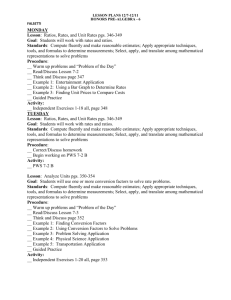
Table of Contents - Prader
advertisement

Scientific Abstract Submissions Presented at the 25th Annual PWSA (USA) Scientific Meeting in Orlando, FL November 11, 2011 Table of Contents Phenotype-Genotype Correlation of Two Patients with de Novo Imbalanced Chromosomal Rearrangements ........... 1 Misdiagnosed as Prader-Willi Syndrome ........................................................................................................ 1 Growth Hormone Effects in Adults with Prader-Willi Syndrome ......................................................................... 2 Serum IGF-1 Levels Do Not Correlate with Growth Hormone Dose in Children with Prader-Willi Syndrome ............ 3 Mechanism of MBII-52 and MBII-85 snoRNA Processing .................................................................................. 4 Molecular Function of psnoRNAs Derived from HBII-52 and HBII-85 Expression Units ......................................... 5 Hyperghrelinemia Begins Early in Prader-Willi Syndrome ................................................................................. 6 Two More Children Born to Women with Prader-Willi Syndrome, One Normal, One with Angelman ....................... 7 Direct Cloning of Double-Stranded RNAs from RNase Protection Analysis Reveals Processing Patterns of C/D Box snoRNAs in PWS Critical Region and Provides Evidence for Widespread Antisense Transcript Expression ................ 8 Loss of the Prader-Willi Syndrome Candidate Gene Magel2 Impairs Leptin Signaling in Mice ................................ 9 Social Functioning in Prader-Willi Syndrome ................................................................................................ 11 Psychiatric Symptoms in Prader-Willi Syndrome ........................................................................................... 12 The Effect of Residential Placement on Weight Control of Individuals with Prader-Willi Syndrome: an Outcome Evaluation ............................................................................................................................................... 13 Parental Role in Physical Activity among Children with Prader-Willi Syndrome .................................................. 14 The Relationship between Early-Onset Obesity and Behavior ......................................................................... 15 Preliminary Results of Strengths and Weaknesses in Neuropsychological Testing in Children with Prader-Willi Syndrome ............................................................................................................................................... 16 Hormonal and Metabolic Responses to Endurance Exercise in Prader-Willi Syndrome ........................................ 18 Postprandial Cardiac Autonomic Function is Impaired in Prader-Willi Syndrome ................................................ 19 Phenomenology of Malignant Hypothermia in PWS ....................................................................................... 20 Cases of Survival and Death from Gastric Dysmotility in PWS ........................................................................ 22 Autonomic Nervous System (ANS) Dysfunction in PWS and Childhood Obesity: Preliminary Findings .................. 24 Progress Report from the Prader-Willi Syndrome Research Strategy Workshop ................................................ 25 Effects of Early Growth Hormone Therapy in Individuals with Prader-Willi Syndrome ........................................ 26 Biochemical and Molecular Characterization of the Serotonin Receptor 2C (HTR2c) Alternative Splicing ............... 28 Outcomes of Adenotonsillectomy in Prader-Willi Syndrome Patients ................................................................ 29 The Australian National Prader-Willi Syndrome Database 2011....................................................................... 30 - 2 - The Genetics Review - 3 - Phenotype-Genotype Correlation of Two Patients with de Novo Imbalanced Chromosomal Rearrangements Misdiagnosed as Prader-Willi Syndrome M.A. Angulo., G. Blaber, M.M. Zak Department of Human Genetics, Winthrop University Hospital, Mineola, NY, USA Introduction: We report on the 17 year old female and a 27 year old male with distinctive facies, intellectual disabilities, hypotonia , short stature, initially diagnosed at another institution with Prader-Willi syndrome (PWS) at the age of four and seven years respectively, based on chromosomal analysis and clinical picture. They had poor growth velocity associated with excessive weight gain, temper tantrums related to food and mild mental retardation. Methods: Blood chromosome analysis (G-banding), fluorescent in situ hybridization (FISH), DNA with methylation and array-comparative genomic hybridization (aCGH) were performed by commercial laboratories. Results/Discussion: PWS is a complex genetic condition that arises from a lack of paternally-inherited genes in chromosome 15q11-q13. We provide correlation between the clinical findings of our patients and the phenotype of the PWS. Also we emphasize the utilization of genetic testing accompanied by genetic counseling. Both patients were seen to consider growth hormone treatments as adults and both were found to have features not consistent with PWS. Both had normal secondary characteristics and female had normal menses. They were able to stop eating when satisfied. Chromosome analysis revealed a de novo imbalanced translocation 46,XX,der (4) t(4;14)(q35.2;q32.2). The use of CGH revealed a presence of a duplication of at least 11Mb at 14q32.2q32.33. The male patient’s SNP/CN microarray copy number analysis revealed a de novo 4.62 Mb interstitial deletion 46,XY, del(2) (q11.2q11.2). Conclusions: Our findings suggest that patients with partial trisomy 14q32 or monosomy 2q11 can be easily misdiagnosed with PWS during early childhood, however, the typical features will change during adolescence. Utilization of new genetic tools accompanied by genetic counseling is imperative in appropriate diagnosis of these microduplication/microdeletion syndromes and may aid in predicting associated characteristics and medical management. - 1 - Growth Hormone Effects in Adults with Prader-Willi Syndrome Merlin G. Butler1, Bryan Smith2, Jaehoon Lee3, Candy Schmoll4, Wayne Moore4, Joe E. Donnelly2 1Departments of Psychiatry & Behavioral Sciences and Pediatrics, University of Kansas Medical Center, Kansas City; 2Center for Physical Activity & Weight Management and 3Center for Research Methods and Data Analysis, University of Kansas, Lawrence; 4Department of Pediatrics, Children’s Mercy Hospital, Kansas City, Missouri Introduction/Background: Prader-Willi syndrome (PWS) is characterized by short stature, reduced lean body mass and increased fat mass while several trials of growth hormone treatment in children with this disorder have demonstrated beneficial effects on body composition, stature and physical strength and endurance. There is a paucity of data on the use of growth hormone treatment in adults with PWS. Therefore, the main research aim of our study was to examine the effects of growth hormone therapy on body composition, physical activity and energy balance in adults with PWS and the impact of cessation of treatment at 12 months. Methods: We screened 12 genetically confirmed adults with PWS and enrolled 11 adults (6F:5M; average age ± SD = 32.3y ± 11.1y; age range = 23y to 50y). The average weight, height and BMI for the 5 males were 98.9 kg, 154.2 cm and 41.6, respectively and 72.5 kg, 144.7 cm and 34.5 for the 6 females. Nine adults had the 15q11-q13 deletion, one showed maternal disomy 15 and one had an imprinting defect. All subjects had low IGF-1 levels and received daily injections of growth hormone (Genentech Nutropin AQ; 0.0125 mg/kg/day). Growth hormone was maintained within therapeutic range for at least 9 of the 12 months of treatment. Fasting blood samples were obtained for general chemistry and for IGF-1, glucose, thyroid, insulin and lipid levels. Dual energy x-ray absorptiometry (DEXA) for body composition, voluntary physical activity measured by CSA accelerometers and strength using the one repetition of maximum method (1RM) with two exercises (bench and leg press) and energy expenditure measures by the use of a whole room respiration chamber for an 8 hour duration at each assessment over the two year period (at baseline, at 12 months after onset of growth hormone therapy and at 24 months after one year of cessation of growth hormone treatment). The data were analyzed using linear mixed modeling to handle non-independence of the data where observations on the same participant were repeatedly collected. In the mixed models, total lean gram, total tissue percent fat, average counts of moderate-vigorous bouts per day, average length of moderate-vigorous bouts per day, IGF-1 and HDL were contrasted between the three measurement periods (baseline, 12 months, 24 months) adjusting for the participant’s gender. All analyses were conducted using SAS 9.2 version. Results/Discussion: In general, total lean gram, moderate-vigorous bouts measures, IGF-1 and HDL increased during the growth hormone treatment (baseline to 12 months) but after treatment offset (12 to 24 months), they decreased back to the baseline levels. In contrast, the participants reduced total tissue percent fat during the first 12 months during growth hormone treatment, but regained more than they lost during the following 12 months. All these changes were significant at 0.05 alpha levels, except for moderate-vigorous bouts changes from 12 to 24 months and HDL change from baseline to 12 months. There were no significant differences between time points for resting metabolic rate, 8 hour energy expenditure, or respiratory quotient (RQ). Conclusions: The beneficial effects of growth hormone treatment noted in treating children with PWS were identified in our adults during the 12 months growth hormone treatment interval but body composition and physical activity measures and both HDL and IGF-1 levels regressed to baseline after treatment cessation for 12 months. The growth hormone treatment had no apparent effect on energy expenditure. - 2 - Serum IGF-1 Levels Do Not Correlate with Growth Hormone Dose in Children with Prader-Willi Syndrome Diane E. J. Stafford, MD Children’s Hospital, Boston, Harvard Medical School, Boston, MA Introduction/Background: Since growth hormone therapy was first approved for children with Prader-Willi Syndrome in 2000, its use has grown significantly to the benefit to many of these patients. Dosing of growth hormone has traditionally been based on body weight with a manufacturer’s recommended dose of 0.24 mg/kg/week. However, concerns about the possible side effects of growth hormone therapy and the desire to optimize therapy for its beneficial effects have raised questions about how to determine an