Reduce Harm Breakout Group
advertisement

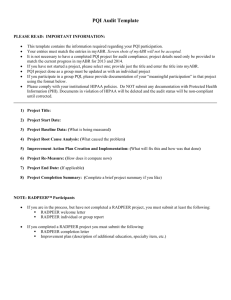
Reduce Harm Breakout Group What is Harm? The National Quality Forum’s definition of harm is: Any physical or psychological injury or damage to the health of a person, including both temporary and permanent injury. How is Harm Identified? Voluntary reporting Patient safety reports. UF&Shands uses IDinc to report and track patient safety events. A high percent of harms are not reported which are believed to be a result of the reporting systems, time constraints, fear of reprisal, shame, lack of feedback, etc. Administrative data sets Captured through ICD-9 codes and demographic data in the medical record. Benefit from objective criteria but limited by quality of documentation and coding as well as lack of contextual clinical information. Able to determine rates. Trigger tools Captured through medical record audit. Triggers are clues for possible harm. Further investigation into harm (and degree) is required. Able to trend rates. Recognized Harm Measures: NQF Serious Reportable Events Surgical Events Surgery performed on the wrong body part Surgery performed on the wrong patient Wrong surgical procedure performed on a patient Unintended retention of a foreign object in a patient after surgery or other procedure Intraoperative or immediately postoperative death in a ASA Class I patient Product or Device Events Patient death or serious disability associated with the use of contaminated drugs, devices or biologics provided by the healthcare facility Patient death or serious disability associated with the use or function of a device in patient care in which the device is used or functions other than as intended Patient death or serious disability associated with intravascular air embolism that occurs while being cared for in a healthcare facility Patient Protection Events Infant discharged to the wrong person Patient death or serious disability associated with patient elopement (disappearance) Patient suicide, or attempted suicide, resulting in serious disability while being cared for in a healthcare facility Care Management Events Patient death or serious disability associated with a medication error (e.g. errors involving the wrong drug, wrong dose, wrong patient, wrong time, wrong rate, wrong preparation or wrong route of administration) Patient death or serious disability associated with a hemolytic reaction due to the administration of ABO/HLA – incompatible blood or blood products Maternal death or serious disability associated with labor or delivery in a low-risk pregnancy while being cared for in a healthcare facility Patient death or serious disability associated with hypoglycemia, the onset of which occurs while the patient is being cared for in a healthcare facility Death or serious disability (kernicterus) associated with failure to identify and treat hyperbilirubinermia in neonates Stage 3 or 4 pressure ulcers acquired after admission to a healthcare facility Patient death or serious disability due to spinal manipulative therapy Artificial insemination with the wrong donor sperm or wrong egg Environmental Events Patient death or serious disability associated with an electric shock while being cared for in a healthcare facility Any incident in which a line designated for oxygen or other gas to be delivered to a patient contains the wrong gas or is contaminated by toxic substances Patient death or serious disability associated with a burn incurred from any source while being cared for in a healthcare facility Patient death or serious disability associated with a fall while being cared for in a healthcare facility Patient death or serious disability associated with the use of restraints or bedrails while being cared for in a healthcare facility Criminal Events Any instance of care ordered by or provided by someone impersonating a physician, nurse, pharmacist, or other licensed healthcare provider Abduction of a patient of any age Sexual assault on a patient within or on the grounds of a healthcare facility Death or significant injury of a patient or staff member resulting form a physical assault (i.e. battery) that occurs within or on the grounds