OGD information sheet - Dr Laksh Ayaru
advertisement

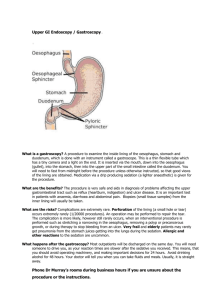
Dr Laksh Ayaru, Bsc MBBS (hons) MRCP PhD Consultant Gastroenterologist Charing Cross Hospital Hammersmith Hospital Highgate Hospital Fulham Palace Road London W6 8RF Du Cane Road London W12 0HS 17-19 View Road Highgate London N6 4DJ Tel: 07586 903 741 Fax: 020 8 866 3620 What is a gastroscopy? Gastroscopy (also known as ‘OGD’ and upper endoscopy) is a visual examination of the lining of the oesophagus (gullet), stomach and duodenum (small intestine). An endoscope (long, flexible tube) is passed through your mouth and down into your throat. Using the light on the end of the endoscope, the doctor is able to look for any abnormalities that may be present. If necessary, biopsies (small samples of tissue) may be taken during the examination and sent to the laboratory for further investigation. Gastroscopy helps your doctor check symptoms of persistent upper abdominal pain, nausea (feeling sick), vomiting and difficulty in swallowing. It is also used for finding the cause of bleeding from the upper gastrointestinal tract. As your stomach needs to be empty for the gastroscopy, you must not eat or drink anything for 6 hours before your appointment. Failure to follow these instructions may result in your gastroscopy being cancelled. Please note You can choose to have this procedure done either with a local anaesthetic spray to numb your throat, or with conscious sedation, where intravenous drugs are used to make you relaxed and/or drowsy. It is different from general anaesthetic as it does not ‘knock you out’ completely and you are still able to respond to your doctor or nurse. Most people have little or no recall of the procedure afterwards. The advantages of having the throat spray are: You can go home immediately after the test. You do not need a relative or friend to take you home. You will be able to drive yourself home after the test. You can return to work after the test. If you choose to have sedation, you must arrange for a relative or friend to take you home approximately 1 hour after the test. This person should be 18 years of age or older. It is recommended that someone stays with you for 12 hours after your procedure. You will not be able to drive or operate any machinery for the remainder of the day and will need to rest quietly at home. Please note that your appointment will be cancelled on the day if you wish to have sedation but have not organised an escort home. Are there any alternatives to gastroscopy? The principal alternative to the test is a ‘barium meal’ x-ray. During this procedure, you drink a special liquid (barium) which allows images (pictures) of your stomach to be seen using x-rays. It is less accurate than gastroscopy at detecting inflammation, ulcers and tumours of the oesophagus, stomach and duodenum. Unlike endoscopy, barium meal does not allow for biopsies to be taken for examination in the laboratory. Please note A ‘capsule endoscopy’ (where a pill-sized video capsule is swallowed) is not a substitute for this type of gastroscopy, as it does not give adequate pictures of either the oesophagus or the stomach and biopsies cannot be taken. Are there any risks associated with gastroscopy? Although complications can occur, they are rare. There is a 0.2% risk of the following occurring after endoscopy: Bleeding, which may require a blood transfusion. Reaction to the sedatives, if used during the test. Perforation (tearing) of the lining of the gastrointestinal tract, which may require surgery to repair. ‘Aspiration pneumonia’ - inflammation of the lungs, caused by inhaling the contents of the stomach. This is why it is important that you follow the instructions about not eating or drinking before the test. Disturbance of crowned teeth or dental bridgework. It is important that you tell us any crowns or bridgework before we start the test. The risk of complications may be increased if treatments such as stretching a narrow area are required, or if you have any pre-existing heart or lung conditions. Your doctor will discuss any increased risks with you before you have the test. Is there anything I should do to prepare for my appointment? If you choose to have sedation, you will not be able to go home by yourself afterwards – a friend or relative who is 18 years of age or older must escort you. It is recommended that someone stays with you for 12 hours after your procedure. Please make sure that you will have access to a telephone when you return home. If you have not been able to make these arrangements, please speak to the nursing staff. We cannot do the test with conscious sedation on this day if you do not have an escort. Please contact us at least 2 weeks before your appointment if you are on any blood-thinning medications, such as warfarin or aspirin, as you may need to stop taking them for a few days before the test. Please also contact us at least 2 weeks before your appointment if you are taking Clopidogrel (Plavix), as you may need to stop taking it for a minimum of 10 days before the test. Preparation for the test involves not having anything to eat or drink for 6 hours before your appointment time. If you are diabetic, you should contact your GP or your Diabetes Nurse Specialist for advice before your appointment. 