers that adult NTC may not only be more ethical than child NTC: it may also be safer. Harm to a minor is not the same as minor harm. i Dennison, S. Five minutes that ended a baby boy’s life, The Independent, 1993 ii Madden NP, Boddy SA. Should religious circumcisions be performed on the NHS.BMJ. 1991;302:47 iii Billings, PJ, Gordon EM. Should religious circumcisions be performed on the NHS?BMJ.1991;302:292 iv Stringer MD, Brereton RJ. Should religious circumcisions be performed on the NHS?BMJ.1991;302:292 v http://www.guardian.co.uk/lifeandstyle/2000/may/23/healthandwellbeing.health2 accessed on 25th May vi http://www.thebcom.org/ourwork/health-forum/219-bcom-bolton-pct-circumcision-service.html vii http://www.scotland.gov.uk/Publications/2008/02/14143159/3 viii Response from the Scottish Government received July 2012 ix Advised as response to a freedom of information request to NHS National Services Scotland in August 2009 x Circumcision Dangers Spelt Out, November 2001, BBC Circumcision dangers spelt out http://news.bbc.co.uk/1/hi/health/1670590.stm xi CORBETT, HJ, HUMPHREY, GME, Early complications of circumcision performed in the community BRITISH JOURNAL OF GENERAL PRACTICE, Volume 53, Number 496: Pages 887-888, November 2003. Available at http://www.cirp.org/library/complications/corbett1/ xii Paranthaman K, Bagaria J, O'Moore E, The need for commissioning circumcision services for non-therapeutic indications in the NHS: lessons from an incident investigation in Oxford. J Public Health (Oxf). 2011 Jun;33(2):280-3. doi: 10.1093/pubmed/fdq053. Epub 2010 Jul 14. xiii Campbell, D. NHS Urged to offer circumcisions to avoid botched operations. July 2010 http://www.guardian.co.uk/society/2010/jul/11/doctors-urgecircumcision-on-nhs xiv Gollins, H, Whittaker, P. Quality Assurance for Male Religious Circumcision Services across Greater Manchester, January 2011, Greater Manchester Safeguarding Children Board xv BACCHNEWS: The Quarterly Newsletter of the British Association for Child Health, June 2012 xvi Non Therapeutic Circumcision of Male Minors, Royal Dutch Medical Association, May 2010 xvii Senator Bacik wants male circumcision banned, Iona Institute, June 2011 http://www.ionainstitute.ie/index.php?id=1500 xviii Legislation on circumcision stalled, HELSINGIN SANOMAT, April 2010 http://www.hs.fi/english/article/Legislation+on+circumcision+stalled/1135256085478 xix 'Intactivists' to San Francisco: Ban circumcision, CNN, November 2010 http://www.cnn.co.uk/2010/HEALTH/11/19/male.circumcision.sf/index.html xx Boy died after circumcision in Oslo, Bergens Tidende, May 2012 Page 15 of 18 xxi Expert Statement: Dr med. Wolfram Hartmann, President of "Berufsverband der Kinder- und Jugendärzte" or the Hearing on the 26th of November 2012 Concerning the Drafting of a Federal Government Bill: "Drafting of a law regarding the scope of child care and custody in the case of male circumcision" German original available at http://www.kinderaerzte-im-netz.de/bvkj/kinpopup/psfile/pdf/70/121126_Ste50aa5e211e6a6.pdf and English translation accesed at http://www.intactamerica.org/german_pediatrics_statement xxii Sheffield Clinical Commissioning Group, Governing Body Meeting minutes 2nd May 2013 accessed at http://www.sheffieldccg.nhs.uk/Downloads/CCG%20Board%20Papers/130502/PAPER%20I%20Commissioning%20of%20non%20therapeutic%20male%20circum cisions.pdf on 22nd May xxiii Response from the Scottish Government received July 2012 xxiv http://wiganlscb.com/downloads/Male%20Infant%20circumcision%20Press%20release.pdf xxv http://www.gmsafeguardingchildren.co.uk/projects/circumcision/ accessed on 24th May xxvi http://www.bristolpct.nhs.uk/theTrust/equality/Religion/Pt%20Info%20Leaflet%20011007.pdf