appropriate dose. In this study, we investigated the relationship between growth hormone dose and measured IGF-1 level in patients with PWS to determine if these are correlated in this group of patients as well as if they are correlated in any individual patient. Methods: Patients with Prader-Willi Syndrome followed at Children’s Hospital Boston and seen between December 1995 and July 2010 were identified by ICD-9 code for PWS. Sixty-seven patients were identified and data from 754 visits were reviewed for growth hormone dose (calculated as mg/kg/week and mg/m2/week), IGF-1 level and other growth characteristics. Correlation coefficients were calculated for 1) IGF-1 and growth hormone dose (mg/kg/week) and 2) IGF-1 and growth hormone dose (mg/m2/week) for all patients as a group and also for 17 individuals with data for more than 5 visits. Results/Discussion: Average age of the patients reviewed was 7.03 years (0-24 years) and average growth hormone dose was 0.157 mg/kg/week or 4.685 mg/m2/week. For the group as a whole, the correlation coefficient between IGF-1 and growth hormone dose in mg/kg/week was 0.26 indicating large variability in IGF1 level for any given dose of growth hormone. The correlation coefficient between IGF-1 and growth hormone dose in mg/m2/week was higher at 0.45, but still reflecting large variation. For most individuals with five or more visits that included measurement of IGF-1, there was no clear correlation between growth hormone dose and IGF-1 level when evaluated as either mg/kg/week or mg/m2/week. For three individual, the correlation between IGF-1 and growth hormone dose was very strong, but evaluation of other associated data provided no insight into any predictive characteristics of these children. Conclusion: Growth hormone therapy has been shown to benefit children with Prader-Willi Syndrome in a variety of aspects. Appropriate dosing of growth hormone for these children, however, has remained difficult to determine and clinical practice is variable. Based on this review of 67 patients with Prader-Willi syndrome, serum IGF-1 levels in those treated with growth hormone are highly variable whether dosing is based on body weight or body surface area. This data supports the need to individualize growth hormone dosing based on measurement of IGF-1 levels. Serial measurements are necessary in individuals when growth hormone doses are altered as there is frequently no linear correlation between dose and IGF-1 level, even in the same patient. Clinicians who prescribe growth hormone therapy for PWS should adjust growth hormone dose based on serum IGF-1 in addition to longitudinal growth rate and body weight. - 3 - Mechanism of MBII-52 and MBII-85 snoRNA Processing Marina Falaleeva, Manli Shen, Justin Surface and Stefan Stamm University of Kentucky, Lexington KY, USA Introduction/Background: MBII-52 and MBII-85 RNAs are localized in the Prader-Willi critical region and have all canonical sequences elements of C/D box snoRNAs. A crucial difference between conventional C/D box snoRNAs and MBII-52 and MBII-85 is that the later are further processed into smaller RNAs that we termed psnoRNAs for processed snoRNAs (1,2). Recent analysis of high-throughput sequencing data indicate that a large number of C/D box snoRNA expressing units give rise to metabolically stable fragments of snoRNAs, suggesting that psnoRNAs represent a large class of new RNAs (3). Methods: RNA was isolated from yeast cells, mouse brains and HEK 293T cells using the Trizol reagent. RNase protection assays were used to analyze snoRNAs processing products. Standard cloning procedures were used to generate MBII-52 snoRNA mutants and to clone MBII-52 and MBII-85 snoRNA into yeast plasmid reporters. Results/Discussion: To determine cis-elements that distinguish psnoRNAs from canonical snoRNAs, we analyzed mutant MBII-52 expression units. Similar to C/D box snoRNAs, psnoRNA expression depends on intact C and D boxes, an intact k-turn motif as well as proper splicing of the hosting intron. In contrast to C/D box snoRNAs, the location of the psnoRNA in the intron has no effect on expression and further processing. We tested trans-acting factors by gene knockdown and use of patient cell lines. We found that psnoRNA production is independent from dicer, pasha and argonautes (ago1-4), proteins that function in miRNA processing. Surprisingly, moving the MBII-52 and MBII-85 RNAs into S. cerevisiae, flanked by heterologous yeast exons and introns, resulted in a processing pattern identical to mouse brain. These data indicate that psnoRNA processing is independent from enzymes of the miRNA processing pathways and flanking intron sequences. Use of knockout S. cerevisiae strains showed that MBII-52 and MBII-85 processing is dependent on debranching enzyme (Dbr1) as well as exosome complex components. Microinjection of oligonucleotides corresponding to psnoRNAs demonstrated that they are mainly located in the nucleoplasm, which again is different from canonical C/D box snoRNAs that are nucleolar. Conclusion: The Prader-Willi critical region expresses predominantly processed snoRNAs, not canonical C/D box snoRNAs that associate with different proteins and have different functions in gene expression. psnoRNAs share the importance of C/D boxes, k-turn motif and intron release with canonical snoRNAs. They differ in their dependency on proper intronic localization and their subnuclear localization. They are not dependent on components of the miRNA pathway and most likely the result of RNase actions. 1. 2. 3. Kishore, S., Khanna, A., Zhang, Z., Hui, J., Balwierz, P., Stefan, M., Beach, C., Nicholls, R.D., Zavolan, M. and Stamm, S. (2010) The snoRNA MBII-52 (SNORD 115) is processed into smaller RNAs and regulates alternative splicing. Hum Mol Genet, 19, 1153-1164. Shen, M., Eyras, E., Wu, J., Khanna, A., Josiah, S., Rederstorff, M., Zhang, M.Q. and Stamm, S. (2011) Direct cloning of double-stranded RNAs from RNAse protection analysis reveals processing patterns of C/D box snoRNAs and provides evidence for widespread antisense transcript expression Nucleic Acids Res, in press. Falaleeva, M., Stamm, S. (2011). Fragments of small nucleolar RNAs as a new source for non-coding RNAs. in: Regulatory RNAs by Z. Ghosh and B. Mallick, Springer, in press. - 4 - Molecular Function of psnoRNAs Derived from HBII-52 and HBII-85 Expression Units Marina Falaleeva1, Justin Surface1, Manli Shen1, Pierre de la Grange2 and Stefan Stamm1 1University of Kentucky, Lexington KY, USA; 2Hopital Saint Louis, IUH, Centre Hayem, Paris, France Introduction/Background: C/D-box small nucleolar RNAs (snoRNAs) are small, non-protein coding RNAs that have been mainly implicated in 2’-O-methylation of pre-rRNAs in nucleoli. SnoRNAs found within PraderWilli region (MBII-52 and MBII-85) do not posses binding sites for rRNA and their function is poorly understood. We showed that RNAs from these C/D box snoRNA expressing units are further processed into small RNAs that we called psnoRNAs (processed snoRNAs). In contrast to canonical snoRNAs, psnoRNAs associate with common hnRNPs and have different function in gene regulation (1,2,3). Methods: RNA was isolated from posterior hypothalamus of subjects diagnosed for PWS or from HEK 293T cells after transfection of MBII-52 or MBII-85 or both snoRNAs. Genome-wide exon junction arrays were used to monitor changes in gene expression, both in RNA abundance and alternative splicing. These changes were confirmed by RT-PCR and Western blot analysis. Results/Discussion: As a result of MBII-52 overexpression we could monitor changes in overall expression of several genes. Interestingly, five out of nine genes were connected with fat/energy metabolism. RT-PCR and Western blot validation showed notable changes in expression of two genes: FIT-2 (fat storage-inducing transmembrane protein) and PEX11A (peroxisomal biogenesis factor 11 alpha). A putative MBII-52 snoRNA binding site was found within intronic sequences of the genes. MBII-85 snoRNA overexpression changed the overall expression of 171 genes, while overexpression of both MBII-52 and MBII-85 snoRNAs gave 309 changes. 38 were genes were changed by either MBII-52 or MBII-85 snoRNA overexpression. Analysis of RNA from human PWS brains showed changes in overall expression of 7281 genes and 195 splicing events. Thirteen genes were changed between the cells with MBII-85, MBII-52/85 overexpression and PWS brains; 55 genes are common for MBII-52/85 and PWS, 52 genes are common for MBII-85 and PWS, 4 genes are common for MBII-52 and PWS array experiments. Changes in overall gene expression of 10 targets (MAP2, ST6GALNAC2, CGD91, PRKCE, NR1H2, SMAD, ST3GAL, ACOXL, CYP46A1, MXRA8) have been validated by RT-PCR. Those genes function in cytoskeleton dynamic/cell-cell interaction (MAP2, MXRA8, ST6GALNAC2, ST3GAL), fat/energy metabolism (ACOXL, CYP46A1, CGD91) and signal transduction (NR1H2, PRKCE, SMAD). Conclusion: Our results indicate that MBII-85 and MBII-52 derived psnoRNAs regulate the expression of multiple RNAs, consistent with their association with a syndrome. The deregulated genes are enriched in biochemical pathways regulating fat/energy metabolism, cell-cell interactions and signal transduction. The strong influence of psnoRNA overexpression on gene expression further underlines that these RNAs have different function of canonical C/D box snoRNAs. Transfection experiments indicate that MBII-52 and MBII-85 act synergistically on some RNA targets, which should be taken into account for the design of rationale therapies. 1. 2. 