INFLUENZA VACCINE VACCINATION OF PRETERM INFANTS In
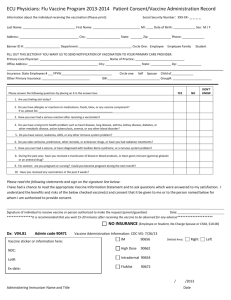
advertisement

INFLUENZA VACCINE VACCINATION OF PRETERM INFANTS In the majority of cases, infants born prematurely, regardless of birth weight, should be vaccinated at the same chronological age and according to the same schedule and precautions as full-term infants and children. Birth weight and size are not factors in deciding whether to postpone routine vaccination of a clinically stable preterm infant, except for hepatitis B (HepB) vaccine. The full recommended dose of each vaccine should be used. Divided or reduced doses are not recommended. Decreased seroconversion rates might occur among certain preterm infants with low birth weights (ie, less than 2,000 g) after administration of HepB vaccine at birth. However, by chronological age 1 month, all preterm infants, regardless of initial birth weight, are as likely to respond as adequately as older and larger infants. Preterm infants born to hepatitis B surface antigen (HBsAg)-positive mothers and mothers with unknown HBsAg status must receive immunoprophylaxis with HepB vaccine within 12 hours after birth. The initial vaccine dose should not be counted towards completion of the HepB vaccine series, and 3 additional doses of HepB vaccine should be administered, beginning when the infant is age 1 month. Attempts should be determine the HBsAg status of mothers with unknown HBsAg status, and unless the mother is found to be HBsAg negative, the infant should receive hepatitis B immunoglobulin (HBIG) with 12 hours of birth. Preterm infants weighing less than 2,000 g and born to HBsAg-negative mothers should receive the first dose of the HepB series at chronological age 1 month or at hospital discharge. If a child is at least 6 weeks old and has been hospitalized since birth, the rotavirus vaccine should be deferred until the time of discharge. The rotavirus vaccine series should not be initiated for infants 15 weeks old or older. BREASTFEEDING AND VACCINATION Neither inactivated nor live vaccines administered to lactating women affect the safety of breastfeeding for mothers or infants. Breastfeeding does not adversely affect immunization and is not a contraindication for any vaccine, with the exception of smallpox vaccine. Yellow fever vaccine should be avoided in breastfeeding women, unless travel to areas endemic for yellow fever cannot be avoided or postponed. Limited data indicate that breastfeeding can enhance the response to certain vaccine antigens. Breastfed infants should be vaccinated according to routine recommended schedules. Although live vaccines multiply within the mother's body, the majority have not been demonstrated to be excreted in human milk. Although rubella vaccine virus might be excreted in human milk, the virus usually does not infect the infant. If infection does occur, it is well-tolerated because the virus is attenuated. Inactivated, recombinant, subunit, polysaccharide, conjugate vaccines and toxoids pose no risk for mothers who are breastfeeding or for their infants. VACCINATION DURING PREGNANCY Risk to a developing fetus from vaccination of the mother during pregnancy is theoretical. No evidence exists of risk from vaccinating pregnant women with inactivated virus or bacterial vaccines or toxoids. Live vaccines pose a theoretical risk to the fetus; live-attenuated virus and liver bacterial vaccines are generally contraindicated during pregnancy. Benefits of vaccinating pregnant women usually outweigh potential risks when the likelihood of disease exposure is high, when infection would pose a risk to the mother or fetus, and when the vaccine is unlikely to cause harm. Pregnant women who had the last dose of tetanus-toxoid-containing vaccine more than 10 years ago should generally receive Td rather than tetanus, reduced diphtheria, acellular pertussis (Tdap), even though Tdap is not contraindicated in pregnancy. A dose of Td during pregnancy ensures adequate tetanus immunity in the mother and prevents disease in both mother and infant. In specific situations, the dose of Td can be withheld if the provider is confident the pregnant woman is immune to tetanus. Regardless of a recent Td vaccination, pregnant women who have not already received Tdap should receive a dose of Tdap as soon as possible after delivery to ensure pertussis immunity and reduce the risk for transmission to the newborn. Pregnant women who are not immunized or only partially immunized against tetanus should complete the primary series. Women for whom Td is indicated but who have not completed the recommended 3-dose series during pregnancy should receive follow-up after