IRB SOPs - University of South Alabama
advertisement

IRB
INSTITUTIONAL REVIEW BOARD
HUMAN SUBJECTS PROTECTION PROGRAM
STANDARD OPERATING PROCEDURES
REVISED: 2015
University of South Alabama
Table of Contents
Page #
INTRODUCTION ................................................................................................................................1
CONTACT INFORMATION ...................................................................................................................2
PRINCIPLES, ROLES AND RESPONSIBILITIES
1.0
Regulatory and Ethical Mandate .................................................................................................................... 3
1.1
The Nuremberg Code........................................................................................................................... 3
1.2
The Declaration of Helsinki ................................................................................................................... 3
1.3
The Belmont Report .............................................................................................................................. 3
1.4
Department of Health and Human Services (DHHS) Regulations ................................................ 4
1.5
Federal Policy (Common Rule) for the Protection of Human Subjects. Food and Drug
Administration (FDA) Regulations at 21 CFR 50 and 56 ................................................................. 4
1.6
Federalwide Assurance ........................................................................................................................ 4
2.0
IRB Mission and Authority ................................................................................................................................... 5
2.1
2.2
2.3
2.4
IRB Purpose.............................................................................................................................................. 5
Definition of Human Subjects Research ........................................................................................... 6
2.3.1 Research .................................................................................................................................... 7
Agreements to provide IRB review of research conducted by unaffiliated investigators ...... 7
Human Research Activities Performed at Other Institutions ......................................................... 7
2.4.1 Requirements for Approval of Research at Non-USA Facilities ....................................... 7
2.4.2 IRB Approval of Research to be Done at a Non- USA Institution ................................... 8
IRB ORGANIZATION AND ADMINISTRATION
3.0
IRB membership .................................................................................................................................................. 8
3.1
3.2
3.3
3.4
3.5
3.6
3.7
3.8
3.9
Chairperson responsibilities ................................................................................................................. 9
Vice-Chair(s) responsibilities ................................................................................................................ 9
Committee member appointment ................................................................................................... 9
Non-voting members ........................................................................................................................... 9
Termination of appointment .............................................................................................................10
Confidentiality agreement .................................................................................................................10
Orientation and training of IRB members ....................................................................................... 10
Member conflict of interest ............................................................................................................... 10
Investigator conflict of interest .......................................................................................................... 10
3.0.1
Duties of IRB Members ...................................................................................................................... 10
4.0
IRB Administrative Support .............................................................................................................................. 11
4.1
Education and training of staff ........................................................................................................ 11
4.2
Investigator and Key Research Personnel Training ....................................................................... 12
5.0
IRB Record keeping and Reporting .............................................................................................................. 12
5.1
Documentation and Retention of IRB documents ...................................................................... 13
5.2
5.4
6.0
Access to IRB records ........................................................................................................................ 13
IRBNet Database ................................................................................................................................ 13
Meeting Materials and Documentation ....................................................................................................... 13
6.1
Meeting minutes ................................................................................................................................ 14
6.2
Review by convened IRB .................................................................................................................. 15
6.2.1 IRB review procedures .......................................................................................................... 15
6.2.2
IRB meeting materials .............................................................................................. 16
6.3
IRB Actions/Project Status ................................................................................................................. 17
6.3.1 Approved ............................................................................................................................... 17
6.3.2 Modifications required ................................................................................... 17
6.3.3 Information Required ........................................................................................................... 17
6.3.4 Pending follow-up of receipt and review of serious adverse event ........................... 17
6.3.5 Deferral ................................................................................................................................... 18
6.3.6 Disapproval ............................................................................................................................ 18
6.3.7 Suspension and termination of research study by IRB ................................................... 18
6.3.8 Closed - Expired ..................................................................................................................... 18
6.3.9 Closed – Project Completion .............................................................................................. 18
6.3.10 Closed ..................................................................................................................................... 19
6.4
Notification of IRB actions ................................................................................................................. 19
6.5
Appeal of IRB decisions ..................................................................................................................... 19
IRB RESEARCH EVALUATIONS, PROCEDURES, CRITERIA AND ACTIONS
7.0
Determination of Type of Review .................................................................................................................. 19
8.0
Expedited Review of Research ..................................................................................................................... 19
8.1
Types of research eligible for expedited review .......................................................................... 20
8.2
IRB review materials ........................................................................................................................... 22
9.0
Exemption from Continuing Review ...................................................................................... 22
9.1
Types of research eligible for exempt continuing review ........................................................... 23
9.2
Modifications to exempt studies ...................................................................................................... 23
10.0
Modifications to Previously Approved Projects .......................................................................................... 24
11.0
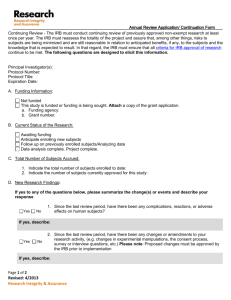
Continuing Review of Approved Applications ......................................................................................... 25
11.1
Criteria for requiring review more often than annually ............................................................... 25
11.2
Reminders/Notices ............................................................................................................................. 25
11.3
Lapsed studies ..................................................................................................................................... 25
12.0
Study Closure or Completion ......................................................................................................................... 26
12.1
Voluntary completion by investigators .......................................................................................... 26
3
IRB Standard Operating Procedures
2014
12.2
12.3
Termination of a study by the IRB .................................................................................................... 26
Expiration of approval period .......................................................................................................... 26
13.0
Adverse Events and Unanticipated Problems in Research ..................................................................... 27
13.1
Definitions ............................................................................................................................................. 27
13.2
Special requirements for research involving gene therapy studies ................................. 28
13.3
Internal vs External Reporting Requirements ................................................................ 28
13.4
IRB responsibilities following receipt of SAE/follow-up report ..................................................... 29
14.0
Safety Alerts, IND Safety Reports, MED Watch Reports ................................................................................ 29
15.0
Protocol Violations and Deviations .............................................................................................................. 30
15.1
Definitions ............................................................................................................................................. 30
15.2
Reporting procedures ........................................................................................................................ 30
15.3
Review by IRB committee ................................................................................................................. 31
15.4
Actions that may be taken during or after the investigation of non-compliance ................ 31
15.5
Continuity of care of research participants when study is suspended .................................... 32
15.6
Final outcome ..................................................................................................................................... 32
16.0
IRB Protocol Audits
17.0
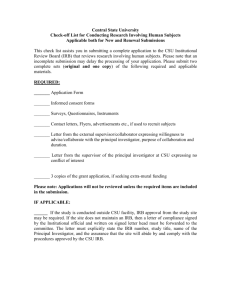
Recruitment and Advertisement Methods ................................................................................................. 33
17.1
Recruitment methods ........................................................................................................................ 34
17.2
Recruitment incentives ...................................................................................................................... 34
17.3
Promotional materials ......................................................................................................................... 35
17.4
External investigators and recruitment of student population ................................................... 35
18.0
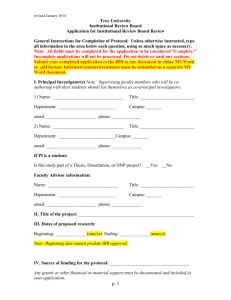
Informed Consent ............................................................................................................................................ 36
18.1
Basic elements of informed consent ............................................................................................... 36
18.2
Additional elements of informed consent ..................................................................................... 37
18.3
Exceptions to informed consent requirements ............................................................................. 38
18.4
Research related injury ...................................................................................................................... 39
18.5
Audio/video recordings .................................................................................................................... 40
18.6
Consent for mail and telephone surveys ...................................................................................... 40
18.7
Short form consent procedures ........................................................................................................ 40
18.8
Waiver of written consent ................................................................................................................. 41
18.9
Consent form templates ................................................................................................................... 42
18.10 Assent by minors ................................................................................................................................. 42
18.11 Parental permission ............................................................................................................................ 43
18.12 Surrogate consent for subjects who are decisionally impaired ................................................ 44
18.13 Obtaining consent from non-English speaking subjects .............................................................. 44
18.13.1 Translation and informed consent .................................................................................................. 45
18.14 Consent for use of stored samples and genetic ........................................................................... 45
.............................................................................................................. 32
4
IRB Standard Operating Procedures
2014
18.15
18.16
18.17
Revised Informed Consent and Reconsenting ............................................................................. 46
Stamped Copies of Consent Forms ............................................................................ 46
Record retention of informed consent documents .................................................................... 47
19.0
HIPAA and IRB Review ..................................................................................................................................... 47
19.1
HIPAA authorization and informed consent ................................................................................. 47
19.2
HIPAA Security ..................................................................................................................................... 48
20.0
Behavioral and Social Science Research .................................................................................................... 48
20.1
Types of risk found with Social/Behavioral research .................................................................... 49
20.2
Research involving deception or withholding of information ................................................... 50
20.3
Oral histories .......................................................................................................................................... 51
21.0
Review of Research Using Data and Specimens ........................................................................................ 51
21.1
Prospective use of existing materials .............................................................................................. 51
21.2
Retrospective use of existing materials .......................................................................................... 52
21.3
Research using data or tissue banks .............................................................................................. 52
CONSIDERATIONS FOR FDA-REGULATED PRODUCTS
22.0
Research involving an investigational drug/device .................................................................................. 53
22.1
Determination of need for an IND .................................................................................................. 54
22.2
Determination of significant vs non-significant for non-exempt medical devices ................ 55
22.3
Controlling distribution and disposition of devices ....................................................................... 55
22.4
Submitting applications ...................................................................................................................... 56
22.5
Submitting reports ............................................................................................................................... 56
23.0
Device studies in pediatric populations ...................................................................................................... 56
24.0
Emergency Use of an Investigation Drug or Biologic ................................................................................. 57
25.0
Exceptions from informed consent requirements for emergency research ......................................... 58
26.0
Emergency use of unapproved medical devices ................................................................................... 58
26.1
Requirements for emergency use ................................................................................................... 59
26.2
After-use procedures ......................................................................................................................... 59
27.0
Reporting the use of a test article to the IRB .............................................................................................. 60
28.0
Treatment use of an investigational drug/device ..................................................................................... 60
28.1
Single patient (non-emergency use) .............................................................................60
28.2
Humanitarian use device ................................................................................................................... 61
29.0
Biologics .............................................................................................................................................................. 61
5
IRB Standard Operating Procedures
2014
SPECIAL POPULATIONS
30.0
Definitions ............................................................................................................................................................ 62
31.0
Elements to consider in research involving vulnerable subjects .............................................................. 63
32.0
Decisionally impaired subjects ...................................................................................................................... 63
33.0
Surrogate permission with subjects judged incompetent to consent ................................................... 63
34.0
Research involving pregnant women, human fetuses and neonates .................................................. 64
34.1
Neonates ............................................................................................................................................... 64
34.2
Placenta, fetal material .................................................................................................................... 67
34.3
Neonates of uncertain viability ........................................................................................................ 67
34.4
Nonviable neonates .......................................................................................................................... 67
34.5
Viable neonate .................................................................................................................................... 68
35.0
Research involving prisoners .......................................................................................................................... 68
35.1
Issues to address in reviewing prisoner research .......................................................................... 68
35.2
Categories of research in which prisoners may participate ...................................................... 69
35.3
Required findings ................................................................................................................................ 69
35.4
Certification of prisoner research ......................................................................................................70
36.0
Research involving minors .............................................................................................................................. 71
36.1
Research in school settings ............................................................................................................... 71
36.2
Categories of research involving minors that may be approved by the IRB ......................... 71
36.3
IRB review of research involving minors ......................................................................................... 72
36.4
Students and Employees .................................................................................................................. 72
APPENDICES:
Appendix A:
Appendix B:
Appendix C:
Appendix D:
The Belmont Report ............................................................................................................................ 74
Unaffiliated Investigator Agreement .............................................................................................. 83
Confidentiality Agreement ................................................................................................................ 85
Requirements for Humanitarian Use Device ................................................................................. 86
6
IRB Standard Operating Procedures
2014
INTRODUCTION
Intended Audience and Distribution
The purpose of the Institutional Review Board (IRB) Standard Operating Procedures (SOP) is to provide
direction to members of the IRB and the IRB staff in carrying out duties assigned to the IRB, and to provide a
“best practices” reference guide. This SOP comprehensively summarizes existing policy as well as the
regulatory expectations found in the Common Rule (45 CFR 46) and the Food and Drug Administration (21
CFR 50 and 56). The SOPs provide valuable guidance, in conjunction with the Investigator’s Handbook, to
principal investigators, research professional and administrative staff, and others conducting or involved in
research.
Maintaining a Current SOP
These SOPs are considered to be a “living document” that will be updated or reviewed annually or more
often as changes in statutes, regulation, guidance, practice or policy occur. The SOP is the primary
location for compiling, organizing, integrating, and pointing to the rules, policies, practices, and guidance
encompassing the University’s Human Subjects Protection Program. At least once every three years the
Offices of the IRB and Research Compliance and Assurance initiate a comprehensive review of the
SOPs. Revisions may be made at any time, however, as required by changes in law, ethical standards,
institutional policy, quality assurance activities, or other considerations. Non-substantive revisions (e.g., to
correct typographical errors, update links, or incorporate summaries of new or revised laws or regulations
governing the IRB) may be made upon approval of the Office of Research Compliance and Assurance
with written notice to the IRB.
The Office of Research Compliance and Assurance would appreciate receiving your questions,
comments, and suggestions for improving this first version by e-mail to dlayton@southalabama.edu
CONTACT INFORMATION AND LINKS
OFFICE OF RESEARCH COMPLIANCE AND ASSURANCE
Dusty Layton, Director
dlayton@southalabama.edu
251-460-6625
Website: http://www.southalabama.edu/researchcompliance/index.html
IRB OFFICE:
SuzAnne Robbins
IRB Compliance Specialist
251-460-6308
srobbins@southalabama.edu
Human Subjects website: http://www.southalabama.edu/com/research/humansubjects.shtml
INSTITUTIONAL OFFICIAL:
Lynne Chronister
VP for Research and Economic Development
251-460-6333
lchronister@southalabama.edu
INSTITUTIONAL REVIEW BOARD CHAIR:
Dr. Ronald J. Russell
Chair, IRB
jrrusell@health.southalabama.edu
251-445-9615
USEFUL LINKS:
DHHS Office of Human Research Protections (OHRP): www.hhs.gov/ohrp/about/
OHRP guidance documents: http://www/hhs.gov/ohrp/policy/index.html
OHRP compliance references : http://www.hhs.gov/ohrp/compliance/
Food and Drug Administration (FDA): www.fda.gov/
FDA guidance documents: www.fda.gov/opacom/morechoices/industry/guidedc.htm
FDA compliance references : www.fda.ora/compliance_ref/
2
IRB Standard Operating Procedures
2014
PRINCIPLES, ROLES AND RESPONSIBILITIES
1.0
Regulatory and Ethical Mandates
The mission of the USA Human Subjects Protection Program is to ensure that:
1.
the rights and welfare of human subjects are paramount in the research process;
2.
the highest standards of ethical conduct are employed in all human subjects research
activities;
3.
research investigators are properly trained in the ethical and regulatory aspects of research with
human subjects;
4.
research investigators inform human subject participants fully of procedures to be followed, and
the risks and benefits of participating in research; and
5.
research using human subjects at USA conforms with all applicable local, state and
federal laws and regulations and the officially adopted policies of the University.
The regulation of human subjects research by the U.S. Department of Health and Human Services is
codified in 45 CFR 46. Because Subpart A of 45 CFR 46 has been adopted for human subjects research
by many federal agencies it is known as the “Common Rule.” The Common Rule requires that every
institution performing federally supported human subjects research file an assurance of protection for
human subjects. This research should be guided by the ethical principles adopted in the Belmont Report
and, additionally, should conform to the guidance documents described below:
1.1
The Nuremberg Code
The modern history of human subject protections begins with the discovery after World War II of
numerous atrocities committed by Nazi doctors in war-related human research experiments. The
Nuremberg Military Tribunal developed ten principles as a means of judging their “research” practices,
known as The Nuremberg Code. The significance of the Code is that it addressed the necessity of
requiring the voluntary consent of the human subject and that any individual “who initiates, directs, or
engages in the experiment” must bear personal responsibility for ensuring the quality of consent.
Additionally, the Nuremburg Code, more than other counterparts listed here, is a recitation of
participants’ legal rights, and has been used as a basis for decisions made in adjudicating the cases
involving human research.
1.2
The Declaration of Helsinki
Similar principles to The Nuremberg Code have been articulated and expanded in later codes, such as
the World Medical Association Declaration of Helsinki: Recommendations Guiding Medical Doctors in
Biomedical Research Involving Human Subjects (1964, revised 1975, 1983, 1989, 1996, 2000, 2013), which
call for prior approval and ongoing monitoring of research by independent ethical review committees.
1.3
The Belmont Report
Revelations in the early 1970s about the 40-year United States Public Health Service Study of Untreated
Syphilis in the Negro Male at Tuskegee and other ethically questionable research resulted in the 1974
legislation calling for regulations to protect human subjects and for a national commission to examine
3
IRB Standard Operating Procedures
2014
ethical issues related to human subject research (i.e., the National Commission for the Protection of
Human Subjects of Biomedical and Behavioral Research). The Commission’s final report, The Belmont
Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research, defines
the ethical principles and guidelines for the protection of human subjects. Perhaps the most
important contribution of The Belmont Report is its explanation of three basic ethical principles:
Respect for persons (applied by obtaining informed consent, consideration of privacy,
confidentiality, and additional protections for vulnerable populations);
Beneficence (applied by weighing risks and benefits); and
Justice (applied by the equitable selection of subjects).
The Belmont Report is attached to this document as Appendix A.
1.4
Department of Health and Human Services (DHHS) Regulations
Federal regulations require specific protections for human subjects. In May of 1974, the Department of
Health, Education, and Welfare (later renamed DHHS) codified its basic human subject protection
regulations at 45 CFR 46, Subpart A. Revised in 1981, 1991, 1996 and 2005, the DHHS regulations
presently include additional protections for fetuses, pregnant women, and human in vitro fertilization
(Subpart B), prisoners (Subpart C), and children (Subpart D). The DHHS regulations are enforced by the
Office for Human Research Protections (OHRP).
1.5
Federal Policy (Common Rule) for the Protection of Human Subjects. Food and Drug Administration
(FDA) Regulations at 21 CFR 50 and 56
When DHHS revised its regulations in 1981, the FDA codified almost identical informed consent
regulations at 21 CFR 50 and IRB regulations at 21 CFR 56. Additional FDA regulations that are relevant
to the protection of human subjects are:
(1) Investigational New Drug Applications (IND) (21 CFR 312)
(2) Radioactive Drugs (21 CFR 361)
(3) Biological Products (21 CFR 600)
(4) Investigational Device Exemptions (IDE) (21 CFR 812)
(5) Additional Safeguards for Children (21 CFR 50, Subpart D).
1.6
Federalwide Assurance
The Common Rule requires that every institution engaged in federally supported human research file an
“Assurance” of protection for human subjects. The University of South Alabama conducts human use
research under the terms specified in its Federalwide Assurance (FWA), the legally-binding agreement
to ensure that all human subjects research complies with the requirements of the governing Federal
Department or Agency head and its policies. All human subjects research activities, regardless of
funding source, will be guided by the ethical principles in the Belmont Report and all other appropriate
ethical standards recognized by Federal Departments and Agencies which have adopted the Federal
Policy for the Protection of Human Subjects. All research studies will comply with subparts of DHHS
regulations as codified in Title 45 CFR Part 4 and its Subparts A, B, C, and D. The Office of Research
Compliance and Assurance will submit the FWA and all updates to the federal Office of Human
Research Protections at least every three years. The Common Rule Terms of Assurance are listed on the
OHRP website. USA conducts human research under FWA #00001602.
4
IRB Standard Operating Procedures
2014
2.0
IRB Mission and Authority
The Institutional Review Board (IRB) has the authority to ensure that all human subjects research
conducted at the University of South Alabama complies with regulations of the Department of Health
and Human Services (DHHS) “45 CFR 46”, applicable Alabama state statues and regulations, the
principles of the Belmont Report and the Federalwide Assurance {FWA 00001602} of the University of
South Alabama.
The Human Subjects Protection Program serves their purpose by:
1.
Administratively supporting the University’s IRB
2.
Reviewing all research involving human subject’s research before it is initiated
3.
Working to protect the rights and welfare of human subjects by fostering and advancing the
ethical and professional conduct of persons engaged in research
4.
Providing education to researchers and staff
5.
Conducting periodic reviews of research involving human subjects, and
6
Serving as the institutional HIPAA Privacy Board
All human subjects research activities must be reviewed, prospectively approved and subject to
continuing oversight (at least annually) by the IRB to ensure the safety and welfare of participants,
pursuant to the regulation provided in 45 CFR 46. The IRB conducts review and approval for all human
subjects research activities conducted under its jurisdiction. This jurisdiction includes research conducted
or directed:
By USA faculty, staff, students, affiliates or outside researchers and occurs on the property of the
University of South Alabama regardless of funding sources
By an outside researcher involving USA faculty, staff, students, or affiliates.
The VP for Research and Economic Development is the Institutional Official for the institution for IRB
purposes through the Federalwide Assurance Agreement.
2.1
IRB Purpose
The IRB is responsible for the review and prior approval processes of research activities involving the use
of human subjects by engaging in deliberations to adequately provide a comprehensive review of the
proposed research activity, assess the risks and benefits to the subjects, ensure the research is
conducted ethically in an ongoing manner, and maintain communications with research personnel.
Duties of members including reviewing IRB application materials in advance of convened meetings
and being prepared to discuss issues related to human subjects protection, serving as primary
reviewer or secondary reviewer when assigned, and having an understanding of the specific
requirements of human subjects regulations. Duties include:
1.
Conduct initial and continuing review of research involving human subjects at intervals
appropriate to the degree of risk, but at least once a year and report IRB findings and actions to
the investigator and the institution.
5
IRB Standard Operating Procedures
2014
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
2.2
Determine which projects require review more often than annually and which projects need
verification from sources other than the investigators that no material changes have occurred
since previous IRB review.
Review proposed changes in research activities to insure that changes in approved research,
during the period for which IRB approval has been given, has not been initiated without IRB
review and approval.
Require or waive documentation of informed consent.
Follow procedures to insure that the IRB and Office for Human Research Protections (OHRP) of
the Department of Health and Human Services (DHHS) receive reports of unanticipated
problems involving risks to subjects and others.
Monitor additional safeguards when vulnerable subjects (minors, mentally incompetent,
prisoners, economically and educationally disadvantaged, pregnant females) are involved in
the research in order to protect against coercion or undue influence.
Conduct its review of research, except when an approved exempt review procedure is used, at
convened meetings at which a quorum of the members of the IRB are present.
Conduct reviews of all adverse event reports
Approve research only with the concurrence of a quorum of those members in attendance.
Report to the institution and OHRP any continuing or serious matters of non-compliance by
investigators with the requirements and determination by the IRB.
Have authority to suspend or terminate approval of research that is not in compliance with the
IRB’s determinations or has been associated with unexpected serious harm or risks to subjects.
Definition of Human Subjects Research
In order to ensure the rights, welfare, and protection of all subjects, all human subjects research, and all
other activities, which in part involve human subject research, regardless of sponsorship, must be
reviewed and approved by the IRB prior to initiation. This includes all interventions and interactions with
human subjects for research, including advertising, recruitment and/or screening of potential subjects.
Human subjects research is any research or clinical investigation that involves human subjects.
Note: The DHHS definition of human subjects will generally apply to all human research conducted by
investigators at the University of South Alabama unless the research involves a test article. Those
investigations involving a test article will also be subject to FDA definitions.
DHHS regulations define a human subject as a living individual about whom an investigator conducting
research obtains (1) data through intervention or interaction with the individual; or (2) identifiable
private information.
Intervention includes both physical procedures by which data are gathered (e.g., venipuncture) and
manipulations of the subject or the subject's environment that are performed for research purposes.
Interaction includes communication or interpersonal contact between investigator and subject or legal
representative in the case of minors or other vulnerable populations.
Private information includes information about behavior that occurs in a context in which an individual
can reasonably expect that no observation or recording is taking place, and information which has
been provided for specific purposes by an individual and which the individual can reasonably expect
will not be made public (for example, a medical record). Private information must be individually
identifiable (i.e., the identity of the subject is or may readily be ascertained by the investigator or
associated with the information) in order for obtaining the information to constitute research involving
human subjects.
6
IRB Standard Operating Procedures
2014
FDA regulations define human subject as an individual who is or becomes a participant in research,
either as a recipient of the test article or as a control. A subject may be either a healthy human or a
patient.
2.2.1
Research
DHHS regulations define research as a systematic investigation, including research
development, testing and evaluation, designed to develop or contribute to generalizable
knowledge.
A systematic investigation is an activity that involves a prospective plan that incorporates data
collection, either quantitative or qualitative, and data analysis to answer a question.
FDA regulations define a clinical investigation as any experiment that involves a test article and
one or more human subjects and that either is subject to requirements for prior submission to the
FDA, or is not subject to requirements for prior submission to the FDA under the Federal Food,
Drug, and Cosmetic Act, but the results of which are intended to be submitted later to, or held
for inspection by, the FDA as part of an application for a research or marketing permit.
A test article means any drug (including a biological product for human use), medical device
for human use, human food additive, color additive, electronic product, or any other article
subject to regulation under the Federal Food, Drug, and Cosmetic Act.
2.3
Agreements to Provide IRB Review of Research Conducted by Unaffiliated Investigators
USA may be asked to provide IRB review for investigators who are unaffiliated with the University of
South Alabama. Circumstances in which this arrangement might be considered would typically involve
a study based at USA in which the unaffiliated investigator is collaborating in the study. It will generally
not be considered appropriate to extend IRB oversight to research by unaffiliated investigators in which
USA is not otherwise engaged.
All requests for USA to serve as the IRB of record for an unaffiliated investigator should be referred to the
Institutional Official. This referral should include an “Unaffiliated Investigator Agreement” based on the
USA approved template attached as Appendix B, together with a recommendation from the USA IRB
with responsibility for that given study and/or group of investigators. Usually, this agreement will apply to
a single research project. Copies of the agreement will be provided to the unaffiliated investigator and
maintained in the Offices of the IRB and Research Compliance and Assurance.
2.4
Human Research Activities Performed at Other Institutions
All research activities performed by, or under the direction of, USA personnel or which use University
resources or facilities, must comply with applicable USA policies and procedures, regardless of funding
and whether performed in USA facilities or at offsite locations.
2.4.1
Requirements for Approval of Research at Non-USA Facilities
Any human subjects research conducted in whole or in part outside of USA facilities must be
reviewed and approved by USA IRB prior to initiation if it satisfies any of the following criteria.
It is conducted by or under the direction of USA personnel in connection with his or her USA
responsibilities.
7
IRB Standard Operating Procedures
2014
2.4.2
It uses USA property, facilities, or resources to support or carry out the research.
The name of the University of South Alabama is used in applying for funds (intra or extramural).
The name of the University of South Alabama is used in explanations and/or representations to
subjects.
The investigator plans to use his/her University of South Alabama association in any publication
or public presentation resulting from the research.
Non-public information from USA will be used to identify or contact human research subjects or
prospective subjects.
IRB Approval of Research to be Done at a Non- USA Institution
The researcher will need to obtain approval from the Non-USA IRB in addition to the USA IRB for
any research done at a Non- USA Institution unless a cooperative review agreement has been
executed in advance of the study.