3. Kishore, S., Khanna, A., Zhang, Z., Hui, J., Balwierz, P., Stefan, M., Beach, C., Nicholls, R.D., Zavolan, M. and Stamm, S. (2010) The snoRNA MBII-52 (SNORD 115) is processed into smaller RNAs and regulates alternative splicing. Hum Mol Genet, 19, 1153-1164. Shen, M., Eyras, E., Wu, J., Khanna, A., Josiah, S., Rederstorff, M., Zhang, M.Q. and Stamm, S. (2011) Direct cloning of double-stranded RNAs from RNAse protection analysis reveals processing patterns of C/D box snoRNAs and provides evidence for widespread antisense transcript expression Nucleic Acids Res, in press. Falaleeva, M., Stamm, S. (2011). Fragments of small nucleolar RNAs as a new source for non-coding RNAs. in: Regulatory RNAs by Z. Ghosh & B. Mallick, Springer, in press. - 5 - Hyperghrelinemia Begins Early in Prader-Willi Syndrome Frederick A. Kweh, Jennifer L. Miller, Carlos R. Sulsona, Daniel J. Driscoll College of Medicine and Department of Pediatrics, University of Florida, Gainesville Introduction: Obesity is the major cause of morbidity and mortality in Prader-Willi syndrome (PWS) and typically begins between 1-4 years of age. The driving mechanisms behind the development of obesity in PWS are unclear. Ghrelin is an orexigenic hormone that increases food intake while decreasing energy expenditure and fat catabolism. It is significantly elevated in older children and adults with PWS. However ghrelin’s role in the obesity and hyperphagia in PWS remains unclear and its level in young children with PWS is controversial. In this study, we measured ghrelin levels in individuals with PWS from early infancy to 36 years of age. Individuals with non-PWS early-onset morbid obesity (EMO) and normal weight sibling controls were used as comparison groups. Methods: Fasting serum ghrelin was measured using a fluorescent Enzyme-linked Immunosorbent Assay (ELISA) kit from Phoenix Pharmaceuticals, Inc., California, USA. Most of the study subjects (PWS, EMO and siblings) had fasting serum samples collected more than once at different time points during the course of our Rare Disease Natural History study. We analyzed 136 PWS fasting serum samples (73 subjects); 55 EMO samples (40 subjects); and 143 sibling samples (95 subjects) for a total of 334 fasting samples. Results: Serum ghrelin was significantly elevated in children with PWS between the ages of 0 and 5 years relative to the control siblings (p=0.0057), but was not significantly higher than in the EMO group (p=0.9951). After 5 years serum ghrelin levels decreased significantly in all groups with the EMO group showing the greatest decrease. PWS serum ghrelin levels were significantly higher than the EMO group in the 5-12 year age range (p=0.0095), but not the control sibling group (p=0.0631). After 12 years of age there was a significant decrease in serum ghrelin in the sibling group. Teenagers (12-20 years) and adults (20-36 years) with PWS had significantly higher ghrelin levels than their counterparts in the EMO and sibling groups. We found that serum ghrelin was significantly elevated in PWS children well before the onset of obesity and hyperphagia (p<0.0001). In fact, the highest ghrelin levels were seen in the first nutritional phase (1a) of PWS, which is a time of poor feeding and reduced appetite. Interestingly, the most significant decrease in PWS serum ghrelin (p=0.0032) coincided with the transition from phase 1b (relatively normal infant growth and appetite) to phase 2a (rapid weight gain with no significant change in appetite or caloric intake). Discussion: Serum ghrelin levels were measured in individuals with PWS from 2 months to 36 years of age. We found that ghrelin levels were significantly elevated beginning in early infancy in PWS well before the onset of obesity and hyperphagia. Given that ghrelin levels were the highest in PWS in infants still in the poor appetite phase (i.e., 1a) it seems unlikely that elevated ghrelin levels are causing the switch to the hyperphagic phases of PWS. However, it has been shown in mice that ghrelin can also act to increase fat mass independent of its effect on appetite (Perez-Tilve et. al, FASEB J. 25:2814, 2011). Therefore, it is likely that the elevated ghrelin levels are causing the increased fat mass seen in infants with PWS compared to normal infants with similar body mass indices (BMI). - 6 - Two More Children Born to Women with Prader-Willi Syndrome, One Normal, One with Angelman Suzanne B. Cassidy, Divya Vats Division of Medical Genetics, Dept. of Pediatrics, University of California San Francisco Introduction/Background: Hypogonadism is one of the major consensus clinical diagnostic criteria for PraderWilli syndrome and contributes to the pathogenesis, physical features and natural history of the disorder. It usually manifests as genital hypoplasia, delayed and incomplete pubertal development, and infertility. The hypogonadism is largely of hypothalamic origin but has recently been shown to also involve primary gonadal defect. Most studies in females demonstrate primary amenorrhoea or oligomenorrhea with delayed menarche. The extent of sexual activity in adults is unknown. Fertility has never been reported in males and reported only twice in females with molecularly confirmed PWS, one with deletion 15q11.2-q13 and the other with maternal uniparental disomy (UPD) 15. One other unpublished case has also been noted worldwide. Case Reports: We report a 34 year old woman with PWS due to deletion 15q who has most of the typical manifestations of the disorder including mild obesity and associated type II diabetes mellitus. She had menarche at 21 with subsequent normal menstruation. At 27 years of age, she was determined to be pregnant with a 7 month fetus when investigated for rapid weight gain and unexplained pedal edema. She was not known to be sexually active and was not on any form of hormonal therapy or contraception. A normal male was delivered by C-section at term, with postnatal maternal respiratory distress for two weeks. The now 8 year old boy is phenotypically and developmentally normal, and genotyping for AS and PWS is negative. We have also learned of another woman in New Zealand, now 38 years of age, who has PWS due to deletion and had a pregnancy which was detected at 36 weeks gestation due to pedal edema and weight gain. She had gestational diabetes, and now has insulin-dependent diabetes. She had menarche at 20 years and has regular periods. She had not been on hormones. She had weighed about 100 kg and had “heart congestion” and behavioral issues, but lost weight to about 79 kg the year before pregnancy. She received citralopram for the 2 years up to the time of pregnancy. She was delivered by planned C/section. She had a daughter who has Angelman syndrome due to del 15q. Discussion/Conclusion: These cases represent the 3rd and 4th reported females with PWS who brought a pregnancy to term. All were on behavioral medications (SSRIs or antipsychotics) at the time they became pregnant, possibly stimulating their FSH and LH response and increasing the likelihood of ovulating and establishing a pregnancy. Three of the four with fertility had significant weight loss prior to pregnancy; the other was never obese. Thus it appears that infertility is not a consistent feature in females with PWS and that there is a variable degree of reduced fertility in untreated females with PWS of any molecular genetic etiology. Though hypogonadism is an important diagnostic feature, it should not preclude the possibility of pregnancy without testing, and sex education and discussion of contraception should be part of management of women with PWS. - 7 - Direct Cloning of Double-Stranded RNAs from RNase Protection Analysis Reveals Processing Patterns of C/D Box snoRNAs in PWS Critical Region and Provides Evidence for Widespread Antisense Transcript Expression Manli Shen1, Eduardo Eyras2, Serene Josiah3 and Stefan Stamm1 1Department of Biochemistry and Molecular Biology, College of Medicine, University of Kentucky, Lexington, KY, 2University Pompeu Fabra, Catalan Institution for Research and Advanced Studies, Passeig Lluis Companys, Barcelona, Spain, 3Shire Human Genetic Therapies Introduction/Background: The Prader-Willi Syndrome is likely linked to the loss of expression from the maternally imprinted small nucleolar RNA (snoRNA) SNORD116 (HBII-85) in the PWS critical region. As an orphan C/D box snoRNA, the biogenesis and biological function of SNORD116 still remains largely unknown. Similar to the downstream snoRNA SNORD115 (HBII-52), SNORD116 also contains tandemly repeated copies and is processed into shorter RNAs (psnoRNAs). In order to further understand this snoRNA, we cloned the processed snoRNAs from one SNORD116 expression unit using a newly developed technique to directly clone dsRNAs from from RNase Protection Assays. Methods: RNase Protection Assays was performed using a full-length copy of one mouse SNORD116 snoRNA as a probe. This protection assay shows that similar to SNORD115, SNORD116 is processed into smaller RNAs. The shorter RNase-protected fragments (psnoRNAs) were cloned and sequenced. Results/Discussion: The mouse C/D box snoRNA SNORD116 (MBII-85) is processed into at lease five shorter RNA fragments using processing sites near known functional elements of C/D box snoRNAs. The comparison with high-throughput sequencing data indicates that all MBII-85 psnoRNA are processed similarly. The comparison with the processing pattern of SNORD115 shows that both snoRNAs are processed in similar regions. Surprisingly, and unrelated to SNORD116, the majority of cloned RNAs from RNase protection were derived from endogenous cellular RNA, indicating widespread antisense expression. The cloned dsRNAs could be mapped to genome areas that show RNA expression on both DNA strands and partially overlapped with known argonaute-binding sites. Conclusion: The data suggest a conserved processing pattern for PWS critical region C/D box snoRNAs and abundant expression of longer, non-coding RNAs in the cells that can potentially form dsRNAs. The considerable conservation of the cleavage patterns of snoRNAs indicates that psnoRNAs are generated by a processing pattern and are not the result of random degradation. Thus, the data show that the PWS critical region gives rise to short processed snoRNA, not just canonical C/D box snoRNAs, which should be the target for therapeutic intervention. Reference: Shen, M., Eyras, E., Wu, J., Khanna, A., Josiah, S., Rederstorff, M., Zhang, M.Q. and Stamm, S. (2011) Direct cloning of doublestranded RNAs from RNAse protection analysis reveals processing patterns of C/D box snoRNAs and provides evidence for widespread antisense transcript expression Nucleic Acids Res, in press. - 8 - Loss of the Prader-Willi Syndrome Candidate Gene Magel2 Impairs Leptin Signaling in Mice Rebecca E. Mercer1, William F. Colmers2 and Rachel Wevrick1 1Departments of Medical Genetics and 2Pharmacolog, University of Alberta, Edmonton, Alberta, Canada Introduction: The brain actively senses circulating adiposity and satiety factors, and initiates responses to control short- and long-term energy balance. Leptin, a key hormone produced by fat tissue, acts on leptin receptors on hypothalamic neurons. In turn, these neurons produce a coordinated response that inhibits appetite and increases energy expenditure. The leptin signaling pathway has garnered increased attention because leptin insensitivity is found in both genetic and diet-induced forms of obesity. Mutations in genes encoding leptin, leptin receptor, SH2B1 (a leptin receptor adaptor protein), or the melanocortin receptor MC4R, a downstream target of leptinresponsive neurons, cause severe, early-onset obesity in humans and in rodents. We now show that one of the genes inactivated in PWS, namely MAGEL2, is important for leptin responses in the hypothalamic neurons that regulate energy balance. Methods: Mice in which Magel2 is disrupted have less lean mass and twice the fat mass of age-matched control mice, and are also far less active. We used feeding studies and electrophysiological measurements in hypothalamic neurons to test leptin responses in Magel2-null mice. Results: Intra-peritoneal injection of leptin into control mice reduced their food intake over the following 24 hours. In contrast, no reduction in food intake was