Occupational therapy management plan
advertisement
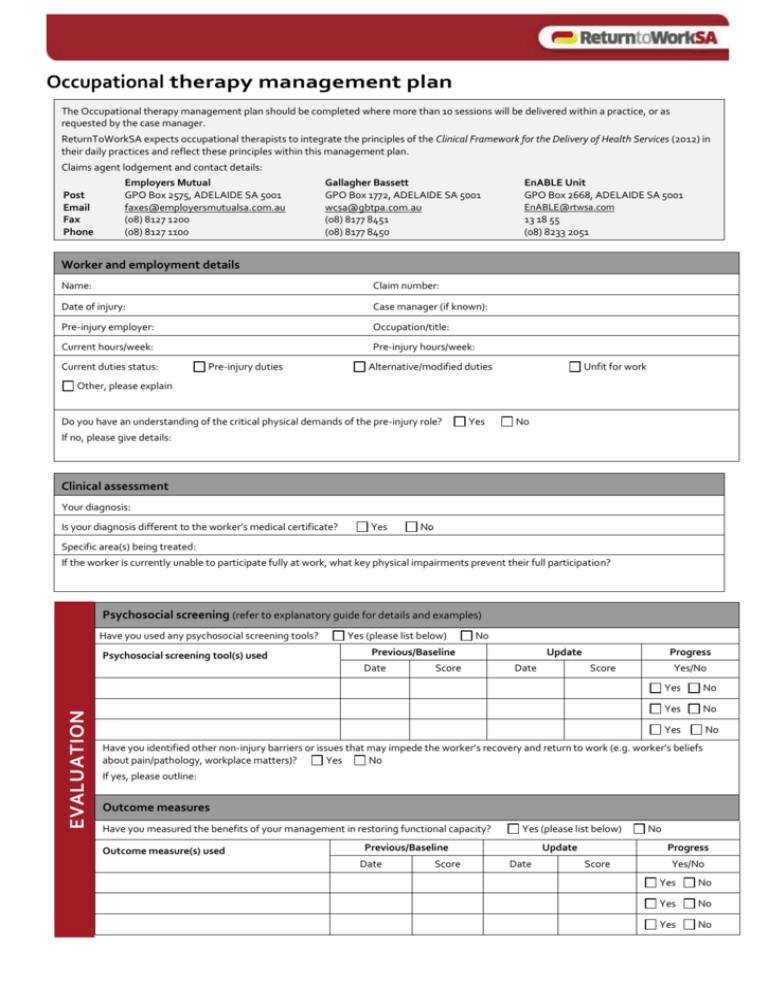
Occupational therapy management plan The Occupational therapy management plan should be completed where more than 10 sessions will be delivered within a practice, or as requested by the case manager. ReturnToWorkSA expects occupational therapists to integrate the principles of the Clinical Framework for the Delivery of Health Services (2012) in their daily practices and reflect these principles within this management plan. Claims agent lodgement and contact details: Post Email Fax Phone Employers Mutual GPO Box 2575, ADELAIDE SA 5001 faxes@employersmutualsa.com.au (08) 8127 1200 (08) 8127 1100 Gallagher Bassett GPO Box 1772, ADELAIDE SA 5001 wcsa@gbtpa.com.au (08) 8177 8451 (08) 8177 8450 EnABLE Unit GPO Box 2668, ADELAIDE SA 5001 EnABLE@rtwsa.com 13 18 55 (08) 8233 2051 Worker and employment details Name: Claim number: Date of injury: Case manager (if known): Pre-injury employer: Occupation/title: Current hours/week: Pre-injury hours/week: Current duties status: Pre-injury duties Alternative/modified duties Unfit for work Other, please explain Do you have an understanding of the critical physical demands of the pre-injury role? Yes No If no, please give details: Clinical assessment Your diagnosis: Is your diagnosis different to the worker’s medical certificate? Yes No Specific area(s) being treated: If the worker is currently unable to participate fully at work, what key physical impairments prevent their full participation? Psychosocial screening (refer to explanatory guide for details and examples) Have you used any psychosocial screening tools? Psychosocial screening tool(s) used Yes (please list below) Date EVALUATION No Previous/Baseline Score Update Date Progress Score Yes/No Yes No Yes No Yes No Have you identified other non-injury barriers or issues that may impede the worker’s recovery and return to work (e.g. worker’s beliefs about pain/pathology, workplace matters)? Yes No If yes, please outline: Outcome measures Have you measured the benefits of your management in restoring functional capacity? Outcome measure(s) used Yes (please list below) Previous/Baseline Date Score Update Date No Progress Score Yes/No Yes No Yes No Yes No Goal setting Goals should relate to return to work, function or other relevant activity participation, be SMART and be developed in collaboration with the worker. Work and functional goals Estimated date of achievement 1. 2. 3. Management to date (at this practice) (If treatment has NOT been provided prior to this plan, go to Proposed management section below) Date of this practice’s initial physiotherapy consult: Has the worker made the progress you expected? If no, outline relevant factors: Total treatments to date at this practice: Yes No Proposed management (at this practice) PLANNING Proposed number of treatments to be delivered: Plan commencement date: treatments over weeks (12 weeks maximum plan duration) Expected discharge date: Briefly outline proposed treatment strategies: Are your management strategies occupationally–specific so as to improve the worker’s capacity to meet the physical demands of their pre-injury duties or suitable employment? Yes No If yes, please outline: Briefly outline your management of any identified psychosocial factors: Do other parties need to be notified/identified to address these psychosocial factors? Case manager Treating doctor Return to work consultant Yes No Other, please outline: If action is recommended, please outline: How is your management plan progressing the worker to self-management and independence? Return to work If the worker is currently unable to participate fully at work, do you think the worker will return to full pre-injury duties and hours? Yes No If yes, in what timeframe? If no, outline why: Do you recommend a graduated return to work schedule for the worker? Yes No Have you communicated your recommendations or the graduated return to work to the treating doctor(s)? Yes No Treating occupational therapist’s details Print name: Practice name: Address: Phone number: Email: Fax number: How would you prefer the case manager to notify you of the receipt of the plan? Email The worker has been involved in the development of this management plan. Yes A copy of this plan has been provided to the case manager, treating doctor and worker. Yes Treating occupational therapist ’s signature: Date: Claims Agent use only Occupational therapist notified of receipt of plan: Yes Date notified: Case manager name: Fax Phone Post Occupational therapy management plan – explanatory guide The Occupational therapy management plan should be initiated and completed by the treating occupational therapist when it is known more than 10 sessions are required to manage