IRB ORGANIZATION AND ADMINISTRATION
3.0
IRB Membership
At least five members of sufficiently diverse backgrounds, including consideration of racial and cultural
backgrounds of members and sensitivity to issues such as community attitudes;
Persons who are able to ascertain the acceptability of research applications in terms of institutional
commitments, applicable law, and professional standards;
Members of both sexes;
At least one member whose primary area of expertise is with handicapped and/or retarded children;
At least two members whose primary concerns are in behavioral disciplines;
At least one member whose primary concerns are in non-scientific areas;
Members representing more than one profession;
A member who is not affiliated or related to a person who is affiliated with the institution;
Persons who are primarily concerned with the welfare of vulnerable subjects (minors, prisoners,
terminally ill, etc.);
When needed, individuals with competence in special areas to assist in the review of complex issues;
Participants in the initial or continuing review of projects who do not have a conflicting interest;
The standards described above represent minimum requirements which the USA IRB typically exceeds.
In many instances, an IRB will have 15 or more members with varied expertise and speciliaization in
order to meet the research review requirements. IRB membership is recorded on a roster that is
submitted to the Office of Human Research Protections (OHRP) and is filed in the IRB office.
3.0.1
Duties of IRB Members
Duties of members include reviewing human subject application materials in advance of meetings and
being prepared to discuss issues related to human subjects protections, serving as primary reviewer when
requested by the chair, and having an understanding of the specific requirements of human subjects
regulations. Duties include:
Protecting rights and welfare of human subjects
Determining risks are minimized
Ensuring that investigators:
o use of procedures are consistent with sound research design and that do not expose
subjects to risks
8
IRB Standard Operating Procedures
2014
when appropriate, use procedures already being performed on the subjects for diagnostic
or treatment purposes, and
o ensuring that the investigator follows a procedure for properly documenting informed
consent
Determining that risks to subjects are reasonable in relation to anticipated benefits to subjects
Determining that selection of subjects is equitable. In making this assessment, the following should
be considered:
o purpose of the research and setting in which the research is conducted
o IRB members should be cogniz2ant of special problems of research involving vulnerable
populations
Determining if informed consent is sufficient and includes all mandated elements, if not, request
clarifications and changes in consent document
Determining that the research plan includes adequate provisions for ensuring the safety of subjects
Determining if adequate protections are afforded to protect the privacy of subjects and maintain
confidentiality of data
If applicable, documenting requirements for wavier of informed consent have been met
Ensuring additional safeguards are in place to protect rights and welfare of subjects that are more
likely to be vulnerable to coercion or undue influence, such as students, children, prisoners,
educationally and economically disadvantaged, etc.
o
3.1
Chairperson Responsibilities
3.2
Vice-Chair(s) Responsibilities
3.3
Chairs convene meetings
Call special meetings when necessary
Make decisions in emergency situations to protect subjects and remain in compliance with regulations
Confirms primary/secondary reviewer assignments made by IRB staff as requested
Conducts review of all protocols discussed at convened meetings
Conducts expedited review of biomedical research studies
Reviews policies and procedures on an ongoing basis
Serves as an advisor/educator in the institution’s research community
Performs duties of the chair in his/her absence
Assists chairperson, IRB staff as need
Committee Member Appointment
Committee members are nominated by a Committee on Committees with input from the Director,
Office of Research Compliance. Prospective members may also be identified by the IRB chair and staff
who review the nature and demands of the IRB. IRB members are appointed for three year terms which
are renewable. If a member resigns prior to the end of their term, a person may be appointed to
complete the original term.
3.4
Non-voting Members
Non-voting members from among the academic or administrative staff of the University are appointed
to aid the IRB in conducting its duties. These members may take part in all meetings of the IRB,
participate in discussions and make recommendations, but they may not vote on the decisions. Nonvoting members are not included in determining or establishing a quorum at the meetings. IRB
meeting minutes reflect the presence of non-voting members.
9
IRB Standard Operating Procedures
2014
3.5
Termination of Appointment:
Appointment to the IRB may be terminated before the expiration of the three-year term. The
Institutional Official may remove an IRB member if he/she, in consultation with the IRB chair or other
parties, determines that the member fails to perform his or her duties as a member.
3.6
Confidentiality Agreement:
Upon appointment to the IRB or attendance at an IRB meeting, members (voting or otherwise),
consultants, guests, etc., will sign a confidentiality agreement attached as Appendix C.
3.7
Orientation and Training of IRB Members:
Following appointment of new members, the Offices of the IRB and Research Compliance and
Assurance conducts an orientation session to include topics such as: research compliance, processing
of protocols, meeting process and expectations of an IRB member. Additionally, a new member will
receive a binder of reference materials and a IRB member handbook (including these SOPs). All
members complete the online educational module entitled “Protecting Human Subject Research
Participants” provided by the NIH Office of Extramural Research or comparable training. Members are
provided with continuing education opportunities within the institution, and receive continuing
education materials at regularly held IRB meetings.
3.8
Member Conflict of Interest:
No IRB or consultant may participate in the IRB initial or continuing review of any project in which
he/she has a conflict of interest, except to provide information requested by the IRB. Examples of such
conflicts of interest could include: a member of the IRB who serves as an investigator or sub-investigator
on research under review by the IRB, or a member who holds a financial conflict of interest in a sponsor
or product under study. In cases where the assigned initial reviewer has a conflict of interest, the review
must declare that conflict of interest and the protocol will be re-assigned to another reviewer. The IRB
member will indicate a conflict of interest in IRBNet (i.e., recusal or abstention) and is recorded in the
minutes as a recusal.
3.9
Investigator Conflict of Interest
It is University policy that individuals conducting human subjects research have a paramount
responsibility to ensure that any conflicting interests of the researchers do not compromise the welfare
and rights of those human subjects. Identification of possible conflicts of interest is an important step to
protect human participants and maintain the integrity of the IRB process. The University requires
submission of an annual conflict of interest disclosure form by all faculty members and Employees in an
administrative position at or above a director level, as well as disclosure throughout the year of changes
that may either: (a) give rise to a potential conflict of interest; or (b) eliminate a potential conflict
previously disclosed. In addition the IRB application includes questions that probe for potential conflict
of interest in relation to the specific study.
Investigators, Co-Investigators and any study personnel are required to disclose Financial Conflicts of
Interest or other interests that are, or may be perceived to be related to the study on the application
for initial IRB review and approval. If there is a potential or perceived conflict related to the study, the
Investigator is asked if the conflict has been disclosed and/or managed. Conflict of Interest disclosure
forms are reviewed by the department chair/supervisor and forwarded to the Office of Research
Compliance and Assurance. If warranted, the IRB will verify that a management plan has been
executed. A management plan template for human subjects research may be used for documenting
10
IRB Standard Operating Procedures
2014
and identifying appropriate actions to eliminate, reduce or resolve financial conflicts of interest or
conflicts of commitment. These matters may be referred to the University Conflict of Interest
Committee and the reporting employee shall be notified of the referral. In instances where a conflict
of interest involving human subjects research is allowed, it is essential that research subjects and other
interested parties be informed of the conflict of interest. If an investigator is participating in a multicenter trial and has been allowed to conduct human subjects research while possessing a financial
interest, that fact should be made known to the Investigator or sponsor by the coordinating center.
Notification of research subjects falls within the purview of the applicable IRB, which will determine
whether and how the conflict of interest should be disclosed to the relevant human research subjects.
This may include a description in the consent form of the conflict of interest.
4.0
IRB Administrative Support
The IRB staff supports the function of the IRB infrastructure and all activities engaged in human subjects
research at the direction and under the supervision of the Director of the Office of Research
Compliance and Assurance (ORCA). The Director, ORCA is responsible for directing and overseeing all
IRB support functions and operations; training, supervising and evaluating IRB staff; and developing and
implementing procedures to facilitate efficient document flow and maintenance of all IRB records.
The IRB administrative staff:
Maintain up-to-date knowledge of policies/procedures and regulations regarding human subjects
research and IRB operations.
Perform administrative duties to assure systematic flow of work through the IRB.
Prepare and distribute review materials to members and consultants.
Maintain files
Prepare and distribute minutes
Send out notification of IRB decisions, requests for additional information and correspondence to
investigators in a timely manner.
Assist in the conduct of educational workshops
IRB forms are used to ensure that polices are integrated into the day to day research and review
operations. This enables execution of functions in which the IRB can manage, review, track and notify
in a consistent manner.
4.1
Education and Training of Staff:
Staff members will initially receive the same orientation as IRB members with an introductory lecture
and orientation to IRB and office procedures. Further training is provided by working in close interaction
with other staff members. Staff members should be provided with continuing education opportunities
and resources should be made available for them to attend regional or national human subject
protection meetings, as deemed appropriate by the Director of the Office of Research Compliance
and Assurance in consultation with the Institutional Official. Credentials as a Certified IRB Professional
(CIP) will be encouraged for IRB staff. A variety of resource materials (i.e., newsletters, textbooks,
meeting materials, etc.) are available.
The administrative staff will make every effort to ensure prompt and through review of all submissions to
ensure the safety and welfare of research subjects. In addition, it is the responsibility of the IRB chair,
Director, ORCA and administrative staff for educating the members of its research community in order
to establish and maintain a culture of compliance with regulations and institutional policies relevant to
human subject protections.
11
IRB Standard Operating Procedures
2014
4.2
Investigator and Key Research Personnel Training
Investigators and research personnel must complete human subjects research training as a condition
of the University’s Federalwide Assurance of Compliance. In addition to human subjects training, all
investigator(s) and key research personnel within USA’s HIPAA covered entity must complete USA’s
HIPAA in Research tutorial. Completion of training is a condition for IRB approval. The Human
Subjects Protection Program has ongoing educational programs for both IRB members, investigators
and study staff. Examples of educational opportunities that are offered include:
5.0
Clinical research coordinators/nurses forum
In-service educational presentations scheduled as a component of convened IRB meetings
Workshops tailored and presented for specific research/departments
IRB 101 for Students which includes class presentation to students conducting research as part of their
class assignment
Record keeping and Reporting:
The Common Rule and, when applicable, Food and Drug Administration (FDA) regulations require
written policies and procedures to govern the operations and direct the activities of the IRB. Record
keeping and documentation requirements for IRB operations are as follows:
Generally, IRB records shall include:
Written standard operating procedures
IRB membership rosters
Training records
IRB correspondence
IRB research application (protocol) files
Research (protocol) tracking system
Documentation of exemptions, exceptions or waiver of informed consent
Documentation of expedited reviews
Documentation of convened IRB meetings – minutes
Documentation of review for adverse events
Documentation of review for protocol deviations/violations
Documentation of review by another institution’s IRB when appropriate
Documentation of cooperative review agreements, e.g., Memoranda of Understanding (MOUs)
for multi-site research, or as otherwise appropriate
(14) Federal Wide Assurances (FWA)
(1)
(2)
(3)
(4)
(5)
(6)
(7)
(8)
(9)
(10)
(11)
(12)
(13)
The study-specific records as outlined above relating to research that is conducted shall be retained for
at least 3 years after completion of the research.
For studies that the IRB has exempted from continuing review, study-specific records shall be retained
for at least three years after the exemption is granted. Annually, the IRB will make an inquiry with the
investigator regarding the current status of the project until the investigator reports that the study is
complete.
Authorized persons shall be able to access records for inspection and copying at reasonable times and
in a reasonable manner. Investigators may be required to follow different record retention policies
depending on study sponsorship.
12
IRB Standard Operating Procedures
2014
5.1 Documentation and Retention of IRB Documents
At a minimum, retention of records is required by 45 CFR 46 for a period or three years after a research
project is completed. USA retains the following documents in accordance with this requirement.
Records will be retained longer if required by applicable FDA or DHHS regulations or by the study
sponsor.
(1)
(2)
(3)
(4)
(5)
(6)
5.2
Copies of all research protocols reviewed, evaluations, approved consent documents,
applications for initial approval, continuing review, amendments, advertisements, adverse events
reports and protocol deviations and any other correspondence from investigators related to the
research study.
Minutes of convened IRB meetings.
Copies of audit reports
Training of IRB members, staff, investigators and key research personnel
Correspondence with government officials concerning unanticipated problems
Correspondence with government officials that could reasonably be expected to affect the
status of USA’s FWA.
Access to IRB Records
Ordinarily, access to IRB records is limited to the IO, the IRB chairperson, IRB members, IRB staff, Office of
Research Compliance and authorized USA representatives, and officials of Federal and state regulatory
agencies, including the Office for Human Research Protections (OHRP), and, if applicable, the Food
and Drug Administration (FDA). Investigators shall be provided reasonable access to files related to
their research. All other access to IRB records is limited to those who have legitimate need for them, as
determined by the IRB Chairperson, the Director, Research Compliance, University Counsel and the
Institutional Official.
5.3
IRBNet Online Management System
The IRB utilizes IRBNet, an online management system for submission, review, and approval of human subjects
research studies. IRB members use the IRB Review Form to document review of assigned research studies and is
uploaded IRBNet. Additionally, adverse events, protocol deviations, and PI conflicts of interest are
electronically tracked.
IRBNet resources, including login instructions, creating new project submissions, etc., can be found on
the IRBNet resource webpage at: http://www.southalabama.edu/researchcompliance/irbnet.html
MEETING MATERIALS AND DOCUMENTATION
6.0
Meeting Agenda
The meeting agenda outlines human subject research activities subject to review by a convened
meeting of board members under the jurisdiction of the IRB. Submission of a research protocol will
satisfy all of the procedural requirements necessary for the comprehensive review of all of the relevant
materials prior to the convened meeting. Additionally, the agenda provides a listing of any discussion
13
IRB Standard Operating Procedures
2014
items relevant to the operations of the human subject protection program .
The IRB Compliance Specialist prepares the meeting agenda. Additionally, relevant materials for review
is distributed via IRBNet to all board members a week in advance of the scheduled meeting.
The agenda shall include the following items:
Date of meeting
Approval of minutes from previous meeting
Adverse Events
Protocol Deviations
Closed/expired protocols
Protocol Reviews (noted for informational purposes)
o Closed protocols
o Exempt protocols
o Expedited protocols
New Protocol Reviews
o New Submissions
o Amendments
o Continuing Reviews
Information/Education
Research Compliance
Old/New Business
6.1 Meeting Minutes
The minutes of IRB meetings shall be compiled by the IRB Compliance Specialist, following the IRB
meeting minutes template. The following specific information shall be recorded in the meeting minutes:
(1)
(2)
(3)
(4)
(5)
(6)
Attendance recorded by name
Approval of previous minutes
Adverse Events action
Protocol Deviations
List of closed/expired protocols
List of approved exempt and expedited approved protocols and specific citation for the category
of expedited review.
(7) Actions taken by the IRB on initial, amendments, and continuing review applications. If applicable,
specific measures taken to protect vulnerable populations and request for waiver of informed
consent.
Votes on these actions
Basis for requiring changes in or disapproving research
Summary of controverted issues
Required IRB findings and determinations
(8) Information/Education
(9) Old/New Business
14
IRB Standard Operating Procedures
2014
The minutes shall record when a member either enters/leaves the convened meeting as evidence of
proper quorum.
The minutes shall records when a member either enters or leaves the convened meeting
The minutes shall record any presence of conflict of interest or abstention
6.2
Review by convened IRB (Full Board Review)
Any study involving greater than minimal risk requires a review by the convened IRB. A few examples of
studies that involve greater than minimal risk:
Studies involving vulnerable populations including pregnant women, prisoners, mentally
incompetent patients, and minors.
Any clinical interventional study that randomly assigns human subjects to alternative
experimental or placebo groups
Studies involving sensitive information connected to personal identifiers
The IRB meets at least once a month on a regularly scheduled day, normally the second Tuesday of
each month. Scheduled meetings may be cancelled by the IRB Compliance Specialist due to the
inability to secure a quorum for attendance, or other reasons as may arise that make a scheduled
meeting unnecessary or otherwise inappropriate. The IRB Office maintains an electronic IRB address
book used to notify members of meetings and other pertinent IRB information.
One week prior to the convened meeting, all members of the IRB shall be provided with detailed initial
review materials describing the research to facilitate discussion of the protocol adequately and
determine the appropriate action during the convened meeting. The materials available in IRBNet are
listed in section 6.2.2 below. All members of the IRB are expected to familiarize themselves with meeting
materials in order to contribute to the IRB’s deliberations.
6.2.1
IRB Review Procedures
Primary/Secondary Reviewers
Both the primary and secondary reviewer for a given research protocol should make an
evaluation of the protocol before the convened IRB meets and should present the protocol
during the meeting. A primary/secondary reviewer system is used for review of initial protocols
which two members are assigned to lead the review and present the protocol for discussion at
the convened meeting. Primary/secondary reviewers are assigned in advance of the meeting
by the IRB chair or staff. This review/presentation should include an overview of the project
and the identification of major issues arising in the project.
Other reviewers
All IRB members receive the IRB agenda, previous month’s minutes for approval, appropriate
IRB application(s), informed consent (or request to waiver informed consent) and
surveys/questionnaires. Relevant materials are to be provided for all types of IRB review
including initial review, continuing review and amendments for review at the convened
meeting.
15
IRB Standard Operating Procedures
2014
6.2.2
IRB Meeting Materials
IRB protocol
IRB application(s)
Consent document(s) or request for waiver of consent as permitted by 45 CFR 46.116(d)
Appropriate special population checklist, if applicable
Related grant applications or progress reports
Subject surveys/questionnaires
Supporting documentation from sponsors
Advertisements or other information provided to research subjects
Drug related information such as Investigator Brochures or package inserts
Any other information known to be relevant to the determination of safety, risks and benefit
to the research study
Subject recruitment materials, flyers, advertisements
Minutes of previous meeting
All members receive a copy of the minutes from the previous meeting of the IRB. The chair
leads the meeting of the convened IRB. This includes calling the meeting to order, leading
the IRB through the agenda, and calling for motions and votes. The chair ensures that all
members have an opportunity to express their opinions and concerns on the research
under review.
Voting
In order for research to be approved, it shall receive the approval of a majority of the members
present at the meeting provided a quorum exists. The voting process proceeds as follows: The
chair may entertain a motion (which usually comes from a primary reviewer) and a second that
the IRB take a certain action regarding a given protocol. The actions the IRB may take are
outlined in section 6.3. After a motion has been made and seconded, there should be an
opportunity for discussion before a vote is taken. Those members present for the vote should be
recorded as either voting for, opposed or abstained.
Recusal of members with a conflict of interest
When an IRB member has a conflict of interest that requires him/her to recuse himself/herself from
discussion of and voting on a particular protocol, that member may not participate in the
discussion unless asked to address questions raised by other members. If the member’s recusal
causes a loss of quorum, the vote should be postponed to another meeting. For this reason, IRB
members should notify the chair prior to the meeting if they have a conflict of interest related to
a specific protocol slated for review at the meeting, and every effort should be made to ensure
adequate members in attendance.
Attendance by investigators
Investigators may be invited to attend the portion of the IRB meeting at which their protocol is
discussed. The investigator may answer questions raised by the IRB. The investigator should not
be present for the final deliberation and vote on his or her protocol.
16
IRB Standard Operating Procedures
2014
Attendance by guests
The IRB may permit guests to attend a meeting, for example, in order for them to learn about the
IRB process. Members should be alerted to the presence of guests and their reason for
attending. Guests should sign the confidentiality agreement prior to the start of their
attendance at the meeting.
Teleconference/videoconferencing
In some cases, teleconferencing and/or videoconferencing may be necessary in order to
have a quorum for a meeting, or to ensure that a protocol is reviewed by someone with a
proper level of expertise. When the IRB makes use of this technology, all other normal meeting
requirements apply. Additionally, whenever teleconferencing and/or videoconferencing is
used, special care must be taken to ensure the security of the data transmissions so that the
privacy of researchers and IRB members is protected.
6.3
IRB Actions/Project Status
The IRB administrative staff shall provide written notification of its determinations to investigators.
IRB actions, upon review of research, include the following:
6.3.1
Approved
In the case of an approval with no changes, the research may begin once the investigator receives
written documentation of IRB approval.
Unless otherwise specified, the approval period for research approved without changes is one year
from the date of the meeting at which approval was granted.
6.3.2
Modifications Required
The IRB may determine that a study may be approved with minor changes or clarifications. Minor
changes are those changes that do not involve potential for increased risk or decreased benefit to the
human subjects. For minor changes, the IRB administrative staff ensures that the investigator makes the
appropriate changes to the research protocol. The research may proceed after the required changes
are verified and the investigator receives IRB letter of approval.
6.3.3
Information Required
The primary reviewer and/or secondary reviewer is responsible for reviewing the changes to ensure
that the changes are adequately addressed. The IRB protocol receives final approval when all
required changes have been submitted and approved by the reviewer(s).
Unless otherwise specified, the approval period for research for which minor changes were
stipulated is one year from the date of the last convened meeting at which the protocol was
reviewed.
17
IRB Standard Operating Procedures
2014
6.3.4
Pending follow-up of receipt and review of serious adverse event
All outstanding serious adverse event(s) pending review and/or response from the investigator during
review of a renewal or amendment submission at the convened meeting will not be granted approval
until the adverse event(s) is resolved.
6.3.5
Deferral
Deferral is used to describe the situation in which the IRB determines that substantive changes must be
made before approval may be granted. The investigators response, including any amended materials,
must be reviewed at the next convened IRB meeting.
Subject to IRB discretion, a proposal may be withdrawn if the investigator does not respond to a
deferral within a reasonable amount of time. If the investigator wishes to conduct a study that has
been withdrawn, he/she must submit a new application, addressing concerns from the prior IRB review.
Unless otherwise specified, the approval period for research protocols that are deferred is one year from
the date of the last convened meeting at which approval was granted or minor changes were
stipulated.
6.3.6
Disapproval
If the IRB determines that the research cannot be conducted at USA or by employees or agents of
the University or otherwise under the auspices of the University, the project, as proposed, is
disapproved and may not go forward. Disapproval usually indicates that a proposal requires
major changes not likely to be feasible without a complete reassessment of the protocol by the
investigator and/or sponsor.
6.3.7
Suspension and Termination of Research Study by IRB
The chair of the IRB or the convened IRB may suspend a study at any time if it is determined that the
study requires further review or evaluation. This determination may be made due to an adverse event,
noncompliance or other danger to human subjects. Once a study has been suspended, the convened
IRB should review the study and either require changes to the protocol, allow the study to restart, or
terminate the study.
Though the chair may suspend a study, only the convened IRB can make the decision to terminate a
study. When a study is suspended or terminated, the IRB notifies the Institutional Official. If the
suspended or terminated study is externally funded, the IRB will notify the Office of Sponsored
Programs. The Institutional Official is responsible for all required reports to federal agencies.
6.3.8
Closed – Expired
IRBNet automatically generates an notice of expiration if a study is not closed or renewed by the date
of expiration.
6.8.9
Closed – Project Complete
Upon receipt of a IRB closure form the IRB Office administratively closes the research project. The
researcher will not be permitted to have any further interaction with subjects or their data in ways that
would require ongoing IRB approval. If the investigator whish to enroll new subjects for the study or
18
IRB Standard Operating Procedures
2014
engage in human subjects research he/she must reactivate the protocol with the IRB Office. The
researcher may close a study when he/she is no longer accruing subjects, using research interventions
on existing subjects, collection data (including follow-up data), or performing any other tasks identified
as part of the IRB approved research study. However, a researcher may continue to analyze
aggregate de-identifed data sets beyond study closure.
6.8.10 Closed
Project closure that is not affiliated with project completion or expiration.
6.4
Notification of IRB Actions
Investigators received automated notifications via IRBNet of the IRBs decision and any changes
required. Summaries of actions taken are provided to the Institutional Official in the form of meeting
minutes. Final approval is not granted until all required changes have been made and submitted for
review and approval. The IRB attempts to retain approval periods constant from year to year
throughout the life of each project. Therefore, when materials are submitted far enough in advance
that the IRB performs the continuing review within 30 days before the current approval period expires,
the IRB retains the original anniversary date as the date for the new approval period to begin. That is,
the clock need not be reset if review occurs within thirty days of the original anniversary date. This
notification process applies to all levels of review. The IRB Chair does not sign approval letters
generated in IRBNet. Federal regulations do not specify the procedure the IRBs must use regarding
signatures of IRB approval letters. USA IRB does not require signature of approval letters by the Chair.
6.5
Appeal of IRB Decisions
Investigators may appeal IRB requirements for specific changes in the protocol and/or consent
document(s). At the discretion of the chair, the investigator may make such an appeal in writing to
the IRB. At the IRB’s discretion, the investigator may be invited to the IRB meeting at which his or her
appeal will be considered.
If the IRB decides to disapprove a research activity, it shall include in its written notification a statement
of the reasons for its decision, and give the investigator an opportunity to respond in person and/or in
writing. An appeal of a disapproved research project must be reviewed at a convened meeting.
Other university officials may, in certain cases, decide that a research study may not be conducted
despite IRB approval. One example could be a circumstance in which a certain project or area of
research is deemed to be inappropriate or underfunded. In the case of a decision by the IRB to
disapprove, suspend, or terminate a project, only the Institutional Official may request that the IRB
reevaluate a project because of procedural questions related to the IRB review. However, the IRB
decision to disapprove, suspend, or terminate a project may not be reversed by the any officer or
agency of the University of South Alabama, state government or federal government
IRB RESEARCH EVALUATIONS, PROCEDURES, CRITERIA AND ACTIONS
19
IRB Standard Operating Procedures
2014
7.0
Determination of Type of Review
The IRB chair or administrative staff screens applications and makes determinations as to
whether a project constitutes human subjects research and, if so, the type of review required
(full board review, expedited review, or exempt). All applications are assigned to full board
review if greater than minimal risk. Minimal risk is defined in §46.102(i) as the probability and
magnitude of harm or discomfort anticipated in the research are not greater in and of
themselves than those ordinarily encountered in daily life or during the performance of routine
physical or psychological examinations or tests. All projects involving the use of investigational
drugs, devices, or biologics for which an IND/IDE are required receive full board review.
Reviewers complete the IRB Review Form to document their review and upload the reviewer
document in IRBNet.
8.0
Expedited Review of Research
Under expedited review procedures, the review may be carried out by the IRB chair, Vice-chair or
designated IRB member utilizing the appropriate IRB evaluation form. In reviewing the research, the
reviewer may exercise all of the authorities of the IRB except that the reviewer may not disapprove the
research. A research activity may be disapproved only after review at convened meetings at which a
majority of the members of the IRB are present, including at least one member whose primary affiliation
is in nonscientific areas.
Federal regulations limit the use of expedited review procedures to specific research categories
published in the Federal Register. Use of expedited review by the IRB must be restricted to those
applications that fulfill one of the nine categories listed below in section 8.1.
8.1
a.
Minimal risk: Research activities that (i) present no more than minimal risk to human
subjects and (ii) involve only procedures listed in one or more of the specific nine
categories below.
b.
The expedited review procedure may not be used where identification of the
participants and/or their responses would reasonably place them at risk of criminal or
civil liability or be damaging to the subject's financial standing, employability, insurability,
reputation or be stigmatizing, unless reasonable and appropriate protections will be
implemented so that risks related to invasion of privacy and breach of confidentiality are
no greater than minimal. Additionally, the expedited review procedures may not be
used for government classified research involving human subjects.