noted in Magel2-null mice injected with leptin. This suggests that Magel2 is required for the central nervous system response to circulating leptin. Next, we used whole cell patch-clamp recordings in brain slice preparations to study leptin responses specifically in neurons that express the leptin receptor. Two types of energy-balance related neurons are normally detected in the arcuate nucleus of the hypothalamus: neurons that are inhibited by leptin (neuropeptide Y (NPY) neurons), and neurons that are excited by leptin (pro-opiomelanocortin (POMC) neurons). Inhibition of NPY neurons reduces the release of orexigenic peptides, reducing the drive to eat. Activation of POMC neurons facilitates the release of anorexigenic peptides, promoting satiety and increasing energy expenditure. While both types of neurons were detected in hypothalamic slices from control mice, no neurons were activated by leptin in hypothalamic slices derived from Magel2-null mice. Conclusions: Our results demonstrate that Magel2 is essential for the centrally-mediated anorexigenic effect of leptin on food intake in vivo and for the activation of anorexigenic neurons in the hypothalamus. This leptin insensitivity results in increased fat mass and reduced activity in mice lacking Magel2. Our data further suggest that loss of MAGEL2 contributes to increased fat mass, reduced satiety, and reduced voluntary activity in PWS. We hypothesize that Magel2/MAGEL2 is an adaptor protein within an intracellular signaling cascade in subtypes of hypothalamic neurons, including neurons that are normally activated by leptin. We propose that defective leptin signaling in hypothalamic neurons mechanistically links the severe obesity present in individuals with leptin receptor, SH2B1, or MC4R mutations with obesity and lack of satiety in Prader-Willi syndrome. Supported by a “Big Ideas Grant” on Hyperphagia from the Prader-Willi Syndrome Association (USA). - 9 - The Behavior/Neuropsychiatry Review - 10 - Social Functioning in Prader-Willi Syndrome Anastasia Dimitropoulos, PhD Department of Psychological Sciences, Case Western Reserve University, Cleveland, Ohio Introduction/Background: In addition to a well-described behavioral phenotype that includes hyperphagia, obsessive-compulsive symptoms, disruptive behavior, and cognitive delays, research also suggests that some persons with Prader-Willi syndrome (PWS) have repetitive behavior and social deficits reminiscent of autism spectrum disorders (ASD). Although repetitive behavior has been well characterized in this population, social functioning has not been well studied thus far. The few findings that have been reported indicate that social problems are common in PWS with individuals with PWS exhibiting more problems with social competence and making fewer gains in competence with age compared to individuals with other neurodevelopmental disorders (Rosner et al., 2004). Further examination of social functioning in PWS is also warranted in light of findings implicating the 15q11-q13 region as a genetic susceptibility region for idiopathic autism. In addition, research to date indicates individuals with the maternal uniparental disomy (m-UPD) subtype of PWS are at greater risk for autistic symptomatology than those with paternal deletions (DEL) of 15q11-q13. The purpose of this research is to examine social competence and responsiveness in individuals with PWS in direct comparison to individuals with ASD and to examine those abilities with respect to PWS genetic subtypes. Methods: 42 individuals with PWS (23 DEL, 19 m-UPD) and 19 individuals with an ASD (7-36 Years old) and their caregivers comprised the total sample. Participants underwent intelligence testing (WISC-IV, WAIS-III, or WASI) and a battery of social and cognitive assessments as part of a larger project; caregivers were interviewed on adaptive functioning (Vineland Adaptive Behavior Scales) and the Autism Diagnostic Inventory-R (ADI-R), and completed the Social Competence Inventory (SCI; Rydell, 1997) and Social Responsiveness Scale (SRS; Constantino & Gruber, 2005). Results & Discussion: For social responsiveness, SRS-Total score significantly differed between ASD, m-UPD, and DEL groups (F = 7.275, p =.002; controlling for age and IQ). Posthoc comparisons indicate significantly more social difficulties were present for participants with ASD and m-UPD than those with DEL. 78.9% of mUPD and 36.4% of DEL participants scored in the highest clinically significant range indicating severe interference in everyday social interactions. For both UPD and DEL, SRS subscales with highest endorsement included Autistic Mannerisms (e.g., stereotypies and restricted interests) and Social Cognition (the ability to understand social cues). However, all SRS subscale means reached clinically significant cutoffs for UPD and four out of five reached cutoffs for DEL. Groups also differed significantly on measures of social competence. Participants with m-UPD and ASD evidenced greater impairment in the SCI Prosocial Orientation Subscale (e.g., empathy, understanding of others, helpfulness) than those with DEL (F=7.2, p=.002 controlling for age and IQ). No differences were found between groups on the Social Initiative Subscale [DEL = 3.04(.82), m-UPD = 2.64(.72), ASD = 2.51(.72)]. Among those with PWS, the SRS-Total score and SCI Prosocial Orientation was significantly negatively correlated with Vineland Social Subscale. These findings indicate individuals with PWS have difficulty initiating social interaction (e.g., making contact with unfamiliar peers) and may be prone to social hesitancy or withdrawal similar to those with an ASD. Prosocial behaviors such as generosity, empathy, and helpfulness were more evident in those with DEL subtype than in individuals with m-UPD or ASD. Results will be discussed in relation to ADI-R diagnostic criteria. These findings give further insight into the social functioning of persons with PWS and indicate need for social-skills intervention in this population. This research was funded by a grant from the PWSA (USA) - 11 - Psychiatric Symptoms in Prader-Willi Syndrome Elizabeth Roof, Carolyn Shivers, Lauren Deisenroth and Elisabeth Dykens Vanderbilt Kennedy Center, PMB 40, 230 Appleton Place, Nashville, TN 37203 Introduction: Although many persons with PWS have problems in thinking, mood and social interactions, most do not meet formal criteria for ASD, psychosis, or other psychiatric disorders. Even so, studies to date on psychopathology in PWS rely primarily on psychiatric diagnoses, and these labels differ considerably across countries, clinical perspectives, labs, and nosologies (i.e., ICD-10, DSM-IV, adapted systems). Making reliable psychiatric diagnoses is also challenging in people with intellectual disabilities in general (Dykens, 2000), which further clouds diagnoses in PWS. Among adolescents and adults with PWS, data are needed on the emergence of specific symptoms of psychosis and affective illness. Those with mUPD are at particularly high risk for these disorders, and some assert that all mUPD cases will develop severe illness, with initial episodes seen in late adolescence or young adulthood (Boer et al., 2002; Vogels et al., 2003; Whittington & Holland, 2004). If so, then PWS due to mUPD may provide an extremely useful window into psychosis in the general population. We hope to identify specific symptoms in PWS and how these emerge and change over the course of time. Methods: This study includes a sample of 94 individuals (48 males) with PWS aged 4 to 50 years, with a mean age of 14.94 years. Participants were recruited with assistance from the PWSA, and through our ongoing research program on PWS conducted at Vanderbilt Kennedy Center. Parents or caregivers completed an in-depth interview with a trained clinician of past and current psychiatric symptoms (K-SADS-PL) and Scale of Prodromal Symptoms (SOPS) and Positive and Negative Syndrome Scale (PANSS) that might indicate increased risk of psychotic symptoms or its precursor. Their offspring with PWS were also observed throughout the day in formal and informal settings to assess these behaviors by the same clinician to determine diagnosis and severity of impairment. Parents also completed a family psychiatric history questionnaire for issues like anxiety, depression and substance abuse to determine family risk factors. Results: Those with the mUPD subtype versus Deletion subtype of PWS showed a significant increase of psychotic symptoms (t= -2.00, p<.05) on the K-SADS-PL with delusions, magical thinking and other perceptual disturbances being the most commonly endorsed features. In addition, age is positively correlated with brief reactive psychosis (r=.29, p<.05) and negatively correlated with ADHD. Those with Imprinting Mutation subtype of PWS are also scoring significantly higher on the psychotic subtype, suggesting they may share some common psychiatric features with those who have the UPD subtype. Discussion: Findings will be discussed further in terms of further refined genetic subtypes (Type I and Type II), gender and age differences, and relation to hyperphagia. Focus will be given to potential family risk factors that may be superimposed on top of the PWS genetic phenotypic predisposition for psychiatric symptoms and how these emerge and change over time. - 12 - The Effect of Residential Placement on Weight Control of Individuals with Prader-Willi Syndrome: an Outcome Evaluation L. Spanbauer, MS, RD, CDN1; K. Stote, PhD, MPH, RD2 1Consultant for Catholic Charities Disabilities Services, Albany, NY, Adjunct Instructor, State University of New York, Empire State College, Center for Distance Learning, Saratoga Springs, NY; 2Assistant Professor State University of New York, Empire State College, Center for Distance Learning, Saratoga Springs, NY Learning Outcome: To advance understanding of effective weight management strategies for adults with Prader-Willi Syndrome (PWS). Methods: A convenience sample all female adults (N=8) diagnosed with PWS and who live in several residential facilities for individuals with developmental disabilities located in Upstate NY was taken. All study participants reside in a New York State approved facility for individuals with developmental disabilities that provides twenty four hour, seven day a week supervision within a food secure environment. In addition, compliance to specific calorie meal plans along with a minimum of thirty minutes of physical activity were included as part of their daily goals. The following variables were extracted from individual medical records; age at time of study, gender, date of admission, ideal body weight, pre-admission weight, pre-admission Body Mass Index (BMI), weight and BMI at time of study. Results: Study participants (N=8) had a mean age of 30 years (range: 38 to 18) and an average pre-admission BMI of 39±14 kg/m2. The mean amount of time since admission into the approved facility