11_T Cell Development - V14-Study
advertisement
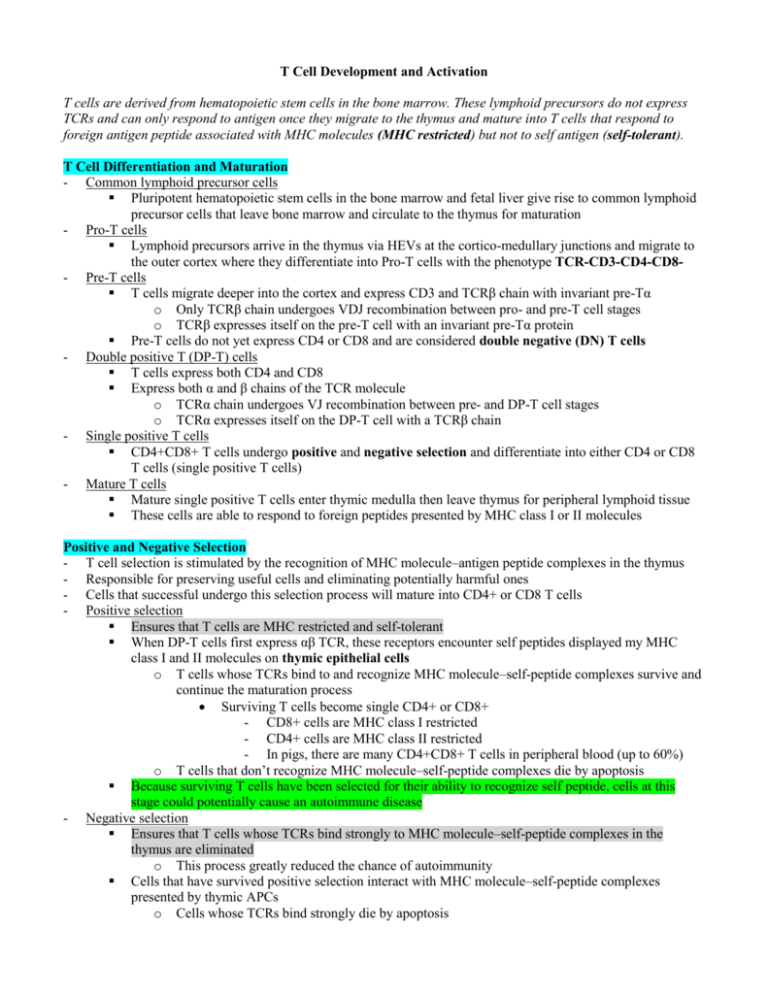
T Cell Development and Activation T cells are derived from hematopoietic stem cells in the bone marrow. These lymphoid precursors do not express TCRs and can only respond to antigen once they migrate to the thymus and mature into T cells that respond to foreign antigen peptide associated with MHC molecules (MHC restricted) but not to self antigen (self-tolerant). T Cell Differentiation and Maturation - Common lymphoid precursor cells Pluripotent hematopoietic stem cells in the bone marrow and fetal liver give rise to common lymphoid precursor cells that leave bone marrow and circulate to the thymus for maturation - Pro-T cells Lymphoid precursors arrive in the thymus via HEVs at the cortico-medullary junctions and migrate to the outer cortex where they differentiate into Pro-T cells with the phenotype TCR-CD3-CD4-CD8- Pre-T cells T cells migrate deeper into the cortex and express CD3 and TCRβ chain with invariant pre-Tα o Only TCRβ chain undergoes VDJ recombination between pro- and pre-T cell stages o TCRβ expresses itself on the pre-T cell with an invariant pre-Tα protein Pre-T cells do not yet express CD4 or CD8 and are considered double negative (DN) T cells - Double positive T (DP-T) cells T cells express both CD4 and CD8 Express both α and β chains of the TCR molecule o TCRα chain undergoes VJ recombination between pre- and DP-T cell stages o TCRα expresses itself on the DP-T cell with a TCRβ chain - Single positive T cells CD4+CD8+ T cells undergo positive and negative selection and differentiate into either CD4 or CD8 T cells (single positive T cells) - Mature T cells Mature single positive T cells enter thymic medulla then leave thymus for peripheral lymphoid tissue These cells are able to respond to foreign peptides presented by MHC class I or II molecules Positive and Negative Selection - T cell selection is stimulated by the recognition of MHC molecule–antigen peptide complexes in the thymus - Responsible for preserving useful cells and eliminating potentially harmful ones - Cells that successful undergo this selection process will mature into CD4+ or CD8 T cells - Positive selection Ensures that T cells are MHC restricted and self-tolerant When DP-T cells first express αβ TCR, these receptors encounter self peptides displayed my MHC class I and II molecules on thymic epithelial cells o T cells whose TCRs bind to and recognize MHC molecule–self-peptide complexes survive and continue the maturation process Surviving T cells become single CD4+ or CD8+ - CD8+ cells are MHC class I restricted - CD4+ cells are MHC class II restricted - In pigs, there are many CD4+CD8+ T cells in peripheral blood (up to 60%) o T cells that don’t recognize MHC molecule–self-peptide complexes die by apoptosis Because surviving T cells have been selected for their ability to recognize self peptide, cells at this stage could potentially cause an autoimmune disease - Negative selection Ensures that T cells whose TCRs bind strongly to MHC molecule–self-peptide complexes in the thymus are eliminated o This process greatly reduced the chance of autoimmunity Cells that have survived positive selection interact with MHC molecule–self-peptide complexes presented by thymic APCs o Cells whose TCRs bind strongly die by apoptosis Development of γδ T cell Populations - γδ T cells (express γδ TCR) Separate lineage of lymphocytes