Types of Research Eligible for Expedited Review
The following nine expeditable categories pertain to both initial and continuing IRB review:
Category 1 Research on drugs for which an investigational new drug application(21 CFR
312) is not required or research on medical devices for which a) an investigational device
exemption application (21 CFR 812) is not required or b) the medical device is
cleared/approved for marketing and the medical device is being used in accordance with its
cleared/approved labeling.
20
IRB Standard Operating Procedures
2014
Category 2 Collection of blood samples by finger stick, heel stick, ear stick or venipuncture as
follows: (a) from healthy, nonpregnant adults, who weigh at least 110 pounds. For these
subjects, amounts drawn may not exceed 550 ml in an 8-week period and no more than 2 times
per week; or (b) from other adults and children, considering the age, weight, and health of the
subjects, the collection procedure, the amount of blood to be collected, and the frequency
with which it will be collected. For these subjects, the amount drawn may not exceed the lesser
of 50 ml or 3 ml/kg in an 8-week period and collection may not occur more frequently than 2
times per week.
Category 3
Prospective collection of biological specimens for research purposes by
noninvasive means. Examples: (a) hair and nail clippings in a nondisfiguring manner; (b)
deciduous teeth at the time of exfoliation or if routine patient care indicates a need for
extraction; (c) permanent teeth if routine patient care indicates a need for extraction; (d)
excreta and external secretions (including sweat); (e) uncannulated saliva collected either in
an unstimulated fashion or stimulated by chewing gumbase or wax or by applying a dilute
citric solution to the tongue; (f) placenta removed at delivery; (g) amniotic fluid obtained at
the time of rupture of the membrane prior to or during labor; (h) supra- and subgingival dental
plaque and calculus, provided the collection procedure is not more invasive than routine
prophylactic scaling of the teeth and the process is accomplished in accordance with
accepted prophylactic techniques; (i) mucosal and skin cells collected by buccal scraping or
swab, skin swab, or mouth washings; (j) sputum collected after saline mist nebulization.
Category 4 Collection of data through noninvasive procedures (not involving general
anesthesia or sedation) routinely employed in clinical practice, excluding procedures
involving x-rays or microwaves. Where medical devices are employed they must be
cleared/approved for marketing. (Studies intended to evaluate the safety and effectiveness
of the medical device are not generally eligible for expedited review, including studies of
cleared medical devices for new indications.) Examples: (a) physical sensors that are applied
either to the surface of the body or at a distance and do not involve input of significant
amounts of energy into the subject or an invasion of the subject's privacy; (b) weighing or
testing sensory acuity; (c) magnetic resonance imaging; (d) electrocardiography,
electroencephalography, thermography, detection of naturally occurring radioactivity,
electroretinography, ultrasound, diagnostic infrared imaging, doppler blood flow, and
echocardiography; (e) moderate exercise, muscular strength testing, body composition
assessment, and flexibility testing where appropriate given the age, weight, and health of the
individual.
Category 5 Research involving materials (data, documents, records, or specimens) that
have been collected, or will be collected solely for non-research purposes (such as medical
treatment or diagnosis).
Category 6 Collection of data from voice, video, digital, or image recordings made
for research purposes.
Category 7 Research on individual or group characteristics or behavior (including, but not
limited to, research on perception, cognition, motivation, identity, language, communication,
cultural beliefs or practices, and social behavior) or research employing survey, interview, oral
history, focus group, program evaluation, human factors evaluation, or quality assurance
methodologies.
Category 8
Continuing review of research previously approved by the convened IRB (a)
21
IRB Standard Operating Procedures
2014
where the research is permanently closed to the enrollment of new subjects, and all subjects
have completed all research-related interventions, and the research remains active only for
long-term follow-up of subjects; or (b) where no subjects have been enrolled and no additional
risks have been identified; or (c) where the remaining research activities are limited to data
analysis and report writing.
Category 9
Continuing review of research, not conducted under an investigational new
drug application or an investigational device exemption where Category 2 through Category
7 do not apply but the IRB has determined and documented at a convened meeting that the
research involves no greater than minimal risk and no additional risks have been identified.
The reviewer must make certain determinations to approve applications. In conducting the
expedited review, the designated reviewer(s) must review materials in sufficient detail to make the
following determinations required under federal regulations:
Risks to subjects are minimized (i) by using procedures which are consistent with sound
research design and which do not unnecessarily expose subjects to risk, and (ii) whenever
appropriate, by using procedures already being performed on the subjects for diagnostic or
treatment purposes.
Risks to subjects are reasonable in relation to anticipated benefits if any, to subjects, and the
importance of the knowledge that may reasonably be expected to result.
Selection of Subjects is Equitable In making this assessment the reviewer(s) should take into
account the purposes of the research and the setting in which the research will be conducted
and should be particularly cognizant of the special problems of research involving vulnerable
populations, such as children, prisoners, pregnant women, mentally disable persons or
educationally disadvantaged persons.
Informed consent will be sought from each prospective subject or the subject’s legally
authorized representative, in accordance with, and to the extent required by federal
regulation and institutional polices.
Informed consent will be appropriately documented, in accordance with, and to the extent
required by federal regulation and institutional polices
If applicable, approve justification and document criteria is met for waiver of obtaining
informed consent or waiver for obtaining signed informed consent
When appropriate, the research plan makes adequate provision for monitoring the data
collected to ensure the safety of subjects
When appropriate, there are adequate provisions to protect the privacy of subjects and to
maintain the confidentiality of data.
Vulnerable Subjects. Additionally, when some or all of the subjects are likely to be vulnerable
to coercion or undue influence, the IRB reviewers must determine that additional safeguards
have been included in the study to protect the rights and welfare of these subjects.
Research approved previously by expedited review is considered eligible for expedited review at the
time of its regular continuing review if during the course of the study, the risks of the study have not
increased. Projects that were initially reviewed by the convened IRB continue to receive the same
type of review unless the IRB determines that the study meets the criteria for expedited review as
described in Category 8 or 9.
8.2
IRB Review Materials
When the IRB administrative staff has determined that a protocol is qualified for expedited review as
set forth in DHHS/FDA regulations, a qualified reviewer shall be chosen from the membership of the IRB
to complete the expedited review. One reviewer shall be assigned to each expedited review.
22
IRB Standard Operating Procedures
2014
The following materials are provided to the reviewer for expedited review applications:
9.0
IRB application(s);
Sponsor Protocol, if applicable;
Investigator Brochure, if applicable;
Informed consent document and/or script as appropriate;
If applicable, request for waiver of informed consent
Appropriate special population checklist, if applicable
Copies of surveys, questionnaires or videotapes;
Approval letter from external site where research is conducted outside USA entity;
Relevant grant application, if applicable;
Advertising materials, including email solicitations
Exemption from Continuing IRB Review
Research activities involving human participants that are exempt from the requirement that they
receive IRB full or expedited review are identified in 45 CFR 46.101(b)(1)-(6). Only the IRB may determine
which activities qualify for an exemption. The Investigators do not have the authority to make an
independent determination of research involving human participants or changes in ongoing research.
The IRB administrative staff will review the Request for Exemption Application and determine if the
project meets one of the six activities listed below. The determination that a research activity is eligible
for exempt review must be documented on the Request for Exemption Application. An investigator
may not initiate research involving human subjects that the investigator believes is exempt until the
investigator has received formal written concurrence of this exempt determination from the IRB.
Changes to exempted studies must be reviewed by the IRB just as amendments to studies receiving
expedited or convened IRB review. In some instances, changes to an exempted study may render it no
longer exempt.
9.1
Types of Research Eligible for Exempt Continuing Review
The following six categories of activities qualify for exempt review:
Category 1
Research conducted in established or commonly accepted educational settings,
involving normal educational practices, such as (i) research on regular and special education
instructional strategies, or (ii) research on the effectiveness of or the comparison among
instructional techniques, curricula, or classroom management methods; or
Category 2
Research not involving children that is limited to the use of educational tests, survey
procedures, interview procedures or observations of public behavior unless information obtained is
recorded in such a manner that human subjects can be identified, directly or through identifiers
linked to the subjects; and (ii) any disclosure of the human subjects' responses outside the research
could reasonably place the subjects at risk of criminal or civil liability or be damaging to the subjects'
financial standing, employability, or reputation. This exemption does not apply to research involving
children except for research involving observations of public behavior when the investigator does
not participate in the activities being observed, or interact directly with the children. All other
exemptions apply to research involving children. [45 CFR 46 101(b)(2) as modified by Subpart D 45
CFR 46.401 (b)]
23
IRB Standard Operating Procedures
2014
Category 3
Research involving the use of educational tests (cognitive, diagnostic, aptitude,
achievement), survey procedures, interview procedures, or observation of public behavior that is
not exempt under Category 2 of this section, if: (i) The human subjects are elected or appointed
public officials or candidates for public office; or (ii) federal statute(s) require(s) without exception
that the confidentiality of the personally identifiable information will be maintained throughout the
research and thereafter.
Category 4
Research involving the collection or study of existing data, documents, records,
pathological specimens, or diagnostic specimens, if these sources are publicly available or if the
information is recorded by the investigator in such a manner that subjects cannot be identified,
directly or through identifiers linked to the subjects.
Category 5
Research and demonstration projects conducted by or subject to approval of a
federal agency and designed to study, evaluate or otherwise examine some aspect of (i) Public
benefit or service programs; (ii) procedures for obtaining benefits or services under those
programs; (iii) possible changes in or alternatives to those programs or procedures; or (iv) possible
changes in methods or levels of payment for benefits or services under those programs.
Category 6
Taste and food quality evaluation and consumer acceptance studies, (i) if
wholesome foods without additives are consumed or (ii) if a food is consumed that contains a food
ingredient at or below the level and for a use found to be safe, or agricultural chemical or
environmental contaminant at or below the level found to be safe, by the Food and Drug
Administration or approved by the Environmental Protection Agency or the Food Safety and
Inspection Service of the U.S. Department of Agriculture.
9.2
Modifications of Exempt Studies
While no continuing review is required for exempt research, any proposed or anticipated changes in
the study must be submitted to the IRB for review and approval. Certain changes may disqualify the
research from receiving further administrative/exempt status.
If information comes to the attention of the IRB suggesting that there are factors increasing the sensitivity
and/or potential risk to human subjects in research that otherwise would appear to qualify for
exemption under the criteria listed above, the IRB may, in its sole judgment, deem the protocol to be
subject to expedited or convened IRB review.
10.0
Modifications to Previously Approved Projects
A modification is a change in an approved research protocol. IRB review and approval is
required before investigators can modify research protocols, except when necessary to
eliminate apparent immediate hazards to the subjects. Any proposed change to a
previously approved project must be submitted as an amendment to that project and may
be reviewed by the expedited review procedure or by the convened IRB, depending on
the IRB’s assessment of associated risk. Minor changes in previously approved research may
be approved by expedited review. Minor changes are those that do not significantly alter
the risks/benefits relationship or other study elements.
Modifications that might increase the risk to human subjects in a study or otherwise represent a
substantive change should be reviewed by the convened IRB. If an amendment requires convened
IRB review, at least one primary reviewer is assigned and the amendment is reviewed by the entire IRB,
as described for initial or continuing review.
24
IRB Standard Operating Procedures
2014
Modifications that have the potential to affect the subject’s willingness to continue participation will
be re-consented. This determination is made during the IRB review process and communicated by the
IRB to the study site via the modification approval letter.
11.0
Continuing Review of Approved Applications
Periodic review of research activities is necessary to determine whether the risk/benefit ratio has
changed, whether there are unanticipated findings involving risks to participants, and whether any new
information regarding the risks and benefits should be provided to participants. The IRB shall have
authority to observe or have a third party observe the consent process and the research. All research
protocols (except protocols determined by the IRB to qualify for administrative review) must be
periodically reviewed, including research for which data analysis is the only on-going research activity.
11.1
Criteria for Requiring Review More Often Than Annually
Intervals for continuing review, in the absence of problems, are often set to a default of one year.
However, the IRB may determine that more frequent intervals are appropriate. The IRB shall consider
the following factors in determining the criteria for studies requiring more frequent review:
Nature, probability and magnitude of anticipated risks to subjects;
Likely medical or psychological condition of the proposed subjects;
Overall qualifications of the investigator and other members of the research team;
Specific experience of the investigator and other members of the research team in
conducting similar research;
Nature and frequency of adverse events observed in similar research at this and other
facilities;
Vulnerability of the population being studied (this should be understood to include
unfamiliarity with the language used on consent forms and other printed matter intended
for subjects in the study);
Other factors the IRB deems relevant.
In specifying an approval period of less than one year, the IRB may define the period with either a time
interval or a research milestone, e.g. number of subjects enrolled. The minutes should clearly reflect any
determination requiring a review more frequently than annually.
11.2
Reminders/Notices:
When a research project is due for continuing review, an automated email notification is generated
via IRBNet and provided to the investigator (and, when applicable the Faculty Advisor for student
research) 60 and 30 days before the date of continuing review. If an application for renewal is not
received from the investigator by the expiration date, then an IRBNet generates an expiration notice
and is automatically emailed to the investigator. Copies of all reminders and expiration notices are
kept in the IRB protocol file.
11.3
Lapsed Studies:
A lapsed study is one for which the approval period has expired prior to the renewal of approval by the
IRB. If the investigator fails to submit the materials for continuing review within one month following the
expiration date, then the lapsed study will be classified as an administrative closure. Notification is
forwarded to the investigator ordering that all study-related measures must immediately cease except
those necessary for welfare of the human subjects.
25
IRB Standard Operating Procedures
2014
12.0
When can project be submitted to the IRB for study Closure
Research studies can be deemed complete for a number of reasons, each requiring a different degree
of IRB involvement. More often, however, the investigator or sponsor will close the study and the IRBs
role will be more passive, receiving study completion documents and archiving the records for the
study.
12.1
Voluntary Completion by Investigators
By submitting a Final Closure report, the researcher confirms that the study is finished and that
researchers have no further interaction with subjects or their data. Once the IRB receives and accepts
the Final Closure report form, the researcher is no longer required to submit for continuing review for
renewal. If the investigator wishes to enroll new subjects for the study, or otherwise engage human
subjects in research, he/she must reactivate the protocol with the IRB. Therefore, an investigator should
only close a study when he/she is no longer enrolling new subjects, using research interventions on
existing subjects, collecting data (including follow-up data), or performing any other tasks that were
identified as part of the approved study. A study will not invariably be considered completed when it is
closed to accrual, as research-related procedures may still be continuing. The IRB, in consultation with
the investigator, may consider closing a study when active data analysis and publication pursuant to
the approved study have ceased, even if the investigator retains records that may identify individual
subjects. Additional research projects using data acquired in the approved study may constitute new
human subjects research studies requiring to separate IRB review.
12.2
Termination of a Study by the IRB
In cases of serious adverse events or unanticipated problems, cases of researcher noncompliance, or
in cases of protocol violations, the IRB may suspend a study to ensure subject safety. Upon investigation
of the problem prompting suspension of the study, the convened IRB may decide that a study should
be terminated. Following the vote of the IRB to terminate a study and the evaluation of any appeals
made by the investigator, the study will be classified as closed. Though the chair may suspend a study,
pending IRB review, only the convened IRB may vote to terminate a study.
12.3
Expiration of Approval Period
Once the approval period for a given study has expired prior to the renewal of approval by the IRB, it
is considered a lapsed study and all research-related procedures must cease, except where doing so
would jeopardize the welfare of the human subjects. The IRB generates a notice of expiration letter
and electronically sends to the investigator and study coordinator, if applicable, indicating that
continuation of research studies is a violation of federal regulations, however if the subjects would be
harmed by halting the activities permission must be obtained by the IRB chair to continue research
study related activities. If the Investigator fails to submit the materials for continuing review within one
month following the expiration date, then the lapsed study will be classified as inactive. If the
investigator submits the materials for continuing review within one month following the expiration
date, the IRB will conduct continuing review and reactivate the protocol. This reactivation establishes
a new approval period that is not retroactive to the prior date of expiration. If the investigator desires
to continue a study that has lapsed for more than one month, then the investigator must submit a
new application for re-review by the IRB, and must receive IRB approval before resuming research
under the protocol.
26
IRB Standard Operating Procedures
2014
13.0
Adverse Events and Unanticipated Problems in Research
Investigators are responsible for prompt reporting to the IRB of "any unanticipated problems involving
risks to participants or others…" (45CFR46.103.b (5)). The IRB maintains responsibility for initial assessment
of the risk/ benefit ratio in a research activity involving human participants. During the course of the
project, investigators are required to promptly inform the IRB of any unanticipated negative effect or
undesirable experience that is possibly, probably or definitely related to study procedure(s).
Adverse events are not necessarily physical in nature; attention must be paid to psychological harm
(such as depression, thoughts of suicide, etc), threats to privacy or participant safety. An event is
considered serious and must be reported when the participant experiences an unusually strong
response, recurring problems, and/or death.
13.1
Definitions:
Adverse Event
The University's policies on adverse events are based on Food and Drug Administration regulations.
According to the FDA, a "serious adverse drug experience" with respect to human clinical experience
includes "any experience that suggests a significant hazard, contraindication, side effect, or
precaution," including "any experience that is fatal or life-threatening, is permanently disabling, requires
inpatient hospitalization, or is a congenital anomaly, cancer, or overdose."
Unexpected Adverse Event
An "unexpected adverse experience" is any adverse experience whose nature, severity, and frequency
of risk are not described in the information provided for IRB review or in the consent form. However, for
purposes of University policy, reportable “unexpected” events are as follows: 1) all adverse events that
are both serious and unexpected (even if not-drug related); 2) unexpected adverse events that are
mild/moderate and may be related to the study drug (in the PI’s opinion); and unexpected adverse
events that are clearly unrelated to the study drug do not have to be reported.
Unanticipated Problems
Unanticipated problems in a study, which might affect subject risk benefit analysis, confidentiality, or
subjects’ willingness to continue in a project are to be reported to the IRB. The IRB will consider the
effect of the problem on the study and on the subjects already enrolled.
In some instances, revisiting the consent process with previously enrolled subjects may be necessary. If
the problem prompts a change in the study, the consent process and documentation may require
alteration for future study subjects. The investigator should use his/her own judgment when determining
if an event is considered reportable beyond the scope of this policy. If there is a question, investigators
are encouraged to err on the side of “over-reporting” or contact the IRB Office at 460-6308 or Office of
Research Compliance and Assurance at 460-6625 for guidance.
Serious Adverse Event
A serious adverse event is defined as an adverse experience that results in any of the following
27
IRB Standard Operating Procedures
2014
outcomes:
a.
b.
c.
d.
death;
a life-threatening adverse experience;
inpatient hospitalization or prolongation of existing hospitalization;
a persistent or significant disability such to disrupt a person’s ability to conduct normal life
functions;
e. a congenital anomaly/birth defect;
f. causes cancer;
g. significant overdose or protocol error; or
h. certain medical events that may not result in death, be life-threatening, or require
hospitalization, may also be considered a serious adverse event when appropriate medical
or surgical intervention is necessary to prevent one of the outcomes listed above.
All serious adverse events that are unexpectedly associated with the study procedures must be
reported to the sponsor and the IRB immediately but no later than 7 working days upon learning of the
event using the USA Adverse Event Report Form. All deaths, whether or not they are directly related to
study procedures, must be reported. For the purpose of this policy, death is never expected. In
addition, any unexpected hospitalization of a research subject must be reported, even if the
hospitalization is unrelated to the study medication
13.2
Special Requirements for Research Involving the Gene Therapy Studies
Investigators who have received approval from FDA to initiate a human gene transfer protocol must
submit a written report of serious adverse events that are unexpected and associated with the use of
the gene transfer product to the NIH Office of Biotechnology Activities (NIH/OBA), the Institutional
Biosafety Committee, the IRB, and the FDA or study sponsor within specified timeframes as found in
Appendix M-1-C-4 in the NIH Guidelines for Research Involving Recombinant DNA Molecules (NIH
Guidelines). Gene therapy investigators must submit annual reports to OBA as set forth in Appendix M-1C-3 of the NIH Guidelines.
13.3
Internal vs External Reporting Requirements
Internal adverse event is an adverse event affecting a research subject who is at a USA study site. For
internal events, the USA IRB requires all serious adverse events and all unexpected adverse events to be
reported to the IRB office within the time table outlined below. Furthermore, any problems involving the
conduct of the study or subject participation at an USA study site, including problems with the
recruitment and/or consent processes, require reporting. Adverse events judged to be the result of
progressive disease need not be reported.
An external adverse event is an adverse event in a subject that is not at an USA study site. All
investigational drug and device studies that are industry-sponsored, the study sponsor typically provides
information regarding non-USA adverse events to the investigator. Therefore, the definition of an
external adverse event is defined according to the sponsor’s federal reporting requirements, pursuant
to 21 CFR 312.32 and 21 CFR 812.150. Study sponsors are required to notify investigators regarding
adverse events related to the study drug occurring at other study sites (external events). Notification of
these events are provided by the sponsor in an IND Safety Report or a MedWatch Report. These safety
reports which describe adverse events from different study sites should be forwarded to the IRB along
with a cover memorandum from the investigator or study coordinator outlining the pertinent
information.
28
IRB Standard Operating Procedures
2014
Adverse Event Reporting
TYPE OF EVENT
Mild or Moderate and unexpected – on-site (if related, possibly related,
probably not related)
Serious and unexpected – on-site
Serious and unexpected – external site
Serious and expected – on-site
Life-threatening – on-site (if related, possible related, probably not
related)
Death – on-site
Death – external site
Report to IRB
14 working days
7 working days
10 working days after receipt
from sponsor
14 working days
7 working days
3 working days from
notification
10 working days after receipt
from sponsor
This timeframe is considered the maximal time for reporting a death.
Title 45 and Title 21 of the Code of Federal Regulations, the USA IRB requires that a report be submitted in writing
for all unanticipated events.
13.4
IRB responsibilities following receipt of SAE/Follow-up Report
An Adverse Events Subcommittee of the IRB will review all adverse event reports and/or incident reports
in order to re-evaluate the risks/benefits of the study and/or the appropriateness of the
recruitment/consent process to determine if any changes should be made in the protocol or consent
form.. If the investigator has already modified the protocol or consent form in response to these events,
the appropriateness of these changes is also reviewed. The Adverse Events Subcommittee may
recommend additional review by the full IRB. The IRB office will provide acknowledgement of receipt of
this information and request additional information if follow-up or clarification is needed. The full
committee has the right to request additional information from the investigator, note the occurrence of
the adverse event but take no action, ask the investigator to modify the protocol or the informed
consent or suspend or terminate the project.
The IRB is responsible for continuing review of all human subject research. This is done through the
annual renewal process required for any ongoing study. Thus, all reported adverse events should also
be described in detail in the Annual Renewal Report Form when a renewal application is submitted for
the study, so that the IRB may consider renewal of the protocol in light of such information.
If the FDA or DHHS is involved, and if the problem is of sufficient magnitude, the appropriate agency
officials will be informed.
14.0
Safety Alerts, IND Safety Reports, MED Watch Reports
During the course of a study, the IRB may receive IND Safety Reports, MedWatch Reports, Data
Safety Monitoring Board (DSMB), problems involving risks to the subject or others or other adverse event
reports from the Sponsor. The IRB acknowledges such reports as the study progresses and the
investigator responsibilities are to ensure that the risk/benefit relationship of the research remains
acceptable. The investigators are accountable for determining the impact on continuation of the
29
IRB Standard Operating Procedures
2014
research, whether the informed consent requires revision, and whether subjects who are already
enrolled in the study need to be re-consented.
Investigators are required to submit the following reports per study sponsor
requirements:
Safety Updates*
IND Safety Reports
MedWatch Reports
SAE Reports for the study from other sites
DSMB reports*
Sponsor annual or interim reports*
* These documents are submitted for review at the time of continuing review for the protocol.
All other external reports are submitted to the IRB with a stamp on each report to include the
following information: study number, chance of occurrence at study site and signed/dated by
the Investigator.
If applicable, the IRB will inform investigators of their review and any required modifications in the
consent or reporting requirements.
15.0
Protocol Violations and Deviations
The IRB has the responsibility to oversee the conduct of research that it approves. Consistent with this
responsibility, the IRB may audit research studies at USA or studies in which faculty and/or staff of USA is
engaged in research outside the institution. The Director, Office of Research Compliance and
Assurance is responsible for conducting periodic and for-cause audits. As a result of an IRB audit, or in
the course of routine IRB business, incidents of noncompliance by investigators with federal regulations
or USA IRB policies may be identified. When these situations occur they are brought to the attention of
the IRB. The incidents of non-compliance are then reviewed and managed in one of several ways
depending on the severity of the non-compliance and the determination as to the willfulness of the
investigator. For each incident of non-compliance that is identified a plan of correction is documented.
Further audit may be required.
15.1
Defintions:
Non-compliance
Failure to comply with applicable Federal Regulations or USA IRB policies/guidelines
Serious non-compliance
An action or omission taken by an investigator or key research personnel that any other reasonable
investigator would have foreseen as compromising the rights and/or welfare of the subject. Examples
include, but not limited to:
Failure to adhere to federal regulations governing use of human subjects in research;
-
failure to obtain IRB approval prior to initiation of research activities
failure to notify the IRB of changes in approved procedures
30
IRB Standard Operating Procedures
2014
failure to obtain and/or document informed consent
IRB approval expires due to failure to renew
Failure to notify the IRB of changes in the scope/intent of the study
Failure to adhere to institutional policies where subject’s welfare has been adversely affected.
Continuing non-compliance
A pattern of repeated actions/omissions taken by an investigator or key research personnel that
indicates a lack of ability and/or willingness to comply with federal regulations or USA IRB
policies/guidelines.
15.2
Reporting Procedures:
Investigators are required to report protocol deviations to the IRB. Protocol deviations should be
reported at the time of continuing review or sooner, as determined by the level of risk to the subject.
Minimal risk protocol deviations are administratively reviewed, while greater than minimal risks deviations
are brought to the full convened board for review.
15.3
Review by the IRB Committee (Serious or Continuing):
All incidences of non-compliance determined to be serious or continuing will be presented to the IRB.
At a convened meeting, the IRB Chair and/or Director of Research Compliance and Assurance will
present the issue(s) to the IRB. IRB members will receive audit reports and communication from the
investigator. Members attending the meeting will review documents and determine whether:
There is no issue of serious and/or continuing non-compliance
There is serious and/or continuing non-compliance
More information is needed and determination is deferred to future meeting pending receipt of
additional information
If the investigator offers a timely and satisfactory explanation for the concern and a plan to eliminate
future incidents of such noncompliance and the IRB accepts, the IRB may elect to terminate the
noncompliance investigation process and report that the noncompliance issues were met with no
further action.
If the corrective action plan calls for any changes to the previously approved research and the
changes involves more than minor modifications, the modification must be reviewed by the convened
IRB. Minor changes will be reviewed by expedited review.
If the Investigator does not provide adequate information or corrective action plan, the IRB may ask the
investigator to meet with the chair or attend an IRB meeting to discuss the issue(s).
DHHS regulations at 45 CFR 46.103(a) and (b)(5) require unanticipated problems involving risks to
subjects, serious or continuing noncompliance, or suspension/termination of IRB approval conducted
under an approved assurance be reported to OHRP.