of a healthcare facility AHRQ Patient Safety Indicators EXP 01 Rate of Complications of Anesthesia EXP 02 Obstetric Trauma Rate - Cesarean Delivery PSI 02 Death in Low-Mortality Diagnosis Related Groups (DRGs) PSI 03 Pressure Ulcer Rate PSI 04 Death among Surgical Inpatients PSI 05 Foreign Body Left During Procedure PSI 06 Iatrogenic Pneumothorax Rate PSI 07 Central Venous Catheter-Related Blood Stream Infection PSI 08 Postoperative Hip Fracture Rate PSI 09 Postoperative Hemorrhage or Hematoma Rate PSI 10 Postoperative Physiologic and Metabolic Derangement Rate PSI 11 Postoperative Respiratory Failure Rate PSI 12 Postoperative PE or DVT Rate PSI 13 Postoperative Sepsis Rate PSI 14 Postoperative Wound Dehiscence Rate PSI 15 Accidental Puncture or Laceration Rate PSI 16 Transfusion Reaction Volume PSI 17 Birth Trauma Rate―Injury to Neonate PSI 18 Obstetric Trauma Rate―Vaginal Delivery With Instrument PSI 19 Obstetric Trauma Rate-Vaginal Delivery wo Instrument PSI 21 Rate of Foreign Body Left During Procedure AHRQ Pediatric Quality Indicators NQI 01 Neonatal Iatrogenic Pneumothorax Rate NQI 02 Neonatal Mortality Rate NQI 03 Neonatal Blood Stream Infection Rate PDI 01 Accidental Puncture or Laceration Rate PDI 02 Pressure Ulcer Rate PDI 03 Foreign Body Left During Procedure PDI 05 Iatrogenic Pneumothorax Rate PDI 06 Pediatric Heart Surgery Mortality Rate PDI 07 Pediatric Heart Surgery Volume PDI 08 Postoperative Hemorrhage or Hematoma Rate PDI 09 Postoperative Respiratory Failure Rate PDI 10 Postoperative Sepsis Rate PDI 11 Postoperative Wound Dehiscence Rate PDI 12 Central Venous Catheter-Related Blood Stream Infection Rate PDI 13 Transfusion Reaction Volume PDI 14 Asthma Admission Rate PDI 15 Diabetes Short-term Complications Admission Rate PDI 16 Gastroenteritis Admission Rate PDI 17 Perforated Appendix Admission Rate PDI 18 Urinary Tract Infection Admission Rate AHRQ Prevention Quality Indicators PQI 01 Diabetes Short-term Complications Admissions Rate PQI 02 Perforated Appendix Admission Rate PQI 03 Diabetes Long-term Complications Admission Rate PQI 05 COPD or Asthma in Older Adults Admission Rate PQI 07 Hypertension Admission Rate PQI 08 Heart Failure Admission Rate PQI 09 Low Birth Weight Rate PQI 10 Dehydration Admission Rate PQI 11 Bacterial Pneumonia Admission Rate PQI 12 Urinary Tract Infection Admission Rate PQI 13 Angina without Procedure Admission Rate PQI 14 Uncontrolled Diabetes Admission Rate PQI 15 Asthma in Younger Adults Admission Rate PQI 16 Rate of Lower-Extremity Amputation Diabetes Hospital Acquired Conditions Foreign Object Retained After Surgery Air Embolism Blood Incompatibility Stage III and IV Pressure Ulcers Falls and Trauma Fractures Dislocations Intracranial Injuries Crushing Injuries Burn Other Injuries Manifestations of Poor Glycemic Control Diabetic Ketoacidosis Nonketotic Hyperosmolar Coma Hypoglycemic Coma Secondary Diabetes with Ketoacidosis Secondary Diabetes with Hyperosmolarity Catheter-Associated Urinary Tract Infection (UTI) Vascular Catheter-Associated Infection Surgical Site Infection, Mediastinitis, Following Coronary Artery Bypass Graft (CABG): Surgical Site Infection Following Bariatric Surgery for Obesity Laparoscopic Gastric Bypass Gastroenterostomy Laparoscopic Gastric Restrictive Surgery Surgical Site Infection Following Certain Orthopedic Procedures Spine Neck Shoulder Elbow Deep Vein Thrombosis (DVT)/Pulmonary Embolism (PE) Following Certain Orthopedic Procedures: Total Knee Replacement Hip Replacement Mortality Rates Infection Rates Central Line Associated Blood Stream Infection Catheter Associated Urinary Tract Infection Ventilator Associated Pneumonia Surgical Site Infections Clostridium Difficile Vancomycin Resistent Enterococcus Discipline Specific Complications Known risks for interventions Medication Related Harm Available Harm Reports UHC Quality and Safety Report AHCA/CMS – publicly reported and delayed Patient Safety Reports How are We Working to Reduce Harm? Root Cause Analysis of serious events Review and respond to patient safety reports Morbidity & Mortality Conferences Review of AHRQ PSIs/PQIs, and HACs Mortality Review Performance Improvement Teams Current Harm Metrics