NOVA ABC Medical History Form - Northern Virginia Area Bariatric
advertisement

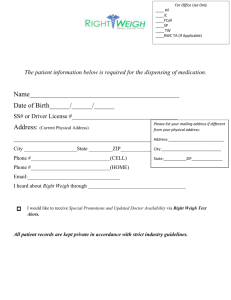
New Patient Form PATENT INFORMATION FORM PATIENT NAME: LAST___________________FIRST________________MI___ PATIENT ADDRESS_________________________________________________ CITY_____________________________STATE_________ZIP_______________ HOME PHONE_____________________CELL____________________________ E-MAIL____________________________________________________________ BIRTH DATE_____________________AGE______SEX M F EMPLOYMENT INFORMATION PATIENT EMPLOYER________________________OCCUPATION___________ EMPLOYER ADDRESS_______________________________________________ CITY___________________________________STATE_______ZIP___________ WORK PHONE NO__________________________EXTENSION_____________ IN CASE OF EMERGENCY NAME___________________________________RELATIONSHIP____________ PHONE__________________________________ PATIENT'S SPOUSE_______________________PHONE____________________ FAMILY PHYSICIAN______________________PHONE____________________ HOW DID YOU HEAR ABOUT OUR PRACTICE: INTERNET_____YELLOW PAGES_____ PHYSICIAN (PLEASE NAME) ________________________________________ FRIEND (PLEASE NAME)____________________________________________ OTHER (PLEASE NAME)_____________________________________________ Nova ABC Weight Loss Center requires a $75 deposit to reserve an initial appointment with the doctor. This charge will be applied to your first visit; or is fully refundable as long as the office is given no less than 24 hours’ notice of cancelation. IF YOU ARE CALLING TO CANCEL AFTER HOURS. YOU CAN LEAVE A MESSAGE ON THE MACHINE BY DIALING 703-494-1020 AND PRESSING #8 In addition, there will be a $50 charge in the event that a patient makes and cancels the first appointment and then reschedules a second appointment and fails to keep that second appointment. In this event the 24 hour rule is waived. YOU MUST KEEP THE SECOND APPOINTMENT IN ORDER TO AVOID THE $50 CHARGE. THERE WILL BE NO EXCEPTIONS TO THIS RULE. We offer prepaid weekly and bi-weekly visits at a discounted rate THESE VISITS EXPIRE, the weekly prepaid visits are good for 5 weeks and the biweekly are good for 6 weeks. I have read and understand the above and agree to these terms. ______________________ _______________ SIGNATURE DATE FIRST APPOINTMENT REQUIREMENTS PLEASE DO NOT WEAR ANY OILS, LOTIONS, OR CREAM THE DAY OF THE TEST LABWORK CMP, CBC, LIPID PANEL, FREE T4, URIC ACID, TSH, PHOS PREP FOR METABOLIC TEST: NO EXERCISE OF CAFFEINE THE DAY OF THE APPOINTMENT 4 HOUR FAST (NOTHING BUT WATER) PRIOR TO THE TEST New Patient Privacy Forms Northern Virginia Area Bariatric Consultants Privacy Practices This notice describes the way in which medical and personal information pertaining to you may be used and disclosed. It also, explains how you can access your health information. Please review it carefully and sign the attached acknowledgement receipt at the bottom of this notice and return it to the receptionist. At Northern Virginia Area Bariatric Consultants the staff is committed to the protection of your private health information. Within our office access to your information is limited to those employees who need access in order to perform their jobs. Northern Virginia Area Bariatric Consultants may use and disclose protected health information in order to facilitate treatment, collect payments and for internal healthcare operations. Examples of these include, but are not limited to referral to other healthcare providers, life insurance physicals, and home healthcare agencies. Payment examples include your health insurance provider for claims and coordination of benefits, workman's compensation or similar programs: Collections agencies, etc. Healthcare operations include auditing of records and internal quality control. Northern Virginia Area Bariatric Consultants is required by law to use and/or disclose protected health information without the patients' written consent or authorization in certain circumstances. These include reporting a crime, responding to a subpoena, warrant or court order; public health officials concerned with controlling disease, disability and injury. Northern Virginia Area Bariatric Consultants may use or disclose protected health information to your personal representative whom you have authorized to act on your behalf in making decisions related to your health care. NOVA ABC Weight Loss Clinic will contact patients at phone numbers provided to us by the patient in order to give appointment reminders or other information regarding treatment and/or tests results. NOVA ABC Weight Loss Clinic will not use or disclose a patients protected health information as is described in this notice without