15.4
Actions That May Be Taken During or After the Investigation of Non-Compliance:
No action
Suspension: suspend enrollment and/or all research procedures for the specific research study in
31
IRB Standard Operating Procedures
2014
15.5
question
Termination of the research
Require a response from the investigator with a plan of corrective action
Initiate audits of all or some part of the investigator’s active protocols
Modification of the research protocol
Modification of the information disclosed during the consent process
Additional information provided to past participants
Modification of the annual review schedule
Acquire additional information pending final outcome
Requirements that current participants re-consent to participate (if applicable)
Monitoring of the research and/or consent process
Continuity of Care of Research Participants when study is suspended:
After the IRB has decided to suspend/terminate a research project, the IRB may make
recommendations to investigators regarding ongoing care and treatment of human subjects who had
been participating in research. The IRB shall take into consideration, the risk to the subjects from
withdrawal of any investigational drug or device or social or behavioral interventions can be continued
by another qualified physician or social/behavioral scientists and need further supervision of the
participant(s).
15.6
Final Outcome:
If a finding of research noncompliance has been made, the IRB chair, or in the case of serious or
continuing noncompliance, the IRB shall decide which corrective action(s) should be taken.
Corrective actions may include any of the following:
16.0
suspension or termination of the investigator’s research protocol(s);
required training with respect to human subjects research and the regulatory requirements for the
conduct of such research;
imposition of changes in such research protocol(s) to further protect Human Subjects;
a monitoring plan
imposition of restrictions as a condition for the continuation of research by the investigator
IRB Protocol Audits
The ORCA is responsible for compliance activities including routine and for-cause audits of IRB
approved protocols to ensure compliance with the protocol, federal and state regulations, and policies
protecting human subjects research. On-site audits are conducted as part of the Human Subjects
Protection continuing compliance oversight in accordance with federal regulations. The purpose of the
audit procedure is to ensure protection of the human subjects participating in research. The information
gathered during the audit is for the IRB to use to monitor the implementation of approved protocols,
identify areas that need improvement, correction or targeted education, and to gather information for
ways to improve the audit tool or the audit process. This process is viewed as an essential function to
maintain a high state of regulatory compliance within the institution. The following information provides
a detailed review of these procedures.
1.
This standard operating procedure applies to all personnel involved in the implementation and
32
IRB Standard Operating Procedures
2014
coordination of research involving human subjects. The auditing function is a core component
of the human subjects protection program and is performed on a proactive and for-cause basis.
2.
ORCA shall contact the principal investigator and the study coordinator, if applicable, in writing
to schedule a date and time for the on-site audit. Depending on the number of subjects
enrolled, a random sample of the subjects’ research records will be audited.
3.
An audit questionnaire will be used as a tool in conducting the audit. All regulatory
documentation and the entire study record are subject to review. A typical audit includes, but is
not limited to, review of regulatory information, protocol adherence, informed consent
documentation, IRB correspondence, adverse events, inclusion/exclusion criteria, drug
accountability, FDA 1572, financial disclosure statements, case report forms and source
documentation.
4.
Upon completion of each review, a written audit report is prepared. The report will be presented
by the ORCA at a scheduled monthly IRB meeting for review and discussion. The IRB may
recommend additional oversight if major deficiencies are observed.
5.
Post-audit procedures include a follow-up letter and copy of the written audit report forwarded
to the investigator and study coordinator, if applicable. If the audit identifies significant
problems or concerns, the principal investigator will be asked to respond in writing by a specified
date to acknowledge and address these issues. The report may include corrective actions
which are tracked to assure that investigator responds appropriately.
6.
Based on the scope and severity of identified problems, the following corrective actions may be
warranted by the IRB:
-
Acknowledgment of the problems, no sanctions required. However, additional information is
provided to the investigator(s) to avoid further infractions;
-
A temporary halt to new subject accrual, until an identified infraction is corrected, but
continued follow-up for subjects already enrolled is allowed;
-
Immediate suspension of the research project;
-
Reporting of IRB infraction(s) and actions to the appropriate academic department chair, dean,
and regulatory agencies such as the FDA, the Office of Human Research Protections, Office of
Research Integrity and/or the funding agency.
7.
Upon completion of the audit process, all audit reports are logged into the IRB database system
and officially complete.
8.
The ORCA will provide consultation and education to investigators and study coordinators who
conduct human subject research when warranted. By identifying noncompliance or potential
noncompliance, advising, and consulting with investigators and key personnel, ORCA insures
that the research operations involving human subjects minimize risks and meet University and
regulatory agency standards
9.
If suspected or alleged noncompliance (e.g., breach in IRB policy) is reported to the IRB office or
ORCA, a for-cause audit may be initiated. A for-cause audit is scheduled immediately, but
otherwise is conducted and reported as described for routine audits.
17.0 Recruitment and Advertisement Methods
33
IRB Standard Operating Procedures
2014
The IRB is charged with protecting the safety and welfare of human participants through providing a
review of the proposed research methodology, including recruitment and advertisement methods. The
IRB must prospectively review all aspects of recruitment as planned or envisioned by the Investigator,
along with all the information that the participant will see in the process of deciding whether to
participate in the research. IRBs and investigators should be aware that advertising for subjects is often
the first step in the informed consent process. When advertising is to be used, IRBs must review the
information contained in the advertisement, as well as the mode of its communication, to determine
whether the procedure for recruiting subjects affords adequate protection and is not misleading to
subjects.
Any advertisement to recruit subjects should state clearly that the project is human subjects research
and may include:
the name and contact information of the investigator;
the purpose of the research, and, in summary form, the eligibility criteria that
will be used to admit subjects into the study;
a straightforward and truthful description of the incentives to the subject for participation in the
study (e.g., payment);
the location of the research and the person to contact for further information;
an indication that the advertisement and the study described therein have been reviewed by
the appropriate IRB. (IRB date stamp for flyers)
If a study involves investigational drugs or devices, no claims should be made, either explicitly or
implicitly, that the drug/device is safe or effective for the purposes under investigation, or that the
drug or device is in any way equivalent or superior to any other drug or device. The IRB should
evaluate the proposed method of recruitment as it would be applied to students, employees or
trainees to make sure that recruitment materials are not presented in a manner that could suggest
that their decision regarding research participation could have an effect on their relationship with
instructors, mentors or employers.
17.1
Recruitment methods
17.2
Verbal recruitment (via telephone or in-person): investigators must provide the IRB with a oral script
of the verbal recruitment process.
Electronic recruitment (via email, web sites, or listservs): investigators must provide the IRB with a
version of the email script or web site view detailing the recruitment process and how consent will
be obtained. The IRB recommends that researchers follow procedures as outlined in the USA
guidance document entitled “Conducting Computer and Internet-Based Research Involving
Human Subjects”.
Recruitment by mail: Investigators must provide the IRB with materials that would be used for the
mailing campaign
Recruitment by advertisements: Investigators must provide the IRB with the intended proposed
advertisements, flyers, and ads used in the recruitment process. All newspaper advertisements
should adhere to USA’s Office of Public Relations template.
Recruitment Incentives
Investigators often use incentives to enhance research participation to include various methods by
offering gift certificates, vouchers, monetary compensation or class “extra credit”. The IRB will consider
whether paid participants in research are recruited fairly, informed adequately and paid appropriately.
When using funds obtained from University accounts, investigators must account for monies disbursed
34
IRB Standard Operating Procedures
2014
during the course of a project. This is a necessary component of financial auditing. However, this
accounting must be done in a way that participant confidentiality is not compromised. Using any type
of identifier will void confidentiality protection mechanisms and possibly contradict what the participant
was informed about in the consent document. Each expense should be tracked by participant ID, the
amount paid and when payment occurred and retained in the protocol file.
Investigators must provide the IRB with a full description of how extra-credit incentives will be used. As
with monetary incentives, a student may decline to participate in the research, but obtain extra-credit
by alternate assignment methods. The student who chooses to participate in the research will be
informed of the specific requirements to obtain extra-credit for participating in research, without
misleading, coercive, or deceiving information. All students must be ensured they will not be penalized
or their grade will not be adversely affected by their decision to not participate in the research.
17.3
Promotional materials
As stated in FDA's Information Sheet Guidance on "Recruiting Study Subjects," FDA requires that an
Institutional Review Board (IRB) review and have authority to approve, require modifications in, or
disapprove all research activities covered by the IRB regulations [21 CFR 56.109(a)]. An IRB is required to
ensure that appropriate safeguards exist to protect the rights and welfare of research subjects [21 CFR
56.107(a) and 56.111]. In fulfilling these responsibilities, an IRB is expected to review all the research
documents and activities that bear directly on the rights and welfare of the subjects of proposed
research. The protocol, the consent document and (for studies conducted under the Investigational
New Drug (IND) regulations) the investigator's brochure are examples of documents that the IRB should
review. The IRB should also review the methods and material that investigators propose to use to recruit
subjects.
The current IRB procedure is to "acknowledge" these materials (rather than facilitating a formal review
and signed approval letter). However, the IRB does review and approve materials used in media
advertising to recruit study subjects. If advertising materials used to recruit potential subjects (i.e.,
newspaper ads, radio script, television) are submitted AFTER initial approval, an amendment request
must be completed to facilitate review and approval. Additionally, all newspaper ads must be
approved for appropriate layout/design through Paul Taylor, Office of Public Relations.
It is the responsibility of the IRB to provide information based on its written standard operating
procedures, and not to deviate to serve specific requests by of study sponsors. It is time intensive to
provide study sponsors specific written documentation. The IRB needs to be consistent in following its
written procedures for handling this type of request for review of promotional or study guidance
materials.
17.4
External Investigators and Recruitment of Student Population
Investigators from external institutions periodically seek to recruit USA students to participate in a
research study on campus. For any USA faculty or administrator receiving an inquiry about participation
of USA students, the following steps should proceed to facilitate appropriate review of such requests:
Obtain IRB approval from the investigator’s home institution, accompanied by the proposal and active
recruitment method that will be used on USA’s campus
Departmental or administrative official must support the study and active on-campus recruiting
USA faculty or administrator submits information collected from the external institution to the USA IRB
Office
35
IRB Standard Operating Procedures
2014
18.0
USA IRB will evaluate the proposal
USA IRB may consider the external investigator’s home institution IRB review sufficient and grant
permission, request USA IRB approval or deny on-campus recruitment.
Informed Consent
The IRB recognizes that informed consent is a process to ensure that subjects are prospectively informed
to sufficiently make a voluntary decision regarding research participation. Thereby, the IRB ensures all
participants are informed about and voluntarily consent to research participation. Any individual
invited to participate in a research study should be given a description of the study that is clear and
complete enough for the individual to judge whether she or he wants to participate. The informed
consent process should be designed to provide potential subjects with readily understandable
information in an amount and timing appropriate to the level of risk in participating. As an IRB
approved best practice, the teach back method will be used to assess that the subject has at least a
basic understanding of what the research involves imparted above the standard of care. A consent
certification template is used to facilitate this process. The utilization of this practice will be
documented in the IRB Biomedical Research application within the informed consent section.
Consent documents must be written in language understandable to the participants or their authorized
representatives. For the typical participant population, use of language at a 6th-8th grade level of
schooling is recommended. The informed consent is a process; the face-to-face discussion the most
important part. The consent form is only a documentation of that process.
The subject’s consent must follow and not precede receipt of this information unless the IRB approves a
waiver or alteration of informed consent (as in some behavioral research that would be compromised
by full disclosure in advance). Consent must be obtained from each subject who is legally, mentally,
and physically able to provide it unless waived by the IRB. Consent should be in writing unless the IRB
finds that written documentation of informed consent may be waived. Consent forms and other
informational documents should be written in simple language to be easily understood by persons with
no technical background in the field.
No informed consent, whether oral or written, may include any exculpatory language through which
the subject or the subject’s authorized representative is made to waive or appear to waive any of the
subject's legal rights, or releases or appears to release the investigator, the sponsor, the institution or its
agents from liability for negligence.
The standard expectation is that all subjects will sign a document containing all the elements of
informed consent, as specified in the federal regulations and noted below. Some or all of the elements
of consent, including signatures, may be waived under certain circumstances.
Categories of consent may include: consent with documentation, consent without written
documentation or oral consent. The informed consent document MUST include the following
basic elements:
18.1
Basic Elements of Informed Consent:
Unless the IRB approves exceptions, the following information must be provided to the subject when
seeking informed consent:
36
IRB Standard Operating Procedures
2014
a)
A statement that the study involves research, an explanation of the purposes of the
research and the expected duration of the subject’s participation, a description of the
procedures to be followed, and identification of any procedures that are experimental;
b)
description of any reasonably foreseeable risks or discomforts to the subject;
c)
A description of any benefits to the subject or to others that may be reasonably
expected from the research;
d)
A disclosure of appropriate alternative procedures or courses of treatment, if any, that
might be advantageous to the subject;
e)
A statement describing the extent, if any, to which confidentiality of the records
identifying the subject will be maintained;
f)
For research involving more than minimal risk, an explanation about compensation
and/or medical treatments are available if injury occurs and, if so, what they consist of, or
where further information may be obtained;
g)
An explanation of whom to contact for answers to pertinent questions about the
research and research subject’s rights, and whom to contact in the event of a research related
injury to the subject, if relevant. Typically, questions concerning a research project should be
referred to the PI for that project, whereas questions concerning the rights of human subjects
should be referred to the IRB.
h) A statement that participation is voluntary, that refusal to participate will involve no penalty
or loss of benefits to which the subject is otherwise entitled, and that the subject may
discontinue participation at any time without penalty or loss of benefits to which the subject is
otherwise entitled.
18.2
Additional Elements of Informed Consent
For some studies, one or more of the following elements or information may be appropriate and
required by the IRB:
a)
A statement that the particular treatment or procedure may involve risks to the subject
(or to the embryo or fetus, if the subject is or may become pregnant) that are currently
unforeseeable;
b)
Anticipated circumstances under which the subject’s participation may be terminated
by the investigator without regard to the subject’s consent;
c)
Any additional costs to the subject that may result from participation in the research;
d)
The consequences of a subject’s decision to withdraw from the research and
procedures for orderly termination of participation by the subject (particularly when
potentially therapeutic experimental interventions are being administered and unscheduled
cessation of the intervention may pose health risks to subjects);
e)
A statement that significant new findings developed during the course of the research
that may relate to the subject’s willingness to continue participation will be provided to the
37
IRB Standard Operating Procedures
2014
subject;
f)
The approximate number of subjects involved in the study.
g)
When seeking informed consent for applicable clinical trials, as defined in 42 U.S.C.
282(j)(1)(A), the following statement shall be provided to each clinical trial subject in informed
consent documents and processes. This will notify the clinical trial subject that clinical trial
information has been or will be submitted for inclusion in the clinical trial registry databank
under paragraph (j) of section 402 of the Public Health Service Act. The statement is: "A
description of this clinical trial will be available onhttp://www.ClinicalTrials.gov, as required by
U.S. Law. This Web site will not include information that can identify you. At most, the Web site
will include a summary of the results. You can search this Web site at any time."
18.3
Exceptions to Informed Consent Requirements
The IRB may approve a consent procedure that does not include, or that alters, some or all of the
elements of informed consent set forth above, or waive the requirement to obtain informed consent
provided the IRB finds and documents that:
During the course of the consent process, investigators must:
a) Provide a copy of the consent form to the participant and/or legal
representative;
b) Keep a copy of the consent form for the approved protocol file
c) Seek consent only if the potential participant has the mental and legal capacity to give
consent; if not, consent must be obtained by a legal
representative;
d) Obtain parental permission for minor participants;
e) Provide sufficient opportunity to the potential participant or legal representative
to consider whether or not to participate;
f) Ensure that the possibility of coercion or undue influence is absent;
g) Enhance each participant’s comprehension of the information; and
h) Utilize a consent form appropriate to the age level.
Investigator(s) may propose a short form written consent document, stating that the elements of
informed consent required by 45 CFR 46.116 will be presented “orally” to the participant or the
participant's legally authorized representative. To do so, investigators must ensure the following:
a) That a witness be present during the oral consent delivery process.
b) Provide the IRB with a written summary of what is to be said to the participant or
the legal representative.
c) Inform the participant or legal representative that he or she only has to sign the short form
itself.
d) Ensure the witness shall sign both 1) the short form; and 2) a copy of the summary;
e) Ensure the person actually obtaining consent shall sign a copy of the summary
f) Provide the participant or legal representative a copy of the summary, in addition to a
copy of the short form.
Investigator(s) may request that the IRB waive certain requirements of the informed consent process
38
IRB Standard Operating Procedures
2014
if:
a) The research involves no more than minimal risk to the participants, and waiver will not
increase the risk; AND
b) The waiver or alteration will not adversely affect the rights and welfare of the participants;
AND
c) The research could not practicably be carried out without the waiver or
alteration (there is no reasonable alternative, without the waiver); AND
d) The participant will be given the opportunity to be debriefed immediately after
participation.
For research using protected health information, see also section 19.0 for additional criteria for waiver
or modification of HIPAA requirement for written authorization.
Investigator(s) may request that the IRB waive parental or guardian permission if:
a) the regular conditions for waiver of consent are met (45 CFR 46.116(c) or 46.117(d));
or
b) the study focuses on a condition for which parental or guardian permission is not a
reasonable requirement to protect the children and an appropriate mechanisms is
substituted, e.g. is of such private and sensitive nature that it is not reasonable to
require permission; or
c) a subject population for which parental or guardian permission is not a reasonable
requirement to protect the children and an appropriate mechanism is substituted
(e.g., abused or neglected children, 45 CFR 46.408)
18.4
Research related injury
The following three options in bold is IRB approved template language for research related injury for
studies greater than minimal risk. If industry sponsored, pick the option that best matches the
proposed contract language.
a. Sponsor pays for injury
If you are injured by being in this study treatment is available. The sponsor will pay for any
necessary medical costs related to the treatment of your injury. If you are injured,
there is no money set aside for lost wages, discomfort, disability, etc. You do not give up
your legal rights by signing this form. If you think you have a research related injury, please
call your study doctor.
Instruction:
a. If limiting treatment sites, the investigator must state specifically where the treatment
will be provided.
b. If the sponsor attaches conditions state them, e.g., if the subject has followed all the
instructions of the investigator, or if the investigator has followed all the procedures in
the research study.
39
IRB Standard Operating Procedures
2014
b. Sponsor pays what insurance does not pay for injury
If you are injured by being in this study, treatment is available. Your insurance will be
billed for the cost of treatment. The sponsor will pay for any necessary medical costs related
to the treatment of your injury due to your taking part in the study and not paid by your
insurance or any other payor. If you are injured, there is no money set aside for lost
wages, discomfort, disability, etc. You do not give up your legal rights by signing this
form. If you think you have a research related injury, please call your study doctor.
Instruction:
a. If limiting treatment sites, the investigator must state specifically where the treatment
will be provided.
b. If the sponsor attaches conditions state them, e.g., if the subject has followed all the
instructions of the investigator, or if the investigator has followed all the procedures in
the research study, or will pay for whatever your insurance will not cover.
c.
Sponsor does not pay for injury
If you are injured by being in this study treatment is available. The study site and/or your
study doctor have not set aside money to pay for treatment of any injury. You
and/or your insurance will be billed for the treatment of these injuries. Before you
agree to take part in this research study you should find out whether your insurance will
cover an injury in this kind of research. You should talk to the study doctor or staff about this.
If you are injured, there is no money set aside for lost wages, discomfort, disability, etc. You
do not give up your legal rights by signing this form. If you think you have a research
related injury, please call your study doctor.
18.5
Audio/Video Recordings
Subjects must be informed that the study will involve the use of audio and/or video recordings. In
addition, subjects should be informed whether or not these recordings are required to participate in
the study (if recording is optional, provide a space at the end of the consent document where
subjects initial to consent specifically for the audio and/or video recording).
Confidentiality should be addressed accordingly. The proposed use, management and storage of
these recordings should be well defined in the consent document. Examples include: how will the
study ensure the security of recordings, who will be transcribing the recordings, who will have access
to the recordings, and when will the tapes be erased/destroyed.
18.6
Consent for Mail and Telephone Surveys
The consent process for mail surveys can be handled in more than one way. The Investigator may
send the subject a letter requesting participation; the letter is accompanied by a conventional
consent form which the individual signs and returns with his/her survey. If the study is to be
anonymous, the consent form is separated from the survey immediately upon opening the package.
In the second way, the Investigator provides on the cover page of the survey the information
generally found in the consent form; also included there is a statement that by answering the
questions and returning the survey, the subject is providing and documenting his/her consent.
40
IRB Standard Operating Procedures
2014
For telephone surveys, the interviewer reads from a “script” written on the survey document. The
script contains a brief description of the study and includes the relevant elements of informed
consent in narrative form. The interviewer solicits any questions the potential subject may have and
answers them. The interviewer directly asks the person if he/she agrees to participate in the survey.
Lastly, the Investigator documents on a data sheet: 1) that the script was read, 2) the individual was
offered the opportunity to ask questions, and 3) the individual agreed or declined to participate in
the study. The script must be submitted to the IRB for review and approval prior to its use in the study.
18.7
Short Form Consent Procedures
There may be circumstances when a subject is unable to read the full consent document (e.g., when
the subject is illiterate or does not speak the language in which the consent document is written). In the
latter circumstance, the IRB expects that a translation of the full form will be provided. However, there
may be times when there is no opportunity to prepare a long form in advance; in such cases, a short
form may be used.
A short form is a written consent document stating that the required elements of informed consent have
been presented orally to the subject or the subject's legally authorized representative. When this
method is used, there shall be a witness to the oral presentation. Also, the IRB shall approve a written
summary of what is to be said to the subject or the authorized representative. Only the short form itself is
to be signed by the subject or the representative. However, the witness shall sign both the short form
and a copy of the summary, and the person actually obtaining consent shall sign a copy of the
summary. A copy of the summary shall be given to the subject or the representative, in addition to a
copy of the short form.
18.8
Waiver of Informed Consent
Investigators must complete the Request for Waiver of Consent form available in IRBNet
forms/templates and submit for IRB review and approval.
Waiver of Signed Consent
The IRB may waive the requirement for the investigator to obtain a signed consent form in cases where
circumstances warrant such a waiver. Such a waiver is allowable if:
The consent document is the only link between the subject and the research and the principal
risk of harm would come from a breach of confidentiality. Each subject will be asked whether
the subject wants documentation linking the subject with the research, and the subject’s wishes
will govern; or [45 CFR 46.117 (c)(1)]
The research presents no more than a minimal risk of harm to the subjects and involves no
procedures for which written consent is normally required outside of the research context. [45
CFR 46.117 (c)(2)]
In lieu of a signed consent form the IRB may require the investigator to provide subjects with a written
statement regarding the research in the form of an information or fact sheet. This statement should
contain, at a minimum:
A statement verifying that the project involves research;
A description of the level of involvement and amount of time expected from subjects;
A description of the study;
A description of the risks and benefits to subjects;
A statement describing the subject’s rights;
41
IRB Standard Operating Procedures
2014
A description of the compensation to be provided to subjects;
Contact information for both the investigator and the IRB.
Examples of circumstances in which a waiver of written consent may be granted include situations
where the researcher plans to use an abbreviated consent form, as in recruiting passersby for a brief,
minimal risk, procedure. Similarly, a waiver may be granted to allow researchers to obtain oral consent
for a survey of passersby or a telephone survey.
Finally, a waiver may also be granted if researchers wish subjects to imply their consent by returning a
survey via the mail or the internet. This last approach is especially useful in preserving the anonymity of
the subjects surveyed. In situations when anonymity of subjects is an important concern, investigators
should ensure that this anonymity is preserved in the process of compensating subjects for their
participation (e.g., obtaining social security numbers for check requests, etc.).
Waiver of Requirement for Informed Consent
An IRB may approve a consent procedure which does not include, or which alters, some or all of the
elements of informed consent set forth in this section, or waive the requirements to obtain informed
consent provided the IRB finds and documents that:
(1) The research involves no more than minimal risk to the subjects;
(2) The waiver or alteration will not adversely affect the rights and welfare of the subjects;
(3) The research could not practicably be carried out without the waiver or alteration; and
(4) Whenever appropriate, the subjects will be provided with additional pertinent information
after participation.
ALL FOUR (4) OF THE ABOVE REQUIREMENTS AS OUTLINED IN 45 CFR 46.116(d) MUST BE MET AND
DOCUMENTED BY THE IRB.
Example: The subject has entered the Emergency Room due to a trauma. They are unable to consent
and there is no Legally Authorized Representative present
18.9
Consent Form Templates
The IRB provides consent form template(s) that may be used for all written consent form documents.
This consent template contains all of the basic elements described above. For clarity and to assure
timely processing by the IRB, the consent form should follow the guidelines described above.
The consent form should be written at a level understandable to all potential participants and it must
contain all information that would reasonably inform the subject’s willingness to participate. In order to
facilitate this requirement, the IRB will provide templates that reflect appropriate language for various
subject populations. The consent form should be written in second person with “you” or “your child”
consistently used to refer to the subject in all statements.
The title of the project as listed on the consent form should be the same as the title listed on the
application form, though the IRB may suggest or require modifications in the title under certain
circumstances (e.g., in case the title would alert subjects to deception in the study or when the title
may be too explicit regarding subject criteria as in a study of dysfunctional parents).
The date on which the consent form was prepared or modified should be indicated on the form so
that revised forms can be easily distinguished from prior versions.
18.10
Assent by Minors
42
IRB Standard Operating Procedures
2014
Except under specific circumstances, assent to participate in a study must be obtained from minors (i.e.,
in Alabama, subjects aged 18 and under) who are capable of providing assent. The IRB shall determine
that adequate provisions are made for soliciting the assent of the minor (this includes providing age
specific language to the prospective subjects), when in the judgment of the IRB the children are
capable of providing assent. In determining whether children are capable of assenting, the IRB shall
take into account the ages, maturity, and psychological state of the children involved. This judgment
may be made for all minors to be involved in research under a particular protocol, or for each child
individually, as the IRB deems appropriate. If the IRB determines that the capability of some or all of the
minors is so limited that they cannot reasonably be consulted, or that the intervention or procedure
involved in the research holds out a prospect of direct benefit that is important to the health or wellbeing of the minors (such as in a study with therapeutic potential), and is available only in the context of
the research, the assent of the child is not a necessary condition for proceeding with the research. The
USA IRB guidelines with respect to obtaining consent from parents or legal guardians and assent from
minors is specified below:
1. In most cases, parental consent must be obtained if the research involves minors under the age of
19. The requirement for parental consent may be inappropriate in some cases such as research on
child abuse.
2. Minors 6 years of age or younger, verbal or written assent is typically not required. Consent is based
on the permission of the parent(s)/guardian(s) and no assent is required. A brief verbal explanation
of the research procedure should be explained to the child.
3. Minors 7 years or older should be involved in the decision to participate in a research projects unless:
a) the subject is not capable or mentally/emotionally, of being consulted, b) the IRB specifically
waives the requirement.