2 weeks before your appointment Unless you have been told otherwise, please stop taking ‘Losec’ (Omeprazole) ‘Zoton’ (Lansoprazole) ‘Protium’ (Pantoprazole) ‘Pariet’ (Rabeprazole) ‘Nexium’ (Esomeprazole) ‘Tagamet’ (Cimetidine) ‘Zantac’ (Ranitidine) ‘Axid’ (Nizatidine) ‘Pepcid’ (Famotidine) The day before the test As an empty stomach allows for the best and safest examination, please do not have anything to eat or drink (not even sweets or chewing gum) for at least 6 hours before your appointment. What happens on the day of the test? If you regularly take medicines in the morning, you should take them before 7.00am on the day of the test, with a small sip of water if necessary, unless you have been advised otherwise. We advise you to wear loose-fitting clothes to your appointment, as during the procedure, the doctor will introduce air into your bowel/ stomach (see below), which may cause bloating afterwards. The bloating will go down, but if you are wearing tight-fitting or tailored clothes, this may increase any initial discomfort you experience. The gastroscopy will be done as close to your appointment time as possible. Every effort is made to keep waiting times to a minimum, but it is not possible to predict how long individual procedures will take. You may wish to bring something to read with you. The procedure will be discussed with you in detail and you will be asked to sign a consent form. This is to make sure that you understand the risks and benefits of having the test. You will be asked to remove any dentures and glasses in the examination room. We will ask you to lie on your left side on a trolley, with your knees slightly bent. If you chose to have the local anaesthetic throat spray, this will be sprayed onto your throat. If you chose to have sedation, you will have an intravenous cannula/drip inserted. You will be connected to a monitor, which will record your blood pressure and pulse throughout the procedure. Oxygen will be given to you through your nose. The conscious sedation will then be given to you. A small probe will be placed on your finger to monitor your pulse and blood oxygen level. A mouth guard will be placed in your mouth to protect your teeth. The doctor will then place the endoscope (long, flexible tube) in your mouth and pass the tube down your throat and into your stomach. Introduction of air will help him/ her to see inside your stomach and duodenum. If any saliva collects in your mouth, the nurse will clear it with a small suction tube similar to that used by dentists. If the doctor thinks an area needs further investigation, s/he might pass an instrument through the endoscope to obtain a biopsy or cytology (sample of the lining of the gastrointestinal tract) for testing in the laboratory. These tests are used to diagnose many conditions and your doctor may request one even if s/he does not suspect cancer. For example, your doctor may use a biopsy to test for Helicobacter pylori, the bacterium that causes ulcers. Gastroscopy can also be done to treat conditions of the upper gastrointestinal tract by passing instruments through the endoscope. For example, your doctor might stretch a narrowed area or treat bleeding with little or no discomfort. Your doctor will discuss any such treatment with you in detail before the test. The endoscope will not interfere with your breathing or cause you any pain. Most patients consider the test to be only slightly uncomfortable. Endoscopy can take up to a maximum of 15 minutes to complete. What happens after the test? If you chose to have the throat spray, you will be able to go home almost immediately afterwards. You should not have anything to eat or drink for half an hour after the test, as your throat may still be numb from the anaesthetic. If you chose to have sedation, you will be left to rest for about an hour before you can go home, accompanied by your escort. Once you are fully awake, you will be able to have something to eat and drink. When will I get the results? In many cases, the results are available immediately after the test. However, biopsy results may take at least a week before they are available. Details of the results and any necessary treatment will be discussed with you at your next clinic appointment. Is there anything I need to watch out for at home? It is normal to experience bloating and mild abdominal discomfort for a few days after having a gastroscopy If you have any severe pain, black tarry stools or persistent bleeding in the hours or days after your gastroscopy, please either contact Dr Ayaru, your GP or telephone switchboard of your local hospital, You may experience a feeling of pressure, bloating or cramping during or after the procedure due to the air that was introduced. This will disappear quickly once you have passed wind. Please do not worry if you have a sore throat for the rest of the day. This is normal and will pass. When can I get back to normal? If you chose to have the throat spray, you may be able to return to work and all your usual activities half an hour after your endoscopy. If you chose to have sedation, you must have a friend or relative (18 years of age or older) to escort you home. It is recommended that someone stay with you for 12 hours after your procedure. For the rest of the day, you must not: drive or operate machinery (including kitchen equipment). drink alcohol. sign any important or legal documents. You should be able to return to work and all your usual activities the day after your appointment.