DOCX ENG
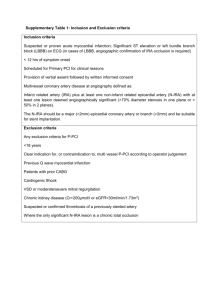
advertisement

B- CRF : Cardiovascular complications E- 05 : Coronary angioplasty or surgery F- 08 : Cardiovascular complications Long-Term Survival and Repeat Coronary Revascularization in Dialysis Patients Following Surgical and Percutaneous Coronary Revascularization with Drug-Eluting and Bare Metal Stents in the United States Gautam R. Shroff, MBBS,1 Craig A. Solid, PhD,2 and Charles A. Herzog, MD1,2 Journal : Circulation Year : 2013 / Month : May Volume : 127 Pages : 1861–1869. ABSTRACT Background Few published data describe long-term survival of dialysis patients undergoing surgical versus percutaneous coronary revascularization in the era of drug-eluting stents (DES). Methods and Results Using United States Renal Data System data, we identified 23,033 dialysis patients who underwent coronary revascularization (6178 coronary artery bypass grafting [CABG], 5011 baremetal stent [BMS], 11,844 DES), 2004–2009. Revascularization procedures decreased from 4347 in 2004 to 3344 in 2009. DES use decreased by 41% and BMS use increased by 85% 2006–2007. Long-term survival was estimated by the Kaplan-Meier method and independent predictors of mortality examined in a comorbidity-adjusted Cox model. In-hospital mortality for CABG patients was 8.2%; all-cause survival at 1, 2, and 5 years was 70%, 57%, and 28% respectively. In-hospital mortality for DES patients was 2.7%; 1, 2, and 5 year survival was 71%, 53%, and 24% respectively. Independent predictors of mortality were similar in both cohorts: age >65 years, white race, dialysis duration, peritoneal dialysis, and congestive heart failure, but not diabetes. Survival was significantly higher for CABG patients who received internal mammary grafts (IMG) (HR 0.83, P<0.0001). Probability of repeat revascularization accounting for the competing risk of death was 18% with BMS, 19% with DES, and 6% with CABG at 1 year. Conclusions Among dialysis patients undergoing coronary revascularization, in-hospital mortality was higher after CABG but long-term survival was superior with IMGs. In-hospital mortality was lower for DES patients, but probability of repeat revascularization was higher and comparable to BMS patients. Revascularization decisions for dialysis patients should be individualized. Keywords: coronary, dialysis, drug-eluting stent, survival COMMENTS Cardiac disease is a major cause of mortality among dialysis patients; according to recent estimates, it accounts for about 38% of all-cause deaths, and about 13% of cardiac deaths are ascribed to myocardial infarction.Patients with end-stage renal disease (ESRD) undergoing maintenance dialysis have been excluded from any randomized evaluation of the comparative efficacy of coronary revascularization strategies. Thus, the optimal option for coronary revascularization in dialysis patients remains a matter of debate.. Using USRDS data, the authors sought to evaluate long-term survival rates and probability of repeat coronary revascularization of dialysis patients undergoing surgical and percutaneous coronary revascularization in the contemporary era, and to identify independent predictors of mortality. From the Registry, 6178 CABG patients, 5011 BMS patients, and 11,844 DES patients were identified in the study period. Median follow-up periods were 1.63 years for CABG (25th percentile, 0.55; 75th percentile, 2.96), 1.60 years for DES, (0.75, 2.96), and 0.99 years for BMS (0.47, 2.26). A greater proportion of younger patients underwent surgical revascularization procedures than percutaneous procedures (P < 0.0001). Among patients who underwent CABG with IMG, 43% were aged 45 to 64 years, 12% 75 to 79 years, and only 7% older than 80 years. Among patients who underwent PCI with DES, however, 35% were aged 45 to 64 years and 31% 65 to 74 years, and proportions in older age groups were relatively higher; 16% were aged 75 to 79 years and 14% 80 years or older. At 12 months after the index revascularization, all-cause survival for CABG with IMG was 72%, versus 64% for CABG without IMG. At 2 years, patients who underwent CABG with IMG had a significant survival advantage (59.6%) compared with patients who underwent CABG without IMG (50.6%, P < 0.0001), a difference that persisted in longer-term follow-up. For patients undergoing percutaneous revascularization, in-hospital mortality was 2.7% for DES and 4.9% for BMS (P < 0.0001). Thus, in-hospital mortality was significantly higher in the context of surgical vs. percutaneous revascularization (8.2% vs. 3.4%, P < 0.0001). Of 6178 patients who originally underwent CABG, 773 (12.5%) underwent a repeat coronary revascularization procedure; of 11,844 patients who originally received DES, 3404 (28.7%) underwent a repeat procedure, and of 5011 who originally received BMS, 1246 (24.9%) underwent a repeat procedure. In summary, regarding the optimal revascularization strategy in this high-risk population the authors propose the alternative: high in-hospital mortality rates but superior long-term survival (especially with use of IMGs) with surgical revascularization, and higher short-term survival but higher probability of repeat revascularization with percutaneous revascularization using BMS and DES. They quote also a recent shift in interventional practice patterns in US dialysis patients, with a decrease in DES use and a corresponding rise in BMS use. Pr. Jacques CHANARD Professor of Nephrology