The HALOS (Hospital Admission Length Of Stay) model: A new tool
advertisement

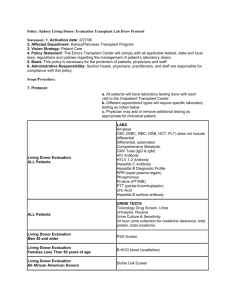
The HALOS model Page |1 The HALOS (Hospital Admission Length Of Stay) model: A new tool for predicting hospital length of stay after liver transplantation Kartik R Krishnan, MD1, Renuka Bhattacharya, MD2, Arema Perreira, MD2, Robert L Carithers, Jr., MD2, Jorge Reyes, MD3 and James D Perkins, MD3. 1Internal Medicine, University of Washington, Seattle, WA, United States; 2Gastroenterology, University of Washington, Seattle, WA, United States and 3Transplant Surgery, University of Washington, Seattle, WA, United States. ABSTRACT Background: Liver transplant centers are under increasing pressure to understand and optimize transplant-related costs. Hospital admission length of stay (LOS) is known to be a significant driver and useful surrogate for cost. We sought to develop and evaluate mathematical models predictive of LOS through retrospective analysis of the large, multi-institutional United Network for Organ Sharing Standard Transplant Analysis and Research files. Methods: Of 45,256 adults (≥18 years) who underwent liver transplantation for any indication between January 1, 2003 and November 30, 2010, 3,705 were excluded for missing LOS data or death less than 19 days into the hospital stay, leaving 41,551 recipients in the study. For predictive model building internal split-group validation was employed, with 75% and 25% of the study population randomly assigned to the training and validation sets, respectively. Multiple linear regression was used to generate four models predicting LOS, correlating to the stages of the transplantation process: (1) using only recipient factors; (2) using a combination of recipient factors and payment source; (3) using a combination of recipient factors, payment source, and donor factors; and (4) using a combination of recipient factors, payment source, donor factors, and one posttransplant factor from the transplant admission (acute cellular rejection episode). Use of the models projected the validation patients as low (≤8 days), moderate (>8 to 18 days), or high risk (>18 days) for prolonged LOS. Using receiver operating characteristic curve analysis from logistic regression of the three groups, we measured discrimination of our models by calculating the area under each curve (AUC). Results: LOS ranged from 1 to 528 days, with a mean of 17.38 days (SD of 22). Overall, xx recipient factors, primary payment sources, x donor factors, and postoperative acute cellular rejection during the transplant admission were identified as predictors of LOS. The HALOS model Page |2 For prediction of the high risk group, the AUC was 0.73, 0.73, 0.74, and 0.75 for models (1) through (4), respectively. For prediction of the moderate risk group, the AUC was 0.55, 0.55, 0.56, and 0.57 for models (1) through (4), respectively. For prediction of the low risk group, the AUC was 0.68, 0.68, 0.70, and 0.71 for models (1) through (4), respectively. Conclusion: This study is the first to identify mathematical models predictive of the risk for prolonged LOS, with each predictor variably weighted based on the data. Most importantly, the models accurately identify patients at high risk for prolonged LOS, and can serve as valuable tools to transplant centers striving to understand transplantrelated costs. INTRODUCTION As their operating costs continue to rise, there is increasing pressure on liver transplant (LT) centers to understand and optimize transplant-associated costs. Patients who are deemed medically “high risk” are sometimes delayed for transplant listing by transplant centers to obtain better insurance coverage, out of concern that their care will be prohibitively expensive to the transplant center. Conversely, financial approval is easier to obtain for those patients thought to be at low risk for an expensive, long hospitalization after LT. Unfortunately, to date these costs have been largely unpredictable at the time of listing, resulting in unnecessary delays in listing while waiting for insurance coverage. Transplant admission hospital length of stay (LOS) is a well-known driver and useful surrogate of transplant-associated costs [1]. While the model for end-stage liver disease (MELD) and donor risk index (DRI) have each been found to be predictors of LOS [2-7], no model currently exists to more directly identify potential LT recipients at highest risk for a prolonged LOS. To aid the difficult decisions involved in recipient listing, donor selection, and postoperative management, there remains an important need to understand the factors that affect costs following LT. Our study uses retrospective analysis of a large, multi-institutional database to construct mathematical models predictive of LOS. Factors examined in the database include recipient factors, payment factors, donor factors, and one postoperative factor (acute cellular rejection). Identification of recipient factors affecting LOS may improve the pretransplant evaluation and listing process, while an understanding of donor factors may assist surgeons in graft selection. The HALOS model Page |3 In our experience, postoperative events such as acute cellular rejection (ACR), biliary stenosis, hepatic artery thrombosis and portal vein thrombosis lengthen hospital LOS, as time is spent managing these complications. Of these events, data on ACR are carefully recorded in the multi-institutional database, making this important complication accessible for our retrospective analysis. ACR was evaluated for any potential correlation with LOS, and to determine its influence on recipient and donor selection factors. PATIENTS AND METHODS Protocol, Design, Data Sources, and Inclusion Criteria The expedited review process of the institutional review board of the University of Washington was used to approve this project. A retrospective cohort study was conducted, including data from LT recipients during the MELD era obtained from the United Network for Organ Sharing Standard Transplant Analysis and Research (UNOS STAR) files. The UNOS STAR files include data submitted by the members of the Organ Procurement and Transplantation Network (OPTN) on all waitlisted candidates, transplant recipients, and donors [8]. The Health Resources and Services Administration within the U.S. Department of Health and Human Services provides oversight for the activities of the OPTN/UNOS contractor. For the present study, inclusion was restricted to adult patients (≥ 18 years) who underwent liver transplantation between January 1, 2003 and November 30, 2010 for any indication. Patients with multiple organ transplants were included, while those lacking length of stay data were excluded. Length of stay was defined within the UNOS STAR files as the number of consecutive hospitalization days from 24 hours prior to transplantation