a worker with an injury. The completed plan should be submitted to the relevant case manager, and copies provided to the treating doctor and worker. The plan should be invoiced using item number OTMP. Please note: Management plans are practice–specific for individual workers. Worker and employment details • It is expected that the occupational therapist will gain an understanding of the worker’s pre-injury role to ensure delivery of occupational therapy management that is focused on early return to work and restoration to usual functional activities. • Modified duties refer to any changes or restrictions that are applied to a worker’s pre-injury duties to facilitate work participation where the injury prevents full participation. • Alternative duties refer to the worker performing different duties to those in their pre-injury role. Clinical assessment • Your diagnosis may differ from the certifying doctor’s injury description on the Work Capacity Certificate. This information will assist the claims management process by highlighting the need to obtain clarity around the diagnosis. • If your diagnosis differs from that of the certifying doctor, it may be appropriate to have a verbal conversation in which this diagnosis or appropriative management can be clarified for consistency. • Key physical impairments refer to the physical deficits resulting from the work-related injury that are impeding the worker’s functional capacity to participate in their pre-injury role or suitable duties: e.g. Unable to lift >5 kg - Store person with a lower back injury Unable to walk greater than 5 mins and kick start work scooter – postman with a knee injury. Psychosocial screening (Principle 2 of Clinical framework) • Poor or delayed recovery can sometimes be explained by biological factors such as serious injuries or conditions, however psychosocial (non-injury) factors often contribute to poor recovery and RTW outcomes for workers. • Psychosocial risk factors can be screened early using psychosocial questionnaires such as, but not limited to: – Orebro Musculoskeletal Pain Questionnaire (state version used in management plan) – Tampa Scale for Kinaesiophobia – Pain Catastrophisation Scale – Pain Self Efficacy Questionnaire. • Interviewing techniques and comprehensive history taking in the assessment phase can also be used to identify risk factors. • Identification of risk factors early in the assessment phase should inform and guide the occupational therapist ’s treatment. • Psychosocial risk factors may include severe pain and disability reporting, low worker expectations about return to work, greater treatment requirements, low job satisfaction, low self-efficacy, fears and anxieties or workplace matters. Outcome measures (Principle 1 of Clinical framework) • The outcome measure(s) used should be reliable, valid and sensitive to change. • They should relate to the worker’s injury, the functional goals of treatment and functional demands of the pre-injury duties. • Baseline measurement of the worker’s functional capacity should be performed at the commencement of management and then regularly re-measured to assess and demonstrate the benefit in improving their functional capacity. • Outcome measures used may include, but not limited to: – Standardised and area-specific questionnaires (e.g. Neck Disability Index (NDI), Shoulder Pain and Disability Index (SPADI)) – Patient-Specific Functional Scale (PSFS) – Work-specific physical capacity measures (e.g. lifting capacity, walking distance or sitting tolerance) such that improvements in these measures should reflect increases in work capacity. • Physical impairment measures (such as ROM, numerically-rated pain scores, etc.) are clinically useful to track changes within a treatment session, however they do not reflect activity limitations, work capacity or participation restriction and therefore should not be used in isolation. Goal setting (Principle 4 of the Clinical framework) • Occupational therapy goals should relate to function and return to work. • Early and collaborative goal setting ensures that the worker and occupational therapist are focused on similar objectives to achieve recovery and return to work. • Goals should be specific, measurable, appropriate, relevant and timed (SMART). • Examples of SMART Occupational therapy goals include: – To return to work within in 2 weeks on modified duties with lifting capacity of 5kg – Increase work hours from 10 hours/ week to 20 hours/week by 31 December Management to date • If sessions have been provided prior to this management plan, confirm the date of initial consultation and the total number of sessions provided to date. • A ‘session’ refers to an initial or subsequent consultation (inclusive of assessment, treatment, graded