that arise from the same precursor as αβ TCR-expressing T cells o Mature in the thymus Play an important role in the first line of defense against pathogens (innate immune response) γδ chains are expressed in association with CD3 and ζ chains Lack CD4 but can express CD8 Do not respond to a wide range of protein antigens o Can recognize mycobacterial antigens, some heat-shock proteins, and native viral proteins Do not generally respond to MHC molecule–peptide complexes o Can respond to non-polymorphic MHC class I and CD1 molecules that present antigen Found in large number in the epidermis, intestines, lung, mammary glands, vagina, and uterus Ruminants (particularly bovine and sheep) have large populations of γδ T cells o Make up 80% of peripheral blood cells in calves o Make up 60% of neonatal peripheral blood cells in sheep o Make up 5-10% of peripheral blood cells in mice Activation and Function of CD4+ and CD8+ T cells - αβ T cells that survive positive and negative selection exit the thymus, able to be activated by antigen - Two phases of T cell-mediated adaptive immune response Activation phase o Occurs in secondary lymphoid organs (LNs, spleen) and involves naïve T cells o Naïve T cells recognize antigen presented by dendritic cells, resulting in clonal expansion and differentiation into effector and memory cells, which then exit lymphoid organs and migrate to tissues to patrol for infectious agents or neoplastic cells o Naïve T cell homing to secondary lymphoid organs Naïve T cells exit the thymus and circulate via the blood to secondary lymphoid organs - Lymphocytes preferentially entering specific tissues is called homing Naïve T cells home to LN via HEVs - Occurs in the absence of antigen and does not involve TCRs If naïve T cell is not activated by antigen, it can remain in the LN for a long time or leave, re-enter blood, and circulate to another secondary lymphoid organ o Antigen recognition by naïve T cell Antigens that invade the host via mucosal surfaces are recognized and trapped by dendritic cells capable of efficient antigen presentation to naïve T cells Dendritic cells process antigen into peptides, display them on surface MHC molecules, then migrate to regional LNs or spleen for presentation Naïve T cell encounters dendritic cell with specific antigen and becomes activated o Activation of naïve T cells T cells activation requires two sets of extracellular signals for activation Signal 1: TCR recognition of the MHC molecule–peptide complex Signal 2: Co-stimulation upon interaction of CD28 (on surface of naïve T cell) with B7-1 or B7-2 (on the surface of the dendritic cell) - Enhances cell survival by increasing expression of anti-apoptitic proteins - Promotes production cytokine IL-2 Stimulates differentiation of naïve T cells into effector/memory cells Without second signal, CD4+ T cells die while CD8+ cells become non-responsive to further antigenic stimulation The cytokine environment of the LN at the time of T cell activation determines whether positive or negative co-stimulatory signals dominate - Positive signaling results in T cell activation - Negative signaling results in T cell inhibition Activation of T cells up-regulates additional co-stimulatory signals - CTLA-4 (CD152) provides a negative signal that inhibits T cell proliferation Effector phase o Occurs in peripheral tissues and involves effector T cells Effector T cells (CD4+ or CD8+) arrive in