to the day of discharge. Patients who died within 18 days of transplant during the initial posttransplant hospital stay were excluded, and we refer to this group as the early death patients. This was done to avoid skewing the data. Our concern was that patients dying posttransplant without first enduring a long hospital stay would share more predictors with those patients with prolonged LOS than with those surviving patients with short or moderate LOS. Therefore, we feared that inclusion of these early death patients would obscure the characteristics of the surviving patients who also did not have prolonged hospital stays. LOS for the entire available population was divided into quartiles, and then the cutoff number of 18 days was chosen because this was the LOS The HALOS model Page |4 of the 75th percentile of patients. This cutoff point was chosen to include in the study those patients who died only after a prolonged (falling within the uppermost quartile) hospital stay, while excluding those who died earlier. Missing categorical data was recorded as “unknown”. For missing continuous data, the mean of the existing data for that variable was substituted. No continuous data variable had data missing for greater than 1% of patients. This work was supported in part by Health Resources and Services Administration contract 234-2005-370011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. Clinical Outcomes and Covariate Definitions The primary outcome was LOS, a useful marker of cost. The secondary outcome was recipient mortality. Recipient covariates included age, gender, body mass index (BMI), self-identified ethnicity, liver disease diagnosis, blood type, medical condition at the time of transplant (living at home, living in a non-intensive care unit (ICU) hospital room, or living in the ICU), primary mode of payment, secondary mode of payment, dialysis in the week before transplant, encephalopathy prior to transplant, ascites prior to transplant, use of any type of life support, use of mechanical ventilation, diabetes mellitus (as recorded in the UNOS STAR files), peripheral vascular disease, portal vein thrombosis, history of previous abdominal surgery, transjugular intrahepatic portosystemic shunt (TIPS) present at the time of transplant, any history of variceal bleeding prior to transplant, serum albumin, laboratory MELD score, receiving exception MELD points for hepatocellular carcinoma (HCC), history of previous transplant, number of previous transplants, days on transplant list, receipt of multiple transplanted organs, allograft type, and transplant procedure (whole or reduced/split). The UNOS database defines life support as mechanical ventilation, intraaortic balloon pump, or a mechanical heart device. Other definitions used by the UNOS database have been described elsewhere [8]. Recipient bilirubin, INR, and serum creatinine were not included in the statistical analysis, given their close correlation with the laboratory MELD score. Model-building was conducted in four broad stages, involving (1) recipient factor analysis, (2) payment factor analysis, (3) donor factor analysis, and finally (4) The HALOS model Page |5 postoperative factor analysis. The staged approach was taken to simulate the transplantation process through its different stages, including recipient listing (at which time payment source is determined), donor selection, and postoperative management, with the goal of maximizing the clinical utility of this study at each of these transplantation process stages. For the purposes of statistical analysis, liver disease diagnoses were grouped into larger umbrella diagnoses. Specifically, the umbrella diagnosis liver cancer was used for all cases with the recorded diagnoses of hepatocellular carcinoma (HCC); HCC and cirrhosis; fibrolamellar carcinoma; cholangiocarcinoma; hepatoblastoma; hemangioendothelioma, hemangiosarcoma, or angiosarcoma; and bile duct cancer. The umbrella diagnosis of cholestatic disease includes recorded diagnoses of primary biliary cirrhosis and all types of secondary biliary cirrhosis. The umbrella diagnosis of viral cirrhosis was assigned to all cases with a hepatitis A, B, C, D, or non-A, non-B diagnosis. The umbrella diagnosis of metabolic disease was assigned to all cases with a recorded diagnosis of α-1 antitrypsin deficiency; Wilson’s disease or other copper metabolism disorder; hemochromatosis or hemosiderosis; glycogen storage disease type I or II; hyperlipidemia or homozygous hypercholesterolemia; tyrosinemia; primary oxalosis/oxaluria or hyperoxaluria; maple syrup urine disease; or metabolic disease: other. The umbrella diagnosis of benign tumor was assigned to all cases with a recorded diagnosis of hepatic adenoma, polycystic liver disease, or benign tumor: other. Also for the purposes of statistical analysis, American Indian, Pacific Islander, and multiracial patients were combined into one group. Donor covariates included age, gender, blood type, cause of death, ethnicity, donor after cardiac death (DCD), extended donor criteria (renal transplant definition) [9], weight, height, BMI, serum creatinine at death, aspartate aminotransferase, alanine aminotransferase, total bilirubin, diabetes, chronic hypertension, hepatitis C virus (HCV) infection, hepatitis B virus (HBV) infection, donor clinical infection, organ sharing region, distance between donor and recipient, and cold ischemia time (CIT). Donor and recipient ABO blood type match was also included in this analysis as a covariate. One postoperative variable, ACR during the transplant admission, was included in separate analysis. Statistical Analysis The HALOS model Page |6 We used descriptive statistics of mean ± SD for the continuous data and percentages for categorical data. Linear regression with standard least squares was used to perform univariable and multivariable analysis to determine factors associated with increasing LOS. A P-value of 0.05 was used to determine statistical significance. Survival curves were generated using Kaplan-Meier analysis with log-rank test for significance. Analyses were performed using JMP version 9.0.2 (SAS Institute, Cary, NC). To build a predictive model, internal split-group validation was employed; 75% and 25% of the study population were randomly assigned to the training and validation sets, respectively. Multiple linear regression was used to generate four models predicting LOS, correlating to the stages of the transplantation process: (1) a model using only recipient factors; (2) one using a combination of recipient factors and payment source; (3) one using a combination of recipient factors, payment source, and donor factors; (4) and one using a combination of recipient factors, payment source, donor factors, and one posttransplant factor from the transplant admission (acute cellular rejection episode). Model-building was