What is a heart attack?
advertisement

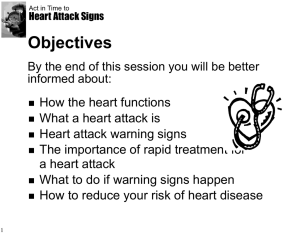
How to Reduce Your Risk of a Heart Attack Heart Attack: Warning Signs and Tips on Prevention What is a heart attack? A heart attack (also called myocardial infarction) is when part of the heart muscle is damaged or dies because it isn't receiving oxygen. Oxygen is carried to the heart by the arteries (blood vessels). Most heart attacks are caused by a blockage in these arteries. Usually the blockage is caused by atherosclerosis, which is the buildup of fatty deposits (called plaque) inside the artery. This buildup is like the gunk that builds up in a drainpipe and slows the flow of water. Heart attacks can also be caused by a blood clot that gets stuck in a narrow part of an artery to the heart. Clots are more likely to form where atherosclerosis has made an artery more narrow. How do I know if I'm having a heart attack? The pain of a heart attack can feel like bad heartburn. You may also be having a heart attack if you: Feel a pressure or crushing pain in your chest, sometimes with sweating, nausea or vomiting. Feel pain that extends from your chest into the jaw, left arm or left shoulder. Feel tightness in your chest. Have shortness of breath for more than a couple of seconds. Don't ignore the pain or discomfort. If you think you are having heart problems or a heart attack, get help immediately. The sooner you get treatment, the greater the chance that the doctors can prevent further damage to the heart muscle. What should I do If I think I am having a heart attack? Right away, call for an ambulance to take you to the hospital. While you wait for the ambulance to come, chew one regular tablet of aspirin. Don't take the aspirin if you're allergic to aspirin. If you can, go to a hospital with advanced care facilities for people with heart attacks. In these medical centers, the latest heart attack technology is available 24 hours a day. This technology includes rapid thrombolysis (using medicines called "clot busters"), cardiac catheterization and angioplasty. In the hospital, you might be given "clot busters" that reopen the arteries to your heart very fast. Nurses and technicians will place an IV line (intravenous line) in your arm to give you medicines. They will also do an electrocardiogram (ECG or EKG), give you oxygen to breathe and watch your heart rate and rhythm on a monitor. Risk factors for a heart attack 1. 2. 3. 4. 5. 6. 7. 8. 9. Smoking Diabetes High cholesterol level High blood pressure Family history of heart attack Atherosclerosis (hardening of the arteries) Lack of exercise Obesity Male sex How can I avoid having a heart attack? Talk to your family doctor about your specific risk factors (see box above) for a heart attack and how to reduce your risk. Your doctor may tell you to do the following: 1. Quit smoking. Your doctor can help you. (If you don't smoke, don't start!) 2. Eat a healthy diet. Cut back on foods high in saturated fat and sodium (salt) to lower cholesterol and blood pressure. Ask your doctor about how to start eating a healthy diet. 3. If you have diabetes, control your blood sugar. 4. Exercise. This sounds hard if you haven't exercised for a while, but try to work up to at least 30 minutes of aerobic exercise (that raises your heart rate) at least 4 times a week. 5. If you're overweight, lose weight. Your doctor can advise you about the best ways to lose weight. 6. If you have hypertension, control your blood pressure 7. Talk to your doctor about whether aspirin would help reduce your risk of a heart attack. Aspirin can help keep your blood from forming clots that can eventually block the arteries. Heart Attack Warning Signs Some heart attacks are sudden and intense -- the "movie heart attack," where no one doubts what's happening. But most heart attacks start slowly, with mild pain or discomfort. Often people affected aren't sure what's wrong and wait too long before getting help. Here are signs that can mean a heart attack is happening: Chest discomfort. Most heart attacks involve discomfort in the center of the chest that lasts more than a few minutes, or that goes away and comes back. It can feel like uncomfortable pressure, squeezing, fullness or pain. Discomfort in other areas of the upper body. Symptoms can include pain or discomfort in one or both arms, the back, neck, jaw or stomach. Shortness of breath. This feeling often comes along with chest discomfort. But it can occur before the chest discomfort. Other signs: These may include breaking out in a cold sweat, nausea or lightheadedness If you or someone you're with has chest discomfort, especially with one or more of the other signs, don't wait longer than a few minutes (no more than 5) before calling for help. Call 9-1-1... Get to a hospital right away. Calling 9-1-1 is almost always the fastest way to get lifesaving treatment. Emergency medical services staff can begin treatment when they arrive -- up to an hour sooner than if someone gets to the hospital by car. The staff are also trained to revive someone whose heart has stopped. You'll also get treated faster in the hospital if you come by ambulance. If you can't access the emergency medical services (EMS), have someone drive you to the hospital right away. If you're the one having symptoms, don't drive yourself, unless you have absolutely no other option. Stroke Warning Signs The American Stroke Association says these are the warning signs of stroke: 1. Sudden numbness or weakness of the face, arm or leg, especially on one side of the body 2. Sudden confusion, trouble speaking or understanding 3. Sudden trouble seeing in one or both eyes 4. Sudden trouble walking, dizziness, loss of balance or coordination 5. Sudden, severe headache with no known cause Cardiac arrest strikes immediately and without warning. If it occurs, call 9-1-1 and begin CPR immediately. Here are the signs of cardiac arrest: Sudden loss of responsiveness. No response to gentle shaking. No normal breathing. The victim does not take a normal breath when you check for several seconds. No signs of circulation. No movement or coughing.