was 6.3±5 years. With the exception of only one participant, all those included in the study sample experienced weight loss and a decrease in BMI. The mean amount of weight loss by study participants was 22kg. The greatest amount of weight loss was 65kg, however; one individual was noted to have a 7 kg weight gain since admission. In addition to weight loss, across all those study participants who lost weight (7 of 8) BMI was noted to decrease by 42%, resulting in a mean BMI of 26.4 kg/m2 (compared to the mean pre-admission BMI of 39±14 kg/m2 prior to residing in the food secure environment). Conclusion: Among those females with PWS included in the study, the introduction of a supervised, food secure environment for people with PWS results in overall weight loss and improvement in BMI. Funding Disclosure: No Acknowledgment: Special thanks to Catholic Charities Developmental Disabilities Services, Upstate, NY, the State University of New York, Empire State College, Center for Distance Learning, Saratoga Springs, New York and Sarah J. Mclean, PhD - 13 - Parental Role in Physical Activity among Children with Prader-Willi Syndrome Jie Weiss, PhD, Michele Mouttapa, PhD, and Daniela Rubin, PhD California State University, Fullerton Introduction/Background: It has been demonstrated that parents play a role in influencing their children’s health-related behaviors. Physical activity is vital to the management of Prader-Willi Syndrome (PWS). One of the determinants of youth physical activity (PA) is the parents’ own PA. Cognitively, parents’ views of the consequences of PA among children predict the child’s PA level. This study examined associations between parents’ self-reported physical activity (PA) and PA of their children with PWS. This study also explored relationships between parents’ perceived consequences of their child’s PA, and child’s actual PA involvement, using the Multi-Attribute Utility (MAU) decision making model as the theoretical framework. Methods: Data was collected from 90 parents of children ages 5 and older with PWS. The survey was mailed to all members of the Prader-Willi California Foundation registry with an information sheet about the purpose of the project. We measured physical activity levels among parents and their children with PWS. We also measured parents’ utilities for PA for their children. Logistic regression examined the association between parental PA levels and the PA involvement of their children with PWS as well as the association between parental perceived utility about their children’s PA and their children’s actual PA involvement. Results/Discussion: Standardized regression coefficients (β) indicated that parents’ estimated duration of their own PA per session was positively associated with the number of structured PA minutes that their children with PWS engaged in. The most positive consequence was “child becoming more physically fit”, and the most negative consequence was “child becoming frustrated”. Vigorous PA among children with PWS was associated with the following consequences: 1) “child not enjoying PA” (negative association), 2) “child in a better mood” (positive association), 3) “child being more energetic” (positive association), and 4) “child not performing PA well” (negative association). Conclusion: The observed positive influence of parental PA on children’s PA suggests that one potentially effective strategy to increase PA among children with PWS may be through promotion of PA among parents. Because children with PWS are more dependent on their parents compared to children without PWS, they may especially benefit from parental support for a healthy lifestyle. - 14 - The Relationship between Early-Onset Obesity and Behavior Krista S. Garner1,2, Jennifer L. Miller2, Jonathan J. Shuster3, John H. Kranzler1, and Daniel J. Driscoll2,4 1Department of Special Education, School Psychology, and Early Childhood, College of Education; 2Department of Pediatrics, College of Medicine; 3Department of Health Outcomes and Policy, College of Medicine; Center for Epigenetics, 4University of Florida, Gainesville, FL Introduction: Although several studies have examined the relationship between obesity and behavior and Prader-Willi syndrome (PWS) and behavior, there is still much to be learned. The present study examined and compared not only the maladaptive behaviors, but also the adaptive behaviors of individuals greater than or equal to 6 years of age in 3 different groups: 1) non-PWS individuals with early-onset morbid obesity (EMO); 2) individuals with PWS; and 3) typically developing sibling controls using the parent, teacher, and self-report ratings of the Behavior Assessment System for Children, Second Edition (BASC-2). The BASC-2 is a multimethod and multidimensional system that can be used to evaluate the behavior and self-perceptions of children and young adults aged 2 through 25 years. Methods: Clinical data on individuals with EMO (N = 28 parent data, N = 22 teacher data, and N = 23 selfreport data), individuals with PWS (N = 29 parent data, N = 24 teacher data, and N = 29 self-report data), and normal weight sibling controls (N = 57 parent data, N = 45 teacher data, and N = 48 self-report data) in a University of Florida cohort were linked to parent, teacher, and self-report assessment using the BASC-2. All PWS individuals had appropriate genetic testing to determine their molecular class and sub-class. The individuals with EMO all had a BMI > 98% by age 4 years and normal genetic testing. Results and Discussion: The results of the present study indicate that (according to parent, teacher, and selfreport) individuals with EMO and individuals with PWS tend to behave similarly, on average, and their behavior tends to be more problematic than typically developing individuals. For example, both the individuals with EMO and the individuals with PWS scored significantly worse than their typically developing sibling controls across raters on the Atypicality, Withdrawal, Somatization, Adaptability, Social Skills, and Leadership scales. These findings suggest that individuals with EMO and individuals with PWS tend to display more strange or odd behaviors, tend to be more withdrawn, pessimistic, or sad, tend to display more health-related concerns, tend to be less adaptable to changing conditions, tend to have more difficulty complimenting others and making suggestions for improvement in a tactful and socially acceptable manner, and tend to have more difficulty making decisions, being creative, and getting others to work together effectively than typically developing individuals. Surprisingly, not only did the individuals with EMO typically score more similarly on the BASC-2 to the individuals with PWS than to their normal weight sibling controls across raters, but they also often scored significantly worse than the individuals with PWS. The reasons behind these findings need to be explored further. - 15 - Preliminary Results of Strengths and Weaknesses in Neuropsychological Testing in Children with Prader-Willi Syndrome Marnie Hutchison1, Wing Sze Wence Leung1, Michelle L. Mackenzie2, Andrea M. Haqq2 and Jacqueline Pei1 1Department Alberta of Educational Psychology, University of Alberta, Edmonton, AB, Canada; 2Department of Pediatrics, University of Introduction: Prader-Willi syndrome is well known for negative physical, cognitive, social, and behavioural outcomes. Less is known however, about the neuropsychological effects of the disorder, particularly in children. This ongoing study has examined executive function and attention abilities in 11 children with PWS. Executive functions include a number of specific abilities including inhibition, working memory, set-shifting, strategy employment, and flexible thinking. Executive functions have been defined as being a variety of higher-order mental processes necessary for complex goal-directed behaviour and adaptation to environmental changes and demands. The present study utilized a set of standardized neuropsychological instruments to shed light on a neuropsychological profile of children with PWS. Such a profile will assist intervention efforts so that we can appropriately capitalize on the strengths and address the needs of these children. Method: The present sample comprised 11 children with a confirmed PWS diagnosis who were recruited from Alberta and British Columbia, Canada. We will be reporting on measures of participants’ IQ (Stanford Binet Intelligence Test – Fifth Edition), attention (Test of Variables of Attention- TOVA), and executive function (selected subtests from the NEPSY-II and parental ratings on the Behaviour Rating Inventory of Executive Function- BRIEF). Scale and standard scores were transformed to z scores in order to meaningfully compare performance across measures. Results and Conclusions: The study sample demonstrated an uneven profile suggesting certain areas of strength and weakness and that children’s IQ does not wholly account for performance on these measures. On average, children with PWS obtained abbreviated intelligence scores in the extremely low range. Participants’ verbal and nonverbal working memory scores are comparable to their IQ. Results from the TOVA indicate that these children demonstrate significant difficulty maintaining attention for sustained periods of time and show signs of fatigue and impulsivity. On the NEPSY-II, children with PWS demonstrated relative strengths on Animal Sort and Response Set but showed relative and normative weaknesses on Auditory Attention and Inhibition. On the BRIEF, parents reported children with PWS to have relative strengths with organizing materials, initiating tasks, and holding information in memory. Parents reported normative and relative weaknesses controlling their emotions, changing tasks, resisting impulses, regulating their behaviour, and self-awareness. Although a small sample size limits our ability to generalize results and make detailed conclusions, this preliminary information can begin to inform practice. As such, we will also discuss implications for intervention and support based on this early information. - 16 - The Medical/Nutrition/Endocrine Review - 17 - Hormonal and Metabolic Responses to Endurance Exercise in Prader-Willi Syndrome Daniela A. Rubin, PhD1, Daniel A. Judelson, PhD1, Susan S. Clark, MD2, Diobel M. Castner, MS1, Joane Less, RN2, and Jason Ng, MS1 1Department of Kinesiology, California State University, Fullerton; 2Department of Endocrinology, Children’s Hospital of Orange County Introduction: Prader-Willi Syndrome (PWS) is characterized by several hormonal and metabolic abnormalities resulting in excessive body fat. The purpose of this study was to determine differences in endocrine and metabolic responses to exercise between youth with PWS and those without, accounting for differences in adiposity. Methods: Thirteen youth with PWS (PWS, age = 11.3 ± 1.9 y, height = 150.4 ± 14.0 cm, body mass = 65.2 ± 28.7 kg, and 45.3 ± 10.6% body fat), 12 youth of normal weight without PWS (NW, age = 9.4 ± 1.2 y, height = 140.1 ± 7.6 cm, body mass = 32.6 ± 6.0 kg, and 17.5 ± 4.6 % body fat), and 13 obese youth without PWS (OB, age = 9.3 ± 1.3 y, height = 141.5 ± 8.4 cm, body mass = 50.1 ± 12.8 kg, and 39.1 ± 7.0 % body fat) completed ten two-min exercise bouts, each separated by one-min rest. Ten of 13 youth with PWS were on growth hormone therapy. Mean heart rates were significantly lower in PWS (143 ± 20 bpm) than NW (169 ± 9 bpm) and OB (163 ± 6 bpm). Blood samples were obtained at rest pre-exercise (PRE), immediately post-exercise (IP), and 15 min (+15), 30 min (+30), and 60 min (+60) into recovery. Blood samples were analyzed by enzyme-linked assays for insulin, glucagon, cortisol, insulin-like growth factor 1 (IGF-1) and testosterone. Glucose, lactate, glycerol, and free fatty acids (FFA) were measured by colorimetric assays. Results: ANOVAS showed there were no significant group differences for any of the changes in the hormones in response to the exercise. Youth with PWS had significantly higher IGF-1 and testosterone than NW and OB at all times but the pattern of the response to the exercise was similar to the response of NW and OB children. PRE glucose levels were significantly lower in youth with PWS compared to NW and OB. Glucose significantly decreased with exercise only in NW and OB. Lactate, glycerol, and FFA responses were similar in all three groups. Discussion: Despite baseline differences in IGF-1 and testosterone, youth with PWS respond similarly to acute exercise compared to youth without PWS for several hormones (insulin, glucagon, IGF-1, cortisol, and testosterone). Metabolically, PWS present lower glucose concentrations than NW and OB; however, glucose concentrations do not seem to limit the rate of glycolysis during exercise as indicated by similar lactate responses. Youth with PWS present similar rate of lipolysis as NW and OB in response to acute exercise. Thus, it appears that in childhood and adolescence, PWS does not drastically affect some hormonal and metabolic responses to acute endurance exercise. Supported by US Army Medical Research and Materiel Command Contract W81XWH-08-1-0025 - 18 - Postprandial Cardiac Autonomic Function is Impaired in PraderWilli Syndrome Louise Purtell1, Lisa Sze2, Arthur Jenkins3, Alexander Viardot1, Herbert Herzog4, Amanda Sainsbury-Salis4, Ellie Smith5, Georgina Loughnan6, Katharine Steinbeck6,7, Lesley V Campbell1,8 1Diabetes & Obesity Research Program, Garvan Institute of Medical Research, 384 Victoria Street, SydneyDarlinghurst NSW 2010, Australia; 2Clinics for Endocrinology, Diabetes and Clinical Nutrition, University Hospital Zurich, Zurich, Switzerland; 3School of Health Sciences, University of Wollongong, NSW 2500, Australia; 4Neuroscience Research Program, Garvan Institute of Medical Research, 384 Victoria Street, SydneyDarlinghurst NSW 2010, Australia; 5Department of Cytogenetics, The Children's Hospital, Westmead Clinical School, Westmead NSW 2145, Australia; 6Prader-Willi Syndrome Clinic, Department for Metabolism and Obesity, Royal Prince Alfred Hospital, Sydney-Camperdown NSW 2050, Australia; 7Academic Department of Adolescent Medicine, University of Sydney, Sydney, NSW 2006, Australia; 8Department of Endocrinology, St Vincent’s Hospital, 390 Victoria Street, Sydney-Darlinghurst NSW 2010, Australia. Introduction: Prader-Willi syndrome (PWS) is a leading genetic cause of obesity, characterised by hyperphagia and endocrine and behavioural complications. The syndrome is associated with increased cardiovascular morbidity and early mortality. Autonomic tone, measurable by analysis of heart rate variability, has been shown to be a cardiovascular risk predictor, and is closely associated with adiposity. It has been suggested that an impairment in autonomic nervous system (ANS) responsiveness could be a cause of cardiovascular morbidity in PWS. However, no differences have been found between people with PWS and BMI-matched controls during orthostatic manoeuvres. Postprandial ANS responsiveness in PWS has not yet, to our knowledge, been studied. Further, due to the relationship between autonomic tone and adiposity, it is desirable to eliminate fat distribution as a confounding factor by matching groups for total and abdominal adiposity. This study assesses basal and postprandial ANS responsiveness in PWS independent of adiposity. Methods: 10 adults with PWS and 10 matched healthy obese subjects consumed a standardised breakfast (600 kCal). Electrocardiographic traces were recorded over a period of 10 minutes at -60, 0, 30, 60, 120 and 240 minute time points. Frequency domain analysis was performed using Fast Fourier Transform to estimate power spectral density in the full spectrum and in low frequency (LF 0.04 - 0.15 Hz) and high frequency (HF 0.15 - 0.40 Hz) bands. Average baseline (-60, 0) and meal (0-240 min) responses were calculated and the effects of Group on log-transformed meal responses were analysed by ANCOVA with log-transformed baseline as covariate. Results: PWS and obese control groups were matched for age, sex, ethnicity, BMI, % total fat and % abdominal fat. There was no difference between groups in systolic blood pressure, diastolic blood pressure or heart rate. Average LF meal response was decreased in the PWS group compared to Obese (p=0.03). No differences were detected between PWS and Obese groups in HF or in HF/LF ratio responses. Conclusion: There was a postprandial defect in ANS responsiveness in adults with PWS. While this impairment had no apparent effect on heart rate, a robust and important predictor of cardiovascular morbidity, the meal-related abnormality we found may contribute to some appetite regulation impairments in PWS. - 19 - Phenomenology of Malignant Hypothermia in PWS Janice Forster MD1, Francie McDougall RN2, Jacqueline Durette APRN, BC2 and Linda Gourash, MD1 1Pittsburgh Partnership, Pittsburgh PA; 2Latham Centers, Brewster MA Background: Persons with PWS have difficulty maintaining core body temperature when ambient temperature changes. In addition to faulty homeostatic mechanisms in the hypothalamus, there is reduced transmission of temperature sensation from the skin; impaired judgment that interferes with selection of appropriate clothing to match the weather; and cognitive inflexibility that interferes with compliance for seasonal changes in clothing. A few individuals have had episodes of sustained (malignant) hypothermia <92oF, severe enough to be life threatening, and these individuals appear to be susceptible to experiencing subsequent episodes. Methods: Literature review and presentation of recent cases of hypothermia in PWS informs the discussion of precipitating factors, phenomenology of symptoms, morbidity, methods of successful intervention and recommended strategies for prevention. Results: Middle aged persons with PWS appear to be more susceptible to malignant hypothermia. They present with medical, cognitive and behavioral symptoms; hypothermia <92oF is usually noted on exam. Infection or sepsis, coagulopathy, adrenal insufficiency, and hypothyroidism are often suspected. Bradycardia and cardiac arrhythmia can occur. Laboratory findings include pancytopenia, hyponatremia, elevated blood urea nitrogen and transaminases, all of which normalize when body temperature returns to baseline. In two cases, external warming was episodically successful but not sustained, resulting in recurrent office visits, emergency room visits and multiple medical admissions for investigation and treatment of hypothermia. Subspecialty consultation included neurology, endocrine, hematology, and cardiology. Symptoms remitted when medications known to be associated with hypothermia were discontinued (Atenolol, Abilify). Discussion: Thermoregulation in typical persons involves afferent sensing, central control and efferent responses. Afferent sensors for cold are located in skin and are triggered by below threshold ambient temperatures. Efferent responses to cold are mediated by cognitively directed behavior and somatosensory mechanisms involving increased sympathetic outflow causing subcutaneous vasoconstriction (alpha 1 adrenergic receptors), increased skeletal muscle tone (shivering) and increased metabolic activity (adrenal secretion of catecholamines; thyroid release of thyroxine). In typical individuals, core temperature is modulated within 0.36 oF through these mechanisms. These mechanisms are not effective in PWS. In a previous study (Hanchett, 1999), persons with PWS were determined to decrease their body temperature by 4-7 oF when challenged by ambient temperatures below 66 oF despite adequate dress and vigorous exercise; all returned to their baseline when ambient temperature normalized, however. In addition to the psychiatric and medical complications of malignant hypothermia, deceased metabolism of medications can also occur contributing to an increased severity of symptoms. Several classes of medication interfere with temperature regulation by inhibiting sympathetic outflow, shivering, and thermogenesis, including opioids, antihypertensives (beta adrenergic antagonists), anesthetics and atypical antipsychotics. Conclusions: Malignant hypothermia is a life threatening problem seen in PWS. Investigation of an underlying medical cause is essential considering iatrogenic etiologies. All individuals with PWS are at risk for mild hypothermia because of impaired peripheral somatosensory and central thermoregulation, poor judgment and cognitive inflexibility. Aging individuals with PWS are at greater risk for malignant hypothermia. Physicians, families and residential providers must learn about the risks of hypothermia in - 20 - PWS. Recommendations include greater supervision and behavioral reinforcement for wearing appropriate clothing, early detection by monitoring vital signs in cold weather, and ongoing monitoring of body temperature in those who have already experienced an episode of malignant hypothermia. Bibliography: Hanchett JE, Hanchett JM: Hypothermia in PWS, presented at the scientific meeting of the PWSA.USA in San Diego in 1999, and published in the Gathered View in 2008. Diaz M and Becker D: Thermoregulation: Physiological and Clinical considerations during sedation and anesthesia, Anesth Prog 57:25-33, 2010. - 21 - Cases of Survival and Death from Gastric Dysmotility in PWS Linda M. Gourash, Janice Forster Pittsburgh Partnership, Pittsburgh, PA Introduction/Background: Abnormalities of smooth muscle are clinically significant in many persons with PWS. Gastric necrosis, rupture and death are described in the literature beginning in 1997 but other important clinical details are still emerging. Additional descriptions of cases of persons who survive gastric dilation are needed in order for clinicians to respond correctly and to guide our surgical colleagues. Methods: Cases of children, adolescents