approached in stages, as described above, to simulate the transplantation process through its different stages (recipient listing, including payment/financial analysis; donor selection; and postoperative management) and to maximize the clinical utility of the study at each of these transplantation stages. For the purposes of our analysis, living donor was included as a covariate in the recipient factors analysis, rather than in the subsequent donor factors analysis. This approach was taken because the presence of a potential living donor is information available around the time of listing, and is therefore information present at the same time other recipient factors become known to the transplant team. This approach is consistent with our goal of maximizing the clinical utility of the study. The four models were then used to predict which of three categories each validation patient would fall into: low (≤8 days), moderate (>8 to 18 days), or high risk (>18 days) for prolonged LOS. The parameters of these categories are based on the quartiles of the entire study cohort’s LOS distribution, with an LOS of 8 days representing the 25th percentile and an LOS of 18 days representing the 75th percentile. Using receiver operating characteristic curve analysis from logistic regression of the three groups, we measured discrimination of our models by calculating the area under each curve (AUC). The HALOS model Page |7 For multivariable analysis, both backward and forward analyses were performed, including variables with a p-value of less than 0.25 and setting a p-value of 0.1 for initial placement in the model. To be kept in the model, a significance of p < 0.05 was required. Primary source of payment was analyzed separately, after the main univariable and multivariable recipient factor analysis. This separate treatment of the payment source variable was done with the goal of better assisting transplant centers in financial analysis. Multivariable analysis was performed on the primary payment variables, controlling for the significant recipient predictors identified earlier. Donor predictors of LOS were likewise identified through univariable and multivariable analysis while controlling for the recipient predictors and payment source already identified. The postoperative variable of transplant admission ACR episode was then analyzed through the same process, now controlling for the significant recipient, payment, and donor predictors already identified. Linear regression, a parametric test, was chosen despite the non-Gaussian distribution of the LOS data. This approach is based on the central limit theorem, which allows the application of linear regression to a non-Gaussian distribution of greater than 100 data points [10]. RESULTS Recipient demographics Between January 1, 2003 and November 30, 2010, a total of 45,256 adult liver transplants were performed and recorded in the UNOS STAR files. Of these transplants, 3,705 cases were excluded due to either missing LOS data or recipient death less than 19 days after transplantation. The mean LOS was 17.38 days (SD of 22), with a minimum LOS of 1 day for a surviving patient and a maximum of 528 days. The mean follow-up period was 1,032 days (764). Of the 41,551 patients included in our analysis, 67.2% were male (table 1). The mean BMI was 28.0 (SD of 5.7) and the mean age was 52.9 years (10.2). A total of 72.6% self-identified as white, 12.7% as Hispanic, and 9.3% as black. The primary liver disease diagnosis was viral cirrhosis for 29.9% of recipients. A majority of recipients, 71.7%, were living at home immediately prior to transplant, while 16.9% were confined to a general hospital floor bed and 11.4% were ICU-bound. Most (61.1%) relied on private The HALOS model Page |8 insurance as a primary source of payment, while Medicare/Medicaid was the primary source for 34.5% of recipients. A large majority of recipients, 65.9%, were reported as exhibiting hepatic encephalopathy prior to transplant, while 77.4% were reported as exhibiting ascites. There were 6,440 cases involving recipients with diabetes, 364 involving recipients with peripheral vascular disease, and 2,287 involving recipients with portal vein thrombosis. A large minority of cases, 40.4%, involved recipients with a history of prior abdominal surgery, with 2,926 cases involving a recipient with a history of previous liver transplant. The mean serum albumin was 2.9 mg/dl (0.7) and mean MELD score was 21.2, with a large SD (9.9). Donor demographics The mean donor age was 40.9 (17), while 60% of donors were male (table 2). Stroke (40.5% of deceased donors) or head trauma (37.5% of deceased donors) were the leading causes of death among deceased donors, while anoxia was the cause of death for 15.5% of donors. A large majority of donors, 68.4%, were white, while 12.8% and 15.4% of donors were Hispanic and black, respectively. A total of 1,729 donors were DCD donors, while 24.9% met extended donor criteria. The mean donor was overweight (BMI 26.7 (5.8)) and had renal insufficiency at the time of death (mean serum creatinine 1.5 (1.6)). A total of 7.1% and 30.9% of donors were known to have diabetes and hypertension, respectively. A small portion of donors were HCV-positive (2.8% with serum HCV-antibody) and HBV-positive (0.2% with serum HBV surface antigen), while a significant portion of donors, 35.6%, had a clinically-significant infection at the time of death. The mean distance from the donor to recipient was 140 miles (247), and the mean cold ischemia time was 7.2 hours (3.7). Hospital course A total of 6.3% of recipients experienced ACR during the transplant admission, with 78.7% of these patients receiving anti-rejection treatment (table 3). Recipient factors associated with hospital LOS Univariable analysis The HALOS model Page |9 A large group of recipient factors emerged as statistically significant predictors of LOS in univariable analysis of the training set, and was included in multivariable analysis (table 4). This included the liver disease diagnoses of acute hepatic necrosis, autoimmune disease, liver cancer, cholestatic disease, cryptogenic disease, alcoholrelated disease, metabolic disease, NASH, and other, with viral cirrhosis as the reference variable. Hospital- and ICU-bound recipient status at transplant were significant in univariable analysis, with home status as the reference variable. Dialysis in the week prior to transplant emerged as a significant predictor in univariable analysis, as did life support and ventilator status. The presence of any degree of encephalopathy was a significant predictor in univariable analysis, with the absence of encephalopathy as the reference variable. Other variables emerging from univariable analysis included recipient diabetes, peripheral vascular disease, portal vein thrombosis, previous abdominal surgery, TIPS presence, history of