4. It is highly encouraged that a separate written assent form be used for children age 7 -12 years old
to document assent. In general, it should briefly explain in basic terms:
o they are being asked to participate in a research study;
o the purpose of the study;
o an estimate of how much time is involved in participating;
o what will happen to them if they agree to participate (e.g., ‘draw some blood’);
o foreseeable risks/discomfort and any benefits they may experience;
o they should ask their parents and doctor/researcher any questions they have about
participation;
o participation is voluntary and they can withdraw at any time
5. Typically, adolescents 13-18 years old (minors) should be fully informed about a study and give
assent to their own participation in the research. In the instance, both the adolescent and the
parents(s)/guardian(s) sign the form, with a signature line for the adolescent first. The signature line
for parental consent/permission should follow.
6. Assent expires when a child becomes an adult. At that time the subject must sign the IRB approved
adult consent for the research study.
Even where the IRB determines that the subjects are capable of assenting, the IRB may still waive the
assent requirement under circumstances in which consent may be waived in accord with 45 CFR
46.116.
18.11
Parental Permission
Unless otherwise provided by state law, or unless this requirement is waived by the IRB pursuant to 45
43
IRB Standard Operating Procedures
2014
CFR 46.408(c), the permission of the parent or legal guardian is required in order for minors to
participate in research. Where research is covered by 45 CFR 46.406 and 46.407, permission is to be
obtained from both parents unless one parent is deceased, unknown, incompetent, or not
reasonably available, or when only one parent has legal responsibility for the care and custody of
the child.
Per 45 CFR 46.408(c), in addition to the normal waiver requirements, the IRB may waive the parental
permission requirement if it determines that a research protocol designed for conditions or a subject
population for which parental or guardian permission is not a reasonable requirement to protect the
subjects. This waiver might apply to studies involving neglected or abused children, or older
adolescents presenting in medical situations wherein a parental consent requirement might deter
the child from seeking needed care (e.g., seeking care at an STD clinic). If parental permission is
waived, the IRB must be sure that an appropriate mechanism for protecting the children is
substituted. The choice of an appropriate mechanism would depend on the nature and purpose of
activities in the protocol, the risk and benefit to the subject, and their age, maturity, status, and
condition.
18.12
Surrogate Consent for Subjects Who Are Decisionally Impaired
There is an important distinction between the legal meaning of the term “incompetent” and our
broader use of the term “decisionally impaired.”
18.13
“Incompetence” is a finding of a court of law that results in the appointment of a
legally authorized representative for the individual judged incompetent by the court.
Decisionally impaired persons are those who have a diminished capacity for
autonomous decision making due to a psychiatric, organic, developmental or other
disorder that affects cognitive or emotional functions. Some adult individuals who
appear to be decisionally impaired may not have been declared legally incompetent.
For these individuals, there may not be a representative authorized under state law to
consent to the individual’s participation in research unless the individual had previously,
while of sound mind, executed a power of attorney broad enough to include consent for
the individual’s research participation.
Seek the guidance of University counsel if there are questions about legal
authorization for surrogate consent in specific situations.
Obtaining Consent from Non-English Speaking Subjects
The federal regulations for the protection of human subjects require that informed consent information
be presented in “language understandable to the subject” and, in most situations, that informed
consent be documented in writing (45 CFR 46.116 and 46.117). Where informed consent is
documented in accordance with 46.117(b)(1), the written consent document should embody, in
language understandable to the subject, all the elements necessary for legally effective informed
consent. Subjects who do not speak English should be presented with a consent document written in a
language understandable to them. Federal officials (DHHS Office of Human Research Protections)
strongly encourage the use of this procedure whenever possible.
Alternatively, 46.117(b)(2) permits oral presentation of informed consent information in conjunction with
a short form written consent document (stating that the elements of consent have been presented
orally) and a written summary of what is presented orally. A witness to the oral presentation is required,
and the subject must be given copies of the short form document and the summary. However, when
44
IRB Standard Operating Procedures
2014
performing research using non-English speaking subjects, the use of short form consent documents
should only be used when unexpected circumstances arise and there is not sufficient time to prepare a
full consent form translation. The short form should not be used as a convenient way to circumvent
translation of the full consent form. Additionally, when the subject population of any research study is
expected to include a significant number of subjects who are not fluent in English but are fluent in any
single language other than English, the IRB requires a full translation of the English version of the study’s
approved consent document (i.e, a long form consent document).
While the use of non-English speaking subjects presents a unique set of challenges for the researcher,
care must be taken not to exclude non-English speaking subjects from research that may have
potential benefits to this group of indiviudals.
18.13.1 Translation and Informed Consent
Attention should be paid to both oral interpretation and written translation in the informed consent
process.
Oral interpretation should be performed by a qualified individual who is not a family member of the
prospective subject. The individual performing the interpretation should be available for ongoing
communication between subjects and investigators.
Written translation of informed consent documents should be performed by a qualified individual.
Though there is no standard definition of what constitutes a “qualified individual,” the investigator
should demonstrate due diligence in obtaining an adequate translation of the informed consent
documents from an individual whose qualifications would appear adequate to a reasonable person.
Back translations to English may be one method for validating the accuracy of the translation.
Acceptable translators include the following, although all may not be appropriate for all types of
research:
An individual who is bilingual and fluent in both English and the language of the Non-English
speaking subjects, for minimal risk studies
A commercial entity that provides translations as a service to the public
An external sponsor such as NIH, NSF, or private industry
For Spanish translations, any translator.
For research that is greater than minimal risk, the translated document may be back-translated into
English by another individual who is also bilingual and fluent in both languages. If the research is a
minor increment over minimal risk, the IRB may waive the requirement of the back translation into
English.
18.14
Consent for Use of Stored Samples and Genetic Testing
In general, all anticipated uses of collected samples of human tissues, body fluids, or biological
products should be carefully delineated in the consent form. The University of South Alabama IRB
biological specimen language and/genetic testing must be used. The study sponsor language
should not be used in place of the USA IRB approved language. Do not duplicate if using multiple
consent documents.
If genetic testing is to be done on the collected sample, the consent form should disclose the specific
genetic information to be obtained, whether the information may be of value to the subject, whether
and how that information will be disclosed or made available to the human subject and, if so, whether
genetic counseling will be available at the subject’s option.
45
IRB Standard Operating Procedures
2014
If specimens are to be collected and stored for as yet unspecified purposes (genetic testing or
otherwise), this should be addressed in the consent form or in an addendum. The IRB provides
templates addressing these issues located in IRBNet forms/templates. An addendum to the consent
may be used when specimen storage is secondary to the main purpose of the study.
The consent form and process for maintaining human specimens in a repository for future research
uses must inform the subjects explicitly about the unspecified possible future use of the specimens
and related personal information. The consent process must include the following:
How the sample will be stored and possibly used in future research studies.
A description of any personal information about the specimen source will be maintained
(this may or may not include identifiers).
If no personal identifiers will be used for labeling the stored samples, i.e., if it is impossible for
the sample to be linked with the subject, the consent form should so state.
If personal identifiers are to be used that will allow future matching of the subject to the
collected sample, the consent form should describe how they will be used, how privacy and
confidentiality will be protected, whether and under what circumstances identifying
information would be disclosed.
Future research using the samples will be reviewed by the IRB prior to additional use of the
samples
Whether and how researchers may contact individuals whose specimens are in the
repository
A statement about any potential commercialization and that there are no plans
for subjects to share in financial proceeds that may accrue from products derived
from the specimens.
18.15
Whether and under what circumstance and how any results from research studies using
the specimens would be communicated to or available to the human subjects, if, for
example, the information gathered also applied to family members.
If specimens are individually identifiable, how the specimens and associated data may
be withdrawn from the repository. If the specimens are not individually identifiable, a
statement that they may not be withdrawn for that reason.
Revised Informed Consent and Reconsenting
As informed consent is an ongoing process, if, during the course of the trial, the protocol has been
modified in such a way that changes are made to the informed consent, subjects who have already
given their informed consent may be required by the IRB to be reconsented using the updated form
with the changes bolded. All participants currently enrolled in the study must sign the bolded copy of
the updated informed consent form to acknowledge the changes. The subject may be reconsented at
the next patient contact unless otherwise stated by the IRB or study sponsor.
For potential subjects who are not yet enrolled in the study, the revised informed consent replaces all
previous versions for the informed consent and is used in its clean format. Informed Consent is obtained
as described above.
46
IRB Standard Operating Procedures
2014
18.16
Stamped Copies of Consent Forms
All approved consent forms will bear the IRB approval stamp which includes the current approval
period. The IRB requires that copies signed by participants include a stamp of approval.
18.17
Record Retention of Informed Consent Forms
As with all protocol related materials, a copy of the approved consent documents should be retained
by the IRB for a minimum of three (3) years following closure of the study.
19.0
HIPAA and IRB Review
HIPAA stands for the “Health Insurance Portability & Accountability Act of 1996” (Public Law 104-191). In
essence, the Rule specifies the actions required to protect the security and privacy of personally
identifiable health care information and establishes the conditions for its use and disclosure. In the
course of conducting research, researchers may obtain, create, use, and/or disclose individually
identifiable health information. Under the Privacy Rule, covered entities are permitted to use and
disclose protected health information (PHI) for research provided an individual gives written
authorization to use or disclose PHI unless such authorization is waived or excepted by an IRBs or Privacy
Board. The use of decedent’s information is protected by the Rule but authorization is not required.
The USA IRB will conduct the following HIPAA review and approval responsibilities within the larger
context of its responsibilities such as:
Review and approval of all authorization documents
Review and approval of all waivers of authorization, included limited waivers of authorization for
access, use and/or disclosure of PHI for University research purpose.
The Privacy Rule does not replace or modify the human research protection regulations found in 45
CFR 46. The Privacy Rule exceeds privacy provisions found in 45 CFR 46 as it extends to decedents,
applies to all research, regardless of funding or activity and extends the definition of “identifiable
information”.
As defined by the regulations, examples of identifiable health or protected health information
include names, telephone numbers, fax numbers, electronic mail addresses, social security
numbers, Internet protocol (IP) address numbers, finger and voice prints and full face photographic
images and any comparable images.
The HIPAA Privacy Rule only applies if investigators use, receive and/or disclose protected health
Information (PHI) from a covered entity in the course of doing research with human participants or
human participant data. USA’s activities include both HIPAA covered and non-covered
functions; the University is considered a “hybrid” HIPAA entity covering the USA Health System (i.e.,
USA Hospitals, USA Physician’s Group, Speech Pathology and Audiology, Psychology Clinic,
Mitchell Cancer Institute, Center for Strategic Health Innovations and Center for Healthy
Communities). Investigators who are not employed or are involved with research falling under the
jurisdiction of the University’s hybrid entity are not covered by HIPAA; therefore, HIPAA regulations
do not apply. However, confidentiality of data collected must be maintained.
47
IRB Standard Operating Procedures
2014
Review of medical records and ePHI: Designation is made in IRBNet for projects involving retrospective
chart review and tagged
(PHI – Medical Records) and / or projects involving electronic
personal health information, which includes the development and completion of the Research Database
Registration Form which will be tagged
(ePHI – dBase)
These two designations / tags
are shared with Linda Hudson and Thad
Phillips for their review. (USAMC Privacy and Security Officers) An automated email is generated and routed
through IRBNet as a notification that reviewer access has been granted. The email will contain a deadline
request for the date of completion. If the review has not been completed within the requested timeframe,
a second email notification will be generated to ensure timely review.
19.1
HIPAA Authorization and Informed Consent
The authorization document must include all elements defined in the HIPAA regulations as
described in the USA HIPAA in Research Compliance Plan. The full compliance plan is available
on the Office of Research Compliance and Assurance website at:
http://www.southalabama.edu/com/research/hipaa.shtml Researchers must generally obtain
authorization for the use of PHI from the human subjects who’s PHI will be included in the study.
The HIPAA authorization is incorporated into the informed consent within the confidentiality
section. The USA IRB provides an authorization template that complies with HIPAA requirements.
The researcher must customize the authorization template for the specific study he/she intends to
perform. The USA IRB approved HIPAA Authorization template is located in IRBNet, Forms/
Templates.
The following differences in procedures for signing an authorization are outlined below:
Adults: A competent individual 19 years of age and older, should always sign the authorization to
use or disclose his/her PHI. (the general ability to understand the concept of releasing his/her
medical information).
Minors: Any parent or legal guardian may sign an authorization for a minor child in
his/her legal custody. HIPAA does not require that an assent document specifically
for research participation include any version of a HIPAA authorization.
19.2
HIPAA Security
The IRB application collects information on the maintenance of electronic identifiable health
information (e-PHI) for each indiviudal study. If e-PHI is maintained, a separate application for the
establishment of a research database or repository is submitted by the study site for review and
approval. There are several key components that are evaluated during the review process to include
the following, 1) workstation use for sending, receiving, storing, or accessing e-PHI information; 2)
workstation security; 3) transmission security and implementing measures to protect the security of EPHI
when transmitted electronically from one point to another; and 4) development of a contingency plan
for the establishment of procedures for the “continuation of business” if the main system goes down.
48
IRB Standard Operating Procedures
2014
Additionally, a risk analysis is conducted to evaluate safeguards and vulnerabilities to the
confidentiality, integrity and availability of e-PHI. The Office of Research Compliance and Assurance
utilizes a survey instrument for collection of the information. Additionally, periodic physical/technical
security inspections are conducted by USA’s HIPAA Security Officer.
20.0
Behavioral and Social Science Research
Behavioral and Social Sciences research often involves surveys, observational studies, personal
interviews, or experimental designs involving exposure to some type of stimulus or intervention.
Social and Psychological Harms
When evaluating behavioral and social science research, the IRB carefully examines the research to
determine the probability of risk of harm to subjects.
The IRB considers the potential for participants to experience stress, anxiety, guilt, or trauma that
can result in genuine psychological harm.
The IRB also considers the risks of criminal or civil liability or other risks that can result in serious social
harms, such as damage to financial standing, employability, insurability, or reputation;
stigmatization; and damage to social or family relationships.
If information is being collected on living individuals other than the primary “target” subjects the IRB
considers the risk of harm to those “non-target” individuals, as well.
To mitigate such risks, the IRB reviews the proposal for appropriate preventive protections and
debriefings, adequate disclosure of risks in the informed consent information, and mechanisms to
protect the confidentiality and privacy of persons participating in or affected by the research.
Privacy and Confidentiality Concerns
The use of confidential information is an essential element of much social and behavioral and
educational research.
It is important to ensure that the methods used to identify potential research subjects or to gather
information about subjects do not invade the privacy of the individuals. In general, identifiable
information may not be obtained from private (non-public) records without IRB approval and the
informed consent of the participant. This is the case even for activities intended to identify
potential participants who will later be approached to participate in research. However, there are
circumstances that are exempt from the regulations, and circumstances in which the IRB may
approve a waiver of the usual informed consent requirements.
It is also important to ensure that adequate measures are taken to protect individually identifiable
private information once it has been collected to prevent a breach of confidentiality that could
lead to a loss of privacy and potentially harm participants.
When information linked to individuals will be recorded as part of the research design, the IRB ensures
that adequate precautions are taken to safeguard the confidentiality of the information. The more
sensitive the data being collected, the more important it is for the researcher and the IRB to be familiar
with techniques for protecting confidentiality. The 45 CFR 16.116(a)(5) regulations and the Common
Rule require that subjects be informed of the extent to which confidentiality of research records will be
maintained.
49
IRB Standard Operating Procedures
2014
The IRB may require that an investigator obtain a Department of Health and Human Services (DHHS)
Certificate of Confidentiality (CoC). The CoC protects against the involuntary release of sensitive
information about individual participants for use in Federal, state, or local civil, criminal, administrative,
legislative, or other legal proceedings.
20.1
20.2
Types of Risk found with Social/Behavioral Research
A.
Breach of confidentiality
B.
Violation of privacy
C.
Validation of inappropriate or undesirable behaviors of participants
D.
Presentation of results in a way that does not respect the participants’ interests
E.
Possible harm to individuals not directly involved in the research, but about whom data are
obtained indirectly (secondary participants), or who belong to the class or group from which
participants were selected
F.
Harm to participants’ dignity, self-image, or innocence as a result of indiscreet or ageinappropriate questions in an interview or questionnaire that results in embarrassment,
harassment, or stigmatization
G.
Harm to a participant because of exposure to potential for criminal or civil liability and/or
damage to financial standing or employability
Research Involving Deception or Withholding of Information.
Where deception is involved, the IRB needs to be satisfied that the deception is necessary and that,
when appropriate, the participants shall be debriefed. (Debriefing may be inappropriate, for example,
when the debriefing itself would present an unreasonable risk of harm without a corresponding benefit.)
The IRB will also make sure that the proposed subject population is suitable. The regulations make no
provision for the use of deception in research that poses greater than minimal risks to participants. The
IRB considers the following issues when reviewing research that involves deception:
A.
The scientific value and validity of the research.
B.
The ability to obtain the information without the use of deception.
C.
Whether the deception used will influence the participants’ willingness to participate.
D.
The possibility of harm to the participant and a plan for debriefing which must be conducted as
soon as possible after the conclusion of the study. Participants should be given the opportunity
to withdraw their participation from the study after debriefing by requesting that any data
collected from them be deleted and/or destroyed.
E.
The possibility that the deception may cause invasions of privacy.
This information is requested in the IRB application form.
The employment of deception by an investigator(s) for the purpose of securing subject participation
and/or to prevent potentially biased reporting of data/information by the subject is permissible
provided all of the following conditions exist:
50
IRB Standard Operating Procedures
2014
Deception is necessary due to the lack of alternative procedures for data collection not
involving deception;
The deceptive procedures will not place subjects at significant financial, physical, legal,
psychological, or social risk;
The data collection/experiment will be followed by careful debriefing sessions whereby the
subjects are fully informed of the nature and purpose of the deception; and
The procedures for deception must meet the guidelines established by the discipline of the
investigator through its professional code of ethics.
20.3
DebriefingIn order for the IRB to adequately review the research, investigators should justify, in
detail, in the protocol, the reasons for deceiving or withholding information from subjects, including an
explanation of:
(a) the necessity for deceiving subjects; (b) how potential benefits of the research justify the use of
deception; and (c) how the investigators will conduct the debriefing. In
addition, investigators should include a debriefing script or statement that indicates the
information subjects will receive regarding their participation in the research.
The IRB in collaboration with the investigator will determine whether subjects should be
debriefed either after unwittingly participating in the research or after knowingly participating in
research that involved deception. The IRB may require debriefing when it contributes to the
subject’s welfare, i.e., when it corrects painful or stressful misperceptions, or when it reduces
pain, stress, or anxiety concerning the subject’s performance. For example, if a subject is lead
to believe through participation in deception research that she/he has committed a crime or has
a disease, a debriefing session may correct the induced stress, pain, and/or anxiety.
20.4
Oral Histories
Oral history interviewing projects generally do not involve the type of research as defined by DHHS
regulations and therefore are excluded from IRB oversight. However, if the project does not fall within
the guidelines below it does require IRB review and routine application submission procedures apply.
For purposes of this SOP, projects fulfilling the following criteria are considered to be an oral history
project and do not require IRB review:
(a) Oral history projects involve interviews that are explicitly intended for preservation as a
historical document.
(b) Projects involving oral history interviews that are not designed to contribute to generalizable
knowledge as the 45 CFR part 46 regulations describe. The project does not seek underlying
principles or laws of nature that have predictive value nor can it be applied to other
circumstances for the purposes of controlling outcomes.
(c) Projects involving oral history narrators that are not anonymous individuals selected as part of
a random sample for the purposes of a survey. Individuals are selected due to their unique
relationship to the topic and the questions are gradually developed and open-ended.
(d) Projects involving oral history interviews where the historian (PI) follows the Oral History
Associations Principles and Standards and Evaluation Guidelines as part of his or her work.
(e) Oral history projects involve interviews in which those being interviewed fully understand the
purposes, potential uses and their freedom not to answer questions. In most cases, the narrators
51
IRB Standard Operating Procedures
2014
are required to sign a release that addresses copyright and terms of access and reproduction
(for interviews deposited in a library or archives), identification of narrators, and disposition of
tapes
21.0
Review of Research Using Data and Specimens
Many studies combine characteristics of behavioural and social research with characteristics of biomedical
research. There are many interdisciplinary combinations of behavioral and medical research. They often
use or create tissue, specimen, or data repositories (banks).
21.1
Prospective Use of Existing Materials
Prospective studies are designed to observe outcomes or events (e.g., diseases, behavioral outcomes,
or physiological responses) that occur subsequent to identifying the targeted group of participants,
proposing the study, and initiating the research.
o
o
21.2
Prospective studies using materials (data, documents, records or specimens) that will
“exist” in the future because they will be collected for some purpose unrelated to the
research (e.g., routine clinical care) do not qualify for exemption under regulations at 45
CFR 46.101(b)(4) and the Common Rule because the materials in these studies are not
in existence at the time the study is proposed and initiated.
However, the IRB may utilize expedited procedures (under expedited category #5,) to
review research that proposes to use materials (i.e., data, documents, records, or
specimens) that will be collected in the future (i.e., after the research has been
proposed and initiated) for non-research purposes (e.g., clinical observations, medical
treatment, or diagnosis occurring in a non-research context).
Retrospective Use of Existing Materials
Retrospective studies involve research conducted by reviewing materials (data, documents, records,
or specimens) collected in the past (e.g., medical records, school records, or employment records)
and existing at the time the research is proposed and initiated.
o
o
o
Such research may be exempt under regulations at 45 CFR 46.101(b)(4) if the
information is publicly available or if the information is recorded in such a manner that
participants cannot be identified, either directly or through identifiers linked to the
participants.
If not exempt, the IRB may review such research utilizing expedited procedures,
provided that the research involves no more than minimal risk to participants
However, retrospective studies using existing materials occasionally entail significant,
greater than minimal risks and require review by the convened IRB (e.g., where the
research reveals previously undisclosed illegal drug use and the expedited review had
concerns about invasion of participants’ privacy and/or the adequacy of
confidentiality protections proposed by the investigators).
52
IRB Standard Operating Procedures
2014
21.3
Research Using Data or Tissue Banks
Human data repositories collect, store, and distribute Identifiable information about individual persons
for research purposes. Human tissue repositories collect, store, and distribute identifiable human tissue
materials for research purposes.
Tissue and Data Bank activities involve three components: (a) the collectors of data or tissue samples;
(b) the bank/repository storage and data management center; and (c) the recipient investigators.
Under a repository arrangement, the IRB formally oversees all elements of repository activity, setting the
conditions for collection, secure storage, maintenance, and appropriate sharing of the data and/or
tissues with external investigators. Specifically, the IRB determines the parameters for sharing data
and/or tissues (which are identifiable within the repository) including whether additional informed
consent of subjects is required. Typically, these parameters involve formal, written agreements
stipulating conditions as follows:
o
o
o
o
The repository shall not release any identifiers to the investigator.
The investigator shall not attempt to recreate identifiers, identify participants, or contact
participants.
The investigator shall use the data only for the purposes and research specified.
The investigator shall comply with any conditions determined by the repository IRB to be
appropriate for the protection of participants.
RESEARCH USING FDA-REGULATED PRODUCTS
22.0
Research involving an Investigational Drug or Device
The information below applies to Investigators and to Investigators who may also be
sponsors holding an Investigational New Drug (IND) or Investigational Device Exemption (IDE)
for the test article under study:
When the principal intent of the investigational use of a test article is to develop
information about the product’s safety or efficacy, an IND or IDE may be required. If an IND
or an IDE is required, it is the investigator’s responsibility to submit the appropriate application
to the FDA, obtain the necessary documentation, and provide this documentation to the IRB as
a part of the approval process.
o An IND may not be necessary if all of the conditions stated in 21 CFR 312.2(b)(1) have
been met. If the Investigator does not already have an IND, IRB approval will remain
pending until receipt of an IND. If there is a debate regarding the need for an IND, the
IRB will require that the Investigator contact the Food and Drug Administration (FDA)
to obtain written documentation that an IND is not necessary.
o The IRB will review protocols involving investigational devices to determine if the device is a
“Significant-Risk device” (SR) or a “Non-Significant Risk”(NSR) device. If the IRB
determines that the research involves a SR device, an IDE is necessary. If the PI does
not already have an IDE, the Investigator will be notified that IRB approval is
pending receipt of an IDE.
Protocols involving an Investigational Drug (IND) or Investigational Device (IDE) require
consideration and satisfaction of the pertinent FDA and the DHHS regulations (21 CFR 50, 21
CFR 56, 21 CFR 312, 21 CFR 812, and 45 CFR 46). When the USA Investigator is acting as the
sponsor of research involving an investigational drug, the IRB requires that the Investigator
submit documentation that the proposed drug preparation has been reviewed and
53
IRB Standard Operating Procedures
2014
compliance with Current Good Manufacturing Practices has been confirmed. In addition,
the IRB requires that the Investigator review the reporting and record-keeping responsibilities
as stated in 21 CFR 312 and 21 CFR 314 (for investigational drugs) or 21 CFR 812 and 21 CFR
814 (for investigational devices).
The Investigator is responsible for assuring the IRB that investigational drugs and devices are stored
in a secure and safe manner and that the storage and safety requirements are consistent with
FDA, sponsor, and affiliated research institutions’ storage requirements for drugs or devices of
the type under study. Whenever possible, the storage of drugs and biologics should be under
the supervision of a registered pharmacist and stored in the pharmacy in a limited access,
locked area. Devices should be stored according to manufacturer’s specifications and
maintained in a limited access area. Access to the test devices must be limited only to those
authorized to use the devices.
The protocol for the study should outline the security and storage plan for the test article(s)
indicating that the plan meets the sponsor’s storage and security requirements. The plan
should include whether or not control will be through a hospital pharmacy and under the
supervision of a registered pharmacist or held in a proper and secure storage area by the
investigator. The protocol should detail how the test article is used in human subjects, indicate
who may have access to the test article(s) and outline the accountability plan for the test
article(s) to ensure that there is no unapproved access to or use of the test article(s).
Protocols involving an IND or IDE will undergo initial and continuing review at a convened
meeting that includes at least one physician or pharmacist unless the protocol meets the
criteria for expedited review (i.e., all treatment components complete, in follow-up only, data
analysis only).
Consent for studies involving an IND and/or IDE will be obtained. Although FDA regulations
allow waiver of consent if research meets the criteria specified in 21 CFR 50.23 or 21 CFR
50.24 and DHHS regulations allow a waiver of consent if research meets the criteria specified in
45 CFR 46 “Waiver of Informed Consent Requirements in Certain Emergency Research,”
consent is required for all non-emergency research that falls under FDA regulations or involves
experimental treatment, tests, or drugs. In addition, the consent form will identify the test
article as investigational and will inform participants that the FDA may inspect research
records.
The Investigator who is a sponsor will provide the IRB with all documentation provided by the
FDA indicating whether or not that sponsor has complied with FDA regulations dealing with
sponsor responsibilities.
22.2
Determination of Need for an IND
Studies that involve FDA-regulated products that are submitted without a valid IND number will
be reviewed with respect to determining the need for an IND, based on the investigator’s
response to questions contained in the IRB application form.
If the IRB determines that the study is exempt from an IND and approves the study, the study
may begin without submission of an IND application to FDA. If the IRB determines that an IND is
needed, the investigator/sponsor must submit an IND application to the FDA and provide
documentation of the outcome of the FDA determination (IND number) to the IRB before the IRB
approves the study.
The IRB may consider a study using a drug product that is lawfully marketed in the United States to
be exempt from the requirements for obtaining an IND if all the following apply:
1.
The investigation is not intended to be reported to FDA as a well-controlled study in support of
a new indication for use nor intended to be used to support any other significant change in
54
IRB Standard Operating Procedures
2014
2.