the individual's written authorization. This authorization may be revoked at any time in writing. Exceptions are those described above as required by law. NOVA ABC Weight Loss Clinic will abide by this notice which is currently in effect as of April 14, 2003, at the time of disclosure. We reserve the right to revise the terms of this notice and make new provisions effective for all protected health information we maintain. NOVA ABC Weight Loss Clinic will keep a posted copy of our current privacy practices in our lobby area. Copies of this notice may also be obtained at any time in our office. Any person/patient, who believes their privacy rights have been violated, may register a complaint with our office manager at 703-494-1020; and to the Secretary of Health of Human Services. It is our office policy that no retaliatory action will be made against any individual who submits a complaint of non-compliance of the privacy standards You have the legal right to inspect copies of your protected health information. This requires a written, signed and dated request. (as allowed by State law, reasonable copy fees may apply) If you believe your health information is inaccurate or incomplete, you may request to amend your information. In the event that we deny your request, we will inform you of our reasons for such a denial in writing. You have the legal right to request restrictions on certain uses of your protected health information as provided by 45CFR 154.522(a). By law we are not required to comply with a requested restriction. Acknowledgement of Privacy Practices: I have received a notice of privacy practices, outlining my rights regarding my protected health information and the specific ways in which my private health information may be used and disclosed as allowed under state and federal law. Patient or legal Representative___________________________Date_____________ Relationship of above if not signed by patient_________________________________ In the event patient refused to sign________________________________________ Document by________________________________________________________ WEIGHT LOSS CONSENT FORM I_______________________________authorize Dr William C. McCarthy and his staff at Northern Virginia Area Bariatric Consultants to help me in my weight reduction efforts. I understand that my program may consist of a balanced diet, a regular exercise program, instruction in behavior modification techniques, and may involve the use of appetite suppressant medications. Other treatment options may include a very low calorie diet, or a protein supplemented diet. I further understand that if appetite suppressants are used, they may be used for durations exceeding those recommended in the medication package insert It has been explained to me that these medications have been used safely and successfully in private medical practices as well as in academic centers for periods exceeding those recommended in the product literature. I understand that any medical treatment may involve risks as well as the proposed benefits. I also understand that there are certain health risks associated with remaining overweight or obese. Risks of this program may include, but are not limited to, nervousness, sleeplessness, headaches, dry mouth, gastrointestinal disturbances, weakness, tiredness, psychological problems, high blood pressure, rapid heartbeat and heart irregularities. These and other possible risks could, on occasion be serious or even fatal. Risks associated with remaining overweight are tendencies to high blood pressure, diabetes, heart attack and heart disease, arthritis of the joints including hips, knees, feet and back, sleep apnea, and sudden death. I understand that these risks may be modest if I am no significantly overweight, but will increase with additional weight gain. I understand that much of the success of the program will depend on my efforts and that there are no guarantees or assurances that the program will be successful. I also understand that obesity may be a chronic, life-long condition that may require changes in eating habits and permanent changes in behavior to be treated successfully. I have read and fully understand this consent form and I realize I should not sign this form if all items have not been explained to me. My questions have been answered to my complete satisfaction. I have been urged and have been given all the time I need to read and understand this form. If you have any questions regarding the risks or hazards of the proposed treatment, or any questions whatsoever concerning the proposed treatment or other possible treatments, ask your doctor now before signing this consent form. Date_______________________________________Time___________________ Witness________________________________Patient______________________ Weight-Loss Consumer Bill of Rights WARNING: Rapid weight loss may cause serious health problems. Rapid weight loss is weight loss of more than 1 1/2 pounds to 2 pounds per week or weight loss of more than 1 percent of body weight per week after the second week of participation in a weight loss program. Consult your personal physician before starting any weight loss program. Only permanent lifestyle changes such as making healthful food choices and increasing physical activity, promote long-term weight loss. Qualifications of this provider are available upon request. You have the right to ask questions about the potential health risks of the program and its nutritional content, psychological support, and educational components; receive an itemized statement of the actual or estimated price of the weight loss program, including extra products, services, supplements, examinations and laboratory tests; know the actual or estimated duration of the program. I have read the above: Patient's Signature_______________________________Date_______________ Release of Medical Records I give permission for my medical records (blood work, chart, EKG) to be release to: Name_________________________________________________ Signature__________________________Date_____________________________ "BEFORE" AND "AFTER" PHOTOS I_____________________________________, give my permission for NOVA ABC to take my "before" and "after" photographs. (photographs will not be used for advertising without patient permission) Signature____________________________________________________________ PATIENT INFORMED CONSENT FOR APPETITE SUPPRESSANTS I. Procedure and Alternatives: 1. I______________________________________(patient or patient's guardian) authorize Dr. William C. McCarthy to assist me in my weight reduction efforts. I understand my treatment may involve, but not be limited to, the use of appetite suppressants for more than 12 weeks and when indicated in higher doses than the dose indicated in the appetite suppressant labeling. 2. I have read and understand my doctor's statements that follow: "Medications, including the appetite suppressants, have labeling worked out between the makers of the medication and the Food and Drug Administration. This labeling contains, among other things, suggestions for using the medication. The appetite suppressant labeling suggestions are generally based on the shorter term studies (up to 12 weeks) using the dosages indicated in the labeling. "As a bariatric physician, I have found the appetite suppressants helpful for periods far in excess of 12 weeks, and at times in larger doses than those suggested in the labeling. As a physician, I am not required to use the medication as the labeling suggests, but I do use the labeling as a source of information along with my own experience, the experience of my colleagues, recent longer term studies and recommendations of university based investigators. Based on these, I have chosen, when indicated, to use the appetite suppressants for longer periods of time and at times, in increased doses." "Such usage has not been as systematically studied as that suggested in the labeling and it is possible, as with most other medications, that there could be serious side effects (as noted below)." "As a bariatric physician, I believe the probability of such side effects is outweighed by the benefit of the appetite suppressant use for longer periods of time and when indicated in increased doses. However, you must decide if you are willing to accept the risks of the side effects, even if they might be serious, for the possible help the appetite suppressants use in this manner may give." 3. I understand it is my responsibility to follow the instructions carefully and to report to the doctor treating me for my weight any significant medical problems that I think may be related to my weight control program as soon as reasonably possible. 4. I understand the purpose of this treatment is to assist me in my desire to decrease my body weight and to maintain this weight loss. I understand my continuing to receive the appetite suppressant will be dependent on my progress in weight reduction and weight maintenance. 