variceal bleeding, serum albumin, MELD score, exception MELD points for HCC, previous liver transplantation, time on the waiting list, simultaneous transplantation of multiple organs, and living donor. Simultaneous pancreas transplant and simultaneous intestine transplant were variables that each emerged from univariable analysis. However, given that 91% of subjects who underwent pancreas transplantation also underwent intestine transplantation at the same time, the pancreas transplantation variable was dropped after the univariable analysis. Similarly, 88% of patients who were requiring mechanical ventilation at the time of transplant were also requiring life support (as defined above); therefore, the ventilation variable was dropped after univariable analysis despite achieving statistical significance in the univariable analysis. Multivariable analysis A large group of covariates emerged as predictors of LOS, with backward and forward analyses each yielding the same set of predictors (table 4). The strongest such predictors included simultaneous intestine transplant (estimate 34.58, 95% CI 31.29 to 37.87), simultaneous heart transplant (18.70, 13.10 to 24.37), two or more previous LT (10.34, 7.60 to 13.10), life support at the time of transplant (9.64, 8.35 to 10.93), and ICU status (7.25, 6.19 to 8.30). Each of these variables was associated with a longer LOS. Other predictors of longer LOS included age in years (0.13, 0.11 to 0.15), hospitalbound status (4.49, 3.78 to 5.20), dialysis within the week prior to transplant (3.62, 2.72 to 4.52), encephalopathy (3.02, 2.18 to 3.87), moderate ascites (1.51, 0.94 to 2.08), diabetes The HALOS model P a g e | 10 (0.91, 0.37 to 1.46), portal vein thrombosis (2.33, 1.31 to 3.37), previous abdominal surgery (0.96, 0.45 to 1.47), TIPS at transplant (1.18, 0.32 to 2.05), one previous LT (5.40, 4.39 to 6.42), and laboratory MELD score (0.14, 0.11 to 0.18). Several variables were instead predictors of a shorter LOS, including male gender (-1.42, -1.93 to -0.92), acute hepatic necrosis (-2.67, -3.80 to -1.54), exception MELD points for HCC (-1.89, -2.56 to -1.21), and living donor (-2.50, -1.27 to -3.74). One covariate, time on transplant list (0.0005, 0.00045 to 0.001) achieved statistical significance, but had an estimate coefficient of minimal clinical significance. Survival analysis Kaplan-Meier survival with log-rank analysis was performed using the groups of patients at low, moderate, and high risk for LOS. Those subjects at high risk for LOS had the worst predicted survival (figure 1). Based on the slope of these curves, this increase in graft failure and mortality risk is most pronounced within the first year after transplant. Payment factors associated with hospital LOS Multivariable analysis Each non-private source of primary payment predicted longer LOS, including Medicare/Medicaid (1.24, 0.84 to 1.85), and Veterans Administration (VA) (3.48, 1.84 to 5.13). Medicare/Medicaid as secondary payment source was also a predictor of longer LOS (1.46, 0.38 to 2.54) (table 4). Donor factors associated with hospital LOS Univariable analysis Donor covariates that emerged from univariable analysis included male gender, living donor, unknown extended criteria donor status, donor weight and height, AST, unknown clinical infection status, and right lobe-only graft, each of which was predictive of a shorter LOS (table 5). Hispanic donor race, non-heart beating donor, regional or national organ sharing, donor height 20% greater than recipient height, The HALOS model P a g e | 11 transplanted left lobe only, ABO incompatible or compatible but not identical, and cold ischemia time were all donor covariates emerging from univariable analysis as predictors of longer LOS. Multivariable analysis Donor covariates that emerged as predictors of longer LOS included non-heart beating donor (3.40, 2.23 to 4.60) and national organ sharing (1.39, 0.34 to 2.44) (table 5). Additionally, CIT emerged as a predictor of longer LOS (0.36, 0.29 to 0.44), independent of national organ sharing, and there was less than a 30% correlation between CIT and sharing area. Donor serum creatinine in mg/dl (0.24, 0.09 to 0.40) and donor age (0.04, 0.02 to 0.05) were statistically significant predictors but had estimate coefficients of minimal clinical significance. Left (6.04, 1.8 to 10.2) and right (2.56, 0.22 to 4.91) transplanted lobes in split graft surgeries were predictive of longer LOS, as was donor HCV-positive status (1.44, 0.03 to 2.85), all with wide confidence intervals. Posttransplant events Univariable and multivariable analysis ACR episode during the transplant admission emerged as a predictor of longer LOS on univariable analysis, whether treated or untreated (table 5). After controlling for the identified recipient, payment, and donor predictors, any ACR emerged as an independent predictor of longer LOS in multivariable analysis (8.20, 7.24 to 9.18). Models Comparison Comparing predicted and actual LOS of the validation set, Model 1 (recipient factors only) yielded a correlation coefficient of 0.9182 and an R-square value of 0.1107 when predicted and actual LOS of the validation set were compared. Model 1 ROC curves for the high, moderate, and low risk groups had AUC values of 0.73, 0.55, and 0.68 respectively. Models 2 through 4 were predictive of LOS to a similar degree, with respective correlation coefficients of 0.9170, 0.9120, and 0.9077, and respective R-square values of 0.113, 0.116, and 0.120. ROC curves constructed from Model 2 (recipient factors and payment source) were no different than Model 1, with the same AUC values for each respective risk group. Model 3 (recipient, payment, and donor factors) ROC The HALOS model P a g e | 12 curves had slightly better AUC values of 0.74, 0.56, and 0.70 for the high, moderate, and low risk groups respectively. Additionally, Model 4 (recipient, payment, donor, and postoperative factors) ROC curves slightly improved upon Model 3, with AUC values of 0.75, 0.57, and 0.71 respectively. DISCUSSION We began this study mindful of the mounting pressure on liver transplant centers to optimize costs. Through retrospective analysis of the large, multicenter UNOS STAR files, we sought to create a mathematical model for estimating the risk of prolonged hospitalization, a driver of higher costs to the transplant center. The current study was conducted in stages focused on recipient, payment, donor, and posttransplant factors, yielding models on which to base decisions at each stage of the transplantation process. The HALOS model can first add valuable information during recipient selection, when in reality financial considerations loom large. Among the four models derived in this study, the two models that are based only on information available during recipient selection - Models 1 and 2 - were nearly as accurate as Models 3 and 4 