BMJ letter version 5_simplified
advertisement
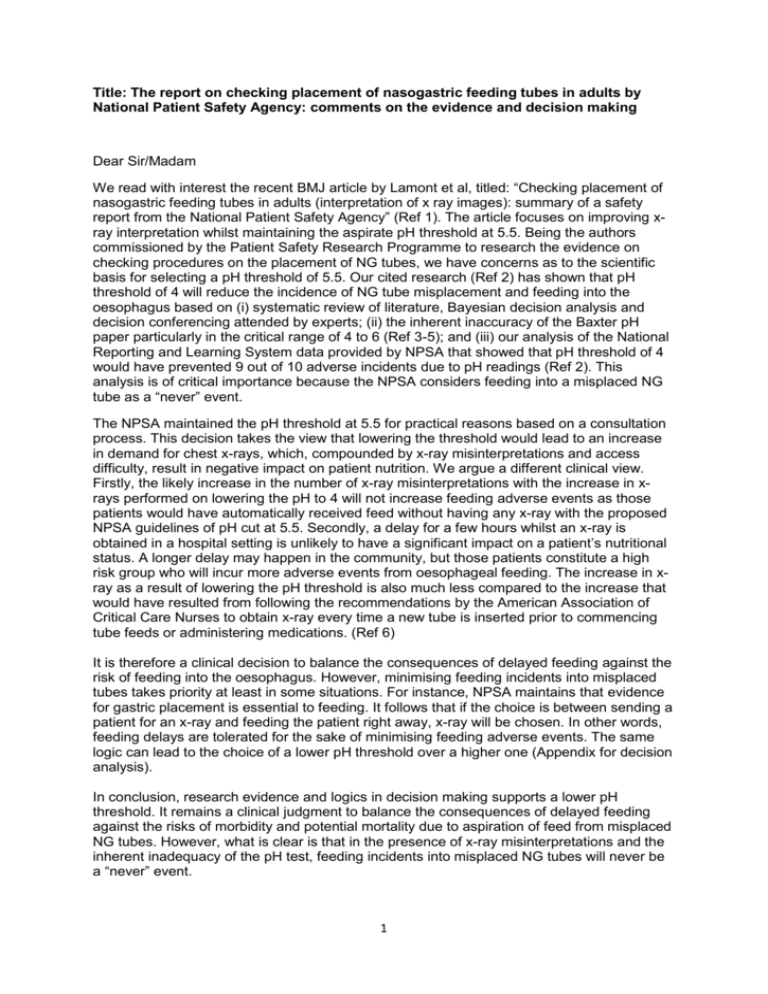
Title: The report on checking placement of nasogastric feeding tubes in adults by National Patient Safety Agency: comments on the evidence and decision making Dear Sir/Madam We read with interest the recent BMJ article by Lamont et al, titled: “Checking placement of nasogastric feeding tubes in adults (interpretation of x ray images): summary of a safety report from the National Patient Safety Agency” (Ref 1). The article focuses on improving xray interpretation whilst maintaining the aspirate pH threshold at 5.5. Being the authors commissioned by the Patient Safety Research Programme to research the evidence on checking procedures on the placement of NG tubes, we have concerns as to the scientific basis for selecting a pH threshold of 5.5. Our cited research (Ref 2) has shown that pH threshold of 4 will reduce the incidence of NG tube misplacement and feeding into the oesophagus based on (i) systematic review of literature, Bayesian decision analysis and decision conferencing attended by experts; (ii) the inherent inaccuracy of the Baxter pH paper particularly in the critical range of 4 to 6 (Ref 3-5); and (iii) our analysis of the National Reporting and Learning System data provided by NPSA that showed that pH threshold of 4 would have prevented 9 out of 10 adverse incidents due to pH readings (Ref 2). This analysis is of critical importance because the NPSA considers feeding into a misplaced NG tube as a “never” event. The NPSA maintained the pH threshold at 5.5 for practical reasons based on a consultation process. This decision takes the view that lowering the threshold would lead to an increase in demand for chest x-rays, which, compounded by x-ray misinterpretations and access difficulty, result in negative impact on patient nutrition. We argue a different clinical view. Firstly, the likely increase in the number of x-ray misinterpretations with the increase in xrays performed on lowering the pH to 4 will not increase feeding adverse events as those patients would have automatically received feed without having any x-ray with the proposed NPSA guidelines of pH cut at 5.5. Secondly, a delay for a few hours whilst an x-ray is obtained in a hospital setting is unlikely to have a significant impact on a patient’s nutritional status. A longer delay may happen in the community, but those patients constitute a high risk group who will incur more adverse events from oesophageal feeding. The increase in xray as a result of lowering the pH threshold is also much less compared to the increase that would have resulted from following the recommendations by the American Association of Critical Care Nurses to obtain x-ray every time a new tube is inserted prior to commencing tube feeds or administering medications. (Ref 6) It is therefore a clinical decision to balance the consequences of delayed feeding against the risk of feeding into the oesophagus. However, minimising feeding incidents into misplaced tubes takes priority at least in some situations. For instance, NPSA maintains that evidence for gastric placement is essential to feeding. It follows that if the choice is between sending a patient for an x-ray and feeding the patient right away, x-ray will be chosen. In other words, feeding delays are tolerated for the sake of minimising feeding adverse events. The same logic can lead to the choice of a lower pH threshold over a higher one (Appendix for decision analysis). In conclusion, research evidence and logics in decision making supports a lower pH threshold. It remains a clinical judgment to balance the consequences of delayed feeding against the risks of morbidity and potential mortality due to aspiration of feed from misplaced NG tubes. However, what is clear is that in the presence of x-ray misinterpretations and the inherent inadequacy of the pH test, feeding incidents into misplaced NG tubes will never be a “never” event. 1 References 1. Lamont T, Beaumont C, Fayaz A, Healey F, Huehns T, Law R, et al. Checking placement of nasogastric feeding tubes in adults (interpretation of x ray images): summary of a safety report from the National Patient Safety Agency. BMJ 2011;342:d2586. 2. Hanna GB, Phillips LD, Priest OH, Ni M. Improving the safety of nasogastric feeding tube insertion. Developing guidelines for the safe verification of feeding tube position - a decision analysis approach. (A report for the NHS patient safety research portfolio.) 2010. 3. Caballero, G.A., et al., Gastric secretion pH measurement: what you see is not what you get! Crit Care Med, 1990. 18(4): p. 396-9. 4. Dobkin, E.D., et al., Does pH paper accurately reflect gastric pH? Crit Care Med, 1990. 18(9): p. 985-8. 5. Bradley, J.S., et al., Clinical utility of pH paper versus pH meter in the measurement of critical gastric pH in stress ulcer prophylaxis. Crit Care Med, 1998. 26(11): p. 1905-9. 6. AACN, AACN practice Alert - Verification of feeding tube placement. American Association of Critical Care Nurses. 2005. 2