5. I understand there are other ways and programs that can assist me in my desire to decrease my body weight and to maintain this weight loss. In particular, a balanced calorie counting program or and exchange eating program without the use of the appetite suppressant would likely prove successful if followed, even though I would probably be hungrier without the appetite suppressants. II. Risks of Proposed Treatment I understand this authorization is given with the knowledge that the use of the appetite suppressants for more than 12 weeks and in higher doses than the dose indicated in the labeling involves some risks and hazards. The more common include nervousness, sleeplessness, headaches, dry mouth, weakness, tiredness, psychological problems, medication allergies, high blood pressure, rapid heartbeat and heart irregularities. Less common, but more serious, risks are primary pulmonary hypertension and valvular heart disease. These and other possible risks could, on occasion, be serious or fatal. III. Risks Associated with Being Overweight or Obese: I am aware that there are certain risks associated with remaining overweight or obese. Among them are tendencies to high blood pressure, to diabetes, to heart attack and heart disease, and to arthritis of the joints, hips, knees and feet. I understand these risks may be modest if I am not very much overweight but that these risks can go up significantly the more overweight I am. IV. No Guarantees: I understand that much of the success of the program will depend on my efforts and that there are no guarantees or assurances that the program will be successful. I also, understand that I will have to continue watching my weight all of my life if I am to be successful. V. Patient's Consent: I have read and fully understand this consent form and I realize I should not sign this form if all items have not been explained, or any questions I have concerning them have not been answered to my complete satisfaction. I have been urged to take all the time I need in reading and understanding this form and in talking with my doctor regarding risks associated with the proposed treatment and regarding other treatments not involving the appetite suppressants. IF YOU HAVE ANY QUESTIONS AS TO THE RISKS OR HAZARDS OF THE PROPOSED TREATMENT, OR ANY QUESTIONS WHATSOEVER CONCERNING THE PROPOSED TREATMENT OR OTHER POSSIBLE TREATMENTS, ASK YOUR DOCTOR NOW BEFORE SIGNING THIS CONSENT FORM. DATE_____________________________TIME_________________________ PATIENT____________________________WITNESS___________________ (can be signed by legal guardian if patient is a minor) VI. PHYSICIAN DECLARATION: I have explained the contents of this document to the patient and have answered all the patient's related questions, and to the best of my knowledge, I feel the patient has been adequately informed concerning the benefits and risks associated with the use of the appetite suppressants, the benefits and risks associated with alternative therapies and the risks of continuing in an overweight state. After being adequately informed, the patient has consented to therapy involving the appetite suppressants in the manner indicated above. Physician's Signature_________________________________________________ NOVA ABC Hours of Operation and Cancellation Policy We make every effort to make sure your visits are pleasant and efficient for you. Please make every effort to arrive at your appointment on time. If you are unable to make your scheduled time just call and notify our office. (AFTER HOURS YOU CAN LEAVE A MESSAGE ON OUR PHONE) Or email us at novaabc@novaabc.com Our patient hours are as follow: Monday 12:30 pm -7 pm Tuesday 12:30 pm -7 pm Wednesday 6:30 am -11:30 am Thursday 6:30 am -1 pm Friday 6:30 am-10 am Phone hours are available to make appointments between 9 am - 4 pm Monday-Tuesday, 9 am - 2 pm Wednesday-Thursday and Fridays between 6:30am - 12 pm (these hours are subject to change depending on staff availability) If you need to miss an appointment please call 24 hours in advance to cancel in order to avoid a $50.00 no-show fee. Again you can call after hours and leave a message on our answering machine. Our phone number is 703-494-1020 and press #8 to leave a message. I ACKNOWLEDGE THE ABOVE MENTIONED NO-SHOW POLICY AND UNDERSTAND I WILL BE CHARGED $50.00 FOR FAILURE TO GIVE 24 HOURS NOTICE TO THE OFFICE OF CANCELLATION. ______________________________________ _________________________ NAME DATE New Patient History Forms NOVA ABC Medical History Form Name: ________________________________ Age: ___________________ Sex: M F (circle one) Family Physician: ______________________ Phone: _________________________ Present Status: 1. Are you in good health at the present time to the best of your knowledge? Y 2. Are you under a doctor’s care at the present time? Y N N If yes, for what? ________________________________________ 3. Are you taking any medications at the present time? Y N What: ______________________ Dosage: ___________________ What: ______________________ Dosage: ___________________ 4. Any allergies to any medications? Y N What: _________________________________________________ 5. History of high blood pressure? Y N 6. History of pre-diabetes or diabetes? Y