in projecting validation set patients into the three risk groups. Importantly, this means that Models 1 and 2 can be used by transplant centers at the recipient selection stage to predict postoperative LOS, before donor or postoperative information is known. Using the HALOS model calculator, patients can therefore be categorized as being at low (≤8 days), moderate (>8 to ≤18 days), or high risk (>18 days) for prolonged LOS, based on information available at any stage of the transplantation process. The calculator is available for free use at http://cbatl.surgery.washington.edu/, to allow providers to assess LOS risk for potential LT recipients. This ability to identify patients at high risk of a prolonged hospitalization can solve an important problem. Transplant centers are at increased financial risk since the advent of the MELD era in 2003, during which organ allocation has appropriately favored the sickest patients [7]. With their financial viability heavily dependent on hospitalization profit margins [1], transplant centers have struggled to adequately curb their financial risk by identifying the cases most likely to become costly outliers. The expense of these cases is usually driven by LOS. Attempting to control their financial exposure, transplant centers are forced to require “high risk” patients to first acquire the broadest possible insurance coverage before proceeding to LT. The difficulty comes The HALOS model P a g e | 13 with identification of these high risk cases, an endeavor fraught with guesswork. The unfortunate reality is that these insurance issues can cause a delay in transplantation, and some patients cannot afford this delay. Our hope is that the HALOS model, more precisely tailored toward identifying such high risk cases prior to LT, can help. The HALOS model best achieves accuracy when identifying patients at either high or low risk of prolonged LOS, rather than moderate risk. Identification of patients at low risk may allow transplant centers to allow these patients to proceed to LT, without delay, with lesser insurance coverage. Transplant centers can then direct efforts to limit financial risk, a necessary endeavor, specifically towards those patients identified as high risk by the HALOS model. All four models are most accurate when used to identify those patients who are at highest risk for prolonged LOS (AUC of 0.73, 0.73, 0.74, and 0.75 for Models 1 through 4, respectively). Each model was also accurate in identifying patients at low risk of prolonged LOS (AUC of 0.68, 0.68, 0.70, and 0.71 for Models 1 through 4, respectively). The models were not as accurate in identifying the moderate risk group. The HALOS model can next be useful during donor selection. Recipient LOS categorization may guide transplant surgeons in choosing donor organs. For example, they may choose to decline organs from donors who confer high risk for LOS on behalf of recipients already at high or moderate risk for prolonged LOS. Indeed, a recent study by Salvalaggio et al. found higher DRI and MELD scores to have a synergistic impact on transplant-related costs [11]. This means, though the survival benefit of high DRI donors appears to be limited to recipients with high MELD scores [12, 13], that this particular donor-recipient pairing leads to expensive transplantations. Most recipient factors that emerged as predictors of LOS were unsurprising. Several factors associated with an increased LOS are seen in clinically decompensated patients, including ascites, encephalopathy, TIPS, higher laboratory MELD scores, life support, and hospital- or ICU-bound status [14]. Others likely predict a more complicated surgery, including previous abdominal surgeries or transplants and simultaneous transplantation of other organs. Recipient diabetes predicted a longer LOS, likely related to an increased risk for wound healing, infectious complications, and cardiovascular events [15]. Increasing age, which also predicted a longer LOS, likely The HALOS model P a g e | 14 diminishes the overall ability to recover from the stresses associated with major surgery [16]. Fewer donor factors emerged as predictors. Organ sharing on a national basis, compared with local sharing, was predictive of a longer LOS. Increasing CIT, representing a risk of increased physiological damage, was also associated with a longer LOS [17]. Interestingly, though, national organ sharing did not strongly correlate with a longer CIT. Donor livers that are shared on a national basis have usually already been assessed and declined by several closer transplant teams. Therefore, organs that are eventually shared on a national basis may be of inferior quality, potentially causing problems with the transplantation (such as primary graft dysfunction) and producing a longer LOS. The prolonged LOS with nationally shared organs should be carefully considered in proposed national organ allocation policies. Similarly, DCD donors were predictive of longer LOS, perhaps related to their association with increased graft failure and biliary complications [18-22]. Split liver grafts, both right and left lobes, were associated with prolonged LOS. Previous studies using (like the current study) pooled registry data [23, 24], in contrast to studies limited to specialized centers [25-30], have shown poorer graft and patient survival with split liver transplantation than whole liver transplantation. The reasons behind the survival differences seen in pooled registry data (such as center inexperience with split grafts, predisposing to ischemic or other complications) may also affect LOS[31]. The one posttransplant factor evaluated, ACR, was also associated with an increased LOS, adding 8 hospital days. This quantitative result may further crystallize the debate about the use of immunosuppression induction agents. There exists controversy among transplant surgeons about whether to utilize these agents in the postoperative setting, revolving around their extremely high cost [32]. Surgeons commonly elect to forgo immunosuppression induction and instead to simply treat episodes of ACR that may result. With the knowledge that ACR lengthens LOS, the more cost-effective strategy may be to prevent ACR with immunosuppression induction, regardless of the initial expense. Even though other posttransplant factors like biliary stenosis and hepatic artery thrombosis are not recorded in the UNOS STAR files, each of these posttransplant factors seem to increase the LOS in our experience. Importantly, our data indicate recipients with a high risk LOS categorization also have a higher mortality risk than recipients falling into the other categories (figure 1), The HALOS model P a g e | 15 consistent with prior studies [33]. One potential criticism of this result is based on our exclusion of patients dying within 18 days of transplant in the hospital. These patients