COAGULATION CHANGES ONE YEAR AFTER RESECTION OF
advertisement

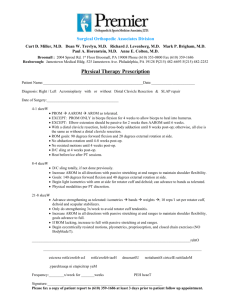
COAGULATION CHANGES ONE YEAR AFTER RESECTION OF INTRAABDOMINAL MALIGNANCY Robert M. Van Haren MD, Evan J. Valle MD, Chad M. Thorson MD MSPH, Gerardo A. Guarch MD, Jassin M. Jouria MD, Alexander M. Busko BS, Danny Sleeman MD, Joe U. Levi MD, Alan S. Livingstone MD, Kenneth G. Proctor PhD Daughtry Dept of Surgery, University of Miami Miller School of Medicine Background: A significant fraction of the morbidity and mortality in cancer patients can be attributed to malignant hypercoagulability. Surgical resection of malignancy should theoretically reverse hypercoagulability. However, we previously demonstrated that patients develop worsening hypercoagulability after resection, and that this condition persists at least one month post-operatively. Objectives: To test hypothesis that cancer induced hypercoagulability is eventually reversed during long-term follow-up from successful resection. Methods: A prospective trial was conducted with informed consent at an academic medical center. Blood samples were obtained from cancer patients undergoing surgical resection for curative intent pre-operatively (pre-op) and post-operatively (post-op) for up to one year. Rotational thromboelastography (ROTEM) provides a global measurement of coagulation and was performed on whole blood samples. Data are presented as mean±SD. Repeated measures ANOVA were used; significance was assessed at p<0.05. Results: 47 patients, age 66±11 yrs and 60% male were enrolled. Cancers primarily involved the esophagus (n=15, 32%), pancreas (n=15, 32%), stomach (n=6, 13%), and liver (n=4, 9%). 13 patients (28%) were hypercoagulable on pre-op ROTEM. Post-op, patients were more hypercoagulable with shorter clot formation time (low CFT) and higher maximum clot firmness (MCF) (all p<0.05). Long term data on average revealed a return to baseline coagulation status (see table), however 21 patients (45%) had a reversal of cancer induced hypercoagulability. . Two patients developed venous thromboembolism (VTE) and were hypercoagulable (alpha: 76.1±3.0 vs. 81.0±4.2, p=0.029). Conclusion: Almost a third of patients with intra-abdominal malignancy are hypercoagulable pre-op. Surgical resection initially increases hypercoagulable state, and then returns to baseline during long term follow-up. Surgical resection reverses cancer induced hypercoagulability in some, but not all patients. This findings support the use of VTE prophylaxis for 1 month postoperatively. Coagulation Changes After Surgical Resection of Intra-abdominal Malignancies, n=47 Pre-Op Post-Op Day 1 6-12 months p= Intrinsic Pathway CT, sec 163.5±27.3 167.1±24.3 177.5±47.0 0.118 CFT, sec 74.9±25.0 68.2±19.5 80.4±40.1 0.103 MCF, mm 61.5±5.7* 64.4±6.7* 62.5±8.9 0.046 Alpha, degrees 76.3±3.1 76.7±3.3 75.0±5.6 0.099 Extrinsic Pathway CT, sec 54.7±15.9 59.3±14.3* 50.6±16.2* 0.004 CFT, sec 82.7±25.3* 74.5±21.6* 79.8±34.9 0.282 MCF, mm 64.7±6.3* 67.7±5.7* 65.0±9.1 0.068 Alpha, degrees 76.0±3.9 76.2±4.3 76.3±5.6 0.461 Final Common Pathway (Fibrin) MCF, mm 20.2±8.1* 25.6±7.8* 22.6±11.0 0.014