N At what age? ___________________________________________ 7. History of heart attack or chest pain? Y 8. History of swelling feet? Y N N 9. History of frequent headaches? Y N Migraines? Y___ N ___ Medications for headaches: __________ 10. History of sleep apnea? Y___ N___ Have you ever had a sleep study? Y N Result: Do you snore? Y___ N___ Have you been told you quit breathing while sleeping? Y___ N___ Do you fall asleep while driving, riding in a car >30 min, reading, or watching TV? Describe __________________________________________________________________ 11. History of constipation (difficulty in bowel movement)? Y N 12. History of glaucoma? Y N 13. Gynecologic history: Pregnancies: Number: _________Dates: _____________________________________________ ________________________________________________________________________________ Is there any chance of pregnancy now? Y___ N___ Natural delivery or C-Section (specify): _____________________ Complications of pregnancy (e. g. gestational diabetes, preeclampsia, eclampsia, etc.) Describe: _______________________________________________________________________ ________________________________________________________________________________ Menstrual: Onset Age: _____ Regular: Y___ N___ If periods are not regular (not regular, excessively heavy, etc.), please describe_________________________________________________________________________ ________________________________________________________________________________ Have you ever been diagnosed with polycystic ovary syndrome? Y___ N___ Pain associated: Y___ N___ Last menstrual period: ___________ Hormone Replacement Therapy: Y N What: __________________________________________ Birth Control Pills: Y N Type: _________________________________________________ Last Checkup:__________________________________________ 14. Serious Injuries: Y N Specify: ____________________________________________________________________ 15. Any surgery: Y N Specify: _________________________________ Date: _____________________________ Specify: _________________________________ Date: _____________________________ 16. Family History: Age Health Disease Cause of Death Overweight? Father: ________________________________________________________________________ Mother: _______________________________________________________________________ Brothers: ______________________________________________________________________ Sisters: ________________________________________________________________________ Has any blood relative ever had any of the following: Glaucoma: Y Asthma: Y Epilepsy: Y N Who: ______________________________ N Who: ______________________________ N Who: ______________________________ High Blood Pressure Y Kidney disease: Y Diabetes: Y N Who: ______________________________ N Who: ______________________________ N Who: ______________________________ Tuberculosis: Y N Who: ______________________________ Psychiatric Disorder Y Heart disease/stroke Y N Who: ______________________________ N Who: ______________________________ Past Medical History: (circle all that apply) Polio Measles Tonsillitis Jaundice Mumps Pleurisy Kidneys Scarlet Fever Liver Disease Lung Disease Whopping Cough Chicken Pox Rheumatic Fever Bleeding Disorder Nervous breakdown Ulcers Gout Thyroid Disease Anemia Heart Valve Disorder Heart Disease Tuberculosis Gallbladder Disorder Psychiatric Illness Drug Abuse Eating Disorder Alcohol Abuse Pneumonia Malaria Typhoid Fever Cholera Cancer Blood transfusion Arthritis Osteoporosis Other: ________ Nutrition Evaluation: 1. Present weight: Height (no shoes): Desired weight: 2. In what time frame would you like to be at your desired weight? ________________ 3. Birth Weight: Weight at 20 years of age: Weight one year ago: 4. What is the main reason for your decision to lose weight? ______________________ 5. When did you begin gaining excess weight? (Give reasons, if known); ___________ _______________________________________________________________________ 6. What has been your maximum lifetime weight (non-pregnant) and when? ________________________________________________________________________ 7. Previous diets you have followed: Give dates and results of your weight loss: ____________________________ ____________________________ ____________________________ 8. Is your spouse, fiancé or partner overweight? Y By how much is he or she overweight? 9. How often do you eat out? N 10. What restaurants do you frequent? 11. How often do you eat fast foods? 12. Who plans meals? Cooks? Shops? 13. Do you use a shopping list? Y N 14. What time of the day and what day do you shop for groceries? 