3.
4.
5.
the labeling for the drug;
If the drug that is undergoing investigation is lawfully marketed as a prescription drug
product, the investigation is not intended to support a significant change in the
advertising for the product;
The investigation does not involve a route of administration or dosage level or use in a patient
population (e.g., children, prisoners, pregnant women and fetuses) or other factor that
significantly increases the risks (or decreases the acceptability of the risks) associated with
the use of the drug product;
The investigation is conducted in compliance with the requirements for institutional review
and with the requirements for informed consent; and
The investigation is conducted in compliance with the requirements with regard to
promotion and charging for investigational drugs in 21 CFR 3 12.7.63
A clinical investigation involving an in vitro diagnostic biological product that is a blood grouping
serum, reagent red blood cells, or anti-human globulin is exempt from the requirements for an IND
if (a) it is intended to be used in a diagnostic procedure that confirms the diagnosis made by
another, medically established, diagnostic product or procedure and (b) it is shipped in
compliance with 21 CFR 312.160.
A drug intended solely for tests in vitro is exempt from the requirements of an IND if it is shipped in
accordance with 21 CFR 312.160.
A clinical investigation involving use of a placebo is exempt from the requirements of an IND if
the investigation does not otherwise require submission of an IND.
22.2
Determination of Significant Risk (SR) vs. Non-significant Risk (NSR) for Non-Exempt Medical
Devices
For determination of the need for an IDE, the convened IRB will address the applicability of
FDA regulations under 21 CFR 812.2 and, if necessary, make a significant risk determination. The
Investigational Device Exemption (IDE) regulations [21 CFR part 812] describe two types of device
studies, "significant risk" (SR) and "nonsignificant risk" (NSR). For both SR and NSR device studies,
IRB approval prior to conducting clinical trials and continuing review by the IRB are required. In
addition, informed consent must be obtained for either type of study [21 CFR part 50].
A Significant Risk (SR) device study is one that presents a potential for serious risk to the health,
safety, or welfare of a subject and
o is intended as an implant; or
o is used in supporting or sustaining human life; or
o is for use of substantial importance in diagnosing, curing, mitigating or treating disease, or
otherwise prevents impairment of human health; or
o otherwise presents a potential for serious risk to the health, safety, or welfare of a subject.
A Non-significant Risk (NSR) device investigation is one that does not meet the definition for a SR
study.
The risk determination is based on the proposed use of a device in an investigation, and not on
the device alone. In deciding if a study poses an SR, the IRB considers the nature of the harm
that may result from use of the device. Studies where the potential harm to subjects could be
life threatening, could result in permanent impairment of a body function or permanent
damage to body structure, or could necessitate medical or surgical intervention to preclude
permanent impairment of a body function or permanent damage to body structure is
55
IRB Standard Operating Procedures
2014
considered SR. Also, if the subject must undergo a procedure as part of the investigational
study, e.g., a surgical procedure, the IRB considers the potential harm that could be caused
by the procedure in addition to the potential harm caused by the device.
FDA has the ultimate decision in determining if a device study is SR or NSR.
If an investigator or a sponsor proposes the initiation of a claimed NSR investigation to an IRB,
and if the IRB agrees that the device study is NSR and approves the study, the investigation
may begin at that institution immediately, without submission of an IDE application to FDA.
To help in the determination of the risk status of the device, an investigator is asked to include
the sponsor’s (including the investigator on investigator-initiated studies) assessment of whether or
not a device study presents a significant or non-significant risk. The investigator must provide the IRB
with a description of the device, reports of prior investigations with the device, the proposed
investigational plan, a description of subject selection criteria, and monitoring procedures.
The investigator must inform the IRB whether other IRBs have reviewed the proposed study and
what determination was made. The investigator must inform the IRB of the FDA’s assessment of
the device's risk if such an assessment has been made. The IRB may also consult with FDA for its
opinion.
22.3
Controlling Distribution and Disposition of Devices
Although investigators are responsible for ensuring that investigational devices are made
available only to persons who are legally authorized to receive them (see 21 CFR 812.110(c)),
sponsors also bear responsibility for taking proper measures to ensure that devices are not
diverted outside of legally authorized channels. Sponsors may ship investigational devices
only to qualified investigators participating in the clinical investigation (§ 812.43(b)). Sponsors
must also maintain complete, current, and accurate records pertaining to the shipment
and disposition of the investigational device (§ 812.140(b)). Records of shipment shall include
the name and address of the consignee, type and quantity of device, date of shipment, and
batch number or code mark. Records of disposition shall describe the batch number or code
marks of any devices returned to the sponsor, repaired, or disposed of in other ways by the
investigator or another person, and the reasons for and method of disposal.
To further ensure compliance with these requirements, sponsors should take appropriate
measures to instruct investigators regarding their responsibilities with respect to recordkeeping
and device disposition. The specific recordkeeping requirements for investigators are set forth at §
8 12.140(a). Upon completion or termination of a clinical investigation (or the investigator's
part of an investigation), or at the sponsor's request, an investigator is required to return to the
sponsor any remaining supply of the device or otherwise to dispose of the device as the sponsor
directs (§ 812.110(c)).
22.4
Supplemental Applications
Supplemental applications are required to be submitted to, and approved by, FDA in the
following situations:
1. Changes in the investigational plan: FDA approval is required for any change that may
affect the scientific soundness of the investigation or the rights, safety or welfare of the
subjects. IRB approval is also required for changes that may affect the rights, safety or welfare of
the subjects. The change in the investigational plan may not be implemented until FDA
approval (and IRB approval, if required) is obtained.
56
IRB Standard Operating Procedures
2014
2. Addition of new institutions/facilities: IRB approval is also required for new
institutions. The investigation at the new institution(s) may not begin until both FDA and IRB
approval(s) are obtained, and certification of IRB approval is submitted to FDA.
22.5
Submitting Reports
A sponsor shall prepare and submit the following complete, accurate, and timely reports.
1.
Unanticipated adverse device effects (with evaluation) to FDA, all IRBs, and investigators within 5
working days after notification by the investigator. Subsequent reports on the effect may be
required by FDA.
Withdrawal of IRB approval
Withdrawal of FDA approval
Current 6 month investigator list
Annual progress report
Recall and device disposition (within 30 working days after the request was made)
Final report
Use of device without obtaining patient informed consent
Significant risk determinations by the IRB when proposed to be nonsignificant risk
Other reports requested by the IRB or FDA
2.
3.
4.
5.
6.
7.
8.
9.
10.
23.0
Device Studies in Pediatric Populations
Because the pediatric population represents a particularly vulnerable group, specific measures
are needed to protect the safety of pediatric study subjects. Adult devices may be
inappropriate for use in pediatric subjects for a variety of reasons, or may require specific
design changes and/or specific labeling to accommodate their use in pediatric subjects. We
recommend that you consider the following when developing devices or plan a clinical trial for
devices intended for pediatric subjects:
24.0
height
weight
growth and development
disease or condition
hormonal i nfl uences
anatomical and physiological differences from the adult population
activity and maturity level
immune status
Emergency Use of an Investigation Drug or Biologic
The FDA human subjects regulations allow for an investigational drug/device to be used in emergency
situations without prior IRB approval. Emergency use is defined as a life-threatening situation in which
no standard acceptable treatment is available and in which there is not sufficient time to obtain IRB
approval for the use. These are typically situations in which the intent is not to conduct research but to
act in the best interest of an individual patient. Nonetheless, the FDA requires IRB involvement. The
health care provider is still required to obtain informed consent under these circumstances. The
emergency use must be reported to the IRB in writing within 5 working days.
The written report submitted to the IRB chair must include a cover letter explaining the medical
condition, reason for use, and date administered as well as a copy of the signed informed consent
document. The health care provider must also include any manufacturer information available on the
57
IRB Standard Operating Procedures
2014
product (e.g., drug brochure). Once the health care provider has provided written notice, the IRB chair
or his/her designee responds in writing that the information has been received. This acknowledgement
of the IRB receipt does not constitute IRB approval.
Written informed consent must be obtained prior to administration or use unless the emergency
situation makes it not feasible to obtain informed consent prior to using the test article. Exemption from
the informed consent requirement is granted only when: (1) a life-threatening situation necessitates use
of the test material; (2) the subject is unable to provide effective consent; (3) there is insufficient time in
which to obtain consent from the subject's legal representative; and (4) there is no available
alternative method of approved or generally recognized therapy of equal or greater likelihood of
saving the subject's life.
The health care provider must document the infeasibility of obtaining consent as follows: The health
care provider and a physician who is not participating in the clinical investigation must certify in writing
the existence of all four conditions listed above before use of the test article. If in the health care
provider's opinion, immediate use of the test article is necessary to save the life of the subject and there
is insufficient time to obtain the independent determination before using the test article, the health
care provider is to make his or her own written determinations, then obtain the written review and
independent evaluation of a physician who is not participating in the clinical investigation. The
documentation of the infeasibility of obtaining informed consent must be submitted to the IRB within
five working days after the use of the test material. The IRB will respond to this report with an
appropriate letter.
Although this procedure is designed to permit only a single emergency use of a test material for the
treatment of one patient by one physician within the University, it is not intended to limit the authority of
a physician to provide emergency care in a life-threatening situation. Should a situation arise that
would require the emergency use of the test material for a second patient, by either the same or a
second physician, subsequent emergency use should not be withheld for the purpose of gaining IRB
approval. If it appears probable that similar emergencies will require subsequent use of the test
material at the University, the health care provider should submit a protocol for future use of the article.
The protocol must be prospectively reviewed and approved by the IRB before future use of the test
material.
The use of a test material in a prospective investigation designed to be conducted under emergency
conditions (e.g., emergency room or intensive care research) does not qualify for the emergency use
exemption. 56.104 21 CFR 56.
25.0
Exceptions from informed consent requirements for emergency research
Even for an emergency use, the investigator is required to obtain informed consent of the subject
or the subject's legally authorized representative unless both the investigator and a physician
who is not otherwise participating in the clinical investigation certify in writing in the
patient/subject’s medical record all of the following [21 CFR 50.23(a)]:
The subject is confronted by a life-threatening situation necessitating the use of the test
material.
Informed consent cannot be obtained because of an inability to communicate with, or
obtain legally effective consent from, the subject.
Time is not sufficient to obtain consent from the subject's legal representative.
No alternative method of approved or generally recognized therapy is available that
provides an equal or greater likelihood of saving the subject's life.
58
IRB Standard Operating Procedures
2014
If, in the investigator's opinion, immediate use of the test material is required to preserve the
subject's life, and if time is not sufficient to obtain an independent physician's determination that
the four conditions above apply, the clinical investigator should make the determination and,
within 5 working days after the use of the material, have the determination reviewed and
evaluated in writing by a physician who is not participating in the clinical investigation. The
investigator must notify the IRB within 5 working days after the use of the test material [21 CFR
50.23(c)].
The IRB will review the submitted documents and will indicate the regulatory basis for the
emergency use and that its use was appropriate. Data obtained from such emergency use may
not be published or otherwise used for research purposes. Submission of a research protocol by
the investigator is required if future use of the test material is anticipated.
26.0
Emergency Use of Unapproved Medical Devices
An unapproved medical device is defined as a device that is used for a purpose or condition for
which the device requires, but does not have, an approved application for premarket approval
under section 515 of the Federal Food, Drug, and Cosmetic Act [21 U.S.C. 360(e)]. An unapproved
device may be used in human subjects only if it is approved for clinical testing under an approved
application for an Investigational Device Exemption (IDE) under section 520(g) of the Act [21 U.S.C.
360(j)(g)] and 21 CFR part 812. Medical devices that have not received marketing clearance under
section 5 10(k) of the FD&C Act are also considered unapproved devices which require an IDE.
The Food and Drug Administration (FDA) recognizes that emergencies arise where an
unapproved device may offer the only possible life-saving alternative, but an IDE for the device
does not exist, or the proposed use is not approved under an existing IDE, or the physician or
institution is not approved under the IDE. Using its enforcement discretion, FDA has not objected if a
physician chooses to use an unapproved device in such an emergency, provided that the
physician later justifies in writing to FDA that an emergency actually existed.
26.1
Requirements for Emergency Use
Each of the following conditions must exist to justify emergency use:
a.
b.
c.
the patient is in a life-threatening condition that needs immediate treatment;
no generally acceptable alternative for treating the patient is available; and
because of the immediate need to use the device, there is no time to use existing
procedures to get FDA approval for the use.
FDA expects the physician to determine whether these criteria have been met, to
assess the potential for benefits from the unapproved use of the device, and to
have substantial reason to believe that benefits will exist. The physician may not
conclude that an "emergency" exists in advance of the time when treatment may
be needed based solely on the expectation that IDE approval procedures may
require more time than is available. Physicians should be aware that FDA expects
them to exercise reasonable foresight with respect to potential emergencies and to
make appropriate arrangements under the IDE procedures far enough in
advance to avoid creating a situation in which such arrangements are
impracticable.
59
IRB Standard Operating Procedures
2014
FDA would expect the physician to follow as many subject protection procedures as
possible. These include:
26.2
obtaining an independent assessment in writing, documented in the
patient/subject’s medical record by an uninvolved physician;
obtaining informed consent from the patient or a legal representative;
notifying institutional officials as specified by institutional policies;
notifying the Institutional Review Board (IRB); and
obtaining authorization from the IDE holder, if an approved IDE for the
device exists.
After-Use Procedures
After an unapproved device is used in an emergency, the physician should:
report to the IRB within five days [21 CFR 56.104(c)] and otherwise comply with
provisions of the IRB regulations [21 CFR part 56];
evaluate the likelihood of a similar need for the device occurring again, and if future use is
likely, immediately initiate efforts to obtain IRB approval and an approved IDE for
the device's subsequent use; and
if an IDE for the use does exist, notify the sponsor of the emergency use, or if an IDE
does not exist, notify FDA of the emergency use and provide FDA with a written
summary of the conditions constituting the emergency, subject protection measures,
and results.
Subsequent emergency use of the device may not occur unless the physician or another
person obtains approval of an IDE for the device and its use. If an IDE application for
subsequent use has been filed with FDA and FDA disapproves the IDE application, the device may
not be used even if the circumstances constituting an emergency exist. Developers of
devices that could be used in emergencies should anticipate the likelihood of emergency use
and should obtain an approved IDE for such uses.
27.0
Reporting the Use of a Test Material (Drug, Biologic or Device) to the IRB
The investigator’s written report is presented at the next appropriate IRB meeting. When an
IRB receives a report by an investigator of an emergency use, the IRB examines the case to assure
that the emergency use was justified and that the emergency use complied with FDA regulations.
Using FDA guidance, the IRB will determine if the emergency use was justified and document the
IRB’s decision in the minutes of the meeting.
The written report submitted to the IRB must include a cover letter explaining the medical
condition, reason for use, and date administered as well as a copy of the signed Informed
Consent Document. The investigator must also include any manufacturer information available
on the product from the manufacturer (e.g., drug brochure).
Once the investigator has provided written notice, the use is assigned a IRB tracking number,
and the chair or his/her designee responds in writing that the information has been received.
60
IRB Standard Operating Procedures
2014
Although this procedure is designed to permit only a single emergency use of a test article for
the treatment of one patient by one physician within the University or affiliated institutions, it is
not intended to limit the authority of a physician to provide emergency care in a life-threatening
situation. Should a situation arise that would require the emergency use of the test article for a
second patient, either by the same or a second physician, for the same test article, subsequent
emergency use should not be withheld for the purpose of gaining IRB approval. If it appears
probable that similar emergencies will require subsequent use of the test article at the University
or affiliated institutions, every effort should be made either to sign on to the sponsor's protocol or
to develop a protocol for future use of the article at the institution. Either of these protocols
would need to be prospectively reviewed and approved by the IRB for future use of the test
article.
28.0
Treatment Use of an Investigational Drug or Device
The IRB reviews the use of investigational drugs/devices if the investigator provides evidence that
a treatment IND or IDE has been obtained or as single patient use (below). In all cases,
treatment use of an investigational drug or device requires prospective IRB approval as well
as subject informed consent.
28.1
Single Patient (Non-emergency Use)
In non-emergency situations, physicians may obtain investigational drugs for use outside of a
controlled clinical trial for a single patient. This is often referred to as “compassionate use.”
Usually, the patient is in a desperate situation and unresponsive to other therapies, or no
approved or generally recognized treatment is available. There may be little evidence that the
proposed therapy is useful, but it is thought to be plausible on theoretical grounds or anecdotal
evidence. Access to investigational drugs for use by a single, identified patient may be gained
either through the sponsor under a treatment protocol, or through the FDA, by first obtaining the
drug from the sponsor and then submitting a treatment IND to the FDA requesting
authorization to use the investigational drug for treatment.
IRB approval is also required prior to administration of the investigational drug. The approval is
granted for the treatment of a single patient. When an investigator desires to obtain single
patient use approval, the investigator submits an application and the study is assigned a
University IRB identification number and sent through the new application procedure. The
treatment use may occur only after IRB approval is obtained. Subsequent treatment use
requires FDA approval for a treatment IND or IDE.
Every single patient use must be reviewed and approved by the IRB as well as the FDA, and all
requirements for informed consent must be met. Although the FDA may waive local IRB review
for a Single Patient Use, the University IRB Policy does not permit such waivers and will not
allow a Single Patient Use without the prior review and approval of the IRB.
28.2
Humanitarian Use Device (HUD)
Humanitarian use of investigational devices is prospectively reviewed by the IRB. The
investigator is required to submit a new application for review. Included in the application must
be evidence that the investigator/sponsor has obtained a Humanitarian Device Exemption
(HDE) from the FDA. These projects are subject to the same new and continuing review
requirements as research projects as outlined in this document. The use of such devices is
61
IRB Standard Operating Procedures
2014
approved only for the purposes noted in the FDA approval letter.
additional information on Requirements for Humanitarian Use Device.
29.0
See Appendix D for
Biologics
IRBs have certain responsibilities when reviewing protocols that include the use of biologics. If
biologics are administered as part of a research protocol, their IND status should be specified.
Vaccine trials fall under the IND regulations. However, they differ from drugs in that: (a) they are not used
to diagnose or cure disease in afflicted individuals, but to prevent a disease in a healthy human; and,
(2) they are used to protect people with a high statistical risk for contracting a particular disease.
Information concerning the dosage, route of administration, previous use, and safety and efficacy
data need to be evaluated along with the phase of testing.
In the review of a protocol involving biologics, the IRB will consider the following:
a. Protocol: Has appropriate FDA clearance and IND approval been obtained? Is there
evidence that the vaccine has been tested in animal trials and in the laboratory? What is
the severity of the disease to be avoided? Does this protocol require NIH RAC and
Biosafety Committee Review?
b. Benefits: What is the direct benefit to the individual subject? Possibility of immunity? To
society as a whole?
c. Risks: What is the likelihood that subjects will be exposed to the infectious disease?
What is the likelihood that the subject will suffer adverse consequences should he / she
contract the disease? What are the adverse events and known complications of the
vaccine therapy? In relation to the infectious disease? Is there any chance of allergic
or anaphylactic reaction?
d. Recruitment: Will adult and pediatric subjects be vaccinated? Are any subgroups
particularly susceptible to side effects i.e. elderly, young, immunocompromised? How
will subjects be recruited? Is this a Phase I trial where low risk subjects will be vaccinated?
Will there be a control group?
e. Monitoring: What provisions has the sponsor made for monitoring the trial? Is there a
DSMB? Does the protocol provide adequate plans to monitor all subjects for immune
status and adverse reactions, respond to problems, and disseminate results?
SPECIAL POPULATIONS
It is the policy of the University of South Alabama IRB to review, approve, and provide guidance on the ethical
and regulatory considerations when special populations are involved in human subjects research. Special
protections are essential to guide research involving vulnerable persons. FDA regulations and the Common Rule
require IRBs to give special consideration to protecting the welfare of vulnerable subjects. At the same time,
there are also requirements that members of specific populations be permitted or encouraged to become
human research subjects to ensure that specific populations are adequately represented in research and have
access to potential benefits of such research. The IRB is required to ensure that it has adequate board
representation or the input of appropriate external consultants to consider specific kinds of research involving
these special populations.
62
IRB Standard Operating Procedures
2014
30.0
Definitions:
Assent: An individual’s affirmative agreement to participate in research obtained in conjunction with
permission from the individual’s parents or legally authorized representative. Mere failure to object
should not, absent affirmative agreement, be construed as assent. Children/Minors: According to
Federal regulations, children are “persons who have not attained the legal age for consent to
treatments or procedures involved in the research. In Alabama, individuals are adults and of legal age
(released from parental authority), when one attains the age of 19 years. Minors are those individuals who
have not attained the age of nineteen years.
Dissent: An individual’s negative expressions, verbal and/or non-verbal, that they object to participation
in the research or research activities.
Legally Authorized Representative: An individual, judicial, or other body authorized under applicable
law to grant permission on behalf of a prospective participant for their participation in research
activities.
Greater than Minimal Risk: The probability and magnitude of harm or discomfort anticipated in the
research are greater than those ordinarily encountered in daily life or during the performance of routine
physical or psychological examinations or tests.
Minimal risk: The probability and magnitude of harm or discomfort anticipated in the research are not
greater in and of themselves than those ordinarily encountered in daily life or during the performance
of routine physical or psychological examinations or tests. An example of minimal risk is the risk of
drawing a small amount of blood from a healthy individual for research purposes (because the risk of
doing so is no greater than the risk of doing so as part of a routine physical examination).
31.0
Elements to Consider in Research Involving Special Populations
32.0
The methods of recruitment, selection and the inclusion/exclusion criteria should be
considered by the IRB, as should informed consent, the confidentiality of data, and
the willingness of the subjects to volunteer.
Group characteristics such as economic, social, physical and environmental
conditions should be considered to ensure that the research includes appropriate
safeguards for the protection of vulnerable subjects.
Applicable state or local laws that bear on the decision-making abilities of
potentially vulnerable populations.
Research studies involving potentially vulnerable subject groups should have
adequate procedures in place for assessing and ensuring subjects’ capacity,
understanding and informed consent or assent. In some cases, researchers should
be expected to enhance understanding for potentially vulnerable subjects.
Whether or not additional safeguards are necessary to protect vulnerable subjects,
such safeguards could include IRB monitoring of the consent process or the
creation of a waiting period between contact and enrollment to allow for family
questions.
Decisionally Impaired Subjects
Decisionally impaired persons are those who have a diminished capacity for autonomous decision
making due to a psychiatric, organic, developmental or other disorder that affects cognitive or
emotional functions. Other individuals who may be considered decisionally impaired, with limited
decision-making ability, or individuals under the influence of or dependent on drugs or alcohol, those
63
IRB Standard Operating Procedures
2014
suffering from degenerative diseases affecting the brain, terminally ill patients, and persons with
severely disabling physical handicaps. There are no regulations specific to research involving
cognitively impaired persons.
The National Bioethics Advisory Commission (NBAC) has issued 21 recommendations for IRBs, the
research community, and Federal regulators to consider regarding the decision-making capacity of
particularly vulnerable participants. The complete report, “Research Involving Persons with Mental
Disorders That May Affect Decision Making Capacity” (December 1998), can be found on-line at
http://bioethics.gov/capacity/TOC.htm.
33.0
Surrogate Permission with Subjects Judged Incompetent to Consent
Where consistent with state law, the IRB recognizes as legally authorized representatives:
Court appointed guardians.
Next of kin in the following order: spouse, adult child, parent, and adult sibling.
Surrogate consent may be used only when the prospective participant is incompetent as determined
by a medical or psychological authority, as appropriate, who is not otherwise associated with the study,
after appropriate mental or medical evaluation, and there is little or no likelihood that the participant
will regain competence within a reasonable period of time, or as established by legal determination.
This definition of incompetence is not limited to the legal definition but also may also be a clinical
judgment that a person lacks the capacity to understand the circumstances of participating in
research and to make an autonomous decision to take part.
Aside from issues of who may give legal permission for research participation of individuals who are
decisionally impaired, there are many issues the IRB must consider in deciding whether to approve the
possible participation of decisionally impaired persons in the research study.
IRBs should take special care to consider issues such as (1) whether decisionally impaired persons may
be suitable subjects for this project; (2) whether, if the study is of more than a minor increase over
minimal risk, the study holds out the prospect of direct benefit to the individual in a risk-benefit ratio at
least as favorable to the subject as that presented by available alternative approaches; (3) whether
the informed consent process can be structured to be appropriate and effective within the limits of the
individual’s decisional capacity; (4) if surrogate consent will be used, whether assent will also be
required; and (5) whether there are any circumstances under which a surrogate decision maker may
enroll a decisional impaired individual in the study over the individual’s objection or resistance.
34.0
Research Involving Pregnant Women, Human Fetuses and Neonates
IRBs must consider that research involving women of childbearing potential might involve pregnant
women (and viable fetuses), and should evaluate research protocols and risks, inclusion and exclusion
criteria, and informed consent procedures, with this in mind.
The following HHS regulations must be applied before an IRB approves research that will deliberately
include pregnant women:
Conditions required for pregnant women or fetuses to be involved in research:
64
IRB Standard Operating Procedures
2014
(a) Where scientifically appropriate, preclinical studies, including studies on pregnant animals, and
clinical studies, including studies on nonpregnant women, have been conducted and provide
data for assessing potential risks to pregnant women and fetuses; (45 CFR 46.204(a))
(b) The risk to the fetus is caused solely by interventions or procedures that hold out the prospect of
direct benefit for the woman or the fetus; or, if there is no such prospect of benefit, the risk to
the fetus is not greater than minimal and the purpose of the research is the development of
important biomedical knowledge which cannot be obtained by any other means; (45 CFR
46.204(b))
(c) Any risk is the least possible for achieving the objectives of the research; (45 CFR 46.204(c))
(d) If the research holds out the prospect of direct benefit to the pregnant woman, the prospect of
a direct benefit both to the pregnant woman and the fetus, or no prospect of benefit for the
woman nor the fetus when risk to the fetus is not greater than minimal and the purpose of the
research is the development of important biomedical knowledge that cannot be obtained by
any other means, her consent is obtained in accord with the informed consent provisions of
subpart A of this part; (45 CFR 46.204(d))
(e) If the research holds out the prospect of direct benefit solely to the fetus then the consent of the
pregnant woman and the father is obtained in accord with the informed consent provisions of
subpart A of this part, except that the father's consent need not be obtained if he is unable to
consent because of unavailability, incompetence, or temporary incapacity or the pregnancy
resulted from rape or incest; (45 CFR 46.204(e))
(f) Each individual providing consent under paragraph (d) or (e) of this section is fully informed
regarding the reasonably foreseeable impact of the research on the fetus or neonate; (45 CFR
46.204(f))
(g) For children as defined in §46.402(a) who are pregnant, assent and permission are obtained in
accord with the provisions of subpart D of this part; (45 CFR 46.204(g))
(h) No inducements, monetary or otherwise, will be offered to terminate a pregnancy; (45 CFR
46.204(g))
(i) Individuals engaged in the research will have no part in any decisions as to the timing,
method, or procedures used to terminate a pregnancy; (45 CFR 46.204(i))
and
(j) Individuals engaged in the research will have no part in determining the viability of a neonate
(45 CFR 46.204(j))
Consent Decision Chart for Pregnant Women and Fetuses
65
IRB Standard Operating Procedures
2014
Direct benefit to
mother only
Direct benefit to
mother and fetus
Direct benefit to
fetus only
No direct benefit or societal
benefits only
Risk is more than
minimal
Mother's consent
Mother's consent
Mother and
father's consent
NOT APPROVABLE BY IRB
Risk is no more
than minimal
Mother's consent
Mother's consent
Mother and
father's consent
Mother's consent
34.1
Neonates
Conditions required for neonates of uncertain viability and nonviable neonates to be involved in
research:
A neonate is defined as a newborn child. The following HHS regulations apply to research involving
neonates:
(a) Neonates of uncertain viability and nonviable neonates may be involved in research if all
of the following conditions are met:
1. Where scientifically appropriate, preclinical and clinical studies have been
conducted and provide data for assessing potential risks to neonates (45 CFR
46.205(a)(1)).