and adults who survived these episodes will be presented highlighting additional understanding gained from direct involvement by the authors in some of these cases. Valuable lessons from a detailed chronology taken from the medical records of a teen with PWS who survived episodic gastric dilation but later died from a final unrecognized episode resulting in gastric perforation will also be reported. Results/Discussion: The condition has been seen at all ages except early childhood and infancy. It is recurrent, but years may pass without problems. Weight does not appear to be a factor. Important preludes appear to be constipation, diarrhea (due to impaction or viral illness), odiferous eructation (“stinky burps”); the last symptom was identified as a helpful warning sign by several parents. Gorging was definitely not a factor in most of our cases. Constipating medications are sometimes but not always present. Refusal of food, distention, abdominal pain and vomiting appear to be later signs and require immediate action. Anecdotally, progression to necrosis and perforation appears within 24-48 hours. Management can be problematic due to unfamiliarity with PWS medical and behavioral characteristics. Important features include the PWS patients’ difficulty in accurately experiencing and reporting abdominal discomfort, late or mitigated appearance of food refusal, vomiting, nausea, abdominal rigidity and inflammatory response. Behavioral issues, including refusal of interventions, can cause misinterpretations of symptoms and can greatly complicate management. Successful recognition and timely action depend heavily on advocacy by parents, familiar caretakers, PCPs, as well as members of the PWSA Clinical Advisory Board. Successful management includes, emergency CT of the abdomen, surgical or GI consultation, NPO and decompression of distended viscus, colonic cleanout where indicated, gradual and closely monitored refeeding. Time until full resolution of the episode varies and careful monitoring is essential. Conclusion: All persons with PWS hospitalized for any reason should be weighed daily and require 1 to 1 supervision at all times both to guarantee no extra food acquisition and to mediate between healthcare providers and the patient. Inappropriate communications with adults with PWS include discussions of uncertain medical possibilities, ambiguous test results and offhand comments or discussions about food or diet which introduce additional uncertainty, stress and behavioral problems. Communications should be done privately with guardians or caretakers who should then interpret to the patient. Prevention for susceptible individuals appears to include careful monitoring of intake and daily bowel patterns and ongoing daily management of constipation. Other factors, no doubt, exist. Continued sharing of crucial clinical details in these cases will guide other clinicians when they are involved in what is often their first experience with this life threatening condition. More detailed but concise information about PWS and gastric dysmotility for the surgical community is needed. 1. Schrander-Stumpel CT, Curfs LM, Sastrowijoto P, Cassidy SB, Schrander JJ, Fryns JP. Prader-Willi syndrome: causes of death in an international series of 27 cases Am J Med Genet A 2004 Feb 1;124A(4):333-8. - 22 - 2. 3. 4. Stevenson DA, Heinemann J, Angulo M, Butler MG, Loker J, Rupe N, Kendell P, Cassidy SB, Scheimann A. Gastric rupture and necrosis in Prader-Willi syndrome. J Pediatr Gastroenterol Nutr. 2007 Aug;45(2):2724. RH. Wharton,*, Wang T , Graeme-Cook F, Briggs S , Cole RE. Acute idiopathic gastric dilatation with gastric necrosis in individuals with Prader-Willi syndrome Am J Med Genet 1997Volume 73, Issue 4, pages 437–441 Turan M, Şen M, Canbay E, Karadayi K Yildiz E: Gastric Necrosis and Perforation Caused by Acute Gastric Dilatation: Report of a Case Surgery Today Volume 33, Number 4, 302-304, - 23 - Autonomic Nervous System (ANS) Dysfunction in PWS and Childhood Obesity: Preliminary Findings Lawrence P. Richer1, Darren S. DeLorey2, Arya M. Sharma3, Felix Kreier4, Michael Freemark5, Michelle L. Mackenzie1 and Andrea M.Haqq1 1Department of Pediatrics, University of Alberta, Edmonton, AB, Canada; 2Faculty of Physical Education and Recreation, University of Alberta; 3Department of Medicine, University of Alberta, Edmonton, AB, Canada; 4Department of Pediatrics, University of Amsterdam, The Netherlands; 5Department of Pediatrics, Duke University, Durham, NC, USA Background:. A number of clinical features in PWS suggest congenital ANS dysfunction, including: viscous saliva, altered gastrointestinal motility and temperature control, hypoglycemia, sleep disturbances, increased pain threshold and a specific neurocognitive profile. Moreover, common causes of mortality in PWS differ from traditional obesity-related causes and may be linked to ANS dysfunction that is unique from the ANS dysfunction associated with general obesity. Methods: All tests were performed in the morning, with standardized restrictions on fluid and salt intake and last meal consumed, in a dedicated pediatric state-of-the-art ANS laboratory. Quantitative Sudomotor Axon Reflex Test (QSART) (Q-Sweat, WR Medical Inc., Stillwater, Minnesota) was used to quantitate the sudomotor (sweat) response to the application of acetylcholine; this provides a measure of post-ganglionic sympathetic function. Heart rate (HR) and blood pressure (BP) were measured non-invasively at a sampling rate of 200Hz. The cardiovagal autonomic testing included: (1) HR response to deep breathing (HRDB) – a preferred and reliable assessment of autonomic control of cardiovascular systems; and (2) HR and BP response and spectral analysis of heart rate variability to head-up tilt (HUT). The pupillary response was assessed as a test of sympathetic innervation of the pupil. Results: 7 children with PWS (Median age = 9.2y; BMI% = 60.8; % Body fat=22.9) and 6 Controls (Median age=12.7 y ; BMI% = 84.0; % Body fat=23.4) were studied. A decrease in sympathetic activity in children with PWS is suggested by: a. decreased low frequency (LF) power at rest and with HUT; b. lower change in HR with head-up tilt; and c. a trend towards lower total sweat volume on Quantitative Sudomotor Axon Reflex Testing (QSART). The QSART data might suggest possible dysfunction in the postganglionic sympathetic nerves in PWS . No difference was observed in the mydriatic response to cocaine, suggesting intact sympathetic innervation of the pupil and a possible difference between rostral and caudal ANS function (as observed in the PWS necdin null mouse model). No difference was observed in predominantly parasympathetic measures of autonomic function including mean HR change with HRDB and the Valsalva ratio. Conclusion: These preliminary findings suggest possible important differences in autonomic cardioregulatory mechanisms between normal control subjects and the children with PWS. Additional subjects are needed for study of ANS dysfunction in PWS. The confirmation of ANS dysfunction in PWS could lead to novel treatment strategies to improve quality of life and prevent premature mortality. - 24 - Progress Report from the Prader-Willi Syndrome Research Strategy Workshop Theresa V. Strong1,2 Jennifer Miller3, Elisabeth M. Dykens4, Rachel Wevrick5, Merlin G. Butler6, Janalee Heinemann7, and Daniel J Driscoll3 1Departments of Medicine and Genetics, University of Alabama at Birmingham, Birmingham, AL, 2 Foundation for Prader-Willi Research, Los Angeles, CA, 3Departments of Pediatrics and Molecular Genetics & Microbiology, University of Florida College of Medicine, Gainesville, FL, 4 Departments of Psychiatry and Pediatrics, Vanderbilt Kennedy Center, Vanderbilt University, Nashville, TN, 5Department of Medical Genetics, University of Alberta, Edmonton, Canada, 6Departments of Psychiatry and Behavioral Sciences and Pediatrics, University of Kansas Medical Center, Kansas City, KS, 7Prader-Willi Syndrome Association (USA), Sarasota, FL. Introduction: The Prader-Willi Syndrome Research Strategy Workshop [November 15-17, 2009], brought together a diverse group of clinical and basic scientists to discuss the strengths, opportunities, gaps in knowledge, and resources needed to advance the science of Prader-Willi syndrome (PWS). Workshop participants focused on five areas of emphasis relevant to PWS: Emerging Clinical Issues, Obesity and Energy Balance, Mental Illness and Psychopathology, Molecular Genetics, and Animal Models. For each area, the current state of knowledge was reviewed, and basic and clinical research questions were prioritized. One overarching theme of the Workshop was the lack of uniformity in assessment of phenotypes in both animal models of PWS and patients. A strong need to develop standardized measures was emphasized. Results/Discussion: To support the recommendations delineated at the Workshop, an international, PWS community-based funding initiative was developed [One SMALL Step]. In the first phase, funding from this initiative has been applied to advance resource development and address several high priority research questions in the field. Multidisciplinary working groups, including an Obesity Clinical Trials Working Group, a Mental Health Working Group, and an Animal Models Working Group, have been convened to develop guidelines to improve uniformity in reporting. The clinical working groups (OCTWG and MHWG) will also provide recommendations on advancing candidate anti-obesity and psychiatric interventions into clinical trials, with special attention to defining informative surrogate endpoints, designing trials with sufficient power to demonstrate efficacy, and consideration of the unique ethical, medical, and logistical challenges that arise in performing clinical trials in this population. A Patient Registry/Biorepository Study group will address the challenge of integrating existing registries, expanding the international registry population, and determining the need and logistics of a PWS biorepository. A web-based Molecular Resource Center has been established to facilitate the exchange of information and reagents among investigators involved in basic PWS research, and support has been allocated for clinical training in PWS research. The Workshop also identified the development and characterization of PWS-derived induced pluripotent stem cells as a priority goal, and funding has been provided to advance that effort. Finally, a Request for Applications has been released to support projects specifically addressing three challenging questions in PWS research: 1. What underlies the shift from failure to thrive to excessive hunger in PWS? 2. Can the maternally silent genes in the PWS region be selectively reactivated? 