xxvii Service Specification NHS Contract For The Provision Of Religious And Cultural Circumcision Scheme, Commissioner Lead Leroy McConnell, April 20092012 xxviii Manual for early infant circumcision under local anaesthesia, WHO (with JHPIEGO) 2010 xxix GMC Fitness to Practice Panel, 27 OCTOBER TO 3 NOVEMBER 2008, Name of Respondent Doctor: Dr Muhammad SIDDIQ http://webcache.gmcuk.org/minutesfiles/Siddiq%20(M)%20PUBLIC%20minutes.htm xxx http://www.sloughexpress.co.uk/News/All-Areas/Slough/Baby-boy-bled-to-death-after-operation-inquest-heard-9875.htm xxxi http://www.mirror.co.uk/news/uk-news/goodluck-caubergs-baby-bled-to-death-1458305 xxxii Queen’s Park baby bled to death two days after being circumcised, June 2012 www.kilburntimes.co.uk/news/queen_s_park_baby_bled_to_death_two_days_after_being_circumcised_1_1419367 xxxiii Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, et al. (2005) Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: The ANRS 1265 trial. PLoS Med 2:e298. xxxiv Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 2007;369:643-56. xxxv Palit V, Menebhi DK, Taylor I, Young M, Elmasry Y, Shah T. A unique service in UK delivering Plastibell circumcision: review of 9-year results. Pediatr Surg Int.2007;23:45–8 xxxvi Circumcision, Factsheet For Medical Professionals Practising In The UK, Medical Protection Society, April 2013 http://www.medicalprotection.org/mps-policyon-circumcision-factsheet.pdf xxxvii Pieretti RV, Goldstein AM, Pieretti-Vanmarcke R. Late complications of newborn circumcision: a common and avoidable problem. Pediatr Surg Int 2010; 26(5): 515–518. xxxviii Malone P, Steinbrecher H, Medical aspects of male circumcision.BMJ. 2007;335(7631):1206. xxxix Joudi M,Fathi M,Hiradfar M, J Pediatr Urol. 2011 Oct;7(5):526-8. Epub 2010 Sep 18, Incidence of asymptomatic meatal stenosis in children following neonatal circumcision xl Bollinger, D, LOST BOYS: AN ESTIMATE OF U.S. CIRCUMCISION-RELATED INFANT DEATHS, THYMOS: Journal of Boyhood Studies, Vol. 4, No. 1, Spring 2010, 78-90 xli American Academy of Pediatrics Task Force on Circumcision. Technical report:male circumcision. Pediatrics 2012;130:e757–85. xlii Cultural Bias in the AAP’s 2012 Technical Report and Policy Statement on Male Circumcision, Morten Frisch, MD, PhD, Yves Aigrain, MD, PhD, et al. xliii http://www.bbc.co.uk/news/uk-england-manchester-21374643 xliv Rickwood, AMK, Kenny SE, Donnell, SC. Towards evidence based circumcision of English boys: survey of trends in practice, BMJ 2000;321:792-793 (30 September) xlv Circumcision: A cut below accessed at www.thebabywebsite.com/article.96.Circumcision_-_A_Cut_Below.htm on 18th March 2013 xlvi Commissioning guide for foreskin conditions: draft (not approved) BAUS BAPS BAPU, accessed online at http://www.rcseng.ac.uk/surgeons/working/docs/foreskin-conditions-draft-commissioning-guidance xlvii An investigation of male circumcision in XXX: Public Health Research Report No XXX (Reference redacted to protect trust anonymity, but available on request) xlviii de la Hunt MN. "Paediatric Day Care surgery: a hidden burden for primary care?" Ann R Coll Surg Engl. 1999; 81:179-82 xlix XXX Primary Care Trust, Religious and Cultural Circumcisions across XXX, June 2005, paper provided to the researcher under FOI, redacted for anonymity purposes but available on request, where appropriate l Special statement, Dangers of Neonatal Circumcision, Doctors Opposing Circumcsion March 2004, accessed at http://www.doctorsopposingcircumcision.org/pdf/specialstatement.pdf on 29th May 2013 li Lubin B., Clin Haematol. 1978 Feb;7(1):19-34., Neonatal anaemia secondary to blood loss lii Laird LD, Amer MM, Barnett ED, Barnes LL. Muslim patients and health disparities in the UK and the US. Arch Dis Child. 