2. Each individual providing consent under paragraph (b)(2) or (c)(5) of this section
is fully informed regarding the reasonably foreseeable impact of the research on
the neonate (45 CFR 46.205(a)(2))
3. Individuals engaged in the research will have no part in determining the viability
of a neonate (45 CFR 46.205(a)(3))
4. The requirements of paragraph (b) or (c) of this section have been met as
applicable (45 CFR 46.205(a)(4)).
(b) Neonates of uncertain viability. Until it has been ascertained whether or not a neonate is
viable, a neonate may not be involved in research covered by this subpart unless the following
additional conditions are met:
1. The IRB determines that:
i.
The research holds out the prospect of enhancing the probability of survival of the
neonate to the point of viability, and any risk is the least possible for achieving that
objective, or
ii.
The purpose of the research is the development of important biomedical knowledge
which cannot be obtained by other means and there will be no added risk to the
neonate resulting from the research; and
66
IRB Standard Operating Procedures
2014
2. The legally effective informed consent of either parent of the neonate or, if neither parent
is able to consent because of unavailability, incompetence, or temporary incapacity, the
legally effective informed consent of either parent's legally authorized representative is
obtained in accord with subpart A of this part, except that the consent of the father or his
legally authorized representative need not be obtained if the pregnancy resulted from rape
or incest.
(c) Nonviable neonates. After delivery, a nonviable neonate may not be involved in
research covered by this subpart unless all of the following additional conditions are met:
1.
Vital functions of the neonate will not be artificially maintained;
2.
The research will not terminate the heartbeat or respiration of the neonate;
3.
There will be no added risk to the neonate resulting from the research;
4.
The purpose of the research is the development of important biomedical
knowledge that cannot be obtained by other means; and
5.
The legally effective informed consent of both parents of the neonate is
obtained in accord with subpart A of this part, except that the waiver and
alteration provisions of §46.116(c) and (d) do not apply. However, if either
parent is unable to consent because of unavailability, incompetence, or
temporary incapacity, the informed consent of one parent of a nonviable
neonate will suffice to meet the requirements of this paragraph (c)(5), except
that the consent of the father need not be obtained if the pregnancy
resulted from rape or incest. The consent of a legally authorized
representative of either or both of the parents of a nonviable neonate will not
suffice to meet the requirements of this paragraph (c)(5).
(d) Viable neonates. A neonate, after delivery, that has been determined to be viable may be
included in research only to the extent permitted by and in accord with the requirements of
subparts A and D of this part.
34.2
The Placenta, the Dead Fetus, or Fetal Material
The following HHS regulations apply to research involving the placenta, dead fetuses, or fetal
material:
(a) Research involving, after delivery, the placenta; the dead fetus; macerated fetal
material; or cells, tissue, or organs excised from a dead fetus, shall be conducted only in
accord with any applicable Federal, State, or local laws and regulations regarding such
activities.
(b) If information associated with material described in paragraph (a) of this section is
recorded for research purposes in a manner that living individuals can be identified, directly
or through identifiers linked to those individuals, those individuals are research subjects and
all pertinent subparts of this part are applicable.
67
IRB Standard Operating Procedures
2014
34.3
Neonates of Uncertain Viability
Until it has been ascertained whether or not a neonate is viable, a neonate may not be involved in
research covered by this subpart unless the following additional conditions are met:
The IRB determines that:
34.3
The research holds out the prospect of enhancing the probability of survival of the
neonate to the point of viability, and any risk is the least possible for achieving that
objective, or (45 CFR 46.205(b)(1)(i))
The purpose of the research is the development of important biomedical knowledge
that cannot be obtained by other means and there will be no added risk to the
neonate resulting from the research; and (45 CFR 46.205(b)(1)(ii))
The legally effective informed consent of either parent of the neonate or, if neither
parent is able to consent because of unavailability, incompetence, or temporary
incapacity, the legally effective informed consent of either parent's legally authorized
representative is obtained in accord with 28.0: Informed Consent, except that the
consent of the father or his legally authorized representative need not be obtained if
the pregnancy resulted from rape or incest. (45 CFR 46.205(b)(2))
Nonviable Neonates
After delivery a nonviable neonate may not be involved in research covered by this subpart unless all
of the following additional conditions are met:
34.4
Vital functions of the neonate will not be artificially maintained; (45 CFR 46.205(c)(1))
The research will not terminate the heartbeat or respiration of the neonate; (45 CFR
46.205(c)(2))
There will be no added risk to the neonate resulting from the research; (45 CFR 46.205(c)(3))
The purpose of the research is the development of important biomedical knowledge that
cannot be obtained by other means; and (45 CFR 46.205(c)(4))
The legally effective informed consent of both parents of the neonate is obtained in
accord with 28.0: Informed Consent, except that the waiver and alteration provisions of
45 CFR 46.116(c) and (d) do not apply. However, if either parent is unable to consent
because of unavailability, incompetence, or temporary incapacity, the informed consent
of one parent of a nonviable neonate will suffice to meet the requirements of this
paragraph, except that the consent of the father need not be obtained if the pregnancy
resulted from rape or incest. The consent of a legally authorized representative of either or
both of the parents of a nonviable neonate will not suffice to meet the requirements of
this paragraph. (45 CFR 46.205(c)(5))
Viable Neonates
A neonate, after delivery, that has been determined to be viable may be included in research only to
the extent permitted by and in accord with the requirements of subparts A and D of 45 CFR 46.
35.0
Research Involving Prisoners
Federal regulations define a “prisoner” as any individual involuntarily confined or detained in a penal
institution. The term is intended to encompass individuals sentenced to such an institution under a
criminal or civil statute, individuals detained in other facilities by virtue of statutes or commitment
procedures that provide alternatives to criminal prosecution or incarceration in a penal institution, and
68
IRB Standard Operating Procedures
2014
individuals detained pending arraignment, trial, or sentencing. [45 CFR 46.303(c)]
The regulations covering research involving prisoners apply not only to research that targets prisoners or
the prison setting, but also to subjects who become incarcerated following their enrollment or subjects
for whom their incarceration is coincidental with their research involvement, (e.g., a prisoner with
cancer enrolled in a treatment oriented study that involves no other prisoners).
For research conducted or supported by HHS to involve prisoners, two actions must occur:
(1) the institution engaged in the research must certify to the DHHS Secretary (through OHRP)
that the IRB designated under its assurance of compliance has reviewed and approved the
research under 45 CFR 46.305; and
(2) the DHHS Secretary (through OHRP) must determine that the proposed research falls
within the categories of research permissible under 45 CFR 46.306(a)(2).
35.1
Issues to Address in Reviewing Prisoner Research
There are special requirements for the IRB involved with review of projects that involve prisoners. The
Board must have a member that is either a prisoner or a prisoner representative with an appropriate
background and expertise.
Any project that involves prisoners will be reviewed and presented (either primary or secondary) by the
IRB’s prisoner representative during the full board meeting. This applies to submissions related to projects
that involve prisoners, including initial, periodic review, revision, deviation/violation, and adverse event
submissions. If prisoners are proposed as part of the inclusion criteria in a new project application, a
Investigator Checklist for Studies Involving Prisoners must be submitted with the new project application.
The checklist ensures that the appropriate review is completed for this population and provides
regulatory documentation in fulfilling Subpart C requirements.
35.2
Categories of Research in Which Prisoners May Participate
The IRB must find that the research is permissible in one of the following categories:
(A) study of the possible causes, effects, and processes of incarceration, and of criminal
behavior, provided that the study presents no more than minimal risk and no more than
inconvenience to the subjects;
(B) study of prisons as institutional structures or of prisoners as incarcerated persons, provided
that the study presents no more than minimal risk and no more than inconvenience to the
subjects;
(C) research on conditions particularly affecting prisoners as a class ( for example, vaccine trials
and other research on hepatitis which is much more prevalent in prisons than elsewhere; and
research on social and psychological problems such as alcoholism, drug addition, and sexual
assaults) provided that the study may proceed only after the Secretary has consulted with
appropriate experts including experts in penology, medicine, and ethics, and published notice,
in the Federal Register, of his intent to approve such research;
(D) research on practices, both innovative and accepted, which have the intent and
reasonable probability of improving the health or well-being of the subject. In cases, in which
69
IRB Standard Operating Procedures
2014
those studies require the assignment of prisoners in a manner consistent with protocols approved
by the IRB to control groups which may not benefit from the research, the study may proceed
only after the Secretary has consulted with appropriate experts, including experts in penology,
medicine, and ethics, and published notice, in the Federal Register, of the intent to approve
such research.
Categories A and B are considered minimal risk. Minimal Risk is defined as risks normally encountered in
the daily lives of non-incarcerated healthy persons, not risks encountered in the daily lives of prisoners.
Categories C and D may require OHRP to have the research reviewed by appropriate experts and may
require a notice of intent to approve the research published in the Federal Register.
35.3
Required Findings
When an IRB is reviewing a protocol in which a prisoner is a subject, the IRB must make, in addition to
other requirements under 45 CFR 46, subpart A, seven additional findings under 45 CFR 46.305(a), as
follows:
(1) the research under review represents one of the categories of research permissible
under 45 CFR 46.306(a)(2);
(2) any possible advantages accruing to the prisoner through his or her participation in
the research, when compared to the general living conditions, medical care, quality of
food, amenities and opportunity for earnings in the prison, are not of such a magnitude
that his or her ability to weigh the risks of the research against the value of such
advantages in the limited choice environment of the prison is impaired;
(3) the risks involved in the research are commensurate with risks that would be
accepted by nonprisoner volunteers;
(4) procedures for the selection of subjects within the prison are fair to all prisoners and
immune from arbitrary intervention by prison authorities or prisoners. Unless the principal
investigator provides to the IRB justification in writing for following some other
procedures, control subjects must be selected randomly from the group of available
prisoners who meet the characteristics needed for that particular research project;
(5) the information is presented in language that is understandable to the subject
population;
(6) adequate assurance exists that parole boards will not take into account a
prisoner’s participation in the research in making decisions regarding parole, and each
prisoner is clearly informed in advance that participation in the research will have no
effect on his or her parole; and
(7) where the IRB finds there may be a need for follow-up examination or care of
participants after the end of their participation, adequate provision has been made for
such examination or care, taking into account the varying lengths of individual
prisoners’ sentences, and for informing participants of this fact.
35.4
Certification of prisoner research
Institutions that conduct HHS-supported research involving prisoners as human subjects must take
several steps to certify that the research is permissible according to federal regulations. The Office of
Research Compliance will send a brief certification letter to OHRP that simply includes the
70
IRB Standard Operating Procedures
2014
certification statement required in 45 CFR 46.305(a) and a statement indicating that the IRB chose
one of the four permissible categories of research in 45 CFR 46.306(a)(2). Inclusion of the following
information is recommended to expedite the prisoner certification process:
In addition to the prisoner certification, researchers should submit the protocol
application (which includes the protocol and any IRB submission materials, including
consent forms) and the grant application(s) (and any grant award updates).
Prisoner research certification letter, including:
o
o
o
o
o
o
o
o
o
o
36.0
OHRP Assurance Number
IRB Number for Designated IRB
Site(s) where research involving prisoners will be conducted
If prisoner research site is engaged in research, provide OHRP Assurance
Number
DHHS Grant Award Number
DHHS Funding Agency Name
Funding Agency Grants/Program Officer Name and Phone #
Title of DHHS Grant
Title of Protocol - if the same as the title of the grant, please indicate as such
Version Date of Consent Document to be used with “prisoners”
Date(s) of IRB Meeting(s) in which protocol was considered including a brief
chronology of:
1. Date of initial IRB review
2. Date of Subpart C reviews
3. Type of IRB review
4. Whether or not this is a special IRB review for prisoner issues
o
Principal Investigator(s)
Research Involving Minors
The federal regulations provide for additional protections for children as research subjects as defined in
Subpart D. In most circumstances Subpart D requires parental permission. IRBs reviewing research
involving minors as subjects must consider the benefits, risks, and discomforts inherent in the proposed
research and assess their justification in light of the expected benefits to the child-subject or to society
as a whole. In calculating the degree of risk and benefit, the IRB should weigh the circumstances of the
subjects under study, the magnitude of risks that may accrue from the research procedures, and the
potential benefits the research may provide to the subjects or class of subjects. An IRB member or a
consultant to the IRB with appropriate background and experience should be involved in the review of
any protocol involving minors.
Procedures that usually present no more than minimal risk to a healthy child include: urinalyses,
obtaining small blood samples, EEGs, allergy scratch tests, minor changes in diet or daily routine, and/or
the use of standard psychological or educational tests. The IRB must also consider the extent to which
research procedures would be a burden regardless of whether the child is accustomed to the
proposed procedures. The assessment of risk and burden should also be informed by an understanding
of the anticipated physical health, emotional maturity and other internal and external factors of the
proposed population of minors.
36.1
Research in School Settings
With respect to non-health care related research involving minors in an educational setting, studies
71
IRB Standard Operating Procedures
2014
should be carefully examined to determine both the level of risk and the potential benefit for the
subjects. The risks involved in social science research are rarely physical; however, minors may be
susceptible to emotional and psychological risks as well as risks to their social standing. In addition to
these considerations, the informed consent process for children within an educational setting is often
quite complex. As part of its review, the IRB would generally expect to see evidence that researchers
have obtained permission from the school district, the school site (e.g., principal or headmaster), and
the classroom teacher (when applicable). In addition, provisions should be made for obtaining the
permission of parents of each participating child and the assent of the child subject.
36.2
Categories of Research Involving Minors That May Be Approved by IRBs
36.3
Research not involving greater than minimal risk. [45 CFR 46.404]
Research involving greater than minimal risk, but presenting the prospect of direct
benefit to an individual subject. Research in this category is approvable provided: (a)
the risk is justified by the anticipated benefit to the subject; and (b) the relationship of
risk to benefit is at least as favorable as any available alternative approach. [45 CFR
46.405]
Research involving greater than minimal risk with no prospect of direct benefit to
individual subjects, but likely to yield generalizable knowledge about the subject's
disorder or condition. Research in this category is approvable provided: (a) the risk
represents a minor increase over minimal risk; (b) the intervention or procedure
presents experiences to subjects that are reasonably commensurate with those
inherent in their actual or expected medical, dental, psychological, social, or
educational settings; and (c) the intervention or procedure is likely to yield
generalizable knowledge about the subject's disorder or condition that is of vital
importance for the understanding or amelioration of the subject's disorder or
condition. [45 CFR 46.406]
Research that is not otherwise approvable, but which presents an opportunity to
understand, prevent, or alleviate a serious problem affecting the health or welfare of
children. Research that is not approvable under 45 CFR 46.404, 46.405, or 46.406 may
be conducted or funded by DHHS provided that the IRB, and the Secretary, after
consultation with a panel of experts, finds that the research presents a reasonable
opportunity to further the understanding, prevention, or alleviation of a significant
problem affecting the health and welfare of children. The panel of experts must also
find that the research will be conducted in accordance with sound ethical principles.
[45 CFR 46.407]
IRB Review of Research Involving Minors
The IRB protocol application should provide sufficient detail in the research plan so that the IRB can
make the determinations as outlined in Subpart D of the regulations. In addition, applications submitted
to the IRB involving minors should include the application supplement entitled “Investigator Checklist for
Research Involving Children”. The checklist is to be utilized by the IRB in determining if proposed
research studies fulfills all the requirements of the federal regulations as outlined in 45 CFR 46 Subpart D
and/or 21 CFR Parts 50 and 56 for inclusion of minors as research subjects. The IRB must concur with the
Investigator’s assessment. Otherwise, the IRB notifies the Investigator with modifications before approval
is granted. In all cases, the IRB must determine that adequate provisions have been made for soliciting
permission from parents or guardian, and soliciting the assent of each child when the IRB deems the
children are capable of assent.
72
IRB Standard Operating Procedures
2014
36.4
Students and Employees
Students
Students and employees of USA are considered vulnerable to undue influence. Such individuals may
feel pressure to participate in a research study, especially if the requesting investigator is their supervisor,
classroom instructor or someone who may be in a position to influence their career. Investigators must
exercise caution to avoid even the appearance of pressuring such individuals in enrollment. When
students participate in research studies for class credit they should be provided alternative methods of
obtaining credit that do not include participation in the study. It is the responsibility of the investigator to
determine that those alternative methods exists. Wherever possible, students should be provided with a
choice of research opportunities, including those not supervised by the investigator. Alternative choices
should be comparable in both time and effort of anticipated study participation.
Researchers need to be cautious when they seek students in a class to participate in research at the
same time. Unintended coercion must be avoided by ensuring voluntary participation, no one knows
who is and is not participating, and a time/effort equivalent alternative for those who wish not to
participate as outlined above. Course grades should not be based on research participation.
Employees
University employees, such as faculty, office staff, lab technicians, and postdoctoral fellows, are
similar to students in that they are vulnerable to perceived, even if not intended, pressures to
appear cooperative and supportive of their supervisor’s work. Accordingly, many of the same
procedures described above to reduce the likelihood of coercion in recruiting student volunteers
apply equally to university employees.
73
IRB Standard Operating Procedures
2014
Appendix A
The Belmont Report
Ethical Principles and Guidelines for the protection of human subjects of research
The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research
April 18, 1979
AGENCY: Department of Health, Education, and Welfare.
ACTION: Notice of Report for Public Comment.
SUMMARY: On July 12, 1974, the National Research Act (Pub. L. 93-348) was signed into law, there-by creating
the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. One of
the charges to the Commission was to identify the basic ethical principles that should underlie the conduct of
biomedical and behavioral research involving human subjects and to develop guidelines which should be
followed to assure that such research is conducted in accordance with those principles. In carrying out the
above, the Commission was directed to consider: (i) the boundaries between biomedical and behavioral
research and the accepted and routine practice of medicine, (ii) the role of assessment of risk-benefit criteria
in the determination of the appropriateness of research involving human subjects, (iii) appropriate guidelines
for the selection of human subjects for participation in such research and (iv) the nature and definition of
informed consent in various research settings.
The Belmont Report attempts to summarize the basic ethical principles identified by the Commission in the
course of its deliberations. It is the outgrowth of an intensive four-day period of discussions that were held in
February 1976 at the Smithsonian Institution's Belmont Conference Center supplemented by the monthly
74
IRB Standard Operating Procedures
2014
deliberations of the Commission that were held over a period of nearly four years. It is a statement of basic
ethical principles and guidelines that should assist in resolving the ethical problems that surround the conduct
of research with human subjects. By publishing the Report in the Federal Register, and providing reprints upon
request, the Secretary intends that it may be made readily available to scientists, members of Institutional
Review Boards, and Federal employees. The two-volume Appendix, containing the lengthy reports of experts
and specialists who assisted the Commission in fulfilling this part of its charge, is available as DHEW Publication
No. (OS) 78-0013 and No. (OS) 78-0014, for sale by the Superintendent of Documents, U.S. Government Printing
Office, Washington, D.C. 20402.
Unlike most other reports of the Commission, the Belmont Report does not make specific recommendations for
administrative action by the Secretary of Health, Education, and Welfare. Rather, the Commission
recommended that the Belmont Report be adopted in its entirety, as a statement of the Department's policy.
The Department requests public comment on this recommendation.
National Commission for the Protection of Human Subjects
of Biomedical and Behavioral Research
Members of the Commission
Kenneth John Ryan, M.D., Chairman, Chief of Staff, Boston Hospital for Women.
Joseph V. Brady, Ph.D., Professor of Behavioral Biology, Johns Hopkins University.
Robert E. Cooke, M.D., President, Medical College of Pennsylvania.
Dorothy I. Height, President, National Council of Negro Women, Inc.
Albert R. Jonsen, Ph.D., Associate Professor of Bioethics, University of California at San Francisco.
Patricia King, J.D., Associate Professor of Law, Georgetown University Law Center.
Karen Lebacqz, Ph.D., Associate Professor of Christian Ethics, Pacific School of Religion.
* David Louisell, J.D., Professor of Law, University of California at Berkeley.
Donald W. Seldin, M.D., Professor and Chairman, Department of Internal Medicine, University of Texas at Dallas.
Eliot Stellar, Ph.D., Provost of the University and Professor of Physiological Psychology, University of Pennsylvania.
* Robert H. Turtle, LL.B., Attorney, VomBaur, Coburn, Simmons & Turtle, Washington, D.C
* Deceased.
Table of Contents
1. Ethical Principles and Guidelines for Research Involving Human Subjects
2. Boundaries Between Practice and Research
3. Basic Ethical Principles
1. Respect for Persons
2. Beneficence
3. Justice
4. Applications
1. Informed Consent
2. Assessment of Risk and Benefits
3. Selection of Subjects
75
IRB Standard Operating Procedures
2014
Ethical Principles & Guidelines for Research Involving Human Subjects
Scientific research has produced substantial social benefits. It has also posed some troubling ethical questions.
Public attention was drawn to these questions by reported abuses of human subjects in biomedical
experiments, especially during the Second World War. During the Nuremberg War Crime Trials, the Nuremberg
code was drafted as a set of standards for judging physicians and scientists who had conducted biomedical
experiments on concentration camp prisoners. This code became the prototype of many later codes(1)
intended to assure that research involving human subjects would be carried out in an ethical manner.
The codes consist of rules, some general, others specific, that guide the investigators or the reviewers of
research in their work. Such rules often are inadequate to cover complex situations; at times they come into
conflict, and they are frequently difficult to interpret or apply. Broader ethical principles will provide a basis on
which specific rules may be formulated, criticized and interpreted.
Three principles, or general prescriptive judgments, that are relevant to research involving human subjects are
identified in this statement. Other principles may also be relevant. These three are comprehensive, however,
and are stated at a level of generalization that should assist scientists, subjects, reviewers and interested citizens
to understand the ethical issues inherent in research involving human subjects. These principles cannot always
be applied so as to resolve beyond dispute particular ethical problems. The objective is to provide an
analytical framework that will guide the resolution of ethical problems arising from research involving human
subjects.
This statement consists of a distinction between research and practice, a discussion of the three basic ethical
principles, and remarks about the application of these principles.
Part A: Boundaries Between Practice & Research
A. Boundaries Between Practice and Research
It is important to distinguish between biomedical and behavioral research, on the one hand, and the practice
of accepted therapy on the other, in order to know what activities ought to undergo review for the protection
of human subjects of research. The distinction between research and practice is blurred partly because both
often occur together (as in research designed to evaluate a therapy) and partly because notable departures
from standard practice are often called ”experimental” when the terms ”experimental” and ”research” are not
carefully defined.
For the most part, the term ”practice” refers to interventions that are designed solely to enhance the well-being
of an individual patient or client and that have a reasonable expectation of success. The purpose of medical
or behavioral practice is to provide diagnosis, preventive treatment or therapy to particular individuals. (2) By
contrast, the term ”research' designates an activity designed to test a hypothesis, permit conclusions to be
drawn, and thereby to develop or contribute to generalizable knowledge (expressed, for example, in theories,
principles, and statements of relationships). Research is usually described in a formal protocol that sets forth an
objective and a set of procedures designed to reach that objective.
When a clinician departs in a significant way from standard or accepted practice, the innovation does not, in
and of itself, constitute research. The fact that a procedure is ”experimental,” in the sense of new, untested or
different, does not automatically place it in the category of research. Radically new procedures of this
description should, however, be made the object of formal research at an early stage in order to determine
whether they are safe and effective. Thus, it is the responsibility of medical practice committees, for example,
to insist that a major innovation be incorporated into a formal research project. (3)
76
IRB Standard Operating Procedures
2014
Research and practice may be carried on together when research is designed to evaluate the safety and
efficacy of a therapy. This need not cause any confusion regarding whether or not the activity requires review;
the general rule is that if there is any element of research in an activity, that activity should undergo review for
the protection of human subjects.
Part B: Basic Ethical Principles
B. Basic Ethical Principles
The expression ”basic ethical principles” refers to those general judgments that serve as a basic justification for
the many particular ethical prescriptions and evaluations of human actions. Three basic principles, among
those generally accepted in our cultural tradition, are particularly relevant to the ethics of research involving
human subjects: the principles of respect of persons, beneficence and justice.
1. Respect for Persons. -- Respect for persons incorporates at least two ethical convictions: first, that individuals
should be treated as autonomous agents, and second, that persons with diminished autonomy are entitled to
protection. The principle of respect for persons thus divides into two separate moral requirements: the
requirement to acknowledge autonomy and the requirement to protect those with diminished autonomy.
An autonomous person is an individual capable of deliberation about personal goals and of acting under the
direction of such deliberation. To respect autonomy is to give weight to autonomous persons' considered
opinions and choices while refraining from obstructing their actions unless they are clearly detrimental to others.
To show lack of respect for an autonomous agent is to repudiate that person's considered judgments, to deny
an individual the freedom to act on those considered judgments, or to withhold information necessary to make
a considered judgment, when there are no compelling reasons to do so.
However, not every human being is capable of self-determination. The capacity for self-determination matures
during an individual's life, and some individuals lose this capacity wholly or in part because of illness, mental
disability, or circumstances that severely restrict liberty. Respect for the immature and the incapacitated may
require protecting them as they mature or while they are incapacitated.
Some persons are in need of extensive protection, even to the point of excluding them from activities which
may harm them; other persons require little protection beyond making sure they undertake activities freely and
with awareness of possible adverse consequence. The extent of protection afforded should depend upon the
risk of harm and the likelihood of benefit. The judgment that any individual lacks autonomy should be
periodically reevaluated and will vary in different situations.
In most cases of research involving human subjects, respect for persons demands that subjects enter into the
research voluntarily and with adequate information. In some situations, however, application of the principle is
not obvious. The involvement of prisoners as subjects of research provides an instructive example. On the one
hand, it would seem that the principle of respect for persons requires that prisoners not be deprived of the
opportunity to volunteer for research. On the other hand, under prison conditions they may be subtly coerced
or unduly influenced to engage in research activities for which they would not otherwise volunteer. Respect for
persons would then dictate that prisoners be protected. Whether to allow prisoners to ”volunteer” or to
”protect” them presents a dilemma. Respecting persons, in most hard cases, is often a matter of balancing
competing claims urged by the principle of respect itself.
2. Beneficence. -- Persons are treated in an ethical manner not only by respecting their decisions and
protecting them from harm, but also by making efforts to secure their well-being. Such treatment falls under the
principle of beneficence. The term ”beneficence” is often understood to cover acts of kindness or charity that
77
IRB Standard Operating Procedures
2014
go beyond strict obligation. In this document, beneficence is understood in a stronger sense, as an obligation.