3. What are the cellular phenotype(s) of PWS? Conclusion: Successful completion of these goals, and the development of additional targets and funding to expediently advance PWS research will be best achieved through the continued engagement of a broad array of stakeholders in this initiative. - 25 - Effects of Early Growth Hormone Therapy in Individuals with Prader-Willi Syndrome Carolina Vac1, Jennifer Miller2, Jonathan Shuster3, and Daniel J Driscoll1,4 1College of Medicine University of Florida; 2Department of Pediatrics, University of Florida; 3Department of Biostatistics, University of Florida; 4Center for Epigenetics, University of Florida Introduction: Studies have shown that children with Prader-Willi syndrome treated with growth hormone have a decrease in fat mass and an increase in lean body mass, as well as an increase in growth velocity and in resting energy expenditure. Studies on growth hormone therapy in infants and toddlers with PWS suggest that early growth hormone treatment may improve acquisition of gross motor milestones and muscle mass, but there is no long term data available at this time on whether these changes persist over time or whether the early treatment affects cognitive development, behavior, or appetite. Individuals with PWS from around the world are followed at the University of Florida as part of an NIH-funded longitudinal study investigating the effects of growth hormone therapy on the natural history of PWS. Participants return annually between ages 1 and 3, and then biennially thereafter, with extremely low attrition rates (<1% attrition). Therefore, in this study we investigated the differences in general intellectual ability, behavior, basal metabolic rate, and body composition between individuals treated in infancy with growth hormone therapy and those treated after age 1. Methods: We analyzed data obtained from 39 individuals who began GH treatment prior to age 1 and 48 individuals who started GH therapy after age 1 with genetically confirmed PWS who were 6-36 years of age at the time the data was obtained. Those who started GH treatment before 1 year of age were significantly younger than those who began treatment later (5.1 vs. 13.3 years; p<0.001) so we performed ANCOVA analysis of the data with age as a covariate. The two groups were compared for BMI Z-score and total body fat by DEXA scan, resting energy expenditure, Woodcock-Johnson Test of Cognitive Abilities (WJ-III), Kaufman Brief Intelligence Test (KBIT-2), and behavioral assessment scores using the Behavioral Assessment Scale for Children (BASC-2). Results and Conclusions: Those who began GH therapy before 1 year of age had a BMI Z-score that was significantly lower than those who started GH later in life (p<0.001). Additionally, those who began treatment before 1 year of age had a lower total percentage of body fat at the time of analysis (p<0.001) and a higher resting energy expenditure (p<0.001) than those who began GH at an older age. Consistent with previous analysis of effects of early GH treatment, those who were treated prior to age 1 had higher verbal skills than those treated later (p=0.02). However, GH treatment prior to age 1 did not have a significant effect on GIA, TIA, working memory, cognitive efficiency, or BSI. Although there was a trend towards higher GIA with early GH treatment, this association was not significant on ANCOVA analysis. Further data will be forthcoming on the entire cohort followed under the auspices of the NIHfunded Rare Disease Consortium. - 26 - The Poster Review - 27 - Biochemical and Molecular Characterization of the Serotonin Receptor 2C (HTR2c) Alternative Splicing Manli Shen1, Serene Josiah2, Ronald Emeson3, Stefan Stamm1 1Department of Biochemistry and Molecular Biology, College of Medicine, University of Kentucky, Lexington, KY, Human Genetic Therapies, Lexington, MA, 3Center for Molecular Neuroscience, Vanderbilt University, Nashville, TN 2Shire Introduction/Background: The Serotonin receptor 2C is crucial for the control of appetite and energy balance. HTR2c-knockout mice develop hyperphagia and obesity andmice with altered serotonin 2C receptor RNA editing display characteristics of Prader-Willi syndrome. HTR2c transcripts undergo extensive processing in the region spanning the competing alternative splicing donor sites of exon5. The RNA there forms an extensive base-paired structure that is subject to RNA editing and regulation by the HBII-52 psnoRNA. Since the regulation of the serotonin receptor is influenced by a psnoRNA missing in PWS, we analyzed its regulation in detail with the aim to identify molecules that influence its processing and possibly influence appetite. Methods: A two-color drug screen was designed to identify chemical modulators of HTR2c splicing. A splicing junction array was then used to find broader targets of one compound Pyrvinium Pamoate (PP) from the screen with the aim to characterize the mechanism of its influence on HTR2c alternative splicing. Results/Discussion: A known DNA intercalater PP was identified as a potent splicing modulator of HTR2c exon5 from the screen. RNA probing assays demonstrated that PP activates the alternative splice site through a change of tertiary structure of the HTR2c pre-mRNA. In vivo splicing assays with mutants changing this structure strongly support the result from the vitro structural analysis. Conclusion: The alternative splicing of the HTR2c appears to be regulated by its structure, which can be influenced by drugs, suggesting a therapeutic avenue for PWS. It is possible that psnoRNAs derived from the HBII-52 cluster generally function by changing the structure of target RNAs. - 28 - Outcomes of Adenotonsillectomy in Prader-Willi Syndrome Patients Stacy Meyer MD, Mark Splaingard MD, Kathyrn Anglin MSN, RN, David Repaske MD., Ph.D., Steven Chung BS, Joan Atkin MD, William Zipf MD, Kris R. Jatana MD Departments: Pediatric Endocrinology, Pediatric Pulmonology/Sleep Medicine, Pediatric Genetics, Pediatric Otolaryngology-Head and Neck Surgery Background: Due to reports of sudden death in children with Prader Willi Syndrome (PWS) on growth hormone, detection of sleep disordered breathing by polysomnography (PSG) has been recommended. However, there is limited data regarding the outcomes of upper airway surgical intervention in PWS patients. Method: Institutional review board approval was obtained. Medical records of 13 patients with PWS who underwent adenotonsillectomy and had pre and post PSG were evaluated to review the efficacy of this treatment in resolution of sleep disturbances. Results: Of the 13 patients included in the review, 46% were female, 61% had genetics consistent with deletion, and the remaining 49% had uniparental disomy as the mode of inheritance. The median age at adenotonsillectomy was 3 years (Range: 6 months to 11 years), and the median age of growth hormone start was 8.5 months (Range: 2 months to 6 years). Nine out of 13 (69%) had mild – moderate obstructive sleep apnea (OSA) or obstructive hypoventilation; 89% normalized after adenotonsillectomy. Four children (31%) had severe OSA prior to surgery. Of these severe OSA patients, 2 normalized after surgery. One of the 2 who did not improve was a 9 month old infant who continued to demonstrate obstructive and central apnea events and was treated with Bipap which was inconsistently worn. His PSG normalized by age 3 years. The other, a 24 month old female, was placed on supplemental oxygen which resolved her central apnea events. Conclusion: We conclude that adenotonsillectomy, while effective in most children with PWS who demonstrate mild to moderate AHI, may not be curative in children with severe OSA. An increase in central apneas can occur in some PWS children post-operatively, and it is important to repeat PSG after upper airway surgical intervention. - 29 - The Australian National Prader-Willi Syndrome Database 2011 Elly Scheermeyer 1,2, Mark Harris3 and Peter Davies1 School of Medicine, University of Queensland, Brisbane, Australia 1, School of Medicine, Bond University, Gold Coast, Australia2, Diabetes & Endocrine, Mater Hospital, Brisbane, Australia 3 In collaboration with the PWS subcommittee of APEG: P. Crock, C. Verge, G. Ambler, G. Werther, P. Bergman, J. Couper, C. Choong, M. Van Driel, P. Hofman, F. Frazer and I.Hughes Introduction/Background: The national Prader-Willi Syndrome (PWS) database was initiated to follow up children with PWS following endorsement of PWS as a specific indication for subsidised growth hormone (GH) treatment up to 18 years. The database aims to provide a reliable estimate of the Australian paediatric population and genetic subtype, collect prospective outcome and safety data of children on GH and looks at various endocrine aspects besides height and weight. This collaboration will facilitate meaningful assessments regarding quality of health interventions and research in the heterogeneous phenotype of this population. Methods: 1) Identification and ethics approvals of paediatric PWS clinics around Australia. 2) Variables identified to be entered on the database. 3) Collaboration between contributing clinicians through the APEG PWS subcommittee and Ozgrow researchers. 4) Agreement on research questions. 5) Obtaining baseline and follow up data via Ozgrow and by direct transfer. 6) Analysis with SPSS 18 and reporting to the team and in publications. Results/Discussion: Information of 240 patients born since 1/1/1989 to 2010 was collected: 149 of these are currently receiving GH. Children with mature bone age (16) are receiving an adult dose. Height SDS (standard deviation scores) of children at base line was well below zero but not significant different (SD) for age groups (1-5 vs 6+ years). Height SDS reduced over 3 year GH therapy in both groups, but more in the younger group (repeated measure analysis from base line). Mean height SDS of children who started under the stringent criteria (GH deficiency or height< 1%, ie before 2009, n=68) vs the current criteria (from 2009, n=68) was SD for the cohorts, but not for age or gender. Mean height SDS improved significantly from baseline after one year GH with the greatest reduction in the 1-5 year old group. Bone age was overall delayed, but there was a significant interaction with gender, especially in the 9-12 year age group. BMI SDS were not different for age or gender at baseline or after 1-2 year GH (2-way ANOVA P>0.05). Repeated measure analysis of the BMI of 92 patients in 5 age groups showed only a marginal increase in BMI (time trend and age SD, P<0.5). Further data may evaluate whether GH assists in curbing the age related rapid weight increase as seen at base line before GH. Conclusion: The PWS database was successfully established with data on body composition and various hormone functions. Our incidence estimate has been refined. The database is continuously growing with the assistance and collaboration of the clinics and the Ozgrow team. Annual reporting and discussion with the team assists in identifying concerns and in optimizing care and best practice of managing PWS in Australia. - 30 -