2007;92:922–926. liii Prais, D, Shoov-Furman, R, Amir, J, Is ritual circumcision a risk factor for neonatal urinary tract infections? Arch Dis Child doi:10.1136/adc.2008.144063 Page 16 of 18 liv Upadhyay V, Hammodat HM, Pease PW. Post circumcision meatal stenosis: 12 years' experience. N Z Med J. 1998 Feb 27;111(1060):57-8. lv Van Howe RS. Incidence of meatal stenosis following neonatal circumcision in a primary care setting Clin Pediatr (Phila). 2006 Jan-Feb;45(1):49-54. lvi Thalassis, N, Circumcision: in whose care? Non‐clinical male circumcision services in Kensington & Chelsea and Westminster, BME Health Forum, July 2009 available at http://www.bmehf.org.uk/files/7713/6536/5068/Circumcision_InWhoseCare.pdf lvii Weiss HA, Larke N, Halperin D and Schencker, I Complications of circumcision in male neonates, infants and children: a systematic review BMC Urology 2010, 10:2 doi:10.1186/1471-2490-10-2 lviii Brisson PA, Patel HI, Feins NR, Revision of circumcision in children: Report of 56 cases, J Pediatr Surg. 2002 Sep;37(9):1343-6. lix http://www.who.int/bulletin/volumes/88/12/09-072975/en/index.html# lx Curtis, P. Police probe death after circumcision Guardian, February 2007 http://www.guardian.co.uk/uk/2007/feb/17/religion.world1 lxi Howard CR, Howard FM, and Weitzman ML. Acetaminophen analgesia in neonatal circumcision: the effect on pain. Pediatrics 1994;93(4):641-646. lxii Lidocaine-prilocaine cream for analgesia during circumcision in newborn boys (Cochrane Neonatal Review) Taddio A, Ohlsson A, Ohlsson K, 2009 lxiii Stang HJ, Gunnar MR, Snellman L, Condon LM, Kestenbaum R. Local anesthesia for neonatal circumcision. Effects on distress and cortisol response. JAMA 1988; 259: 1507-11. lxiv Lander J, Brady-Freyer B, Metcalfe JB, et al. Comparison of ring block, dorsal penile nerve block, and topical anesthesia for neonatal circumcision. JAMA 1997; 278:2158-62. Accessible at http://www.cirp.org/library/pain/lander/ lxv http://www.mohel-circumcision.co.uk/1298.html lxvi http://www.pcc.org.uk/news/index.html?article=NjIyNA== Press Complaint against Daily Mail by Dr John Warren regarding an article on NTCC dated July 14, 2009. The Mail revealed in correspondence that all doctors consulted for the article said they ‘preferred not to use pain relief. lxvii Prof Fleming, in commentary to the Coroners Court, as reported by inquest attendee Dr John Warren, Chairman of Norm-UK, private correspondence lxviii "Snitt som kostar - om omskärelse av pojkar". Sveriges Radio (in Swedish). 22 October 2006. lxix GP-Mohel Cohen recommends wine as anaesthesia, and anecdotal evidence suggests this is a routine practice in Jewish ritual circumcision. lxx The video Cut, by Elijahu Ungar-Sargon reveals wine may be given both before and repeatedly during ritual circumcision lxxi At the Moshe inquest, Mohel Moshe Perry answering a question about pain relief said he gave the infant “W…grape juice.” Reported in personal correspondence by Dr John Warren, Chair, NORM-UK lxxii Riley, Harrison, Senior Commissioning Manager, Heart of Birmingham tPCT: Religious Circumcision, 9.12.03 lxxiii http://ripe-tomato.org/2013/03/31/bostonbotswana-circumcision-trial-2/ lxxiv Taylor, J. et al., "The Prepuce: Specialized Mucosa of the Penis and Its Loss to Circumcision," BJU 77 (1996): 291–295. lxxv Cold, C. and Taylor, J., "The Prepuce," BJU 83 (1999): suppl. 