Two general rules have been formulated as complementary expressions of beneficent actions in this sense: (1)
do not harm and (2) maximize possible benefits and minimize possible harms.
The Hippocratic maxim ”do no harm” has long been a fundamental principle of medical ethics. Claude
Bernard extended it to the realm of research, saying that one should not injure one person regardless of the
benefits that might come to others. However, even avoiding harm requires learning what is harmful; and, in the
process of obtaining this information, persons may be exposed to risk of harm. Further, the Hippocratic Oath
requires physicians to benefit their patients ”according to their best judgment.” Learning what will in fact
benefit may require exposing persons to risk. The problem posed by these imperatives is to decide when it is
justifiable to seek certain benefits despite the risks involved, and when the benefits should be foregone
because of the risks.
The obligations of beneficence affect both individual investigators and society at large, because they extend
both to particular research projects and to the entire enterprise of research. In the case of particular projects,
investigators and members of their institutions are obliged to give forethought to the maximization of benefits
and the reduction of risk that might occur from the research investigation. In the case of scientific research in
general, members of the larger society are obliged to recognize the longer term benefits and risks that may
result from the improvement of knowledge and from the development of novel medical, psychotherapeutic,
and social procedures.
The principle of beneficence often occupies a well-defined justifying role in many areas of research involving
human subjects. An example is found in research involving children. Effective ways of treating childhood
diseases and fostering healthy development are benefits that serve to justify research involving children -- even
when individual research subjects are not direct beneficiaries. Research also makes it possible to avoid the
harm that may result from the application of previously accepted routine practices that on closer investigation
turn out to be dangerous. But the role of the principle of beneficence is not always so unambiguous. A difficult
ethical problem remains, for example, about research that presents more than minimal risk without immediate
prospect of direct benefit to the children involved. Some have argued that such research is inadmissible, while
others have pointed out that this limit would rule out much research promising great benefit to children in the
future. Here again, as with all hard cases, the different claims covered by the principle of beneficence may
come into conflict and force difficult choices.
3. Justice. -- Who ought to receive the benefits of research and bear its burdens? This is a question of justice, in
the sense of ”fairness in distribution” or ”what is deserved.” An injustice occurs when some benefit to which a
person is entitled is denied without good reason or when some burden is imposed unduly. Another way of
conceiving the principle of justice is that equals ought to be treated equally. However, this statement requires
explication. Who is equal and who is unequal? What considerations justify departure from equal distribution?
Almost all commentators allow that distinctions based on experience, age, deprivation, competence, merit
and position do sometimes constitute criteria justifying differential treatment for certain purposes. It is necessary,
then, to explain in what respects people should be treated equally. There are several widely accepted
formulations of just ways to distribute burdens and benefits. Each formulation mentions some relevant property
on the basis of which burdens and benefits should be distributed. These formulations are (1) to each person an
equal share, (2) to each person according to individual need, (3) to each person according to individual effort,
(4) to each person according to societal contribution, and (5) to each person according to merit.
Questions of justice have long been associated with social practices such as punishment, taxation and political
representation. Until recently these questions have not generally been associated with scientific research.
However, they are foreshadowed even in the earliest reflections on the ethics of research involving human
subjects. For example, during the 19th and early 20th centuries the burdens of serving as research subjects fell
largely upon poor ward patients, while the benefits of improved medical care flowed primarily to private
patients. Subsequently, the exploitation of unwilling prisoners as research subjects in Nazi concentration camps
78
IRB Standard Operating Procedures
2014
was condemned as a particularly flagrant injustice. In this country, in the 1940's, the Tuskegee syphilis study used
disadvantaged, rural black men to study the untreated course of a disease that is by no means confined to
that population. These subjects were deprived of demonstrably effective treatment in order not to interrupt the
project, long after such treatment became generally available.
Against this historical background, it can be seen how conceptions of justice are relevant to research involving
human subjects. For example, the selection of research subjects needs to be scrutinized in order to determine
whether some classes (e.g., welfare patients, particular racial and ethnic minorities, or persons confined to
institutions) are being systematically selected simply because of their easy availability, their compromised
position, or their manipulability, rather than for reasons directly related to the problem being studied. Finally,
whenever research supported by public funds leads to the development of therapeutic devices and
procedures, justice demands both that these not provide advantages only to those who can afford them and
that such research should not unduly involve persons from groups unlikely to be among the beneficiaries of
subsequent applications of the research.
Part C: Applications
C. Applications
Applications of the general principles to the conduct of research leads to consideration of the following
requirements: informed consent, risk/benefit assessment, and the selection of subjects of research.
1. Informed Consent. -- Respect for persons requires that subjects, to the degree that they are capable, be
given the opportunity to choose what shall or shall not happen to them. This opportunity is provided when
adequate standards for informed consent are satisfied.
While the importance of informed consent is unquestioned, controversy prevails over the nature and possibility
of an informed consent. Nonetheless, there is widespread agreement that the consent process can be
analyzed as containing three elements: information, comprehension and voluntariness.
Information. Most codes of research establish specific items for disclosure intended to assure that subjects are
given sufficient information. These items generally include: the research procedure, their purposes, risks and
anticipated benefits, alternative procedures (where therapy is involved), and a statement offering the subject
the opportunity to ask questions and to withdraw at any time from the research. Additional items have been
proposed, including how subjects are selected, the person responsible for the research, etc.
However, a simple listing of items does not answer the question of what the standard should be for judging how
much and what sort of information should be provided. One standard frequently invoked in medical practice,
namely the information commonly provided by practitioners in the field or in the locale, is inadequate since
research takes place precisely when a common understanding does not exist. Another standard, currently
popular in malpractice law, requires the practitioner to reveal the information that reasonable persons would
wish to know in order to make a decision regarding their care. This, too, seems insufficient since the research
subject, being in essence a volunteer, may wish to know considerably more about risks gratuitously undertaken
than do patients who deliver themselves into the hand of a clinician for needed care. It may be that a
standard of ”the reasonable volunteer” should be proposed: the extent and nature of information should be
such that persons, knowing that the procedure is neither necessary for their care nor perhaps fully understood,
can decide whether they wish to participate in the furthering of knowledge. Even when some direct benefit to
them is anticipated, the subjects should understand clearly the range of risk and the voluntary nature of
participation.
79
IRB Standard Operating Procedures
2014
A special problem of consent arises where informing subjects of some pertinent aspect of the research is likely
to impair the validity of the research. In many cases, it is sufficient to indicate to subjects that they are being
invited to participate in research of which some features will not be revealed until the research is concluded. In
all cases of research involving incomplete disclosure, such research is justified only if it is clear that (1)
incomplete disclosure is truly necessary to accomplish the goals of the research, (2) there are no undisclosed
risks to subjects that are more than minimal, and (3) there is an adequate plan for debriefing subjects, when
appropriate, and for dissemination of research results to them. Information about risks should never be withheld
for the purpose of eliciting the cooperation of subjects, and truthful answers should always be given to direct
questions about the research. Care should be taken to distinguish cases in which disclosure would destroy or
invalidate the research from cases in which disclosure would simply inconvenience the investigator.
Comprehension. The manner and context in which information is conveyed is as important as the information
itself. For example, presenting information in a disorganized and rapid fashion, allowing too little time for
consideration or curtailing opportunities for questioning, all may adversely affect a subject's ability to make an
informed choice.
Because the subject's ability to understand is a function of intelligence, rationality, maturity and language, it is
necessary to adapt the presentation of the information to the subject's capacities. Investigators are responsible
for ascertaining that the subject has comprehended the information. While there is always an obligation to
ascertain that the information about risk to subjects is complete and adequately comprehended, when the
risks are more serious, that obligation increases. On occasion, it may be suitable to give some oral or written
tests of comprehension.
Special provision may need to be made when comprehension is severely limited -- for example, by conditions
of immaturity or mental disability. Each class of subjects that one might consider as incompetent (e.g., infants
and young children, mentally disable patients, the terminally ill and the comatose) should be considered on its
own terms. Even for these persons, however, respect requires giving them the opportunity to choose to the
extent they are able, whether or not to participate in research. The objections of these subjects to involvement
should be honored, unless the research entails providing them a therapy unavailable elsewhere. Respect for
persons also requires seeking the permission of other parties in order to protect the subjects from harm. Such
persons are thus respected both by acknowledging their own wishes and by the use of third parties to protect
them from harm.
The third parties chosen should be those who are most likely to understand the incompetent subject's situation
and to act in that person's best interest. The person authorized to act on behalf of the subject should be given
an opportunity to observe the research as it proceeds in order to be able to withdraw the subject from the
research, if such action appears in the subject's best interest.
Voluntariness. An agreement to participate in research constitutes a valid consent only if voluntarily given. This
element of informed consent requires conditions free of coercion and undue influence. Coercion occurs when
an overt threat of harm is intentionally presented by one person to another in order to obtain compliance.
Undue influence, by contrast, occurs through an offer of an excessive, unwarranted, inappropriate or improper
reward or other overture in order to obtain compliance. Also, inducements that would ordinarily be
acceptable may become undue influences if the subject is especially vulnerable.
Unjustifiable pressures usually occur when persons in positions of authority or commanding influence -especially where possible sanctions are involved -- urge a course of action for a subject. A continuum of such
influencing factors exists, however, and it is impossible to state precisely where justifiable persuasion ends and
undue influence begins. But undue influence would include actions such as manipulating a person's choice
through the controlling influence of a close relative and threatening to withdraw health services to which an
individual would otherwise be entitled.
80
IRB Standard Operating Procedures
2014
2. Assessment of Risks and Benefits. -- The assessment of risks and benefits requires a careful arrayal of relevant
data, including, in some cases, alternative ways of obtaining the benefits sought in the research. Thus, the
assessment presents both an opportunity and a responsibility to gather systematic and comprehensive
information about proposed research. For the investigator, it is a means to examine whether the proposed
research is properly designed. For a review committee, it is a method for determining whether the risks that will
be presented to subjects are justified. For prospective subjects, the assessment will assist the determination
whether or not to participate.
The Nature and Scope of Risks and Benefits. The requirement that research be justified on the basis of a
favorable risk/benefit assessment bears a close relation to the principle of beneficence, just as the moral
requirement that informed consent be obtained is derived primarily from the principle of respect for persons.
The term ”risk” refers to a possibility that harm may occur. However, when expressions such as ”small risk” or
”high risk” are used, they usually refer (often ambiguously) both to the chance (probability) of experiencing a
harm and the severity (magnitude) of the envisioned harm.
The term ”benefit” is used in the research context to refer to something of positive value related to health or
welfare. Unlike, ”risk,” ”benefit” is not a term that expresses probabilities. Risk is properly contrasted to
probability of benefits, and benefits are properly contrasted with harms rather than risks of harm. Accordingly,
so-called risk/benefit assessments are concerned with the probabilities and magnitudes of possible harm and
anticipated benefits. Many kinds of possible harms and benefits need to be taken into account. There are, for
example, risks of psychological harm, physical harm, legal harm, social harm and economic harm and the
corresponding benefits. While the most likely types of harms to research subjects are those of psychological or
physical pain or injury, other possible kinds should not be overlooked.
Risks and benefits of research may affect the individual subjects, the families of the individual subjects, and
society at large (or special groups of subjects in society). Previous codes and Federal regulations have required
that risks to subjects be outweighed by the sum of both the anticipated benefit to the subject, if any, and the
anticipated benefit to society in the form of knowledge to be gained from the research. In balancing these
different elements, the risks and benefits affecting the immediate research subject will normally carry special
weight. On the other hand, interests other than those of the subject may on some occasions be sufficient by
themselves to justify the risks involved in the research, so long as the subjects' rights have been protected.
Beneficence thus requires that we protect against risk of harm to subjects and also that we be concerned
about the loss of the substantial benefits that might be gained from research.
The Systematic Assessment of Risks and Benefits. It is commonly said that benefits and risks must be ”balanced”
and shown to be ”in a favorable ratio.” The metaphorical character of these terms draws attention to the
difficulty of making precise judgments. Only on rare occasions will quantitative techniques be available for the
scrutiny of research protocols. However, the idea of systematic, nonarbitrary analysis of risks and benefits should
be emulated insofar as possible. This ideal requires those making decisions about the justifiability of research to
be thorough in the accumulation and assessment of information about all aspects of the research, and to
consider alternatives systematically. This procedure renders the assessment of research more rigorous and
precise, while making communication between review board members and investigators less subject to
misinterpretation, misinformation and conflicting judgments. Thus, there should first be a determination of the
validity of the presuppositions of the research; then the nature, probability and magnitude of risk should be
distinguished with as much clarity as possible. The method of ascertaining risks should be explicit, especially
where there is no alternative to the use of such vague categories as small or slight risk. It should also be
determined whether an investigator's estimates of the probability of harm or benefits are reasonable, as judged
by known facts or other available studies.
Finally, assessment of the justifiability of research should reflect at least the following considerations: (i) Brutal or
inhumane treatment of human subjects is never morally justified. (ii) Risks should be reduced to those necessary
to achieve the research objective. It should be determined whether it is in fact necessary to use human
81
IRB Standard Operating Procedures
2014
subjects at all. Risk can perhaps never be entirely eliminated, but it can often be reduced by careful attention
to alternative procedures. (iii) When research involves significant risk of serious impairment, review committees
should be extraordinarily insistent on the justification of the risk (looking usually to the likelihood of benefit to the
subject -- or, in some rare cases, to the manifest voluntariness of the participation). (iv) When vulnerable
populations are involved in research, the appropriateness of involving them should itself be demonstrated. A
number of variables go into such judgments, including the nature and degree of risk, the condition of the
particular population involved, and the nature and level of the anticipated benefits. (v) Relevant risks and
benefits must be thoroughly arrayed in documents and procedures used in the informed consent process.
3. Selection of Subjects. -- Just as the principle of respect for persons finds expression in the requirements for
consent, and the principle of beneficence in risk/benefit assessment, the principle of justice gives rise to moral
requirements that there be fair procedures and outcomes in the selection of research subjects.
Justice is relevant to the selection of subjects of research at two levels: the social and the individual. Individual
justice in the selection of subjects would require that researchers exhibit fairness: thus, they should not offer
potentially beneficial research only to some patients who are in their favor or select only ”undesirable” persons
for risky research. Social justice requires that distinction be drawn between classes of subjects that ought, and
ought not, to participate in any particular kind of research, based on the ability of members of that class to
bear burdens and on the appropriateness of placing further burdens on already burdened persons. Thus, it can
be considered a matter of social justice that there is an order of preference in the selection of classes of
subjects (e.g., adults before children) and that some classes of potential subjects (e.g., the institutionalized
mentally infirm or prisoners) may be involved as research subjects, if at all, only on certain conditions.
Injustice may appear in the selection of subjects, even if individual subjects are selected fairly by investigators
and treated fairly in the course of research. Thus injustice arises from social, racial, sexual and cultural biases
institutionalized in society. Thus, even if individual researchers are treating their research subjects fairly, and
even if IRBs are taking care to assure that subjects are selected fairly within a particular institution, unjust social
patterns may nevertheless appear in the overall distribution of the burdens and benefits of research. Although
individual institutions or investigators may not be able to resolve a problem that is pervasive in their social
setting, they can consider distributive justice in selecting research subjects.
Some populations, especially institutionalized ones, are already burdened in many ways by their infirmities and
environments. When research is proposed that involves risks and does not include a therapeutic component,
other less burdened classes of persons should be called upon first to accept these risks of research, except
where the research is directly related to the specific conditions of the class involved. Also, even though public
funds for research may often flow in the same directions as public funds for health care, it seems unfair that
populations dependent on public health care constitute a pool of preferred research subjects if more
advantaged populations are likely to be the recipients of the benefits.
One special instance of injustice results from the involvement of vulnerable subjects. Certain groups, such as
racial minorities, the economically disadvantaged, the very sick, and the institutionalized may continually be
sought as research subjects, owing to their ready availability in settings where research is conducted. Given
their dependent status and their frequently compromised capacity for free consent, they should be protected
against the danger of being involved in research solely for administrative convenience, or because they are
easy to manipulate as a result of their illness or socioeconomic condition.
(1) Since 1945, various codes for the proper and responsible conduct of human experimentation in medical
research have been adopted by different organizations. The best known of these codes are the Nuremberg
Code of 1947, the Helsinki Declaration of 1964 (revised in 1975), and the 1971 Guidelines (codified into Federal
Regulations in 1974) issued by the U.S. Department of Health, Education, and Welfare Codes for the conduct of
82
IRB Standard Operating Procedures
2014
social and behavioral research have also been adopted, the best known being that of the American
Psychological Association, published in 1973.
(2) Although practice usually involves interventions designed solely to enhance the well-being of a particular
individual, interventions are sometimes applied to one individual for the enhancement of the well-being of
another (e.g., blood donation, skin grafts, organ transplants) or an intervention may have the dual purpose of
enhancing the well-being of a particular individual, and, at the same time, providing some benefit to others
(e.g., vaccination, which protects both the person who is vaccinated and society generally). The fact that
some forms of practice have elements other than immediate benefit to the individual receiving an intervention,
however, should not confuse the general distinction between research and practice. Even when a procedure
applied in practice may benefit some other person, it remains an intervention designed to enhance the wellbeing of a particular individual or groups of individuals; thus, it is practice and need not be reviewed as
research.
(3) Because the problems related to social experimentation may differ substantially from those of biomedical
and behavioral research, the Commission specifically declines to make any policy determination regarding
such research at this time. Rather, the Commission believes that the problem ought to be addressed by one of
its successor bodies.
83
IRB Standard Operating Procedures
2014
APPENDIX B
Unaffiliated Investigator Agreement
Name of Institution with the Federalwide Assurance (FWA):
Applicable FWA #:
Unaffiliated Investigator’s Name:
Specify Research Covered by This Agreement:
(1) The above-named Unaffiliated Investigator has reviewed: 1) The Belmont Report: Ethical Principles and
Guidelines for the Protection of Human Subjects of Research (or other internationally recognized
equivalent; see B1 of FWA Terms for institutions outside the United States); 2) the U.S. Department of Health
and Human Services (DHHS) regulations for the protection of human subjects at 45 CFR 46 (or other
internationally recognized equivalent, see B3 of FWA Terms for institutions outside the United States); 3) the
Federalwide Assurance (FWA) referenced above; and 4) the relevant institutional policies and procedures
for the protection of human subjects.
(2) The Unaffiliated Investigator understands and hereby accepts the responsibility to comply with the
standards and requirements stipulated in the above documents and to protect the rights and welfare of
human subjects involved in research conducted under this Agreement.
(3) The Unaffiliated Investigator will comply with all other National, State, or local laws or regulations that may
provide additional protection for human subjects.
(4) The Unaffiliated Investigator will abide by all determinations of the IRB designated under the above
Assurance and will accept the final authority and decisions of the IRB, including but not limited to directives
to terminate participation in designated research activities.
(5) The Unaffiliated Investigator will complete any educational training required by the Institution and/or the
IRB prior to initiating research covered under this Agreement.
(6) The Unaffiliated Investigator will report promptly to the IRB any proposed changes in the research
conducted under this Agreement. The investigator will not initiate changes in the research without prior IRB
review and approval, except where necessary to eliminate apparent immediate hazards to subjects.
(7) The Unaffiliated Investigator will report immediately to the IRB any unanticipated problems involving risks to
subjects or others in research covered under this Agreement.
(8) The Unaffiliated Investigator will obtain, document, and maintain records of informed consent from each
subject or the subject’s legally authorized representative as required under DHHS and FDA regulations (or
other international or national equivalent) and stipulated by the IRB.
(9) The Unaffiliated Investigator acknowledges and agrees to cooperate in the IRB responsibility for initial and
continuing review, record keeping, reporting, and certification. The Unaffiliated Investigator will provide all
information requested by the IRB in a timely fashion.
84
IRB Standard Operating Procedures
2014
(10)
In conducting research involving FDA-regulated products, the Unaffiliated Investigator will comply with all
applicable FDA regulations and fulfill all investigator responsibilities (or investigator-sponsor responsibilities,
where appropriate), including those described at 21 CFR 312 and 812.
(11)
The Unaffiliated Investigator will not enroll subjects in research under this Agreement prior to its review and
approval by the IRB.
(12)
Emergency medical care may be delivered without IRB review and approval to the extent permitted under
applicable Federal regulations and State law. However, data and information obtained as a result of
emergency medical care may not be included as part of federally-supported or –conducted research.
(13)
This Agreement does not preclude the Unaffiliated Investigator from taking part in research not covered by
the Agreement.
(14)
The Unaffiliated Investigator acknowledges that he/she is primarily responsible for safeguarding the rights
and welfare of each research subject, and that the subject’s rights and welfare must take precedence
over the goals and requirements of the research.
Investigator Signature:
Date:
Name:
Degree(s):
(Last)
Address:
(First)
(City)
Phone #:
(Middle Initial)
(State/Province)
FAX #:
(Zip/Country)
Email:
FWA Institutional Official (or Designee):
Date:
Name:
Degree(s):
(Last)
Address:
(First)
(City)
Phone #:
(Middle Initial)
(State/Province)
FAX #:
Email:
85
IRB Standard Operating Procedures
2014
(Zip/Country)
APPENDIX C
CONFIDENTIALITY AGREEMENT
University of South Alabama
Institutional Review Board
I, _________________________________, will be participating in the review of proposed human subject
research (i.e., convened meeting or expedited review) on behalf of or with the University of South Alabama’s
Institutional Review Board. Regardless of my role, I understand and agree that the information and
documentation to which I will be exposed during and related to my participation with the Institutional Review
Board is confidential.
I further acknowledge and agree that I will not, without appropriate authorization, access information
that the IRB considers privileged or confidential, release such privileged or confidential information to anyone
outside of the review process within or without the University, or use such information for unauthorized purposes.
I understand that I am authorized to discuss for educational and/or professional purposes only the
general aspects of the review process but may not include specific information regarding any of the research
proposals made to or discussed by the Institutional Review Board. I also agree that I will not copy or otherwise
take any documentation or written information from the Institutional Review Board without express permission
from the IRB Office.
Regardless of my association with the Institutional Review Board, I further understand and agree that this
confidentiality agreement continues after the end of my affiliation with the University.
Signature: _____________________________________
Date:
Affiliation:
__________________
IRB Member
Guest: (faculty investigator)
86
IRB Standard Operating Procedures
2014
Guest: (student)
APPENDIX D
REQUIRMENTS FOR HUMANITARIAN USE DEVICE
1. Definition of Humanitarian Use Device - The definition of a HUD is a device that is intended to benefit
patients in the treatment and diagnosis of diseases or conditions that affect or are manifested in fewer
than 4,000 individuals in the United States per year.
2. Physician Responsibilities for the Use of a HUD
A physician may utilize a HUD when agreeing to the following:
The HUD will be utilized for treatment, diagnosis, or research in accordance with the labeling of the
device, intended purpose, and in the designated population for which the FDA approved its use;
The patient must be informed that the HUD is a device authorized under Federal law for use;
however, the effectiveness of the device for a specific indication has not been demonstrated; and
The informed consent of the patient or the patient’s legally authorized representative will be
obtained when the use of the HUD involves research or when required by the IRB. The UCI IRB
generally requires that treating physicians obtain informed consent.
3. The IRB’s Role in HUD Review and Approval
Pursuant to 21 CFR 814.124(a), the FDA requires IRB review and approval before a HUD is used, as well as
continuing review of the use of the HUD. The IRB must ensure that the proposed use is within the FDAapproved indication and that the use of the device does not exceed the scope of the FDA’s approval.
The use of a HUD does not constitute research unless the physician or health care provider intends to
collect data from its use.
4. Initial IRB Approval. The HUD and its proposed use must be submitted to the IRB for review and approval
by a convened IRB committee. Thirty-five copies of the following materials should be provided for
review:
The HUD manufacturer’s product labeling, clinical brochure and/or other pertinent
manufacturer information materials
The FDA HDE approval letter
Written statement from the principal investigator specifying how (ie, for what clinical
indication(s), where and by whom the HUD will be used within the clinical setting. The clinical
indication should be limited to what is specified in the FDA-approved product labeling.
5. Clinical Consent Form
All invasive clinical procedures require written informed consent. Therefore, there should be a consent
form addressing the proposed clinical use of the HUD. Because the HUD is approved for clinical use,
terms such as “research” should be avoided in the consent document. Although the FDA regulations
do not require a consent form, it is up to the institution to determine whether one should be used.
Historically, the University’s IRB has requested that consent be obtained and that the proposed consent
form be reviewed by the IRB. Please submit a copy with your IRB application or provide justification for
waiver of consent. The consent form should be modeled after other clinical consent forms for invasive
procedures. A HUD informed consent template has been developed for your use.
87
IRB Standard Operating Procedures
2014
6.
Continuing Review
Federal regulations require that an annual review be submitted to the IRB. The annual review
can be reviewed in an expedited manner. A renewal report should be submitted to the IRB to
include the total number of patients who have received the device in the previous year, a copy
of the current FDA approved product labeling for the HUD, a copy of the current IRB approved
consent document.
7. Reporting Adverse Events to the IRB
Investigators are required to submit adverse events as they would on a research study using the
IRB Adverse Event Report form.
8. Off-Label Use of a HUD in Emergency or Compassionate Situation
In special instances an HUD can be used on an emergent basis. If an HUD is used under
emergency circumstance, it can not be used again until a complete IRB application has been
submitted and approved. Emergency use is defined as necessary to save the life or protect the
well-being of a given patient. Under these circumsantances, the physician should, on a case by
case basis:
a. Before the device is used, if at all possible, notify the IRB Chair or Vice Chair of the
planned “off-label” use of the HUD. The IRB Chair or Vice-Chair will provide an
independent assessment as to whether the proposed use constitutes an emergency or
compassionate situation.
b. Obtain clinical informed consent for the “off-label” use of the HUD.
c. FDA approval for “off-label” use of the HUD should be obtained by the device
manufacturer (HDE holder) prior to the device for the emergency/compassionate use
procedure. Please remember that use of an HUD in an off-label manner is a violation of
federal laws. The IRB has been mandated to monitor HUD uses so that off-label uses are
reported to the FDA.
d. After the emergency use occurs, the physician should submit a follow-up report on the
patient’s condition and information regarding the patient protection measures to the
HDE holder, who then submit this report as an amendment to the HDE.
9. Compassionate Use of a HUD in a Non-Emergency Sitatution
The IRB may approve compassionate use of a HUD if the physician determines that there is no
emergency, but there is no alternative device for the patient’s condition. The physician who
wishes to use the HUD should provide the HDE holder with the following:
a.
b.
c.
a description of the patient’s condition and the circumstances necessitating
treatment with the device
a discussion of why alternative therapies are unsatisfactory, and
information to address patient protection measures.
88
IRB Standard Operating Procedures
2014
APPLICABLE REGULATIONS AND GUIDELINES
FDA, Humanitarian Device Exemption (HDE) Regulation: Questions and Answers; Final Guidance for
Industry, July 12, 2001
21 CFR 814, Premarket Approval of Medical Devices
21 CFR 814, Subpart H, Humanitarian Use Devices
Humanitarian Use Devices, A brief guide for clinicians, investigators, and IRB members, Dale E.
Hammerschmidt, M.D., University of Minnesota, October, 2001
(http://www.research.umn.edu/irb/members/education/HUDs.pdf)
89
IRB Standard Operating Procedures
2014