15. Food Allergies (list): 16. Food dislikes (list): 17. Foods you crave: 18. Any specific time of the day or month do you crave food? 19. Do you drink coffee or tea? Y N 20. Do you drink soft drinks? Y N 21. Do you drink alcohol? Y N 22. Do you use a sugar substitute? Y How much daily? How many daily? Diet or regular? How much? N 23. Do you awaken hungry during the night? Y N What do you eat? Have you ever found evidence of night time eating without your knowledge?____________ 24. What are your worst food habits? Do you binge eat? Y___ N ___ How often? _________________________________________ 25. Have you ever induced vomiting or taken laxatives or diuretics for weight loss? Have you ever been diagnosed with bulimia? Y____ N___ Have you ever been diagnosed with Anorexia Nervosa? Y___ N___ 26. Snack Habits: What? When? How Much? 27. When you are under a stressful situation at work or family related, do you tend to reach more? Explain: 28. Do you think are currently undergoing a stressful situation or an emotional upset? Explain: 29. Smoking habits: (answer only one) ____ You have never smoked cigarettes, cigars or a pipe ____ You quit smoking _______ years ago and have not smoked since_________ ____ You have quit smoking cigarettes at least one year ago and now smoke cigars or a pipe without inhaling smoke ____ You smoke 20 cigarettes per day (1 pack) ____ You smoke 30 cigarettes per day (1 1/2 pack) ____ You smoke 40 cigarettes per day (2 packs) 30. Typical Breakfast Typical Lunch Typical Dinner Time eaten: ______________Time eaten:_________________ Time eaten:___________________ Where: _____________________________________________ With whom: _________________________________________ 31. Describe your usual energy level: 32. Activity Level: (answer only one) ____ Inactive not regular physical activity with a sit-down job. ____ Light activity no organized physical activity during leisure time. ____ Moderate activity-occasionally involved in activities such as weekend golf, tennis, jogging, swimming or cycling. ____ Heavy activity consistent lifting, stair climbing heavy construction, etc. or regular ____ Vigorous activity participation in extensive physical exercises for at least 60 minutes per session 4 times per week. 33. Behavior style: (answer only one) ____ You are always calm and easy going. ____ You are usually calm and easy going. ____ You are sometimes calm with frequent impatience. ____ You are seldom calm and persistently driving for advancement. ____ You are hard-driving and can never relax. Current Symptoms (please circle if present) General: Appetite Increase Appetite Decrease Chills Fatigue Fever Sweats Eyes Last check up (Date or how long ago)__________ Blurred vision Double vision Cataracts Eye pain Redness Glaucoma Y N Recent change in vision Y N Ears Decreased hearing Pain Ringing/Use of hearing device Y N Nose Allergies Congestion Obstruction Y N Throat Enlarged tonsils Snoring Sore throat trouble swallowing Y N Cardiovascular Chest pain or pressure, fainting or black out spells / Heart murmur Palpitations(racing heart or skipped beats) Shortness of breath Trouble lying flat Swelling in legs or feet Respiratory (Lungs) Congestion Cough Rattling or wheezing Stomach and gastrointestinal Last colonoscopy (year) ______ Bloody stools Cramps Constipation Diarrhea Heartburn or reflux Nausea Pain Vomiting Muscles, joints, and bones Arthritis Back pain Joint pain or stiffness (where)______________________________________ Morning stiffness Muscle pain Muscle weakness Skin Acne Dry or scaly Itching Lump, nodule, or mole (where)______________ Nail changes Rash (where)________________ Breast Last mammogram___________ Discharge Lump Pain Rash or redness Neurologic Forgetfulness Numbness Weakness Psychiatric Anxiety Crying spells Depression Insomnia Panic attacks Rage or temper problems Suicidal feelings Hormones (Circle all that applies) Excessive hunger Excessive thirst Decreased libido Hoarseness Recent hair growth Hormones (Female) Last female exam ________ Change in periods Y N Blood and circulation Clotting problems Easy bruising Allergy and immune Frequent infection Seasonal allergies Please describe your general health goals and improvements you with to make: What kind of dietary approach do you feel is best for you? (Circle one, feel free to leave blank, we’ll go over this): ALL FOOD, PARTIAL MEAL REPLACEMENT (USE A MEAL REPLACEMENT FOR ONE OR MEALS DAILY, OR TOTAL MEAL REPLACEMENT (Very low calorie protein Sparing fast for quicker weight loss). Do you feel you will need medication for appetite suppression? Do you want vitamin B12 shots? (These are not given routinely, but many patients request them) Y N This information will assist us in assessing your particular problem areas and establishing your Medical management. Thank you for your time and patience in completing this form.