delivery to ensure the series is completed. Women in the second and third trimesters of pregnancy are at increased risk for hospitalization from influenza. Therefore, routine influenza vaccination is recommended for healthy women who will be pregnant (in any trimester) during influenza season (usually early October through late March in the United States). Inactivated poliovirus vaccine (IPV) can be administered to pregnant women who are at risk for exposure to wild-type poliovirus infection. HepB vaccine may be administered to pregnant women who have an indication for the vaccine. Hepatitis A (HepA), pneumococcal polysaccharide, meningococcal conjugate, and meningococcal polysaccharide vaccines should be considered for women at increased risk for those infections. Pregnant women who must travel to areas where the risk for yellow fever is high should receive yellow fever vaccine, because the limited theoretical risk from vaccination is substantially outweighed by the risk for yellow fever infection. Pregnancy is a contraindication for smallpox (vaccinia) vaccine and measles-, mumps-, rubella-, and varicella-containing vaccines. Smallpox vaccine is the only vaccine known to cause harm to a fetus when administered to a pregnant woman. Smallpox vaccine also should not be administered to a household contact of a pregnant woman. Unvaccinated children born to mothers vaccinated with rubella vaccine during pregnancy have had rubella antibody levels, which could represent passive transfer of maternal antibody to the fetus or a fetal antibody response to vaccine virus infection in the fetus. No cases of congenital rubella or varicella syndrome or abnormalities attributable to fetal infection have been observed among infants born to susceptible women who received rubella or varicella vaccines during pregnancy. Because of the importance of protecting women of childbearing age against rubella and varicella, reasonable practices in any immunization program include asking women if they are pregnant or intend to become pregnant in the next 4 weeks; not vaccinating women who state that they are pregnant or plan to be pregnant; explaining the theoretical risk for the fetus if MMR, varicella, or MMRV vaccine were administered to a woman who is pregnant; and counseling women who are vaccinated not to become pregnant during the 4 weeks after MMR, varicella, or MMRV vaccination. Routine pregnancy testing of women of childbearing age before administering a live-virus vaccine is not recommended. If a pregnant woman is inadvertently vaccinated or if she becomes pregnant within 4 weeks after MMR or varicella vaccination, she should be counseled regarding the theoretical basis of concern for the fetus; however, MMR or varicella vaccination during pregnancy should not be a reason to terminate pregnancy. Persons who receive MMR vaccine do not transmit the vaccine viruses to contacts. Transmission of varicella vaccine virus to contacts is rare. MMR and varicella vaccines should be administered when indicated to the children and other household contacts of pregnant women. Infants living in households with pregnant women should receive the rotavirus vaccine according to the same schedule as infants in households without pregnant women. All pregnant women should be evaluated for immunity to rubella and varicella and be tested for the presence of HBsAg in every pregnancy. Women susceptible to rubella and varicella should be vaccinated immediately after delivery. A woman known to be HBsAg-positive should be followed carefully to ensure that the infant receives HBIG and begins the HepB vaccine series 12 hours or earlier after birth and that the infant completes the recommended HepB vaccine series on schedule. No known risk exists for the fetus from passive immunization of pregnant women with immune globulin preparations Reference 1. Centers for Disease Control and Prevention : General Recommendations on Immunization. MMWR 2011; 60(2):3-. 2. Product Information: MENVEO(R) intramuscular injection solution, meningococcal [groups A, C, Y and W-135] oligosaccharide diphtheria CRM197 conjugate vaccine intramuscular injection solution. Novartis Vaccines and Diagnostics, Inc, Cambridge, MA, 2011. เวป นี ้นะhttp://www.thomsonhc.com/micromedex2/librarian/ND_T/evidencexpert/ND_PR/evidencexper t/CS/19721C/ND_AppProduct/evidencexpert/DUPLICATIONSHIELDSYNC/F4A57D/ND_PG/evidencex pert/ND_B/evidencexpert/ND_P/evidencexpert/PFActionId/evidencexpert.IntermediateToDocumen tLink?docId=9672&contentSetId=50&title=IMMUNIZATION+GUIDELINES+-+SPECIAL+SITUATIONS+- +CDC+RECOMMENDATIONS&servicesTitle=IMMUNIZATION+GUIDELINES+-+SPECIAL+SITUATIONS++CDC+RECOMMENDATIONS