Clinical Assessment (CA) MS WORD
advertisement

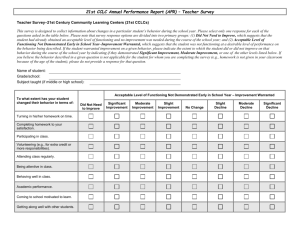
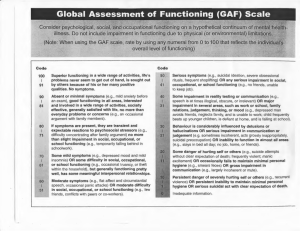
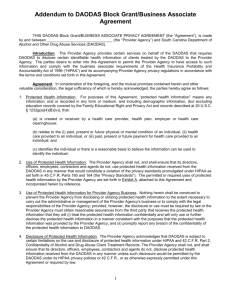
Clinical Assessment (Diagnostic Assessment) Client Name (Last, First, MI) ID # Medicaid # Age: Sex: Identifying Information: DOB: Ethnic Group: Marital Status: Occupation: Education: Multiaxial Diagnosis: Axis I: Clinical Disorders / Other Conditions That May Be a Focus of Clinical Attention Diagnostic Code DSM-IV Name Axis II: Personality Disorders / Mental Retardation Diagnostic Code DSM-IV Name Axis III: General Medical Conditions ICD-9-CM Code ICD-9-CM Name Axis IV: Psychosocial and Environmental Problems Problems with primary support group (Specify): Problems related to the social environment (Specify): Educational problems (Specify): Occupational problems (Specify): Housing problems (Specify): Economic problems (Specify): Problems with access to healthcare services (Specify): Problems related to interaction with the legal system/crime (Specify): Other psychosocial and environmental problems (Specify): Axis V: Global Assessment of Functioning Scale Score: Admitted to Services: Time Frame: Yes No, Reason for Non-admission: Statement of Medical Necessity: I recommend that the above-named Medicaid beneficiary receive Rehabilitation Services for the maximum reduction of emotional, behavioral, and functional developmental delays, and for restoration of the beneficiary to his or her best possible functioning level. This beneficiary meets the medical-necessity criteria for Rehabilitative Services evidenced by a Psychiatric/Substance Abuse Disorder diagnosis from the current edition of the DSM or the ICD. Licensed Professional of Health Arts Signature and Credentials: CA 6/11 DAODAS FORM Date: Page 1 of 3 Clinical Assessment (Diagnostic Assessment) Client Name (Last, First, MI) ID # Medicaid # Master Problem List: In concise statements, list the most immediate problems the client is presenting. Indicate whether each problem will be addressed on the Treatment Plan (T); whether it will be referred (R) for services elsewhere; or whether it will be monitored (M). Place the letter that corresponds to the appropriate disposition in the space provided to the left of each problem statement. 1. 2. 3. 4. 5. 6. Interpretive Summary: Include an integration of potential interrelationships between findings; interpretation of all pertinent assessment information; identification of any disabilities/co-existing disorders; central themes; the client’s perception of his/her needs, strengths, limitations, or problems; both positive and negative factors likely to affect client’s course of treatment and clinical outcomes following discharge (e.g., recovery); recommended treatments; anticipated level and length of care; and intensity of treatment and expected focus (goals) with recommendations. Clinician Signature and Title : Date: Clinical Assessment Outline: Presenting Problem: Include reason for entry, source of referral, legal involvement, self-identified problems, and recent stressor. Health/Medical/Development History: Describe general health, nutrition, medical problems (include visual and motor function), prenatal exposure to alcohol or other drugs and possible effects, remarkable developmental milestone delays, medications for the past year, allergies, hospitalizations, disabilities, tuberculosis screening, and HIV-risk behaviors. Identify need for assistive technology or resources. Provide physician’s name and telephone number. Complete “Special Populations” section as appropriate. Family/Social Interaction: In chronological order, describe family of origin and present family, including relationships with all family members. Describe any history as a survivor, perpetrator, victim and/or witness of any psychological, emotional, physical, and/or sexual abuse. Include family history of substance use/abuse, current family use, and family psychiatric history. Describe other intimate and social relationships. Identify needed and available social supports. Include peer group functioning. Include pertinent current and historical life situation information on sexual orientation, gender expression, and cultural, ethnic and spiritual background. Psychoactive Substance Use History: Drug Age at First Use Frequency (past 12 months) Quantity (specify time frame) Last Use How Used Alcohol Amphetamines Caffeine Cannabis Cocaine Hallucinogen Inhalant CA 3/12 DAODAS FORM Page 2 of 3 Clinical Assessment (Diagnostic Assessment) Client Name (Last, First, MI) ID # Medicaid # Nicotine Opioid PCP Sedative Hypnotic Other Psychoactive Substance Use: Include other relevant substance use factors such as loss of control, tolerance, treatment history, patterns of use, and problems related to use. Include data to differentiate between use, abuse, and dependence. Psychological: Include mental status, cognitive functioning, activities of daily living, communication skills/abilities, present emotional state, behavioral functioning and issues, management of emotions, risk-taking behaviors, violence / risk to others, personal safety concerns, suicide attempts/thoughts, hallucinations, and other psychiatric history (to include history of eating disorder behaviors). Complete “Special Populations” section as appropriate. Special Populations: Client is a member of the following special population group: Child/Adolescent Senior None of the Above (Go to next section) Dual Diagnosis Other Coexisting Disabilities/Disorders Assessments for children/adolescents should include motor development and functioning; speech, hearing, and language functioning; immunization status; evaluation of developmental age factors; learning ability; and intellectual functioning. Assessments for seniors should include motor, speech, hearing, language, and cognitive functioning. Assessments for persons with coexisting psychiatric disabilities and other coexisting disabilities/disorders should include (if appropriate or applicable) history of previous mental health services, previous medical services, pharmacotherapy, hospitalizations, use of community programs, differential diagnosis, mental status, all prescription and non-prescription medications at time of admission and at least the previous six months, past and current medication efficacy, medication allergies and/or adverse medication reactions, and psychological/social adjustment to disability/disorder. Gambling: Include the age at which gambling began and describe preoccupation with gambling, loss of control, tolerance, treatment history, gambling patterns (including patterns impacted by substance use/abuse), and problems related to gambling. Educational/Vocational: Include years of education/apparent educational deficiencies, education history, literacy level, military service (self, other family members, or significant others), and job history. Abilities, Strengths, Needs and Preferences: Describe client and clinician perceptions of abilities, strengths, needs, and preferences. Include unique factors affecting the course of treatment and client expectations of treatment outcomes. Include financial status, leisure skills/activities/interests, and recovery environment. Other: Sources of Information Other than Client: Name: Relationship: Name: Relationship: Clinician Signature and Title: Date: CA 3/12 DAODAS FORM Page 3 of 3