activity/exercise, pain management, stress management, relaxation training, biomechanical education and independent living skills training) and splint fabrication/adjustment. • The occupational therapist should indicate whether their treatment to date has achieved the expected recovery in the timeframe they estimated and if the worker has not made the expected progress briefly outline why they think this may be the situation. • Occupational therapy management that has failed to make measured progress towards functional goals, activity-related or participation related goals may be inappropriate for a number of reasons. In these circumstances, it is expected the occupational therapist will reassess the treatment approach, consider other strategies which may include ceasing treatment. Proposed management • Outline the proposed number of treatments required, the duration of the treatment and the anticipated treatment completion date. • Briefly outline proposed treatment strategies. It is expected that passive treatment strategies are used appropriately as the injury demands and there is timely progression to more active and self-efficacious strategies (such as exercise). • The occupational therapist should outline how their strategies will address the worker’s physical impairment findings reported under the Clinical assessment section. Exercises should be condition-specific and occupation-specific so that they simulate work postures, tasks and loads. Successful participation in the exercise program should result in corresponding improvement in technique, physical conditioning and confidence for work-specific tasks. • If psychosocial screening indicates the presence of non-injury risk factors to poor or delayed recovery, outline these risk factors and the occupational therapy management strategies recommended (e.g. improve the worker’s understanding of their injury/pathology or pain thereby promoting empowered decision-making and active coping responses). Psychosocial barriers pertaining to industrial matters, the claim/compensatory system or psychological barriers should be brought to the attention of the case manager, treating doctor/relevant health provider or other relevant party for assessment. • Outline the strategies implemented to support the worker’s self-management and reduced dependence on professional support. Occupational therapy management should work towards a model of self-management and independence. It is expected that occupational therapists will not facilitate patient dependency on passive techniques by administering regular ongoing management for a prolonged period. Workers should be provided with sufficient skills for self-management. (Principle 2, 3, 4 and 5) Return to work • The occupational therapist should provide their opinion about the likelihood of the worker returning to full pre-injury capacity. An understanding of the critical physical demands of the pre-injury role or suitable duties is presumed (refer to Work details section). Where this outcome is likely, the occupational therapist should outline the estimated timeframe for full participation at work. • If the occupational therapist feels that the worker may not be able to return to their pre-injury duties this should be indicated with the relevant factors that lead them to this opinion. • The occupational therapist is expected to provide information to the treating doctor to assist them certify the capacity of the worker. Treating • Following review of the management plan the case manager will notify the treating occupational therapist to acknowledge receipt of the plan and support of the proposed management. The occupational therapist should indicate their preferred method of communication for this process. • It is important that the worker is actively involved in the development of the management plan and that a copy of the plan is made available to them. • A copy of the plan is required to be sent to the case manager and the certifying/treating medical practitioner or referrer. occupational therapists details The following free information support services are available: If you are deaf or have a hearing or speech impairment you can call ReturnToWorkSA through the National Relay Service (NRS): TTY users can phone 13 36 77 and ask for 13 18 55. Speak & Listen (speech-to-speech) users can phone 1300 555 727 and ask for 13 18 55. Internet Relay users connect to NRS on www.relayservice.com and ask for 13 18 55. For languages other than English call the Interpreting and Translating Centre on 1800 280 203 and ask for an interpreter to call ReturnToWorkSA on 13 18 55. For Braille, audio or e-text call 13 18 55. ReturnToWorkSA Enquiries: 13 18 55 400 King William Street, Adelaide SA 5000 info@rtwsa.com www.rtwsa.com © ReturnToWorkSA 2015 Amended: March 2015