were excluded to avoid skewing the data as previously described. The question that follows: does this exclusion artificially lower the mortality rates within the low or moderate risk LOS categories? To answer this question, a post-hoc analysis was performed. The donor, recipient, and posttransplant predictors identified on multivariable analysis were found to be significantly more prevalent in the excluded early death patients than among those included patients who likewise did not have a prolonged LOS (data not shown). This finding supports our initial assumption that the excluded early death patients were not representative (in terms of LOS risk factors) of the surviving patients who also did not have a prolonged LOS. This did not hold true for one recipient LOS predictor, male gender, which was not significantly different in proportion between these two groups. Criticism can also potentially be directed towards the use of LOS as a proxy for costs, given one study that found the last days of hospitalization after trauma surgery to be the less costly than the first days [34]. However, another study found an increased risk of adverse events with each added hospital day [35]. Additionally, opportunity cost may be an important consideration, in that a prolonged LOS limits a transplant center from caring for other patients because of bed availability. This may lead to fewer operations and procedures, events which produce needed revenue. In conclusion, this study provides the first analysis of a large database identifying predictors of hospital length of stay for potential liver transplant recipients. The resultant HALOS mathematical model, with variable weighting of predictors, can serve as an important tool for transplant centers striving to better understand and optimize transplant-related costs. The HALOS model P a g e | 16 REFERENCES 1. Abecassis, M. M. (2006). Financial outcomes in transplantation--a provider’s perspective. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 6(6), 1257-63. doi:10.1111/j.1600-6143.2006.01329.x 2. Abecassis, M. (2009). Making Dollars and Sense out of Liver. Transplantation, 1159-1161. doi:10.1002/lt. 3. Axelrod, D. a, Koffron, A. J., Baker, T., Al-Saden, P., Dixler, I., McNatt, G., Sumner, S., et al. (2005). The economic impact of MELD on liver transplant centers. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 5(9), 2297-301. doi:10.1111/j.1600-6143.2005.01025.x 4. Feng, S., Goodrich, N. P., Bragg-Gresham, J. L., Dykstra, D. M., Punch, J. D., DebRoy, M. a, Greenstein, S. M., et al. (2006). Characteristics associated with liver graft failure: the concept of a donor risk index. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 6(4), 783-90. doi:10.1111/j.1600-6143.2006.01242.x 5. Buchanan, P., Dzebisashvili, N., Lentine, K. L., Axelrod, D. A., Schnitzler, M. A., & Salvalaggio, P. R. (2009). Liver Transplantation Cost in the Model for EndStage Liver Disease Era : Looking Beyond the Transplant Admission. Liver, 12701277. doi:10.1002/lt. 6. Washburn, W. K., Pollock, B. H., Nichols, L., Speeg, K. V., & Halff, G. (2006). Impact of recipient MELD score on resource utilization. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 6(10), 2449-54. doi:10.1111/j.16006143.2006.01490.x The HALOS model P a g e | 17 7. Axelrod, D. a, Schnitzler, M., Salvalaggio, P. R., Swindle, J., & Abecassis, M. M. (2007). The economic impact of the utilization of liver allografts with high donor risk index. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 7(4), 990-7. doi:10.1111/j.1600-6143.2006.01724.x 8. Data collection forms. Available at: http://www.unos.org/data/about/collection.asp. Accessed July 2011. 9. Metzger, R. a, Delmonico, F. L., Feng, S., Port, F. K., Wynn, J. J., & Merion, R. M. (2003). Expanded criteria donors for kidney transplantation. American Journal of Transplantation, 3(s4), 114-125. doi:10.1034/j.1600-6143.3.s4.11.x 10. Katz, M. (2002). Study Design and Statistical Analysis (Third Edit., p. 81). New York, NY: Cambridge University Press. 11. Salvalaggio, P. R., Dzebisashvili, N., Macleod, K. E., Lentine, K. L., Gheorghian, A., Schnitzler, M. A., Hohmann, S., et al. (2011). The Interaction Among Donor Characteristics , Severity of Liver Disease , and the Cost of Liver Transplantation. Liver Transplantation, 233-242. doi:10.1002/lt. 12. de Vera, M. E., Lopez-Solis, R., Dvorchik, I., Campos, S., Morris, W., Demetris, a J., Fontes, P., et al. (2009). Liver transplantation using donation after cardiac death donors: long-term follow-up from a single center. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 9(4), 773-81. doi:10.1111/j.16006143.2009.02560.x 13. Schaubel, D. E., Sima, C. S., Goodrich, N. P., Feng, S., & Merion, R. M. (2008). The survival benefit of deceased donor liver transplantation as a function of candidate disease severity and donor quality. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 8(2), 419-25. doi:10.1111/j.1600-6143.2007.02086.x 14. Al Sibae, M. R., & Cappell, M. S. (2011). Accuracy of MELD scores in predicting mortality in decompensated cirrhosis from variceal bleeding, hepatorenal syndrome, alcoholic hepatitis, or acute liver failure as well as mortality after non-transplant surgery or TIPS. Digestive diseases and sciences, 56(4), 977-87. doi:10.1007/s10620-010-1390-3 15. Moon, J., Barbeito, R., Faradji, R., Gaynor, J., & Tzakis, A. (2006). Negative impact of new-onset diabetes mellitus on patient and graft survival after liver transplantation: Long-term follow up. Transplantation, 82(12), 1625-8. 16. Watt, K. D. S., Pedersen, R. a, Kremers, W. K., Heimbach, J. K., & Charlton, M. R. (2010). Evolution of causes and risk factors for mortality post-liver transplant: results of the NIDDK long-term follow-up study. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 10(6), 1420-7. doi:10.1111/j.16006143.2010.03126.x 17. Colina, F. (1992). The role of histopathology in hepatic transplantation. Semin Diagn Pathol, 9(3), 200-9. The HALOS model P a g e | 18 18. Jay, C., Lyuksemburg, V., Ladner, D., Wang, E., Caicedo, J., Holl, J., Abecassis, M., et al. (2011). Ischemic cholangiopathy after controlled donation after cardiac death liver transplantation: a meta-analysis. Annals of Surgery, 253(2), 259-64. 19. Chan, E. Y., Olson, L. C., Kisthard, J. A., Perkins, J. D., Bakthavatsalam, R., Halldorson, J. B., Reyes, J. D., et al. (2008). Ischemic Cholangiopathy Following Liver Death Donors. Liver, 604-610. doi:10.1002/lt. 20. Kaczmarek, B., Manas, M. D., Jaques, B. C., & Talbot, D. (2007). Ischemic cholangiopathy after liver transplantation from controlled non-heart-beating donors-a single-center experience. Transplantation proceedings, 39(9), 2793-5. doi:10.1016/j.transproceed.2007.08.081 21. Perkins, J. D. (2009). Risk Factors for Developing Ischemic-Type Biliary Lesions After Liver Transplantation Incidence of and risk factors for ischemic- type biliary lesions following orthotopic liver Available at : Health-Related Quality of Life Scores Used to Improve Patient. Liver Transplantation, 1882-1887. doi:10.1002/lt. 22. Adam, R., Cailliez, V., Majno, P., Karam, V., McMaster, P., Caine, R. Y., O’Grady, J., et al. (2000). Normalised intrinsic mortality risk in liver transplantation: European Liver Transplant Registry study. Lancet, 356(9230), 621-7. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10968434 23. Merion, R. M. (2010). Current status and future of liver transplantation. Seminars in liver disease, 30(4), 411-21. doi:10.1055/s-0030-1267541 24. Cardillo, M., Fazio, N. D., Pedotti, P., Feo, T. D., Fassati, L. R., Mazzaferro, V., Colledan, M., et al. (2006). Split and Whole Liver Transplantation Outcomes : A Comparative Cohort Study. Organ, The, 402-410. doi:10.1002/lt. 25. Bonney, G. K., Aldouri, A., Attia, M., Lodge, P. a, Toogood, G. J., Pollard, S. G., & Prasad, R. (2008). Outcomes in right liver lobe transplantation: a matched pair analysis. Transplant international : official journal of the European Society for Organ Transplantation, 21(11), 1045-51. doi:10.1111/j.1432-2277.2008.00722.x 26. Hong, J. C., Yersiz, H., & Busuttil, R. W. (2011). Where are we today in split liver transplantation? Current opinion in organ transplantation, 16(3), 269-73. doi:10.1097/MOT.0b013e328346572e 27. Hong, J. C., Yersiz, H., Farmer, D. G., Duffy, J. P., Ghobrial, R. M., Nonthasoot, B., Collins, T. E., et al. (2009). Longterm outcomes for whole and segmental liver grafts in adult and pediatric liver transplant recipients: a 10-year comparative analysis of 2,988 cases. Journal of the American College of Surgeons, 208(5), 682-9; discusion 689-91. American College of Surgeons. doi:10.1016/j.jamcollsurg.2009.01.023 28. Humar, A., Beissel, J., Crotteau, S., Kandaswamy, R., Lake, J., & Payne, W. (2008). Whole liver versus split liver versus living donor in the adult recipient: an analysis of outcomes by graft type. Transplantation, 85(10), 1420-4. doi:10.1097/TP.0b013e31816de1a3 29. Wilms, C., Walter, J., Kaptein, M., Mueller, L., Lenk, C., Sterneck, M., Hillert, C., et al. (2006). Long-term outcome of split liver transplantation using right extended grafts in adulthood: A matched pair analysis. Annals of surgery, 244(6), 865-72; discussion 872-3. doi:10.1097/01.sla.0000247254.76747.f3 30. Schaubel, D. E., Sima, C. S., Goodrich, N. P., Feng, S., & Merion, R. M. (2008). The survival benefit of deceased donor liver transplantation as a function of candidate disease severity and donor quality. American journal of transplantation : The HALOS model P a g e | 19 official journal of the American Society of Transplantation and the American Society of Transplant Surgeons, 8(2), 419-25. doi:10.1111/j.1600-6143.2007.02086.x 31. Olthoff, K. M., Merion, R. M., Abecassis, M. M., Freise, C. E., Hulbert-shearon, T. E., & Emond, J. C. (2005). Outcomes of 385 Adult-to-Adult Living Donor Liver Transplant Recipients. Annals of Surgery, 242(3), 314-325. doi:10.1097/01.sla.0000179646.37145.ef 32. McKenna, G. J., & Klintmalm, G. B. (2011). The question of induction? Maybe not all antibodies are equal …*. Transplant international : official journal of the European Society for Organ Transplantation, 24(7), 637-9. doi:10.1111/j.1432-2277.2011.01262.x 33. Smith, J. O., Shiffman, M. L., Behnke, M., Stravitz, R. T., Luketic, V. A., Sanyal, A. J., Heuman, D. M., et al. (2009). Incidence of Prolonged Length of Stay After Orthotopic Liver Transplantation and Its Influence on Outcomes. Liver Transplantation, 273-279. doi:10.1002/lt. 34. Taheri, P. a, Butz, D. a, & Greenfield, L. J. (2000). Length of stay has minimal impact on the cost of hospital admission. Journal of the American College of Surgeons, 191(2), 123-30. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10945354 35. Hauck, K., & Zhao, X. (2011). How Dangerous is a Day in Hospital?: A Model of Adverse Events and Length of Stay for Medical Inpatients. Med Care, E pub. Table 1. Baseline recipient characteristics Characteristic Age, years Male gender BMI Ethnicity American Indian Asian Mean (SD) or Percentage 52.9 (10.2) 67.2% 28.0 (5.7) 0.5% 4.4% The HALOS model Black Hispanic Multiracial Pacific Islander White Diagnosis Acute hepatic necrosis Autoimmune disease Liver cancer Cholestatic disease Cryptogenic cirrhosis Alcohol-related cirrhosis Metabolic disease NASH Other Viral cirrhosis Blood type A/AB/B/O Medical condition at transplant Home/Hospital/ICU Primary payment Medicaid or Medicare/Other or Unknown/Private/VA Secondary payment Medicaid or Medicare/Other or Unknown/Private/VA Dialysis week prior to transplant Encephalopathy 1-2/3-4/None Ascites Mild/Moderate/None Any type of life support On ventilator Recipient diabetes None/Other or unknown/Type I/Type II Peripheral vascular disease No/Unknown/Yes Portal vein thrombosis No/Unknown/Yes Previous abdominal surgery No/Unknown/Yes TIPS presence at transplant No/Unknown/Yes Variceal bleeding prior to transplant No/Unknown/Yes Albumin – mg/dl MELD score Exception MELD points for HCC Previous transplant Number of previous liver transplants 0/1/≥2 Days waiting Liver transplant with another transplant Heart/Intestine/Kidney/Pancreas Transplant procedure Whole/Reduced or split Liver type Living left lobe Living right lobe Split/reduced left lobe Split/reduced right lobe Whole liver P a g e | 20 9.3% 12.7% 0.4% 0.1% 72.6% 5.2% 2.4% 17.2% 9.4% 6.1% 17.2% 2.6% 4.4% 5.6% 29.9% 37.2/4.9/13.3/44.6% 71.7/16.9/11.4% 34.5/2.4/61.1/2.0% 4.9/89/5.7/0.4% 9.7% 54.7/11.2/34.1% 50.7/26.7/22.6% 6.0% 5.2% 75.0/9.5/2.5/13.0% 85.9/13.2/0.9% 90.7/3.8/5.5% 55.0/4.6/40.4% 88.3/3.8/7.9% 81.6/13.9/4.5% 2.9 ± 0.7 21.2 ± 9.9 19.9% 7.2% 92.8/6.4/0.8% 247 ± 473 0.1/0.5/6.2/0.5% 95.0/5.0% 0.3% 3.5% 0.2% 1.0% 95.0% The HALOS model P a g e | 21 Table2. Donor baseline characteristics Characteristic Age, years Donor male gender Donor blood type A/AB/B/O Cause of death or living Anoxia/CNS tumor/CVA/Head trauma/Living/Other Donor ethnicity American Indian Asian Black Hispanic Multiracial Pacific Islander White Donor after cardiac arrest No/Unknown/Yes Extended criteria donor (renal definition) Donor weight – kg Donor height – cm Donor BMI Serum creatinine, mg/dl AST, mg/dl ALT, mg/dl Total bilirubin, mg/dl Diabetes of donor No Insulin dependent Non-insulin dependent Diabetes present, type unknown Unknown if diabetes present Chronic hypertension of donor No/Unknown/Yes Donor HCV infection No/Unknown/Yes Donor HBV infection No/Unknown/Yes Clinical infection of donor No/Unknown/Yes Sharing region Local/Regional/National Distance Donor to Recipient, miles Cold ischemia time, hours Donor and recipient matching ABO blood type match Identical/Compatible/Incompatible Incompatible Mean (SD) or Percentage 40.9 (17) 60.0% 36.8/3.0/11.4/48.8% 15.5/0.6/40.5/37.5/3.8/2.1% 