1: 34–44. lxxvi Kim, D. and Pang, M., "The Effect of Male Circumcision on Sexuality," BJU International 99 (2007): 619-22. lxxvii Bronselaer, G. et al., "Male Circumcision Decreases Penile Sensitivity as Measured in a Large Cohort," BJU International (2013). lxxviii Frisch, M., Lindholm, M., and Grønbæk, M., "Male Circumcision and Sexual Function in Men and Women: A Survey-based, Cross-sectional Study in Denmark," International Journal of Epidemiology (2011);1–15. lxxix Sorrells, M. et al., "Fine-Touch Pressure Thresholds in the Adult Penis," BJU International 99(2007): 864-869. lxxx O’Hara, K. and O’Hara, J., "The Effect of Male Circumcision on the Sexual Enjoyment of the Female Partner," BJU 83 (1999): suppl. 1: 79–84 lxxxi Bensley, G. and Boyle, G., "Effects of Male Circumcision on Female Arousal and Orgasm," N Z Med J 116 (2003): 595-596. lxxxii Personal correspondence with Tom De Jong, Professor of Paediatric Urology, Netherlands lxxxiii Fox M, Thomson M. A covenant with the status quo? Male circumcision and the new BMA guidance to doctors. J Med Ethics 2005;31:463-9. lxxxiv Hall, A. Religious groups outraged after German court rules circumcision amounts to 'bodily harm', Daily Mail August 2012 lxxxv http://www.mirror.co.uk/news/uk-news/ritual-circumcisions-illegal-431574 lxxxvi Robinson, R, Makin, E, and Wheeler, R. Consent for Non-Therapeutic Male Circumcision on Religious Grounds, Ann R Coll Surg Eng 2009 March; 91 (2): 152-154 lxxxvii http://www.amsclinic.co.uk/aftercare.html lxxxviii Mum to sue over botched circumcision operation, The Sentinel, June 2009 http://www.thisisstaffordshire.co.uk/Mum-sue-GP-son-s-botched-circumcisionoperation/story-12490751-detail/story.html#axzz2V0UYAoOk lxxxix Personal correspondence with Chair, xc http://www.circumcisioncentre.co.uk/about-circumcision-centre/for-doctors xci Unpublished paper, “CIRCUMCISION CLINICS an easy idea but fraught with statistics” 28-7-07 - obtained via an applicant for work at the clinic. xcii Information was supplied under FOI in April 2010 concerning allegations relating to circumcision processed in the period since a database was introduced in April 2006 – these number 29 over this four year period xciii Correspondence 4 September 2009 Page 17 of 18 xciv Gairdner D. The fate of the foreskin: a study of circumcision. Br Med J 1949;2:1433-7. xcv Riley, Harrison Religious Circumcision, Heart of Birmingham tPCT REPORT, December 2002 xcvi Hutson, J M, Circumcision: a surgeon’s perspective J Med Ethics 2004;30:238-240 doi:10.1136/jme.2002.001313 Symposium on circumcision xcvii Bowa K, Li MS, Mugisa B, Waters E, Linyama DM, Chi BH, Stringer JS, Stringer EM. A controlled trial of three methods for neonatal circumcision in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2013 Jan 1;62(1):e1-6. doi: 10.1097/QAI.0b013e318275741b. xcviii Young MR, Bailey RC, Odoyo-June E, Irwin TE, Obiero W, Ongong'a DO, Badia JA, Agot K, Nordstrom SK. Safety of over twelve hundred infant male circumcisions using the Mogen clamp in Kenya. PLoS One. 2012;7(10):e47395. doi: 10.1371/journal.pone.0047395. Epub 2012 Oct 17. http://www.ncbi.nlm.nih.gov/pubmed/23082162 xcix Plank RM, Ndubuka NO, Wirth KE, Mwambona JT, Kebaabetswe P, Bassil B, Lesetedi C, Hussein FM, Magetse J, Nkgau M, Makhema J, Mmalane M, Creek T,Powis KM, Shapiro R, Lockman S. A Randomized Trial of Mogen Clamp versus Plastibell for Neonatal Male Circumcision in Botswana. J Acquir Immune Defic Syndr. 2013 Jan 10. [Epub ahead of print] c McNEIL, DG, Circumcision Device Approved by World Health Organization, May, 2013 http://www.nytimes.com/2013/06/01/health/circumcision-device-approved-by-world-health-organization.html?_r=0 ci Keller, DM, Nurses Take on Task of 2 Million Circumcisions in Africa August 2012 http://www.medscape.com/viewarticle/768679 cii Tasamba, J The Do-It-Yourself Circumcision, April 2013, Independent http://www.independent.co.ug/News/regional-news/4068-the-do-it-yourself-circumcision Page 18 of 18