peripheral tissues, recognize antigen presented by either APCs or somatic cells, then perform their respective functions Effector T cells require less antigenic and co-stimulation to become activated o CD4+ effector T cells Classified based on their cytokine production and function - Th1, Th2, Th17 cells - Th17 cells were recently discovered to have important roles in chronic inflammatory diseases (MS, rheumatoid arthritis, inflammatory bowel disease) Cytokines Secreted by Th Cells CD4+ T cell Type Th1 Th2 Th17 - Cytokines Produced IFN-γ, TNF-β IL-4, IL-5, IL-13, IL-10 IL-17 Recognize antigen on APCs expressing MHC class II molecules Secrete cytokines to stimulate an immune response - Promote expansion and proliferation of activated CD8+ CTLs (Th1) - Promote activation of macrophages to kill phagocytosed microbes are neoplastic cells (Th1) - Promote maturation and differentiation of B cells to produce antibodies (Th2) o CD8+ T cells Recognize antigen on APCs/infected somatic cells expressing MHC class I molecules - Generally, CD8+ T cells recognize antigen synthesized in the cell cytoplasm Differentiate into Tc cells (CTLs) that function to kill infected or neoplastic target cells - Secrete perforin and granzymes that induce apoptosis of infected cell Apoptosis involves segmental DNA fragmentation, nuclear blebbing, cell morphology changes CD8+ T cells mediate apoptosis through interaction of CD95L (on surface of the T cell) and CD95 (on surface of target cell) Produce cytokines (particularly IFN-γ) to amplify local inflammation o Memory T cells Long-lived, expanded population of CD4 of CD8 T cells Accumulate with age - More than half of the T cells in an adult are memory cells Functionally quiescent until re-exposure to antigen Respond rapidly to subsequent antigen encounters and differentiate into effector cells High levels of CD44 on the cell surface promotes migration to peripheral sites of infection and inflammation Antigen-specific CD4 and CD8 cell numbers increase during the course of an immune response Before antigen exposure, the frequency of naïve T cells specific for any antigen is ~1 in 105 After antigen exposure, the frequency of T cell specific for that antigen vastly increases o 1 in 10 for CD8+ T cells o 1 in 100 (or 1000) for CD4+ T cells After the specific antigen is cleared, the immune response wanes and the number of lymphocytes specific for that antigen declines to ~1 in 104 o Remaining cells taking on a memory cell phenotype Alternate mechanisms of T cell activation Mitogens Stimulate the proliferation of lymphocyte clones without normal antigen processing and presentation Laboratory examples o Conconavalin A, phytohemagglutinin – activate T cells o Pokeweed mitogen – activates T and B cells o Lipopolysaccharide (LPS) – activated B cells - Superantigens Produced by bacteria, mycoplasms, and viruses Recognized by T cells without being processed and presented by MHC Activate T cells with a particular Vβ region, irrespective of the Vα region of the TCR o Activate T cells irrespective of antigen specificity Stimulate 2-20% of all T cells, resulting in massive production of cytokines by CD4+ T cells o Results in systemic toxicity and suppression of adaptive immune response Laboratory examples o Staphylococcal infections Bunmblefoot disease in chickens raised in cages Sorehock in rabbits o Streptococcus (rheumatic fever, shock) o Cytomegalovirus o Epstein Barr viruses