0.3% 2.3% 15.4% 12.8% 0.5% 0.3% 68.4% 88.9/5.5/5.6% 24.9% 79.1 (10.3) 171.7 (10.7) 26.7 (5.8) 1.5 (1.6) 81 (154) 67 (148) 1 (1.3) 86.6% 3.4% 1.6% 3.1% 5.3% 68.5/0.6/30.9% 97.0/0.2/2.8% 98.8/1.0/0.2% 56.6/7.8/35.6% 72.8/21.5/5.7% 140 (247) 7.2 (3.7) 92.7/6.6/0.7% 0.7% Table 3. Hospital course Acute rejection on transplant admission No Unknown Percentage 79.3% 14.4% The HALOS model P a g e | 22 Yes, no treatment Yes, treatment 1.4% 4.9% Table 4. Recipient and payment factor univariable and multivariable analysis Variable Age, years Male gender BMI Ethnicity Asian Black Hispanic Other White Diagnosis Acute hepatic necrosis Autoimmune disease Liver cancer Cholestatic disease Cryptogenic disease Alcohol-related disease Metabolic disease Other Viral cirrhosis Medical condition at transplant Home Hospital-bound ICU-bound Dialysis week before tx Encephalopathy Grade 1-2 Grade 3-4 None Ascites Mild Moderate None Any life support Mechanical ventilation Diabetes Peripheral vascular disease No Unknown Yes Portal vein thrombosis No Unknown Yes Previous abdominal surgery No Unknown Yes TIPS presence at transplant No R 0.008 -2.93 -0.05 Univariable Analysis 95% CI p-value (-0.01 to 0.03) 0.5 (-3.39 to -2.47) < 0.0001 (-0.09 to -0.01) 0.01 R 0.13 -1.42 Multivariable Analysis 95% CI p-value (0.11 to 0.15) < 0.0001 (-1.93 to -0.92) < 0.0001 -1.26 0.25 0.66 0.70 Reference (-2.32 to -0.19) (-0.5 to 1) (0.002 to 1.32) (-2.81 to 1.41) 0.02 0.5 0.05 0.5 4.37 1.62 -3.74 -0.03 2.02 0.74 2.01 2.07 7.27 Reference (3.35 to 5.39) (0.19 to 3.05) (-4.39 to -3.09) (-0.83 to 0.77) (1.06 to 2.98) (0.09 to 1.39) (0.63 to 3.39) (0.97 to 3.16) (6.29 to 8.26) < 0.0001 0.03 < 0.0001 0.9 < 0.0001 0.02 0.004 0.0002 < 0.0001 -2.67 (-3.80 to -1.54) < 0.0001 (7.45 to 8.59) (15.93 to 17.26) (11.14 to 12.59) < 0.0001 < 0.0001 < 0.0001 4.49 7.25 3.62 (3.78 to 5.20) (6.19 to 8.30) (2.72 to 4.52) < 0.0001 < 0.0001 < 0.0001 2.03 11.78 Reference (1.57 to 2.50) (11.05 to 12.52) < 0.0001 < 0.0001 3.02 (2.18 to 3.87) < 0.0001 0.74 5.62 Reference 20.36 20.93 1.37 (0.19 to 1.28) (5.01 to 6.24) 0.008 < 0.0001 1.51 (0.94 to 2.08) < 0.0001 (19.47 to 21.25) (19.98 to 21.88) (0.87 to 1.87) < 0.0001 < 0.0001 < 0.0001 9.64 (8.35 to 10.93) < 0.0001 0.91 (0.37 to 1.46) 0.001 Reference 1.24 4.22 (0.60 to 1.88) (1.90 to 6.55) 0.0001 0.0004 Reference 1.24 4.11 (0.11 to 2.38) (3.16 to 5.06) 0.03 < 0.0001 2.33 (1.31 to 3.37) < 0.0001 Reference 2.26 2.79 (1.21 to 3.30) (2.35 to 3.24) < 0.0001 < 0.0001 0.96 (0.45 to 1.47) 0.0002 Reference 8.02 16.59 11.86 Reference The HALOS model Unknown Yes Variceal bleed prior to transplant No Unknown Yes Albumin, mg/dl MELD score Exception MELD points for HCC Number of previous LT 0 1 ≥2 Time on transplant list, days Simultaneous transplantation of another organ Heart Intestine Kidney Pancreas Living donor Primary payment Other Medicare/Medicaid VA Private Secondary payment Medicare/Medicaid Other Private P a g e | 23 1.03 2.08 (-0.10 to 2.15) (1.27 to 2.88) 0.07 < 0.0001 1.18 (0.32 to 2.05) 0.007 Reference 1.02 1.5 -1.04 0.49 -7.18 (0.39 to 1.65) (0.45 to 2.54) (-1.33 to -0.74) (0.47 to 0.51) (-7.72 to -6.65) 0.001 0.005 < 0.0001 < 0.0001 < 0.0001 0.14 -1.89 (0.11 to 0.18) (-2.56 to -1.21) < 0.0001 < 0.0001 (9.24 to 10.99) (11.47 to 16.47) (-0.001 to 0.0005) < 0.0001 < 0.0001 < 0.0001 5.40 10.34 0.0005 (4.39 to 6.42) (7.60 to 13.10) (0.00045 to 0.001) < 0.0001 < 0.0001 0.03 16.95 35.67 5.70 33.24 -1.22 (11.35 to 22.54) (32.62 to 38.71) (4.80 to 6.60) (30.23 to 36.25) (-2.34 to -0.10) < 0.0001 < 0.0001 < 0.0001 < 0.0001 0.03 18.70 34.58 (13.1 to 24.4) (31.3 to 37.9) < 0.0001 < 0.0001 2.50 (1.27 to 3.74) < 0.0001 3.84 2.22 2.50 Reference (2.40 to 5.27) (1.76 to 2.68) (0.96 to 4.04) <0.0001 <0.0001 0.002 3.75 1.24 3.48 (2.22 to 5.28) (0.84 to 1.85) (1.84 to 5.13) <0.0001 <0.0001 <0.0001 2.19 -0.33 Reference (0.86 to 3.52) (-1.26 to 0.60) 0.001 NS 1.46 (0.38 to 2.54) 0.008 Reference 10.11 13.97 -0.0009 Table 5. Donor and postoperativefactor univariable and multivariable analysis Variable Age, years Male donor Cause of death or living Anoxia CNS tumor Stroke Head trauma Living Other Donor ethnicity Asian Black Hispanic Other White Non-heart beating donor DCD donor R -0.003 -0.55 Univariable Analysis 95% CI p-value (-0.02 to 0.01) 0.6 (-0.99 to -0.11) 0.01 0.004 0.35 0.36 Reference -1.1 0.48 (-0.65 to 0.65) (-2.41 to 3.11) (-0.13 to 0.85) NS NS 0.2 (-2.27 to 0.07) (-1.05 to 2.01) 0.07 NS 0.45 0.35 2.07 0.83 Reference 2.29 (-1.01 to 1.91) (-0.26 to 0.96) (1.41 to 2.72) (-1.23 to 2.88) NS NS <0.0001 NS (1.21 to 3.37) <0.0001 R 0.04 Multivariable Analysis 95% CI p-value (0.02 to 0.05) <0.0001 3.40 (2.23 to 4.60) <0.0001 The HALOS model No Unknown Yes Extended criteria donor (renal definition) No Unknown Yes Donor weight, kg Donor height, cm Donor BMI Serum Cr, mg/dl AST, mg/dl ALT, mg/dl Total bilirubin, mg/dl Donor diabetes No Unknown Yes Chronic hypertension No Unknown Yes HCV-positive donor Negative Unknown Positive Clinical infection of donor No Unknown Yes Sharing region Local Regional National Donor distance, miles Cold ischemia time, hours ABO blood type match Identical Compatible Incompatible Transplanted lobes Left Right Whole Size mismatch Donor 20% larger Donor 20% smaller No size mismatch Transplant admission ACR Yes, no treatment Yes, treatment Unknown No P a g e | 24 Reference -0.35 -0.29 (-1.31 to 0.6) (-0.97 to 0.91) NS NS Reference -1.31 -0.36 -0.02 -0.05 -0.03 -0.02 -0.001 -0.001 -0.03 (-2.43 to -0.18) (-0.87 to 0.15) (-0.03 to -0.006) (-0.07 to -0.03) (-0.06 to 0.01) (-0.16 to 0.12) (-0.003 to 0.0002) (-0.002 to 0.0004) (-0.20 to 0.15) 0.02 0.2 0.003 <0.0001 0.2 NS 0.1 0.2 NS Reference 1.62 0.19 (-1.73 to 5.00) (-0.56 to 0.94) NS NS Reference 2.16 -0.15 (-0.64 to 4.96) (-0.61 to 0.32) 0.1 NS Reference -0.69 -0.94 (-5.10 to 3.70) (-2.24 to 0.36) 0.2 NS Reference -0.92 -0.02 (-1.74 to -0.09) (-0.48 to 0.44) 0.03 NS Reference 2.27 3.23 0.003 0.33 (1.74 to 2.80) (2.29 to 4.17) (0.002 to 0.004) (0.27 to 0.39) <0.0001 <0.0001 <0.0001 <0.0001 Reference 3.97 5.46 (3.10 to 4.80) (2.73 to 8.18) <0.0001 <0.0001 4.48 -1.50 Reference (1.57 to 7.38) (-2.56 to -0.46) 0.002 0.005 4.67 0.67 Reference (2.07 to 7.27) (-2.08 to 3.43) 0.0004 NS 9.51 8.54 0.68 Reference (7.70 to 11.33) (7.54 to 9.54) (0.07 to 1.30) <0.0001 <0.0001 0.03 0.24 (0.09 to 0.40) 0.002 1.44 (0.03 to 2.85) 0.05 1.39 (0.34 to 2.44) 0.01 0.36 (0.29 to 0.44) <0.0001 6.04 2.56 (1.80 to 10.20) (0.22 to 4.91) 0.005 0.03 8.20 (7.24 to 9.18) <0.0001 The HALOS model P a g e | 25 Figure 1. Patient survival by LOS group. Kaplan-Meier survival with log-rank analysis was performed using the groups of patients at low, moderate, and high risk for LOS. Those subjects at high risk for LOS had the worst predicted survival. Based on the slope of these curves, this increase in graft failure and mortality risk is most pronounced within the first year after transplant.